Lecture Notes
Intro to Pathogenesis (3/3) - Wk 5
Pathogenesis: The biological mechanisms that lead to disease
how viruses make us sick
Common Symptoms - from Innate
Fever
Redness/swelling/rashes
mucus
body aches
Immune system composed of:
Proteins (cytokines & antibodies)
Non-protein molecules ( histamines and leukotrienes)
Cells (macrophages, neutrophil, T cells)
Tissues (GALT)
Organs (bone marrow, thymus, spleen)
Innate
non specific; born with it
antigens
minutes to hours
Adaptive
specific defenses
Activated by innate
several days
Sections of Innate
Chemical defense
Cellular defense
Pathogen recognition & phagocytosis
Chemical
Acute phase proteins
Cytokines
Inflammation eliciting mediators
antimicrobial peptides
plasma protein mediators
chemical & enzymatic mediators found in bodily fluids
Cytokines
soluble proteins that act as communication
Autocrine - act on same cell
Paracrine - act on a nearby cell
Endocrine - travel through blood stream
Important cytokines
IL-x
Chemokines
Interferons
Cellular Immunity
Hematopoeisis
PMNs
Macrophages
DCs
Diapedesis or extravasion
PAMPS & PRRs
once binded - signal transduction results in transcriptional changes
recruit DCs - carry phagocytosed microbes to present to the adaptive immune system
Innate immune system is very dependent on phagocytic cells that each serve a different purpose:
Macrophages - surveillance and recruitment
found in tissues and blood stream
Neutrophils - infection control w/in 30 min
DCs - APCs
Pathogenesis of Rhinovirus & Flu (3/4) - Wk 5
Rhinvirus
ssRNA (+) genome
Family Picornaviridae
Naked, iscosahedral
Have only 10-11 genes
Use endosomal entry - use of ICAM - 1 host cell receptors
Rhinovirus Immune Activation
Viral RNA is a PAMP
Binds to PRRs in the endosome
Results in transcription of cytokines by turning on transcription factors through signal transduction
cause a release of cytokines
Rhinovirus: The Uncommon Cold
Individuals with and without asthma had roughly equal nasal viral loads (amount of viruses in their noses)
P value indicate the likelihood that the two groups are not different from each other
Individuals with asthma
worse upper respiratory symptoms
much worse lower respiratory symptoms
worse peak expiratory flow
how much free flow the pts have
By day four asthmatic pts are more symptomatic
Asthmatics have more cytokine release - more inflammation
Common Principles
symptoms are often linked to spread
symptoms arise from immune response
PAMP + PRR = cytokine release = more symptoms and inflammation
evolutionarily successful viruses are often not very pathogenic
Influenza
Symptoms: fever, runny nose, sore throat, muscle, pain, headache, coughing, and fatigue
Number of strains: 4
Four types: A, B, C, & D
Influenza A and B viruses cause seasonal epidemics of disease in humans almost every winter in the US (CDC, 2024)
Influenza A viruses are divided into subtypes based on two proteins on the surface: hemagglutinin (H) and neuraminidase (N)
There are 18 different hemagglutinin subtypes are 11 different neuaminidase subtypes ( H1 through H18 and N1 through N11, respectively)
So flue A = 130 different combinations in nature
But through reassotrment…many more!
Reassortment
process by which influenza viruses swap gene segments
Reassortment can occur when two influenza viruses infect a host at the same time and swap genetic information
Pigs and birds - flu is not attaching onto respiratory cells
Koch’s Postulates and Viruses (3/6) - Wk 5
Common Principles
Symptoms are often linked to spread
Symptoms arise from immune response
Evolutionarily successful viruses are often not very pathogenic
Immune system kills viruses - not very succesful
Vocab
Infectious disease
disease caused by the direct effect of a pathogen
Signs of disease
clinically measurable deviation for normal body functioning
fever, BP, HR
Symptoms of disease
things that are felt or experiences by a pt
nausea, pain
Koch’s Postulates
How do you know a disease is infectious?
Rhinovirus: caused by weather? or caused by pathogen?
Koch’s Postulates
The suspected pathogen must be found in every case of disease and not found in healthy individuals
The suspected pathogen can be isolated and grown in pure culture
A healthy test subject infected with the suspected pathogen must develop must develop the same signs and symptoms of disease as seen in postulate 1
The pathogen must be re-isolated from the new host and must be identical to the pathogen from postulate 2
Developed by Robert Koch, 1884 - before viruses were identified
Koch’s Postulates Updates
Some pathogens cause disease in some subjects but not others
this means that u can find a causative agent in some healthy subjects
Natural genetic and physiological variation in the host population
Some pathogens are not microorganisms that can be grown in pure culture
Bacteria can grow on their own
viruses need host cells!
Could we research a respiratory disease like rhinovirus following Koch’s postulates?
No - not bc to inject a healthy subject, not able to isolate the virus
ethical issues - informed consent
Pathogenicity and Virulence
Pathogenicity
The ability of a microbial agent to cause disease
Virulence
the degree to which a microbial agent is pathogenic
how weak or strong
How much of a viral pathogen does it take to cause a disease in host?
It varies
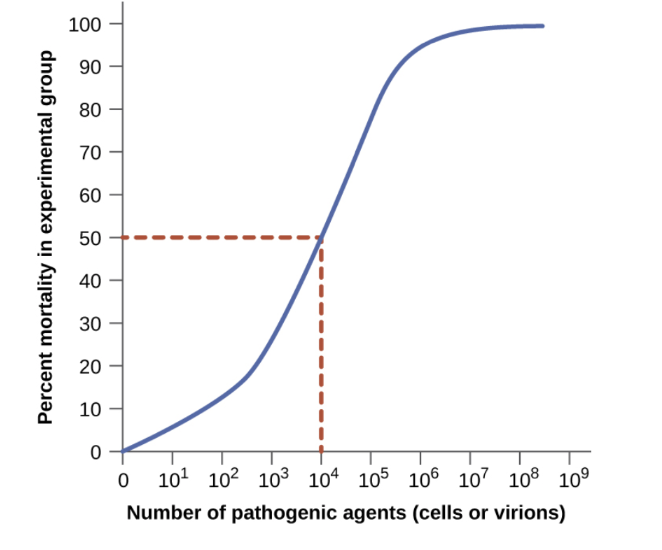
Infectious and lethal dose
A single virion of most types of viruses is likely to cause disease
It could fail to find a cell to infect before falling apart
It could infect a single cell and the innate immune response shuts down replication before an infection can be established
ID50 (infectious dose) - number of virions that will cause disease in 50% of subjects
LD50 (lethal dose) - the number of virions that will cause lethal disease in 50% of subjects
BE ABLE TO UNDERSTAND GRAPH
X axis - ID
Y axis - LD
Primary and Opportunistic Pathogens
Multiple pathogen exposures can occur in one host individual simultaneously or concurrently
Primary Pathogen - microorganism that initially causes disease
Opportunistic Pathogen - microorganism that takes advantage of the opportunity presented by the first infection to also establish an infection and cause disease
Other viruses can hop on as well
Bacteria can hop on as well - even from own body
Bacterial Co-Infections with Respiratory Viruses
Study that shows bactieral coinfection with influenza
Neurovirulence: West Nile Virus (3/10) - Wk 6
West Nile Virus
An enveloped virus with an icosahedral capsid
ssRNA (+) sense genome
Member of the genus Flavivirus
other viruses in this genus - dengue virus, yellow fever virus, & Zika
West Nile Viruses causes West Nile Fever in ~20% of infected humans
WNV causes West Nile Encephalitis or other neurological disease in ~1% of people with West Nile Fever
WNV is an Arbovirus
Arbovirus is not part of the formal order/family/genus classification
Arbovirus - ARthropod BOrn Virus
Disease Vectors
Vectored Diseases do not spread directly from a host of a certain species to another host of that same species
Vectored diseases spread using some sort of vector
Insects are common vectors
Rodents (not arbovirus vectors)
WNV Transmission Cycle
Mammals are ‘dead end’ hosts for WNV
Titers of virus in the blood are too low in mammals to spread the virus back to mosquitoes
Birds are the amplifier host - natural transmission regularly occurs btw birds and mosquitoes
ramps up viral load - makes lots of virus
birds can spread to other birds
The Central Nervous System
Brain & Spinal Cord
Meninges - membranes surrounding brain
Meningitis - inflammation of the meninges
Meningitis symptoms
severe headache
stiff neck
fever
convulsions
confusion
Encephalitis - inflammation of the brain tissue
Meningitis symptoms plus
Lethargy
Seizures
Personality changes
Blood Brain Barrier - specialized endothelial barrier that makes crossing into the central nervous system very difficult
Peripheral Nervous System
Nerves outside the brain and spinal cord
the PNS is less well protected from viruses than in the CNS
due to lack of barrier protection
Neurovirulence
The degree to which it is able to cause a disease in the nervous system of its host
Usually linked to neuroinvasiveness - the ability of a pathogen to enter the nervous system
Neuroinvasion leads to inflammation within the CNS - the cause of many of the symptoms of meningitis and encephalitis
Leads to damage of the CNS is a common feature of zoonotic viruses for which humans are not primary host
The CNS is not a great site from which to spread
Viruses that are better adapted to spread from human to human usually stay put of the CNS
WNV Dissemination
Dissemination - moving from the original site of infection (the skin where you get bit by a mosquito) to the rest of the body
Innate Immune Cells (DCs) at the site of infection become infected by WNV
DCs travel to lymph nodes (immune organs)
Also Provdies a new place for the virus to replicate
From lymph nodes spreads to another immune system organ - the spleen
critical step
lymph and blood gets filtered to the spleen
High levels of viral replication in immune organs leads to virus titers rising in blood
Virus in blood allows for neuroinvasive strains of WNV to cross the BBB
How does it get across the BBB?
“Trojan Horse” - an immune cell is allowed to cross the BBB - WNV rides along inside - hides with DCs
Inflammatory cytokines disrupt the BBB, allowing WNV through
The virus infects the endothelial cells that line the BBB and then get out the other (brain) side
Once inside, WNV can infect astrocytes (a non-neuronal brain cell) and neurons, leading to symptoms of neuroinvasive disease
Rabies virus
Rabies virus primarily enter the CNS by traveling from the site of infection to the CNS using neurons
A majority of rabies virus infections lead to neuroinvasive
Arbovirus
neuroinvasive abroviruses largely enter the CNS by crossing the BBB
A small majority of arbovirus infections lead to neuroinvasive disease
Neurovirulent Viruses: Rabies, Herpes, Polio WNV - Wk 6
Rabies Virus (RABV)
Enters mammals through saliva/mucous membranes → peripheral nerve → spinal cord → brain
Rabies enters a neuron in the PNS by binding to a nerve growth factor receptor called p75, responsible for health neurons
RABV is transported faster than NGF suggesting that RABV not only hijacks the transport machinery but can also manipulate it, gettin git into the neuron fast
Once inside cell body neuron → directly path to the brain
Slow, progressive zoonotic disease characterized by fatal encephalitis. Once symptoms appear, almost always fatal
Two forms
Furious Rabies
agitation, disorientation, seizures, twitching
hydrophobia
Dumb rabies
pt paralyzed, disoriented, stuporous
Both progress to coma phase → lead to respiratory arrest
Rabies Transmission
Reservoirs: wild mammals such as canine, skunks, raccoons, badgers, porcupines cats, & bats
Spread through bites and scratches, & inhalation of droplets
Estimated 35,000 to 50,000 human cases
US: 6k to 7k animal cases per year
2004: transmission of rabies through donated organs tissues
Transmission through cornea implants
Herpes (HSV) Encephalitis
high restricted from CHNS (HSV-1 oral, HSV-2 genital)
primarily causes by HSV-1
Can be neonates-transferred through HSV+ mother
Can be treated with antiviral if caught early…BUT
within days: massive necrotic destruction of brain tissue, coma, & death
You don’t have to have an outbreak before you get encephalitis
HSV
Herpes simplex types I and II can cause encephalitis in newborns of HSV positive mothers
Virus is disseminated and progress is poor
Older children and adults over 50 are also susceptible
Caused most commonly by HSV 1
Represents a reactivation of dormant HSC form the trigemminal ganglion
HSV 1 most common cause of encephalitis
Neurovirulent Viruses
Viruses that cause viral meningitis
Many viruses that do not normally cause neurovirulence can in rare cases cause viral meningitis
Echo and coxsachieviruses, herpesviruses, measles viruses, influenza, mumps, etc.
They most frequently occurs in immunocompromized individuals or very young infants
Polio
Causes poliomyelitis in small subset of infections
acute flaccid paralysis - affects PNS
fecal to oral & repiratoy
dangerous respiratory paralysis
spread as a fecal oral pathogen
(+)ssRNA, naked virus
MWMR Discussion
Group One
2813 cases total in 2018
caused by mosquitoes and ticks → other hosts → humans
mainly WNV, La Crosse, Jamestown, Powassan, EastEequineEnceph
Classified by sex, age, symptoms
Group Two
WNV first reported in 2018
Clinical Syndromes: meningitis, encephalitis, acute flaccid paralysis
Powassan in Indiana: Likely caused by a blood transfusion from a donor in Wisconson
Group Three
Limitations: Doesn’t require info abt clinical signs and symptoms, most are underreported
Information campaign abt household habits/community effors - get rid of standing water, control mosquitoes, considering arboviruses then properly reporting
Neurovirulence: TBEV (test heavy material) - Wk 6
Paper Discussion
Tick Bonre Encephalitis Virus (TBEV)
Member of Flavivirdae
Arbovirus vectored by ticks
TBEV causes Tick-Borne Encephalitis (TBE)
Generally two phases of disease
Phase I: Generic viral illness, no CNS involvement (most infections resolve here)
Phase II: CNS involvement
meningitis
encephalitis
Focus Forming Units (FFU) - measure of how many infectious virus particles are in solution
Named for a variation on a plaque assay
Plaque Assays - experiments used to determine how many virus particles are in solution - BE ABLE TO EXPLAIN ON EXAM
Dilute the viruses until there are a countable number/unit of volume
Why dilute?: So that the amount of virus particles is measurable
Add that unit of volume to a petri dish that is 100% filled with a flat layer of cells that the virus can infect
After giving the virus enough time to perform several rounds of replication, look for ‘holes’ in the layer of cells
Each hole (plaque) = where one virus started an infection
Focus Forming Assays - Plaque assays for viruses that don’t lyse their host cells - therefore going through budding
First steps are identical, but instead of looking for holes, rely on detection of a ‘foci’ of viruses with an antibody
Gene Expression Analysis
Not all genes in host cells are transcribed all the time
Certain genes only get turned on when needed for an immune response
How can you measure the expression of a gene?
Measure the amount of RNA transcript in a cell
How do you measure the amount of RNA transcript in a cell?
qRT-PCR
mRNA → complementary DNA (cDNA) → quantitative PCR (qPCR)
Kurhade ET Al
Figure 1
B & C: More RNA expression in Toro → more viral load
You use spleen & lymph nodes bc of their filtration & greater immune response - you would see the viral load bc of the filtration presence
D,E,F,G,H,I - measuring cytokine response
D: GAPDH (spleen) - expressed more in spleen
E: IL6 - Toro spikes at day 9
F: CXCL10
G: TNFalpha (lymph node) - expressed more in the lymph nodes
H: IL6 - Toro spikes at day 9
I: CXCL10
Cytokine storm
Figure 2
HB171/11 not present until 10 day
Toro present until around day 5
Concept Map
Hemorrhagic Fever Viruses (3/17) - Wk 7
Zoonotic Infections
Zoonotic infections - caused by a pathogen that has ‘jumped” from one species to another
Distinct from vectored infection
vectored infection - natural transmission cycle includes back ad forth btw two or more host species
Vectored infections are a type of Zoonotic infection - many Zoonotic infections are not vectored
Viruses with a long evolutionary history with a host species tend to be more benign
natural selection tends to favor lower virulence and higher contagiousness
the replication cycle - do not want to kill the host
More severe viral diseases in humans tend to be recently ‘jumped” zoonoses
Recent: Last 20-30 years
HIV
SARS/SARS-CoV-2Ebola
Pandemic potential
Epidemic but world-wide
host plasticity - ability to infect more than one species
rodents, monkey, bats
human-to-human
geographic distribution
Reservoir - host species that is maintaining a pathogen pool
Spillover - infection event where a pathogen that has historically circulated in one species infects a different host species
What kinds of animals spark zoonotic events?
Zoonotic Infections + Bats
Viral richness - number of viral species in a particular host (one individual organism)
Proportion of zoonotic viruses
how many of those viruses have been seen before in human
Bats, primates, and rodents - host a lot of zoonotic viral pathogens
a virus that has been found at least once in humans and once in another species
Bats, primates, & rodents - also host a lot of viruses
Many viral hemorrhagic fevers are caused by zoonotic viruses
Ebola
Hanta
Lassavirus
Rift Valley Fever Virus
Viral Hemorrhagic Fevers
Viral hemorrhagic fecers
severe multisystem syndrome
vascular system extensively damaged
symptoms usually accompanied by hemorrhage (bleeding)
Viral Causes of Hemorrhagic Fevers
all enveloped RNA viruses
All zoonotic infections
Families
Arenavirdae
Bunyavirdae
Filoviridae
Falviviridae
Ebola Virus
Ebola virus
causes a viral hemorrhagic fever
transmission human to human relies on direct contanct with bodily fluids
untreated mortality rate 50%-90%
Ebolavirus is a genus
Zaire ebolavirus is the species that most commonly causes ebola virus disease
member of the family filoviridae
Pathogenesis of Ebolavirus
Entry into the host depends on direct contact of infected bodily fluids with mucosal surface
At those mucosal surfaces Ebolaviruses encounter many potential host cells
resident macrophages and DCs
cells that make up the mucosal tissue
Key to pathogenesis
very broad cell/tissue tropism
attachment and entry depend on Ebolavirus Glycoprotein (GP)
Attachment and entry
Does not rely on a specific host cell receptor
Relies on non-specific host cell surface molecules that interact with phosphatidylerine and glycoproteins - non specifc cell surface markers
Ebola v. SARS-CoV
Ebola infects more cells
Find only SARS-CoV in like respiratory cells
Ebola disables and dysregulates many of the early innate immune mechanisms a host uses in attempt to halt infection
Blocks production of interferons, which are involved in preventing local spread of viral infections
causes ‘cytokine storm’
Cytokine storm
what is a cytokine?
soluble proteins that act as communication signals btw cells
autocrine - act on same cell
paracrine - act on a nearby cell
endocrine - travel through bloodstream to act on remote cell
Important cytokines
Interleukines (IL-x)
Chemokines
Interferons
Cytokine storm - caused by uncontrolled release of excess cytokines
Cytokines ideally should result in targeted, lack immune response leading to pathogen clearance
Cytokine storms lead to systemic inflammatory response
immune response attacks organs can lead to multi organ failure, extremely high fever
What causes hemorrhagic part?
Exact pathogenesis unknown
drop in platelets, clotting factors have been observed
injury of endothelial cells that line blood vessels by viral replication is implicated
not all pts develop the hemorrhage, can be fatal w/o it
Viral replication in multi organ systems
liver (important in production of clotting factors)
spleen
Ebolavirus Outbreak
2014-2016
west Africa started in guinea in late 2013
Ebolavirus (3/18) - Wk 7
Ebolavirus Outbreak of 2014-2016
West Africa Ebolavirus outbreak started in Guinea in late 2013
Likely started with spillover event form bats
Total outbreak numbers
28,600 cases
11,000 deaths
What ended it?
Public Health Measures
Vaccine Development
December 2013
18 month old boy died from EbolaVirus Disease in rural Guinea
Likely contracted by a bat
March 2014
Ebolavirus identified in the capital of Guinea, Conakry
Outbreak declared by WHO with 49 cases and 29 deaths
AUgust 2014
Ebolavirus is spreading exponentially in capital cities of Guinea, Sierra, Leona, and Liberia
During 2014-2016 there were 11 cases in the US
Using Genome Mutations to Track Viral Spread
During infection of a single pt, an Ebolavirus will replicate millions of times
this is an opportunity for the accumulation of genetic mutations in the viral genome
Hemorrhagic Viruses - Marburg & Hanta - (3/24) Wk 8
Marburg Virus Disease (MVD)
Cousin of Ebola, Filovirdae family
MVD is severe, often fatal in humans
The average MVD case fatality rate is around 50%. Case fatality rates have vareid from 24% to 88% in past outbreaks
MVD initially detected in 1967 after two simultaneous outbreaks in marburg and Frankfurt in Germany, & in Belgrade, Serbia
Traced to lab work using African Green monkeys imported from Uganda
initial outbreak in labs where sera and vaccines were being made
initial patients had direct contact with blood, organs, and cell cultures of African green monkeys
Monkeys imported from Uganda were used for producing kidney cell cultures, critical for culturing polio vaccine
Latest out break in 2024
Natural host fruit bats
MVD Symptoms
Fever, chills, headache muscle aches
rash with both flat and raised bumps, often on torso
chest pain, sore throat
nausea, vomiting, & diarrhea
as the disease advances, symptoms can become more severe, including liver failure, delirium, shock, bleeding, & multi organ failure
Recent Outbreaks
‘22 - Guinea
‘22 - Ghana
‘23 - Guinea
‘23 - Tanzania
‘24 - Rwanda
Diagnosing
Can be difficult to diagnose
Confirmations that symptoms are caused by Marbug virus infection are made using the following methods
ELISA or PCR
Treatment
Rehydration
no vaccines or antivirals that are approved
monoclonal antibody and antivirals
Hanta Virus
Causes hantavirus pulmonary syndrome (HPS) and hemorrhagic fever with renal syndrome (HFRS)
Transmitted via rodents, not person-to-person
(-)ssRNA virus
How Does it Spread?
Virus is present in the rodent’s urine, feces, or saliva
Inhaling viruses - the most likely form of transmission - when they become airborne from distributed rodent droppings or nesting materials
Touching things contaminated with virus, such as nest, and then touching your mouth, eyes, or nose
Being bitten or scratched by an infected rodent
Viral Replication
Macrophages and vascular endothelial cells, particularly those in the lungs and kidneys, are targeted by Hantavirus
Hantaviruses found in the Western Hemisphere including here in the US, can cause hantavirus pulmonary syndrome (HPS). The most common hantavirus that cause HPS in the US is spread via deer mice.
Symptoms of HPS
Earl phase symptoms (1-8 wks after exposure)
Fever, fatigue
muscle aches
headaches, dizziness, chills
abdominal problems, like nausea, vomiting, diarrhea, and abdominal pain
Late Phase symptoms (4-10 days have early phase)
coughing shortness of breathe
tightness in chest w/ fluid in lungs
HFRS Symptoms
Hemorrhagic fever w/ renal syndrome (HFRS) - mostly in Europe & Asia
Seoul Virus, a type of hantavirus that causes HFRS, is found worldwide, including US
1-2 wks after exposure
acute shcok
intense headaches
fever/chills
blurred vision
low BP
lack of blood flowinternal bleeding (acute shock)
acute kidney failure
Treatment
supportive care, rest, hydration, treatment
pts with HFRS may need dialysis
survival rate depends on the strain of the virus, but is relatively good
using small interfering RNA (siRNA) and other immune based therapies to target specific gene segments
drugs have shown efficacy in increasing survival rates during early stages of infection. Some of these drugs include lactoferrin, ribavirin, ETAR, favipiravir, and vandetanib.
Oncoviruses (3/25) - Wk 8
Intro to Cancer
Cancer - a group of related diseases
Hallmarkscells divide w/o stopping
Cells invade surrounding tissues
Tumor - a growth of cells from inappropriate cell division
Malignancy - the ability to invade other tissues
Why do tumor cells divide without stopping?
Ignore cell death signals
inappropriate expression of telomerase
Broken cell cycle checkpoints
Cause blood vessel growth to feed themselves
evade the immune system
Cell Cycle Review
Phases of the Cell Cycle
Interphase
G1, S, G2
M Phase
mitosis
cytokinesis
Checkpoint Control of Cell Cycle
Origin of Cancer
Often, genetic changes
errors during DNA replication
Environmental exposures
chemicals (tobacco smoke)
Radiation (sun exposure)
Important Types of Genes in Cancer
Proto-oncogenes
products are normally involved in cell growth and division
mutations that increase activity can lead to cancer
Tumor Suppressor genes
products negatively regulate cell growth and division
mutations that decrease activity can lead to cancer
DNA repair genes
products involved in repairing damaged or mutated DNA
mutations that decrease activity can lead to failure to fix proto-oncogene or tumor suppressor gene mutations
Oncogenic Viruses
7 known viruses that cause cancer in human cells
HPV, EBV, Kaposi’s associated Herpesvirus, Hep B, Hep C, Human Adult T cell leukemia virus, Merkel Cell
Discovered 1960s (EBV) - 2008 (MCV)
Observations
very prevalent
about 90% of humans have EBV
In the US, ~1200 people/year are diagnosed with Burkitt’s lymphoma
Discovery path
Study cancer → find virus
Viruses & Cancer
What potential mechanisms can you image for viral oncogenesis
integration into host genome causing damage
viral proteins interfere with host cell cycle regulations
Human Papilomavirus
Member of the Papillomavirdae family
dsDNA genome
Non-enveloped
Causes warts
some types cause sexually transmitted cancers, particularly cervical cancer
Enters a cervical cell through endosomal entry
uncoats through pH dependent mechanism
Trafficked to the trans-golgi (the outgoing side)
ability to incorporate itself with the proteins
How does it cause cancer from here?
When the nuclear membrane dissolved during mitosis, HPV is trafficked to the host chromosomes
In daughter cells of the initially infected cell, HPV is in the nucleus
Steps to carcinogenesis:
integration of viral genome into host genome
‘Normal” HPV is maintained as an episome
small piece of viral dna is incorporated into host cell dna
sometimes it is integrated
integration of viral genome into host genome
integration changes viral gene expression patterns, leads to increased expression of two viral oncogenes: E6 & E7
Viral oncogenes: genes whose products promote cancer formation
p53 - tumor suppressor gene “guardian of the genome”
mutated in >50% of human cancers
transcription factor that changes transcriptional profile of the cell activated
activates DNA repair proteins
arrests cell growth at the G1/S checkpoint
intimates programmed cell death when needed
responds to short telomeres
E6 from HPV causes p53 to be ubiquitanated and degraded by the proteasome
ubiquitin is a small regulatory protein found in most tissues of eukaryotic organisms
ubiquitination affects proteins in many ways: it can mark them for degradation via the proteasome
proteasome are part of a major mechanism by which cells regulate the concentration of particular proteins and degrade misfolded proteins
Cancerous cells: no longer are the right type
become invasive
Pap Smear
pap smears - tests that examine cervical samples for cancerous for pre-cancerous cells
Oncogenesis Themes
access to the nucleus
integration of viral genome into host genome
long periods of time
expression of viral oncogenes
Viral Epidemiology: HIV - Wk 9
Epidemiology of Pandemics
HIV/AIDS pandemic: 1981 - present
1918 Influenza Pandemic: 1918-1919
COVID-19 pandemic: 2019-2023
Epidemiology - study of how disease originates and spreads throughout a population
Epidemiology encompass:
geographic distribution + timing of a disease
the etiology (cause) of a disease
the transmission of a disease
Endemic disease - constantly present in a particular region
HPV - Human Papillomavirus
Epidemic: much larger than expected number of cases occur in short period of time in a particular reason
Annual Influenza Epidemics
Outbreak: epidemic in a very limited geographic area
current cluster of Ebolavirus disease cases in Guineea: declared Feb. 14 2021 by WHO
Pandemic: Worldwide epidemic
COVID 19
Pathogenesis of HIV
Stage 1: Acute HIV Infection
Direct contact with bodily fluids introduces HIV to a new human host
1-2 week “flu-like” illness
Resolves on its own
Stage 2: Clinical (Classical) Latency
Virus is not completely latent, but no clinical signs of infections
usually lasts 2-15 years
Stage 3: AIDS - Acquired Immunodeficiency Syndrome
Opportunistic Infections
Rare Cancers
Kaposi’s Sarcoma
Leads to skin lesions
Wasting Syndrome
Survival of ~3 years w/o treatment
HIV exhibits cell tropism for CD4+ T cells
CD4+ T Cells
Part of the adaptive immune system'
interact with DCs carrying an antigen from an infected site in the body
Become a “Helper” T cell that coordinates the rest of the adaptive immune response
Succesful antiviral drugs for HIV have been developed
HIV+ people can live full lives and expect to never progress to AIDS
Vocabulary of Epidemiology
Morbidity - the state of being diseased
Prevalence - number of diseased individuals within a population at a point of time
Incidence - number of new cases within a population over a period of time
How do Epidemiologists Do Their Work?
Tracking source of illness
determining etiology
John Snow - 1813-1858
British physician
Investigated 1854 cholera outbreak in London
Common source spread - a single source for all infected individuals
Propagated spread - through person to person contact
Tracking causes of mortality
Florence Nightingale (1820-1910)
English Nurse and statistician
Mapped causes of death in 1854 Crimean War
Types of Modern epidemiological studies
Observational
No manipulation by researcher
measure associations
gather data
Descriptive epidemiology - gathers info abt an outbreak
Analytical Epidemiology - attempts to test hypotheses abt cause
Analytical Studies can be:
retrospective: gather past info abt present cases
Prospective: follow individuals over course of a study
Analytical studies can use:
Cohort method: group of individuals with a shared characteristic compared to some other group
Case Control Study Method: retrospective studies compare group of subjects with disease to matches ‘control’ group w/o the disease
Cross Sectional Method - randomly select individuals in a population and compare affected to unaffected individuals
Viral Epidemiology: 1918 Influenza (4/14) - Wk 10
Viral Life Cycle: Ex. Influenza Virus
Flu is a respiratory virus
Fever
Runny nose
sore throat
aches/fatigue
cough
Caused by influenza virus
enveloped virus with (-) ssRNA, segmented genome
Attachment → penetration (endocytosis) → uncoating → replication → assembly → release
Assembly of particles with segmented genome is more complicated
influenza virus: example of concerted assembly - everything comes together at once to make a viral particle
Pathogenesis of Influenza
Influenza exhibits cell tropism for cells that have Sialic Acid on their surface - including respiratory epithelial cells
infections begin through inhalation of droplets carrying infectious virus or contact with contaminated surfaces
Influenza causes destruction of lung epithelium
Influenza infectious causes immune response symptoms that are both systemic
fever/chills
aches
fatigue
and local…
coughing
sore throat
congestion
Epidemiology of Influenza
Influenza causes destruction of lung epithelial cells
difficulty breathing
open door for opportunistic infections
severe cases lead to pneumonia (inflamed air sacs, often includes fluid in lungs)
Influenza is a seasonal illness
reasons??
humidity
% of all deaths in the US due to influenza and pneumonia
Why do people still get the flu w/ vaccines
different strains
Influenza: Zoonotic Infections and Reassortment
Birds are a natural reservoir for influenza viruses
Potential for zoonoses, and can cause disease in birds
Ongoing highly pathogenic avian influenza outbreak 2022-2023
Reassortment
Two different influenza viruses infect one cell
during virion assembly, a mix of genome segments from both viruses go into one capsid
Influenza
HxNx Nomenclature
H = hemagglutinin
N = neuraminidase
Viral proteins found in envelope
important antigens
important to entry and infectivity of virus
HxNx Nomenclature
18 different known H versions and 11 known N versions
Reassortment can give rise to influenza epidemics or pandemics
Attachment and Entry
Hemagglutinin binds to sialic acid
neuaminidase cleaves silaic acid on the way out to allow exit
Viral Epidemiology: 1918 Influenza (4/17) - WK 10
Influenza Pandemic
Worldwide 1918-1918
1/3 world population infected
aprox. 10% mortality rate
Caused H1N1 virus of avian origin
unusual mortality characteristics - most deadly for 20-40 y/o
normal flu follow hourglass shape
1918 flu was the inverse
Native American Boarding Schools
schools often over crowded
attendance was compulsory 1891-1978
1820s-1980 Government funded schools for native American children
Understanding the Virology
How did it end?
decedent circulated un humans until 19509
genetic adaptations reducded virulence
the virus developed a more typical epidemic mortality curve
Story of reconstruction
Part One
Brevig Misson
Native American site
Dr. Johan Hultin
in charge of misson
Lucy
native american woman who was preserved in permafrost which lung tissue was taken from
Taubenberger et al.
article that inspirers group to go back
first sequence of 1918 flu
Part Two
HA Gene
H entry piece
Antigenic drift
changes in surface proteins
Why 1918 flu different from other strains
didn’t have cleavage site mutation
activate w/o trypsin
Dr. Peter Palese
created plasmid to recreate 1918 flu
created first genetic map
Part Three
Dr. Terrance Tumpey
in charge of reconstructing the 1918 flu
ended up reconstructing the virus
BSL Level?
biosecurity lvl 3
PAPR, scrubs, shower, gloves, shoe covers
Requirements/rules for reconstruction
one person to be granted access, lab access, and to reconstructed
required to take prescribed medicine
work mostly nights with no one else in building
Effects in mice
highly lethal in mice
100x more lethal than recombinant viruses tested
spread to vital organs - brain, liver, heart, spleen
fluid filled lungs - serious pneumonia
Part Four
What is different today
have had pandemics today
there is a flu vaccine now
What is 1918 flu occurred now?
not as severe affect now
Tumpey et. al
Table 1
1918 (2) takes a lot less to infect w/ and w/o trypsin
Table 2
infecting eggs with LD and ID
1918 had more of a death rate
Fig. 1
A: leathlity
B: % survival tanked after day 4
Fig. 3
how soon virus is released
Viral Epidemiology: COVID-19 pt. 1 (4/21) - Wk 11
Coronavirdae
First CoV identified - in chickens, 1937s
Pig CoV - millions of piglets died, 2014
Feline, Canine CoVs - disease in domestic cats, dogs
First human CoV cultured in 1960s from nasal cavities of people with common colds
Categorized by 4 Greek letters: alpha, beta, delta, gamma
Affects host immune responses, antagonistic for interferons
Enveloped
RNA recombination frequency in highest known of any RNA virus
The cause of 15-25% of common colds
Spreads like the flu and during cold/flu
SARS
emerged in the human population in China 2002
the virus most likely jumped form bats into Himalayan palm civets and then into humans
Human to human transmission was by respiratory and fecal routes
8000 cases were reported worldwide, 26 countries
774 deaths occurred (~10% case mortality rate)
Economic losses in Hong Kong were ~5.9 billion
In July 2003, WHO reported that the last known human chain of transmission was broken
Bats and birds are natural reservoirs of SARS-like viruses
Laboratory-associated infections occurred in China
MERS
MERS begins with coughing, fever, and breathing problems but may progress to pneumonia and kidney failure
over 1600 human cases and the outbreak is ongoing
Case fatality >30%
sporadic, cant be linked to a single source
countries most affected in Arabain peninsula
most person-person transmission occurs in hospital setting
many questions about the virus unanswered
healthy camels have antibodies against
COVID-19 Pandemic
first observations of COVID-19
Cluster of pneumonia cases of unknown etiology in Wuhan China in Dec. 2019
Epidemiological work identified Huanan Market as possible source of contagion
Later work suggests spread was already propagating at that point
Global Public Health
WHO - World Health Organization
Agency of the UN
3.4 billion annual budget proposed for 2024
For reference: The US annual spending for 2022 was 6.27 Trillion
WHO
monitors and reports diseases
coordinates international responses during epidemics/pandemics
Designs and executes campaigns to reduce disease burdens globally
smallpox vaccination
other infectious disease control
CDC - Centers for Disease Control and Prevention
part of the US department of Health and Human Services
formed in 1946
national public health agency
Viral epidemiology: COVID-19 pandemic pt. 2 - WK 11
COVID-19 Pathogenesis and Long COVID
When an individual is exposed to SARS-CoV-2
the virus usually first infects cells in the nasopharynx, trachea, or nasal olfactory mucosa
some infections are cleared by the immune system
the virus then can move lower the respiratory tract
these infections can then develop into more critical cases
inflammation in the alveoli due to the viral replication and consequent immune responses can lead to dyspnea
SOB due to poor gas exchange in the alveoli due to inflammation and fluid (pneumonia)
leads to hypoxia
progressive respiratory failure from this point ca nlead to the development of ARDS
ARDS
inflammation in lungs
widespread lung damage
pulmonary vascular leakage
Early control of SARS-CoV-2 by the immune system is critical to prevent later inflammatory mediated disease
Post acute sequelae
Myalgic encephalomyelitis/chronic fatigue syndrome
Long term illness
fatigue not improved with rest
sleep issues
brain fog/dizziness
COVID Pt. III (4/24) - WK 11
Hypothesis One
Direct zoonosis/natural transmission
SARS-CoV-2 evolves from a bat coronavirus
human contact with bats
immediate animal contact with bats then contact with humans
‘Lab Leak’
centers around work at Wuhan Institute of Virology
Does not imply engineering of virus
Engineered Virus
could you ever definitely prove a virus wasn’t engineered by humans
Scientific process
always open to change with new evidence
extraordinary claims require extraordinary evidence
Pandemic
virologists tend to favor the direct zoonosis hypothesis
Podcast evidence for zoonotic hypothesis
came from seafood market
studies are preliminary
photographic evidence
raccoon dogs and flying foxes
can easily spread possible virus
near stall where scientists find SARS-CoV-2
found the virus on lots of surfaces - food machines, cages, etc.
shows that virus jumped from animal to animal
not evolved from human
genetics showed two diff. variants, which are not found in humans
Evolution
Variant
mutations in the genome
variants of concern
characteristics that put public health at risk
alpha, beta, gamma, delta, ommicron
alpha, beta, gamma dominate population
delta and omicron
omicron is now dominant concern
argues that omicron should be strain and not a variant
delta displayed increased disease severity
omicron less disease severity but most dominant globally
transmission increased and increased immune invasiveness
Vaccines & Antivirals: Intro to Vaccination (4/28) - WK 12
Vaccines + Adaptive Immunity
Vaccination relies on the adaptive immune system
Two crucial components of adaptive immunity
specificity
memory
Primary Immune Response is critical in generating memory
Initial exposure → primary immune response → secondary exposure → secondary immune response
During the primary immune response, some immune cells are programmed to remember a specific antigen
These cells differentiate into memory
Adaptive Immunity
Two crucial cell types for adaptive immunity
T cells
mature in the thymus
B cells
mature in the bone marrow
T and B cells are generated by hematopoiesis from the same stem cells that innate immune cells are derived from
T cells - responsible for cellular immunity
T cells direct T cells and other immune cells to target and kill specific pathogens or pathogen infected cells
B cells - responsible for humoral immunity
Humors - bodily fluids
Humoral immunity - mediated by macromolecules found in bodily fluids
mostly antibodies
B cells - make and secrete antibodies
Adaptive Immunity and Vaccines
Both cellular and humoral immunity are important in their function of vaccines
Adaptive Immunity
Where does specificity come from?
Antigens -
name originally comes from antibody generating molecules
also stimulates cellular immunity
proteins are the best antigens
Epitopes
small exposed regions on surface of antigens that T cell/B cell receptors or antibodies interact with
Antibody Structure
Antibodies - glycoproteins produced and secreted by B cells
Structure is critical to function and specificity
Fab (variable) and Fc (constant)
Five classes of antibodies are made by human B cells
Each has a heavy chain with a unique purpose
each has distinct purpose
IgG is the most abundant and ‘multifunctional’ antibody
Antibody Function
neutralization - antibodies bind to antigens on target viruses, preventing cellular attachment and entry
Opsonization- antibodies bind to pathogens
The opposite end of the antibody binds to receptors on phagocytic innate immune cells, like macrophages, enhancing phagocytosis
Adaptive Immunity and Vaccines
Immunity - the ability to resist infection with or pathogenesis of a pathogen
generally relies on adaptive immunity
Immune memory can be acquired through the active function of the adaptive immune system
Option 1: Become ill with a pathogen, recover
Option 2: Introduce the adaptive immune system to relevant antigens in a lower risk setting (w/o giving the infectious pathogen)
Natural
active: immunity from sickness
passive: breastmilk
Artificial
active: vaccination
passive: serum transfusion
Natural acquired immunity
requires natural infection with the pathogen against which you build a memory response
Ex: Smallpox
Viral Illness
eradicated in the 1970s
20-30% mortality rate
Smallpox
first infection with smallpox has 20-30% mortality rate!
but if you survive, you are protected
Goal of vaccination - induce immune memory more rapidly and with less harm than natural infection
Intro to Vaccines
Option One: Take virus or pieces of virus that cause an immune response but not enough to cause disease
Option Two: engineered vaccine designed to raise immunity by mimicking a piece of virus
Vaccine Types to Focus On
Live attenuated vaccines
Inactivated
Subunit Vaccines
purified from original virus
engineered into viral vector
ex: tetanus
Nuclei Acid Vaccines
How Do Vaccines Get Approved?
Three phases of clinical trails in people occur after tesing has occured in animal models
phase i: small group of participants, testing safety (maybe ~45)
phase ii: larger group of participants, testing safety and some immune response parameters (~600)
phase iii: largest group, safety and efficacy (30,000-40,000)
Smallpox & History of Vaccine (4/29) - WK 12
Smallpox vaccination
smallpox is a disease caused by Variola virus
Variolation
procedure developed by empirical methods
inoculation of healthy individual with a scab from a recently recovered smallpox individual
mortality rate of 2%
As compared to 20-30%
Edward Jenner in 1796 noted that milkmaids who recovered from cowpox rarely got smallpox
developed an injection from a cowpox sore and gave it to a young boy
exposed the child to variola virus and never developed smallpox
1801 published his work
Modern smallpox vaccines still consist of a live Vaccinia virus
no longer produced by isolation from a sore on a milkmaids hand
What Is In a Vaccine?
Whole viral particles, pieces of a virus, or nucleic acid from virus
Adjuvant - enhances the reaction of the immune system
can cause allergic reactions
ex: formaldehyde (polio, diptheria), aluminum (DTAP, HPV, Hep B, pneumo), albumin (flu), and squalene (flu)
Antibiotics
certain antibiotics may be used in some vaccine production to help prevent bacterial contamination during manufacturing
neomycin, polymyxin B, streptomycin, and gentamicin
Vaccine Clinical Trials (5/1) - WK 12
Development of COVID Vaccines
Vaccine development was a critical part of the public health response to the COVID-19 pandemic
First shots went into arms in clinical trials in the US on March 16, 2020
Operation Warp Speed was announced on May 15, 2020
$10 billion dollars in government funding to a public-private patnership to advance COVID-19 vaccine development
Up to $1 Billion dollars by Oct. 2020
Funded development of 6 different COVID vaccines by private companies
COVID MRNA Vaccines
mRNA vaccines: mRNA delivered directly to human cells
This is the technology used by Moderna and Pfizer vaccines
Clinical Trial Process
IND Application - Investigational New Drug
Phase I - small number of patients, monitors safety
Phase II - are responses as expected? Larger group of pts, monitors safety
Phase III - Will treatment produce desirable outcome, while monitoring safety
marketing application submitted & FDA makes final decision
Standard time: 8-15 years from IND submission
Fast Track: 5 years or less (usually for drugs that treat highly contagious or aggressive diseases)
Antivirals (5/5) - WK 13
Antiviral Drugs
Antibiotics target bacteria
bacteria are cellular life forms with their own replication machinery, enzymes, cellular structure, and ways of harvesting energy, that are potential drug targets
Antivirals
viruses use host cell machinery for almost all functions
this severely limits drugability
Acyclovir
antiviral used for treatment of many kinds of herpes virus infections
genital herpes
chickenpox/shingles
EBV (mono)
inhibits nucleic acid synthesis by herpes virus
Antiviral Drugs
Acyclovir
nucleoside analog - mimics guanosine
specifically for virally infected cells - virus enzymes needed to add phosphate group to acyclovir
when acyclovir is incorporated by a DNA polymerase, elogation terminates
Tamiflu (olsetamivir)
neuraminidase inhibitor
enzymes cleaves sialic acids and helps entry in to cells
Highly Active Antiertroviral Therapy (HAART)
a combination of 3+ antiviral drugs
daily HAART successfully suppresses HIV load and prevents progression to AIDS
HAART
Drug category 1
reverse transcriptase inhibitors
often work by being nucleoside analogs
same mechanism as acyclovir
Drug category 2
fusion inhibitors
stop binding of HIV to cell
Drug category 3
viral protease inhibitors
these are essential for replication
Drug category 4
integrase - viral enzyme responsible for inserting viral genome into host genome
HAART generally consists of a combination of 2 RT inhibitors and at least one other drug
importance of combination therapy - to prevent development of resistant viral variants
preventing replication = preventing mutation & variants
Succesful HAART therapy
represses viral load
prevents transmission
because viral load is low
allows for maintenance of increased CD4
delays/prevents progression to AIDS death
PREP
PrEP - PreExposure Prophylaxis
can you administer antiretroviral drugs prophylactically (a preventative) to individuals at high risk of infection with HIV?
COVID 19 & Antiviral Treatments (5/8) - WK 14
target
inflammation
thrombosis
ARDS
RAAS activation
Antivirals for COVID
Remdesivir
nucleoside core
inhibits RNA replication
stop at RNA replication
Paxlovid
nirmatrelvir boosted with liver modifier drug
Blocks proteolysis
Class Activity
Pt I
paxlovid?
Pt II
paxlovid - bc higher risk
Pt III
paxlovid - for pregnant women
Pt IV
nothing - healthy