Ch6_Circulatory System
Chapter 6: The Circulatory System
Heart Structure: (in my words)
pump that circulates blood throughout the body
located in center of thoracic cavity btw lungs, apex points down and to the left
four chambered, hollow, muscular organ
surrounded by thin fluid filled sac- pericardium
heart walls have 3 layers
heart has two sides- right and left
each side has two chambers- upper and lower
right and left chambers are separated by septa(partition-septum)
Layers:
epicardium: the outermost layer of the heart, providing a protective covering and reducing friction between the heart and surrounding structures.
myocardium: the muscular middle layer responsible for heart contractions
endocardium: the inner lining of the heart that provides a smooth surface for blood flow.
Chambers:
Atria : the two upper chambers of the heart that receive blood from the veins and pump it into the ventricles.
Ventricles: the two lower chambers of the heart that receive blood from the atria and pump it out to the lungs and the rest of the body.
Valves:
atrioventricular
mitral valve- located between the left atrium and left ventricle, it ensures one-way blood flow and prevents backflow during ventricular contraction.
tricuspid valve - located between the right atrium and right ventricle, it ensures that blood flows in one direction and prevents backflow during contraction.
semilunar valves - these include the aortic valve and the pulmonary valve, which control blood flow from the ventricles into the aorta and pulmonary artery, respectively.
Septa:
The septa are muscular walls that separate the left and right sides of the heart, specifically the interatrial septum between the atria and the interventricular septum between the ventricles, ensuring that oxygen-rich and oxygen-poor blood do not mix.
interatrial septum - a thin wall that divides the right and left atria
interventricular septum a thicker wall that separates the right and left ventricles
septum mostly consists of myocardium
Coronary circulation
the flow of blood to and from the tissues of the heart, supplying oxygen and nutrients while removing waste products.
Angina
angina pectoris
chest pain due to reduced blood flow to heart muscle
caused by narrowing, obstruction or spasm of coronary arteries
Atherosclerosis:
buildup of plaque can lead to servere narrowing of coronary arteries which reduces blood flow to heart
this condition is called coronary artery disease
Heart attack:
myocardial ischemia- partial obstruction of the coronary arteries can result in ischemia, where the heart muscle doesn't receive enough oxygen, potentially leading to a heart attack if blood flow is not restored quickly.
myocardial infarction- complete obstruction
Overview of the Circulatory System
Functions of the Circulatory System:
Transports essential substances, including oxygen and nutrients to body cells, thereby facilitating cellular metabolism.
Removes carbon dioxide and other metabolic waste products from cells, helping to maintain homeostasis.
Aids in blood coagulation through the action of platelets and clotting factors, preventing excessive bleeding during injury.
Helps defend the body against disease by transporting white blood cells and antibodies throughout the body.
Assists in body temperature regulation by redistributing blood to the skin and extremities.
Main Components:
Cardiovascular System: Composed of the heart, a complex muscular organ, blood vessels (arteries, veins, and capillaries), and blood, which acts as the transport fluid for nutrients, gases, and wastes.
Lymphatic System: Comprising lymph vessels, lymph nodes, and lymph, it is important for immune responses and maintaining fluid balance in the body.
The Heart
Structure:
The heart is a four-chambered hollow muscular organ, roughly the size of a man’s clenched fist, located in the thoracic cavity between the lungs.
Enclosed by the pericardium, a thin, fluid-filled sac that reduces friction as the heart beats.
Layers of the Heart Wall:
Epicardium: Thin, outer layer that is part of the pericardial sac and contains blood vessels that supply the heart muscle.
Myocardium: The thick muscular middle layer, responsible for the contraction and relaxation of the heart muscle, thus pumping blood.
Endocardium: A thin inner layer that lines the heart chambers and valves, providing a smooth surface for blood flow.
Heart Chambers and Valves
Chambers:
Right and left atria (upper chambers that receive blood).
Right and left ventricles (lower chambers that pump blood).
Valves:
Atrioventricular (AV) Valves: Prevent backflow into the atria during ventricular contraction (tricuspid valve on the right and bicuspid/mitral valve on the left).
Semilunar Valves: Prevent backflow into the ventricles during relaxation (pulmonary valve on the right and aortic valve on the left).
Septa:
Interatrial septum: Separates the right atrium from the left atrium.
Interventricular septum: Separates the right ventricle from the left ventricle.
Coronary Circulation
Encompasses the blood flow to and from the tissues of the heart muscle itself.
Conditions Related to Blood Flow:
Angina Pectoris: A condition characterized by chest pain due to reduced blood flow to the heart muscle during periods of stress or exertion.
Atherosclerosis: A condition where plaque builds up in the arteries, leading to narrowed passages and restricted blood flow.
Myocardial Ischemia: Occurs when blood flow to the heart muscle is reduced, causing insufficient oxygen for the heart muscle to function properly.
Myocardial Infarction: Commonly known as a heart attack, this occurs from complete obstruction or prolonged ischemia leading to damage of the heart muscle.
Function of the Heart
Cardiac Cycle:
Represents the complete sequence of contraction (systole) and relaxation (diastole) lasting approximately 0.8 seconds.
Electrical Conduction System:
Composed of specialized cells capable of generating and conducting electrical impulses necessary for heart function.
Sinoatrial (SA) Node:
Located in the right atrium near the entrance of the superior vena cava.
Acts as the natural pacemaker of the heart, initiating electrical impulses that trigger heartbeats.
Sets the normal sinus rhythm, allowing the heart to maintain a regular pace (about 60-100 beats per minute at rest).
Atrioventricular (AV) Node:
Situated at the junction of the atria and ventricles.
Receives impulses from the SA node and delays them for a brief moment (about 0.1 seconds) to allow the atria to contract and empty blood into the ventricles before they contract.
Sends signals to the Bundle of His.
Bundle of His (Atrioventricular Bundle):
A pathway of fibers located in the interventricular septum.
Transmits impulses from the AV node to the right and left bundle branches.
Right and Left Bundle Branches:
Extend through the interventricular septum towards the apex of the heart and conduct impulses to the ventricles.
Purkinje Fibers:
A network of fibers that spread throughout the ventricular walls.
Conduct the impulse rapidly, allowing for a synchronized contraction of the ventricles, which efficiently pumps blood to the lungs and body.
Function and Mechanism:
The electrical impulse begins at the SA node, causing the atria to contract and push blood into the ventricles.
The impulse then travels to the AV node where it is briefly delayed, ensuring that the atria fully empty before the ventricles contract.
Following the delay, the impulse travels through the Bundle of His, branching into the right and left bundle branches and then into the Purkinje Fibers, stimulating the ventricles to contract in unison.
Regulation of Heart Rate:
The SA node is influenced by the autonomic nervous system: the sympathetic nervous system can increase heart rate while the parasympathetic nervous system can decrease it.
Hormones such as adrenaline can also affect heart rate by enhancing activity of the SA node.
Electrocardiogram (ECG or EKG):
A diagnostic tool that records the heart's electrical activity throughout the cardiac cycle, providing valuable insights into heart health.
lectrograph (ECG or EKG): A diagnostic tool used to record the heart's electrical activity.
Function: Detects electrical impulses generated by the heart as it beats.
How it Works:
Electrodes are placed on the skin to capture electrical signals.
Signals are transmitted and processed to create a visual graphical representation.
Utility: Provides insights into heart rhythm, identifies irregularities, and detects conditions such as ischemia.
Heart Sounds and Rates:
contract- systole
relax- diastole
Heart Sounds:
First sound (“lubb”): Created by the closure of AV valves during ventricular contraction.
Second sound (“dupp”): Resulting from the closure of semilunar valves as the ventricles relax.
Heart Rate and Cardiac Output:
Heart Rate: Normally averages around 72 beats per minute.
Cardiac Output: The volume of blood pumped by the heart per minute, calculated as the product of heart rate and stroke volume.
Arrhythmia: A condition characterized by an irregular heartbeat, which can affect the efficiency of cardiac output and overall heart function.
Bradycardia- slow heart rate, under 60 bpm
Tachycardia- fast heart rate over 100 bpm
Pulse and Blood Pressure
Pulse: A rhythmic throbbing felt in arteries as a result of alternating expansion and contraction due to the heartbeat.
Typical pulse rates vary from 60 to 100 beats per minute in adults.
Blood Pressure: Refers to the force exerted by circulating blood on the walls of blood vessels.
Sphygmomanometer: A device used to measure blood pressure, typically denoted as systolic/diastolic pressures.
Systolic Pressure: The pressure in the arteries during ventricular contraction, representing the peak pressure.
Diastolic Pressure: The pressure in the arteries during ventricular relaxation, representing the lowest pressure.
Disorders of the Heart
Common Disorders:
Angina Pectoris
Aortic stenosis
Bacterial endocarditis
Congestive heart failure
Myocardial Infarction
Pericarditis
Diagnostic Tests:
Tests include arterial blood gases analysis, lipid profile (cholesterol levels), electrocardiograms (ECGs), echocardiograms, and stress tests, among others.
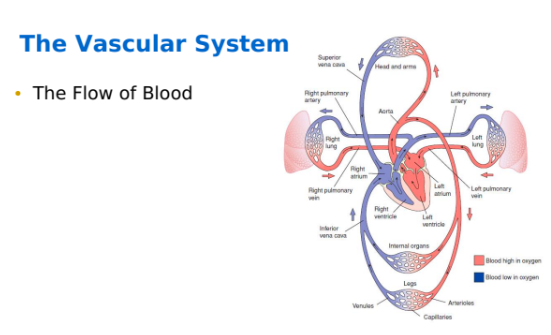
The Vascular System
Functions:
Pulmonary Circulation: Transports deoxygenated blood from the right ventricle to the lungs for gas exchange, releasing carbon dioxide and absorbing oxygen.
Systemic Circulation: Distributes oxygenated blood and essential nutrients from the left ventricle to the various tissues of the body.
Structures:
Arteries: Vessels that carry oxygen-rich blood away from the heart to the body; characterized by thick elastic walls that can withstand high pressure.
Veins: Vessels that return deoxygenated blood to the heart; have thinner walls and contain valves to prevent backflow, aiding in venous return against gravity.
Capillaries: Microscopic blood vessels where the exchange of oxygen, carbon dioxide, nutrients, and wastes occurs between blood and tissues, facilitating cellular respiration.
Blood Vessel Structure
– Layers
Tunica externa:
outer layer of a blood vessel
connective tissue
thicker in arteries than in veins
Tunica media:
middle layer
thickest layer of the blood vessel
made of smooth muscle & elastic fibers
Tunica interna:
inner layer
made of single layer of endothelial cells with an basement membrane, connective tissue, & elastic internal membrane
— Lumen: Internal space of a blood vessel, through which blood flows
— Valves- Thin, membranous leaflets in veins prevent backflow of blood
Phlebotomy Related Vascular Anatomy
Antecubital fossa
shallow depression in arm anterior and below elbow bend
site of major veins
first choice for venipuncture
H- shaped pattern of antecubital veins
median cubital vein
located near center of AC
preferred vein/ first choice
cephalic vein
located in lateral aspect of AC
second choice
basilic vein
located in medial aspect of AC
last choice
M- shaped pattern of antecubital veins
Cephalic vein
Median vein- first choice
Median cephalic- second choice
Median basilic- third choice
Basilic vein
greatest risk of nerve injury is w/ venipuncture in most medial and lateral portions of AC.
Bicipital aponeurosis
median vein and lateral aspect of median cubital vein overlie this fibrous membrane
which serves as a protective barrier for the underlying structures during procedures such as blood draws.
The bicipital aponeurosis also provides a layer of protection for the brachial artery and median nerve, which are critical structures that must be preserved during venipuncture.
an attempt to locate one of these veins on either arm before an alternate AC vein is considered.
Infant scalp veins
used only with physician permission and special training
Dorsal forearm, hand, and wrist veins
veins on lateral wrist above thumb to mid forearm must be avoided due to nerve injury risk
Leg, ankle, and foot veins
high risk for
phlebitis- vein inflammation followed by erythema and edema
thrombosis- thrombus(blood clot) formation can obstruct blood flow
only used with physicain permission
Arm and leg arteries- not routinely used for blood collection
Disorders
Aneurysm- A localized, blood-filled balloon-like bulge in the wall of a blood vessel, often leading to serious complications if it ruptures.
Arteriosclerosis- thickening and hardening of the arterial walls, which can restrict blood flow and increase the risk of heart attack and stroke.
Artherosclerosis- buildup of fatty deposits (plaque) in the arteries, leading to reduced blood flow and an increased risk of cardiovascular diseases.
Embolism- characterized by the obstruction of a blood vessel by an embolus
Embolus- blood clot that travels through bloodstream; causing a blockage in a blood vessel, potentially resulting in serious complications such as stroke or pulmonary embolism.
Hemorrhoids- swollen and inflamed veins in the rectum and anus that cause discomfort and bleeding.
Phlebitis- vein inflammation followed by erythema and edema
Thrombophlebitis- vein inflammation accompanied by blood clot formation, leading to pain, edema, and erythema in the affected area.
Thrombus- blood clot that forms in a blood vessel and remains attached to its place of origin.
Diagnostic tests
DIC screens
Lipoproteins
Prothrombin time
Partial thromboplastin time
Triglycerides
Blood Composition
Plasma:
90% water
gases(O2, CO2, N)
minerals(Na, K, Ca, Mg)
Carbs & lipids
proteins
waste products
vitamins, hormones, drugs
Formed elements
Erythrocyes- RBCs
most numerous in body
carry O2, CO2
produced in bone marrow
Leukocytes- WBCs
formed in bone marrow and lymphatic tissue
neutralize/ destroy pathogens
2 types-
Granulocytes: a type of white blood cell that plays a key role in the immune response by attacking and engulfing pathogens.
Agranulocytes: A type of white blood cell that includes lymphocytes and monocytes, playing a crucial role in the immune response and the formation of antibodies.
Lymphocytes: A subtype of agranulocytes that are essential for adaptive immunity, including T cells and B cells, which help to recognize and remember specific pathogens.
Monocytes: Another subtype of agranulocytes that differentiate into macrophages and dendritic cells, aiding in the phagocytosis of pathogens and the activation of other immune cells.
Thrombocytes: Also known as platelets, these are small cell fragments essential for blood clotting(coagulation) and wound healing.
Blood type
inherited
determined by presence or absence of specific antigens on RBCs
a person’s blood either contains or has the ability to develop antibodies for the opposite blood type.
receiving the wrong blood type can cause erythrocytes tp agglutinate(clump together) or hemolyze(burst)
some types may also include additional factors such as the Rh factor, which can further influence compatibility during blood transfusions.
two common types of blood group systems
ABO
two antigens- A & B
Four blood types A, B, AB, O
Rh
based on D antigen/Rh factor
Rh+ : RBCs have D antigen
Rh- : RBCs don’t have D antigen
Hemolytic disease of the newborn- RhoGam immune globulin
Compatibilty test/cross match is performed to ensure that the blood types of the donor and recipient are compatible, reducing the risk of transfusion reactions. This process involves mixing a small sample of the donor's blood with that of the recipient to observe any agglutination, which indicates an incompatibility.
Blood Specimens
serum
fluid portion of blood that remains after clotting
can be separated from clot by centrifugation
doesn’t contain fibrinogen
plasma
fluid portion of whole blood separate from RBC, WBC, platelet by centrifugation
contains fibrinogen
specimen must be collected in anticoagulant tube
used when serum cannot be used
whole blood
blood in same form as bloodstream
cannot clot or separate
must be colleted in anticoagulant tube
must be mixed min. twice just before test