Impotence and Sterility
Definitions of Key Terms
Impotence: Inability of a person to perform sexual intercourse.
Sterility: Inability of a male to beget children or a female to conceive children.
Sexual Dysfunction: Impairment in sexual desire or the ability to achieve sexual gratification. It can take three forms:
Erectile Dysfunction (Impotentia): Difficulty in attaining or sustaining an erection.
Failure to Ejaculate (Impotentia Ejaculandi): Inability to ejaculate.
Premature Ejaculation (Ejaculatia Precox): Releasing semen earlier than desired.
Importance of Erection
The ability to gain and maintain an erection is crucial for sexual intercourse. Impotence can have legal ramifications in both civil and criminal contexts.
Civil Implications
Nullity of Marriage: Marriage can be declared void if sexual intercourse is not consummated.
Divorce: Inability to engage in sexual intercourse can be grounds for divorce.
Adultery Defense: Impotence may be used as a defense in adultery cases.
Disputed Paternity: Can be raised in legal disputes about parentage.
Compensation Claims: Loss of potency due to injury or hazards can lead to claims for damages.
Criminal Implications
Adultery: Men may face legal consequences; impotence might serve as a defense.
Rape and Sexual Assault Cases
Unnatural Sexual Offenses
Blackmail and Defamation Issues
Anatomy of Male and Female Genitals
Male External Genitalia
Includes the penis and scrotum.
Penis Structure: Composed of vascular muscular tissue:
One corpus spongiosum and two corpora cavernosa.
Glans Penis: Located at the tip of the spongiosum; urethra passes through it.
Erectile tissues feature sinusoids lined by smooth muscle cells and endothelial cells.
Nervous System Innervation
Dorsal Nerve of Penis: Sensory innervation from the pudendal nerve.
Parasympathetic Input: From S2, S3, and S4 segments responsible for arousal.
Sympathetic Input: From thoracolumbar plexus (L1 and L2) providing inhibitory signals.
Male Reproductive Structures
Testes: Contain seminiferous tubules that produce spermatozoa.
Vas Deferens: Connects testicles to the prostate gland.
Seminal Vesicles: Two pouches that meet with the vas deferens to form the ejaculatory duct.
Female External Genitalia
Called the vulva or pudendum.
Includes mons pubis, labia majora, labia minora, clitoris, vestibule of vagina, and greater vestibular glands.
Internal Genitalia: Consists of ovaries, fallopian tubes, uterus, and vagina.
Sexual Cycle in Males
Stimulation
Excitation
Erection
Emission and ejaculation with orgasm
Resolution
Sexual Cycle in Females and Physiology of Erection
Female Sexual Cycle
Stimulation
Excitation
Arousal with vaginal congestion
Orgasm
Resolution
Physiology of erection
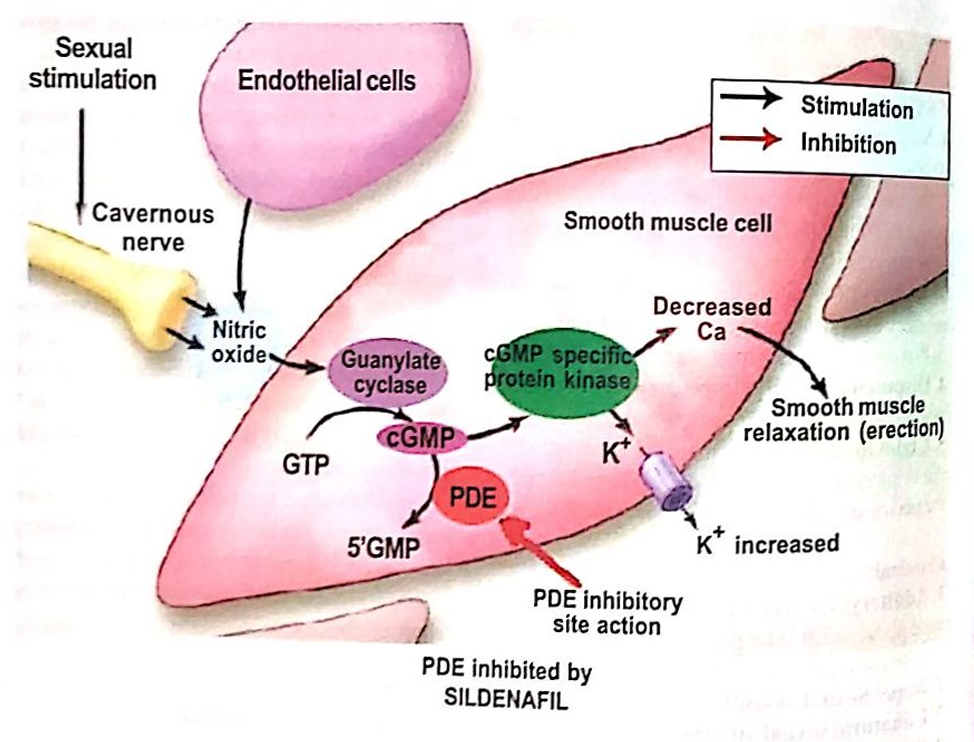
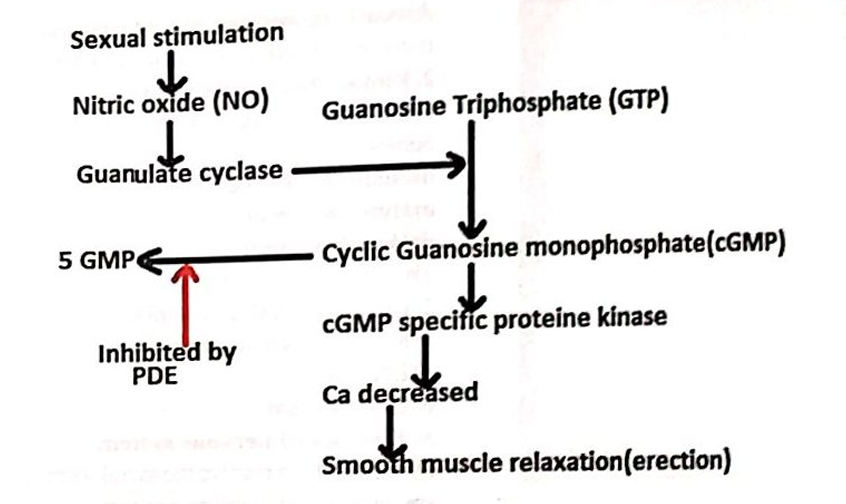
Erection Mechanism: Driven by psychogenic and somatogenic stimuli and facilitated by parasympathetic stimulation.
Nitric Oxide Release: Following stimulation, nitric oxide (NO) is released from endothelial cells in the cavernosa.
NO activates guanylate cyclase, converting GTP to cGMP, which reduces intracellular calcium concentration, leading to muscle relaxation.
Increased blood flow engorges the cavernous spaces, compressing veins and causing rigidity in the penis.
Phosphodiesterase (PDE): Regulates levels of cGMP; inhibition of PDE (e.g., by Sildenafil/Viagra) sustains erection by preventing breakdown of cGMP.
Ejaculation Process
Initiated by sympathetic stimulation, leading to closure of the urethral sphincter and rhythmic contractions that eject semen at orgasm.
Resolution Phase: Characterized by vasoconstriction and smooth muscle contraction (detumescence).
Causes of Male Impotence
Age: Potency may vary; very young and very old individuals may experience impotence.
Local Causes:
a)Congenital absence of penis
b)Very rudimentary and infantile penis
c)Large hydrocele
d)Gross abnormality of external genitalia
e)Hypospadia and epispadia
f)Traumatic amputation of penis
g)Surgical removal of testicles after puberty
Endocrinological Causes:
a)Diabetic neuropathy
b) Addison’s disease
c) Hypopituitarism
d) Hypothyroidism
c) Cushing’s syndrome
Chromosomal Anomalies:
a) Klinefelter’s Syndrome
b) Intersex
c) Eunuchoidism
Nervous System Diseases: Conditions impacting sacral nerve function.
a) Tabes dorsalis
b) Disseminated sclerosis
c) Spina bifida
d) Meningomyelocele
e) Tumours of cauda equina
f) Hemiplegia, paraplegia and quadriplegia
Injuries:
a) Fractures of lumbar vertebrae at Ll and L2
b) Fracture pelvis
c) Injury to cauda equina.
Drug Abuse:
a)Cannabis,Alcohol
b)Beta blockers
c)Estrogen therapy
Vascular Issues: Conditions affecting arterial flow (e.g., Leriche syndrome).
Chronic Poisoning: Exposure to toxins like lead or arsenic.
Psychogenic Factors: A substantial portion of impotence cases stems from psychological origins.
Psychogenic Causes of Impotence
Anxiety, guilt, and learned responses can significantly impact sexual function. Notable conditions include:
Honeymoon Impotence: Anxiety associated with newlywed couples.
Quoad Hanc: relative impotence, a person may be impotent to a particular woman.
Oedipus Complex: Seeing the mother in his own wife, not able to have sex with his wife.
Tests for potency
Nocturnal penile tumescence
Doppler ultrasound
Psychological test
Common causes of impotence
Vasculogenic impotence (40%)
Chronic diabetic neuropathy (20%)
Psychogenic (12%)
Neurogenic causes (8%)
Malignancy and others (20%)
Impotence in Females
Types of Impotence
Developmental Abnormalities: Congenital conditions leading to structural issues.
Local Diseases: Tumors or obstructions in the reproductive tract.
Psychogenic Factors: Conditions such as vaginismus, marked by involuntary contractions of vaginal muscles.
Electra complex
Medicolegal Significance of Female Impotence
Grounds for Nullity of Marriage: If the marriage is not consummated.
Grounds for Divorce: Impotence can be presented in divorce cases.
Sterility
Sterility: Permanent inability to conceive, which may be present in both genders, not always correlating with impotence.
Infertility: Defined as inability to conceive after one year of unprotected intercourse.
Causes of Sterility in Males
Cryptorchidism: Undescended testicles can lead to sterility.
Endocrinological Diseases: Conditions impacting hormonal function can inhibit spermatogenesis.
Chromosomal Abnormalities: Such as Klinefelter syndrome affecting testicular function.
Testicular Diseases: Mumps and tuberculous infections can lead to infertility.
Auto-immune Mechanisms: Body may attack sperm, impacting fertility.
Chronic Poisoning and Drug Abuse: External substances can disrupt reproductive capabilities.
Causes of Sterility in Females
Ovarian Issues: Conditions like Turner's syndrome affecting ovulation.
Tubal Diseases: Such as infections causing blockages.
Uterine Anomalies: Abnormal uterus structures can lead to sterility.
Cervical Problems: Such as chronic cervicitis affecting conception.
Age Factor: Women become fertile at menarche but may struggle with infertility in later years.
Artificial Insemination
Types of Artificial Insemination
Artificial Insemination Homologous (AIH): Utilizes husband's sperm for insemination.
Applicable when the husband is impotent but has viable sperm.
Can also address hostile cervical mucus situations.
Artificial Insemination Donor (AID): Involves using donor sperm.
Indicated for cases like azoospermia or hereditary diseases in the husband.
Criteria for AID
Donor characteristics must be taken into account:
Must not be a relative, under 40, healthy, and free of hereditary diseases.
Written consent required from both donor and recipients.
Donor and recipient identities must remain confidential.
Regulations to prevent issues like incest or genetic complications.
The Delhi Artificial Insemination (Human) Bill 1995
Purposes of the Legislation
To allow issue-less couples to have a child.
To give legal status to artificial insemination.
To control the spread of HIV.
To regulate the donation, sale, or supply of human sperm or ovum.
To ensure medical practitioners do not segregate xx or xy chromosomes.
To maintain donor and recipient confidentiality.
To prohibit unregistered semen banks.
Legal Problems Associated with AID
Adultery: Cannot be charged against the donor and recipient, as sexual intercourse is essential for this charge under section 497 I.P.C.
Legitimacy: A child born from AID may be deemed illegitimate since the husband is not the biological father.
Marriage Nullity
Incest Concerns
Psychological Issues
Assisted Reproductive Technology (ART)
Definition
ART involves fertility treatments where gametes (eggs and sperm) are manipulated outside the body and then reintroduced to establish pregnancy.
The process of surgical removal of eggs is referred to as egg retrieval.
Most Common Procedures
In Vitro Fertilization (IVF): Ovum is fertilized in a lab and implanted in the uterus, often using donor sperm if the husband is infertile.
Gamete Intrafallopian Transfer (GIFT): Involves retrieving the gamete and sperm, then transferring them into the fallopian tube via laparoscopic surgery.
Zygote Intrafallopian Transfer (ZIFT): Similar to GIFT, but a fertilized zygote is transferred to the fallopian tube.
Intracytoplasmic Sperm Injection (ICSI): A single sperm is injected into an ovum microscopically, potentially enhanced by selecting sperm using magnification (IMSI).
Supervision and Regulation of ART Clinics
Governed by the National Guidelines for Accreditation by ICMR, 2005.
ART clinics must be registered and meet specific guidelines regarding facilities and qualifications of staff.
All procedures require informed consent, and confidentiality must be maintained.
Restrictions on age for donors: 21-45 years for sperm and 18-35 for egg donors, with no usage of gametes from those under 21.
Protection of embryos: They may be frozen or used later by the couple or discarded after 5 years.
No embryo sex selection is permitted.
Surrogate Mother
Definition and Types of Surrogacy
A surrogate mother carries a child for another person or couple under a contractual agreement.
Altruistic Surrogacy: Surrogacy performed without financial compensation.
Commercial Surrogacy: Surrogacy for monetary gain.
Types
Traditional Surrogacy: The surrogate is the biological mother, with conception using the father’s sperm.
Gestational Surrogacy: IVF is performed, and the fertilized ovum is implanted in the surrogate without her genetic contribution.
Legal Considerations
Surrogate mothers have no rights to the child, as the biological parents retain custody post-birth.
Ethical, legal, and social issues regarding surrogacy need elucidation, especially given the legal shifts since 2014.
Indian Surrogacy Regulation
Commercial surrogacy has been banned as of 2018 with further amendments in 2020.
Couples must be legally married, have no children from unprotected intercourse within 5 years, and only Indian citizens can opt for surrogacy.
Ethical screening for donors must occur, and ART clinics must be accredited.
Surrogate mothers can be widows or divorced but can serve only once as a surrogate.
Sterilization Practices
Guidelines
Clients must be married, mentally sound, and meet stipulated age limits (22-49 for women).
Surgical procedures for women should consider timing relative to menstrual cycles and postpartum conditions.
Informed Consent Process
Written informed consent is mandatory from the person undergoing sterilization; consent from spouses is not required.
Surgical Techniques in males
Conventional Vasectomy: Involves incising the scrotum to cut and suture the vas deferens post-excision.
No-Scalpel Vasectomy (NSV): Similar results with minimal invasiveness.
Surgical Techniques in females
Minilap : MBBS
Laparoscopic sterilization : MBBS,MD/DGO
Certification and Outcomes
Certification post-surgery is contingent on the established absence of sperm in semen analysis for men and completion of menstrual cycle for women.
Success rates are high for both procedures with considerations for reversibility differing.
Hormone Replacement Therapy (HRT)
Overview
HRT (menopausal hormone therapy) compensates for falling estrogen levels in menopausal women, addressing symptoms like hot flashes and mood changes.
Signs and symptoms
Hot flashes
Vaginal dryness
Osteoporosis
Leg cramps
Mood changes
Irritability
Loss of sexual urge
Treatment Methods
Estrogen therapy
Combination of Estrogen and Progestin
Combination of Estrogen and other medicines
Adverse effects
Breast swelling, tenderness
Headache
Mood changes
Nausea
Vaginal bleeding
Thromboembolism
Risk of liver disease, breast and ovarian cancer
Concerns and Regulations
Emphasis has shifted over time after studies indicated increased health risks associated with HRT, leading to decreased usage among women.