A&P: Structural Organization
FALL SEMESTER 2024
Instructor: Anthony Uzwiak Made by: Ruby :x
uzwiak@dls.rutgers.edu

Structural Organization
An understanding of the various primary tissue types present in the human body is essential for understanding the structure and function of organs.
Topics included:
Identity the four basic tissue types, their general characteristics, and describe their contribution to more complex body structures
Describe the common characteristics of epithelial tissue
Classify the subtypes of epithelial tissue and describe characteristics associated with each subtype
Describe the common characteristics of connective tissue
Classify the subtypes of connective tissue and describe characteristics associated with each subtype
Classify the subtypes of muscle tissue and describe characteristics associated with each subtype
Classify the subtypes of nervous tissue and describe characteristics associated with each subtype

Classes of Tissue
Tissue, as you may now, are a group of closely associated cells performing a similar function. Histology is the study of tissue structure.
Tissue Type |
Nervous Muscular Epithelial Connective |
Primary Function Information Processing Contraction to Generate Force (movement) Cover exposed surfaces Structure and support |
Cell Types Neurons Smooth Cardiac Skeletal Squamous Cuboidal Columnar Transitional Pseudostratified Glandular Fibroblasts WBCs Mast cells Plasma Cells Macrophages Adipocytes |
Fibers Minimal Minimal Basement Membrane Collagen Reticular Elastic |
Fluids Nutrient-rich, aqueous Minimal Limited Depends on the type of Connective Tissue |

Epithelial
Epithelial tissues cover and protect surfaces inside and outside of the body.
Functions of Epithelial Tissue
Protection
Acts as a barrier and protects underlying structures from abrasion
Prevents substances from moving through it (toxic molecules and microorganisms).
Absorption
Contain carrier proteins which regulate the absorption of materials.
Filtration
Permits passage such as oxygen or carbon dioxide through
Secretion
Sweat
Enzymes
Characteristics of Epithelial Tissue
Mostly composed of cells: Cellularity
Close-packed cells with limited extracellular material
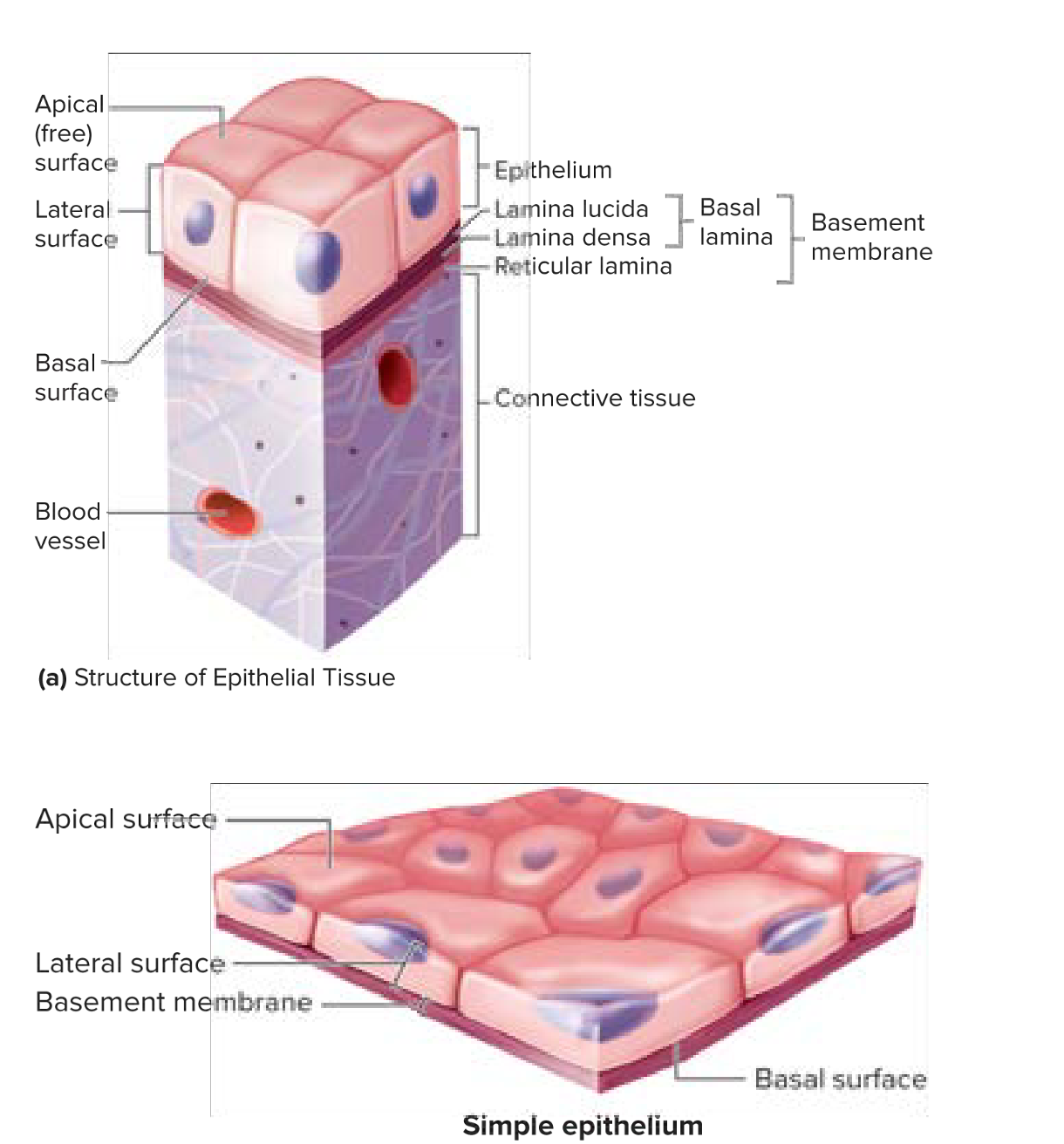
Cover body surfaces
Have an exposed surface
I.e, skin exposed to air; stomach lining exposed to food: the surface that is exposed is called apical (free) surface.
Cellular organization— attaches at the basal surface
Surface of cells that are anchored in place is called the basal surface
Material is called the basement membrane
Made up of two layers: basal lamina and reticular lamina
Can be further divided into lamina lucia and lamina densa.
Made up of extracellular material secreted by epithelial cells— important role in supporting/guiding cell migration in tissue repair
Deep to the basement membrane is the reticular lamina.
Between the epithelial cells (where epithelial cells are connected to each other) is the lateral surface.
All epithelial sheets are supported by connective tissue.
Cellular Connections
Tight junctions, desmosomes, and gap junctions
Tight junctions: held tightly together with proteins
Desmosomes: proteins extended from the cytoplasm of one cell into the cytoplasm of neighboring cells. Strong connection— etc; muscles
Avascular (meaning no blood vessels)
Innervated
Receives nervous innervation, includes nerves
Capable of regeneration
Replaced rapidly by cell division
Cell loss due to friction and contact with hostile environments
|
Classification of Epithelial Tissue
Epithelial cells are classified by the number of cell layers and shape of superficial cells. There are four major types of epithelium.
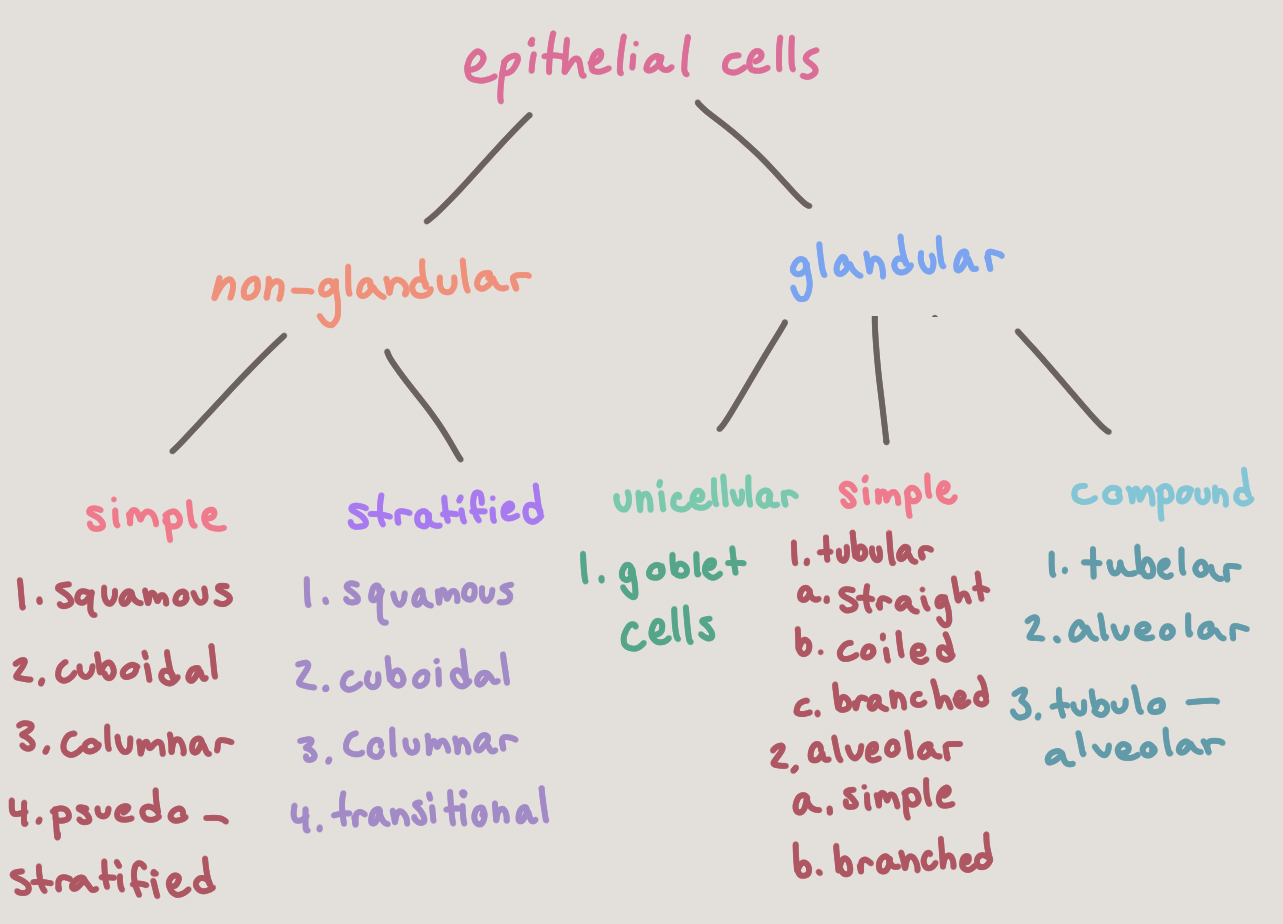
Epithelial tissue is nomenclature. In other words, they have two names— the first indicates the number of cell layers, and the second indicates the cell shape. All cells within a given layer will have the same shape. |
Layers
Simple (1 layer)
Single cell layer
Areas of absorption and filtration
Stratified (2+ layers)
Two or more cell layers
Areas of high abrasion
Cell Shape
Squamous
Flattened
Scale-like
“Squished”
Cuboidal
Boxlike
As tall as wide
“Cube”
Columnar
Tall
“Column”
Special Types
Transitional
Changes the number and layers and shape to have more surface area
Pseudostratified
One ayer but looks like more due to different sizes of cells
Has cilia on apical side
Shape of Nucleus
The shape of the nucleus conforms to the cell shape.
Squamous—disc shaped
Cuboidal—spherical
Columnar—elongated from top to bottom
Types of Simple Epithelia
Simple Squamous Epithelia
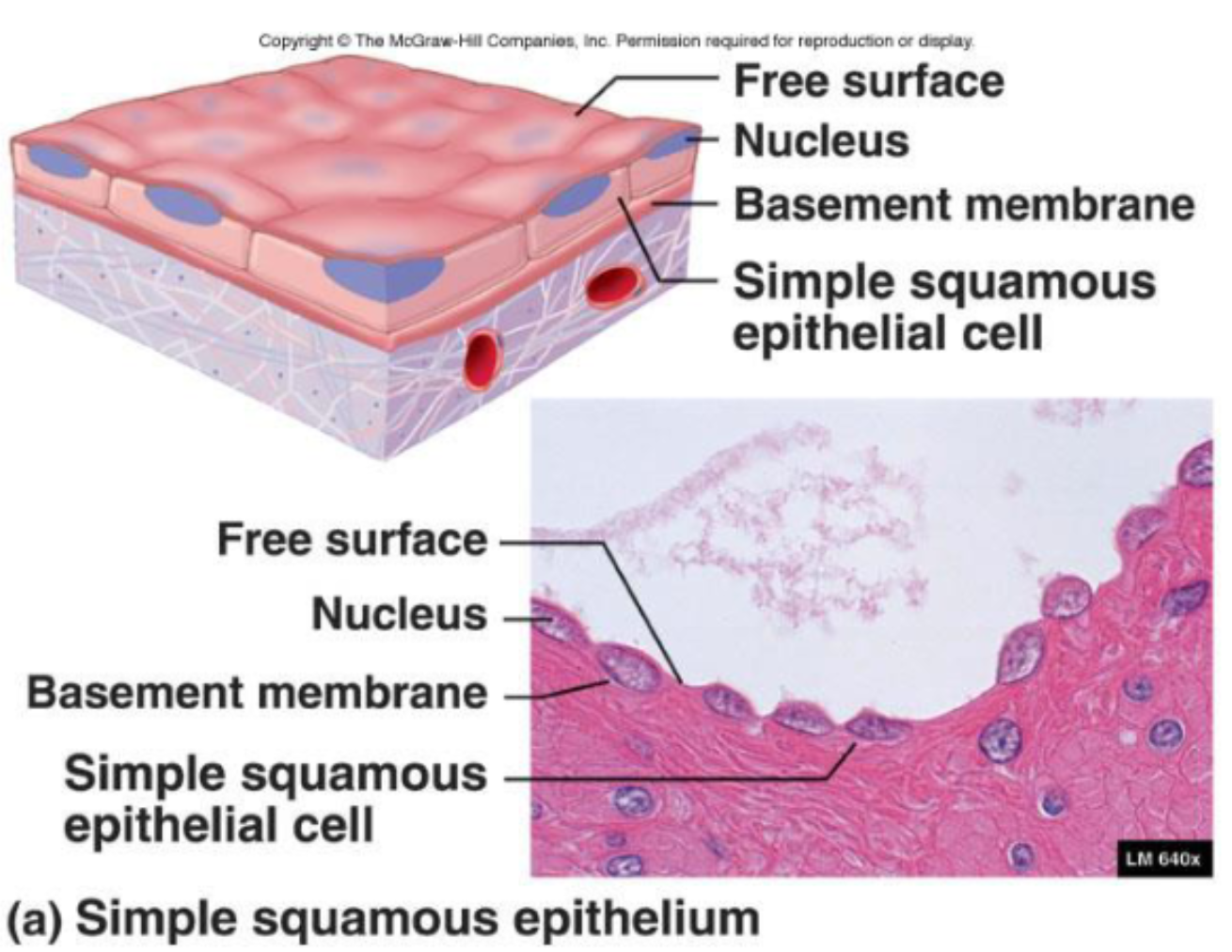
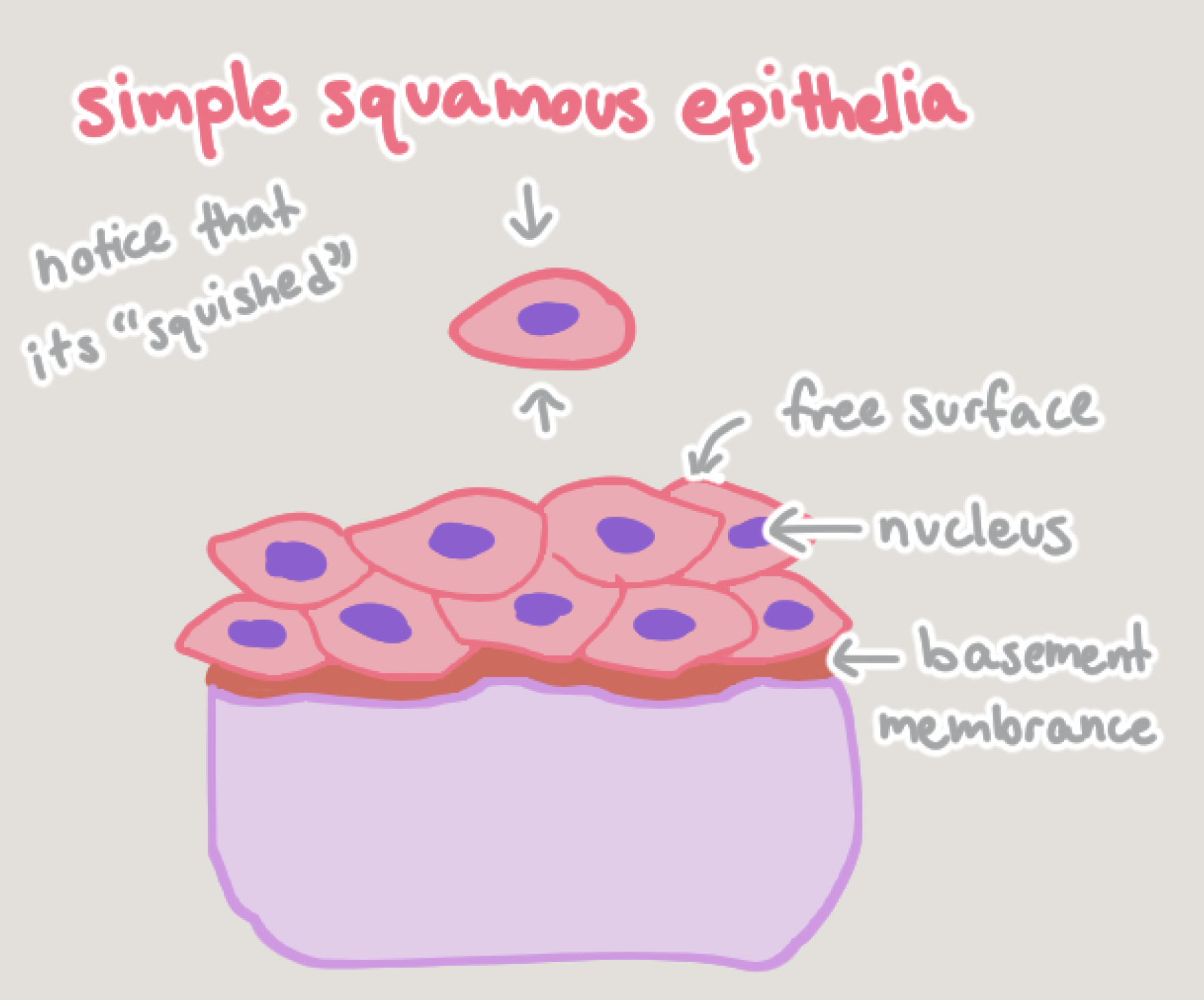
Function:
Diffusion, secretion, and filtration
Needed when fluids or air must readily travel for diffusion
Location:
Endothelium
Lining of the lymphatic system
Lining of all organs in cardiovascular system
Mesothelium
Serous membrane linings of ventral body cavity
Alveoli or capillary beds
Simple Cuboidal Epithelia
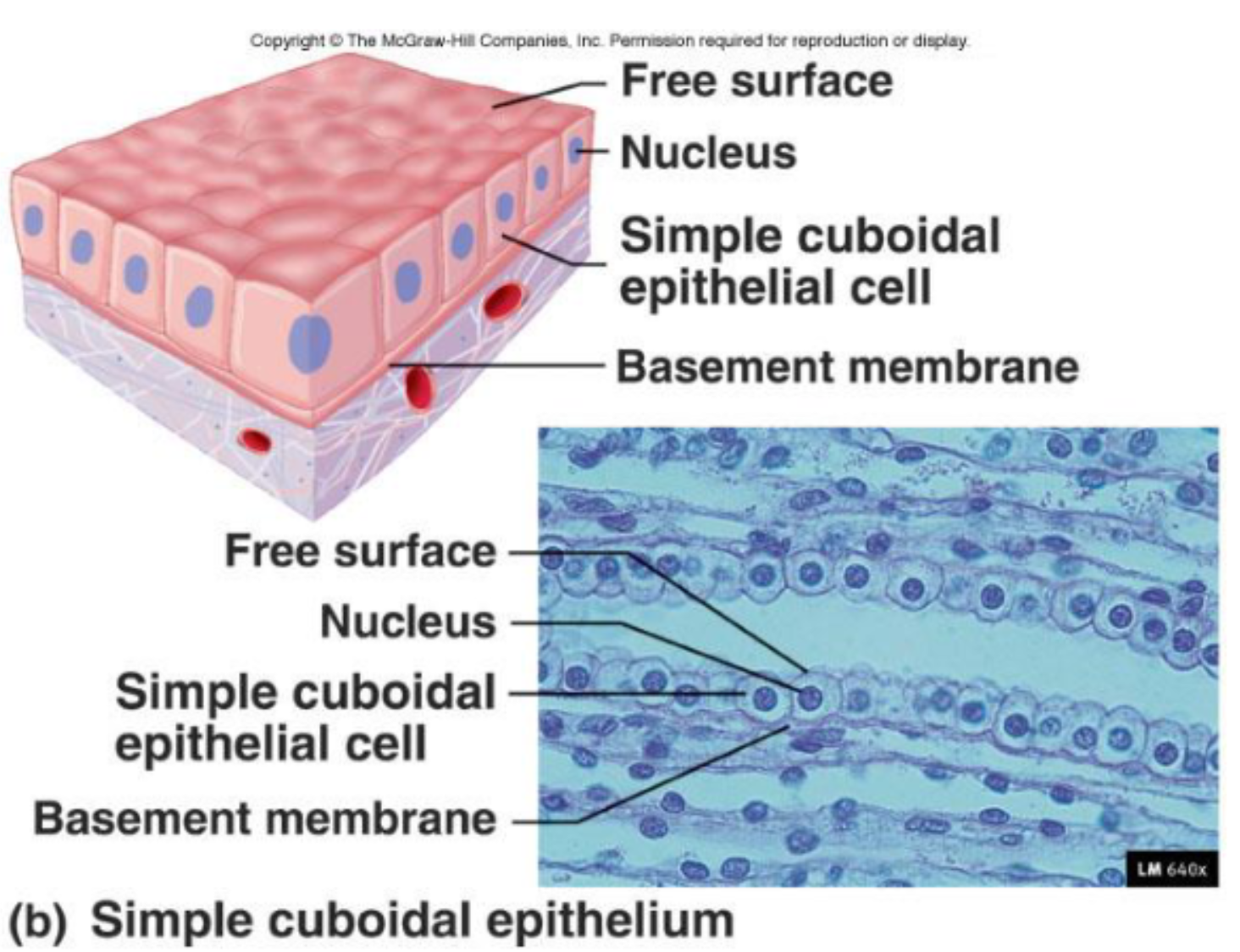
Function:
Secretion and absorption
Location:
Kidneys (nephron cells)
Plexus of the brain
Lining of lung bronchioles
Surfaces of ovaries
Microvilli may be present to increase surface area.
Simple Columnar Epithelia
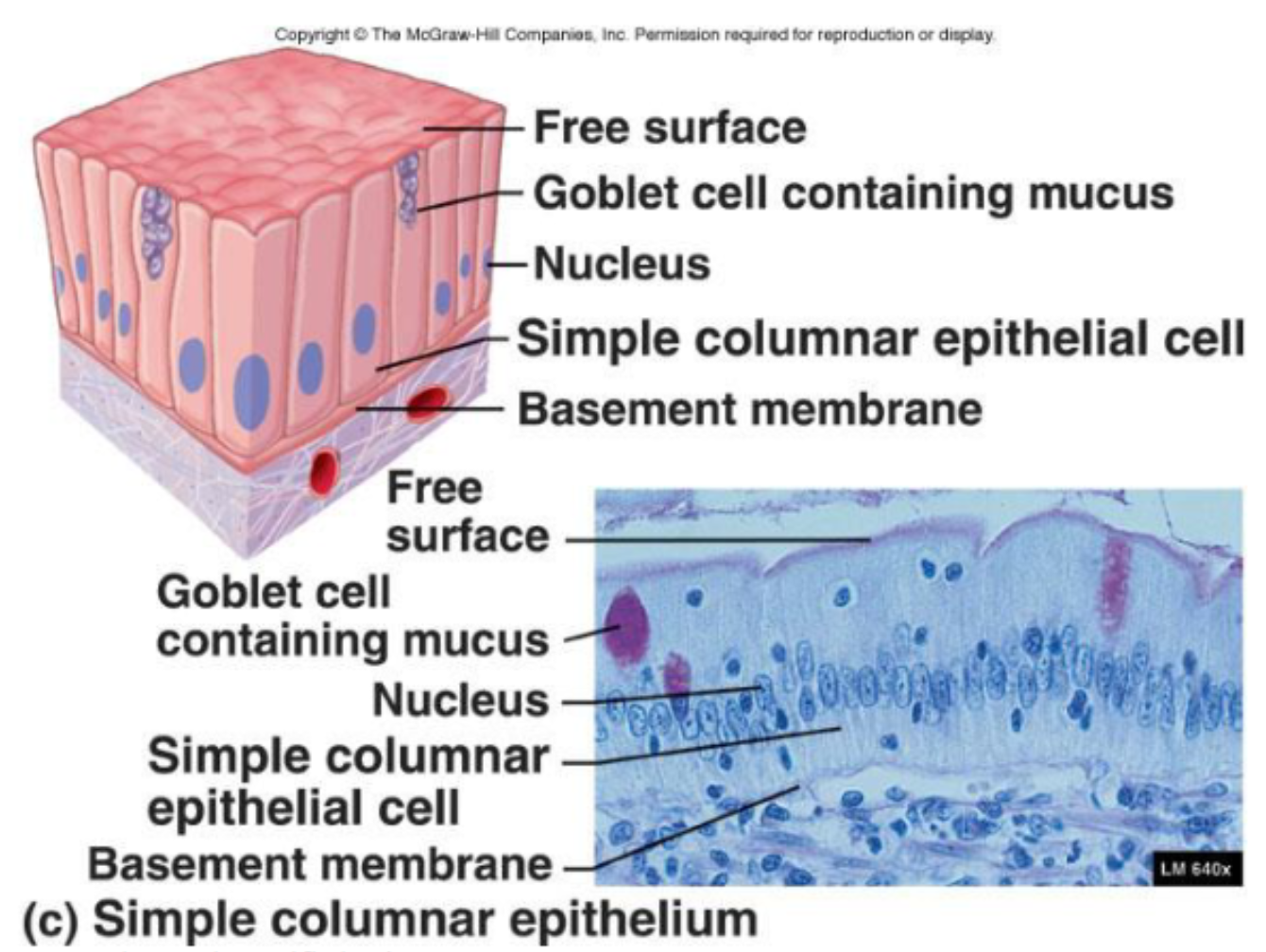
Function:
Absorption (specifically pinocytosis), protection, and secretion
Location:
Digestive tract, GI tract
Modifications:
Dense microvilli on apical surface
Goblet cells that secret protective lubricant
Pseudostratified Columnar Epithelia
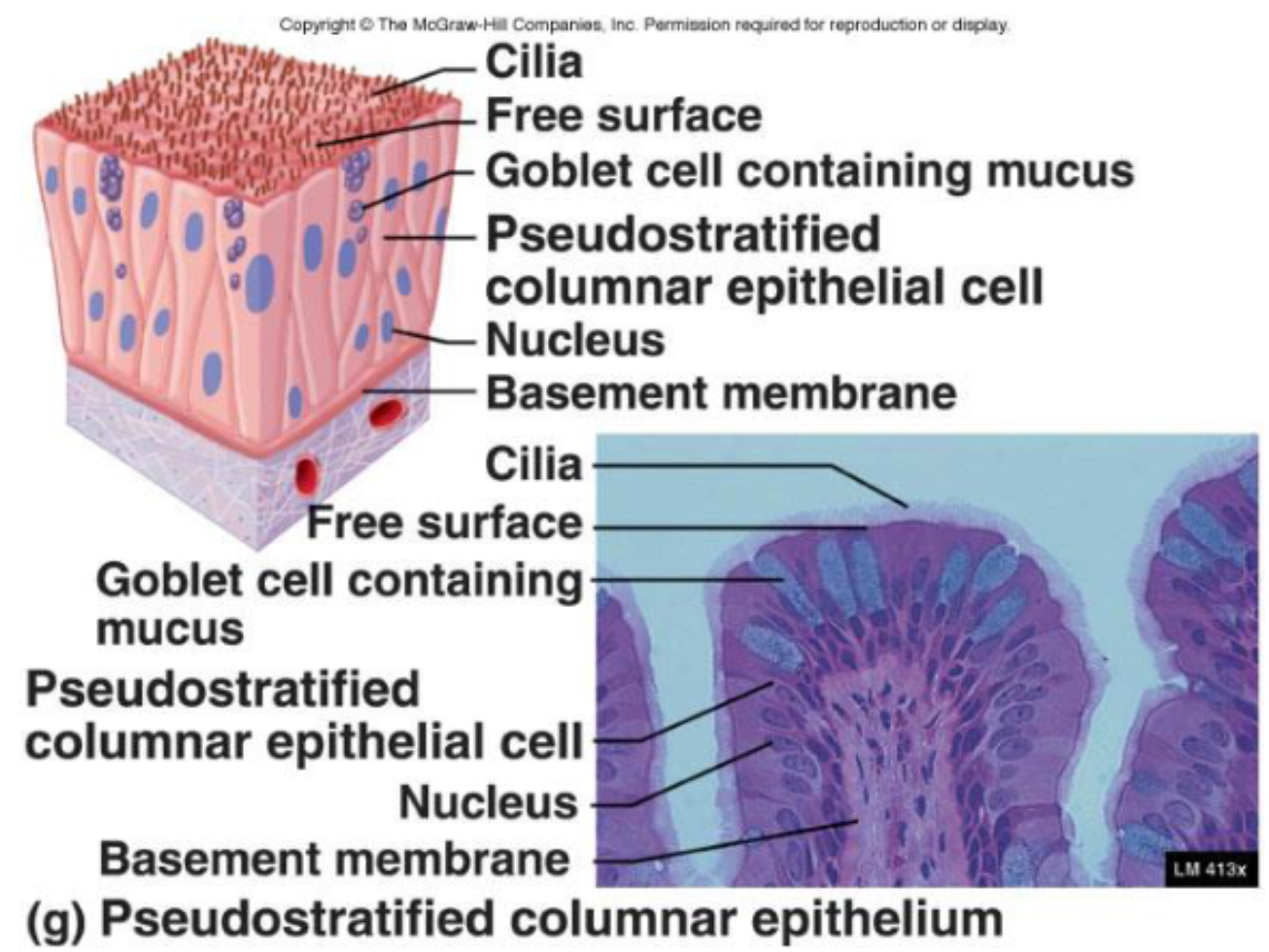
Single layer of cells that vary in height
Only tallest reach apical surface
Always ciliated
Cilia propel trapped matter out
Goblet cells secrete mucus
Mucus traps particulate matter
Nuclei are located at different heights
Function:
Absorption and secretion
Location:
Respiratory system (nasal cavities)
Reproduction
Types of Stratified Epithelia
Stratified epithelia typically have two or more layers.
Regenerate from below via mitotic division
Basal cell divide
Move apically to replace older surface cells
Durable
Provide protection
Stratified Squamous Epithelia
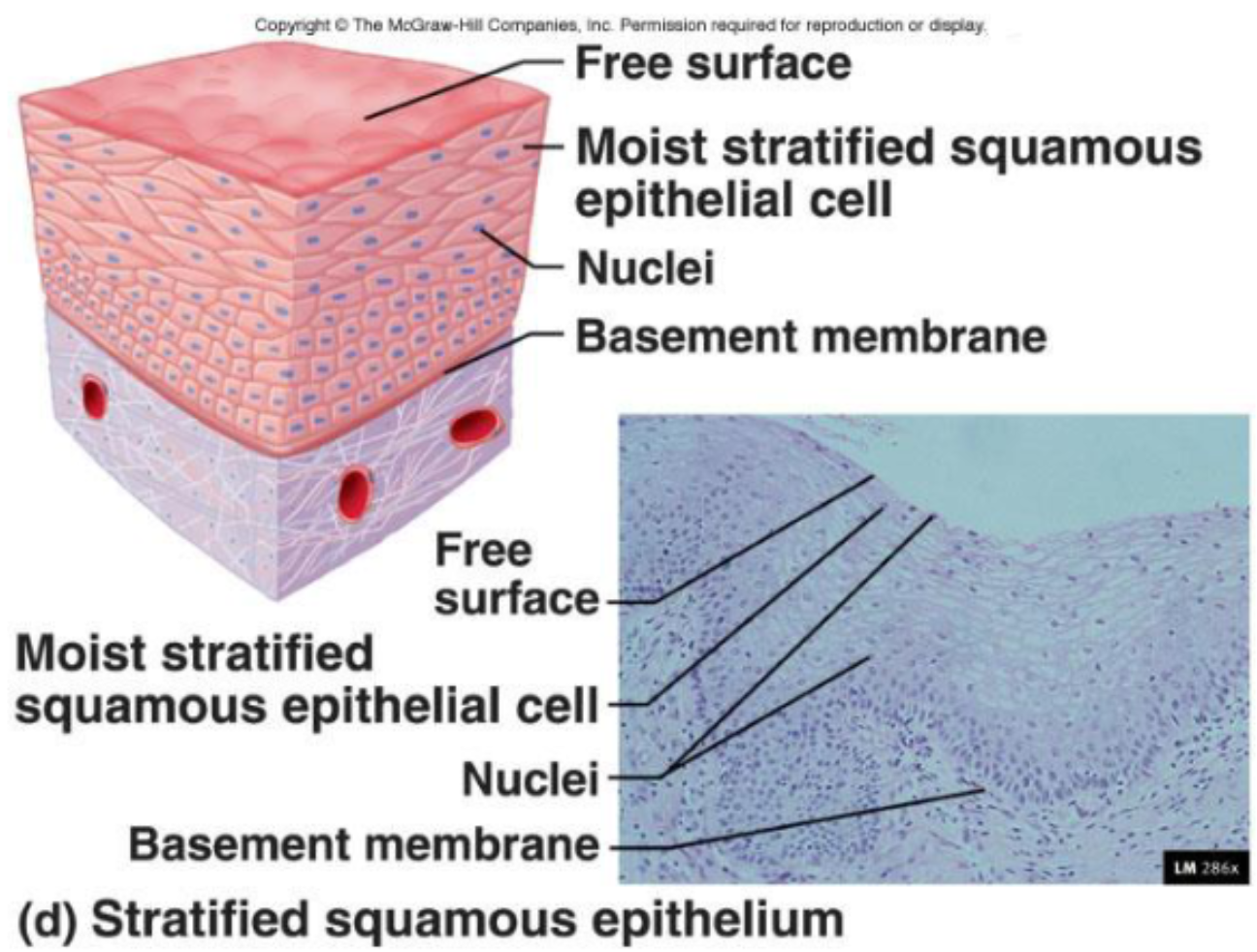
Surface cells are squamous
Deep layers consist most often of cuboidal
Stratified squamous is categorized as non keratinized (moist) or keratinized.
Non keratinized are living cells in the deepest and superficial layers— a layer of fluid covers superficial layers, making them moist
Keratinized are living cells only in the deepest levels, and the superficial layers are composed of dead cells
Function:
Protects against abrasion; mechanical protection wherever there is friction
Location:
Areas of abrasion
I;e, tongue or epidermis
Forms external surface of the body
Extends into all body openings
Outer layer (epidermis) is keratinized
Surface cells are flattened and atrophied
Stratified Cuboidal Epithelia
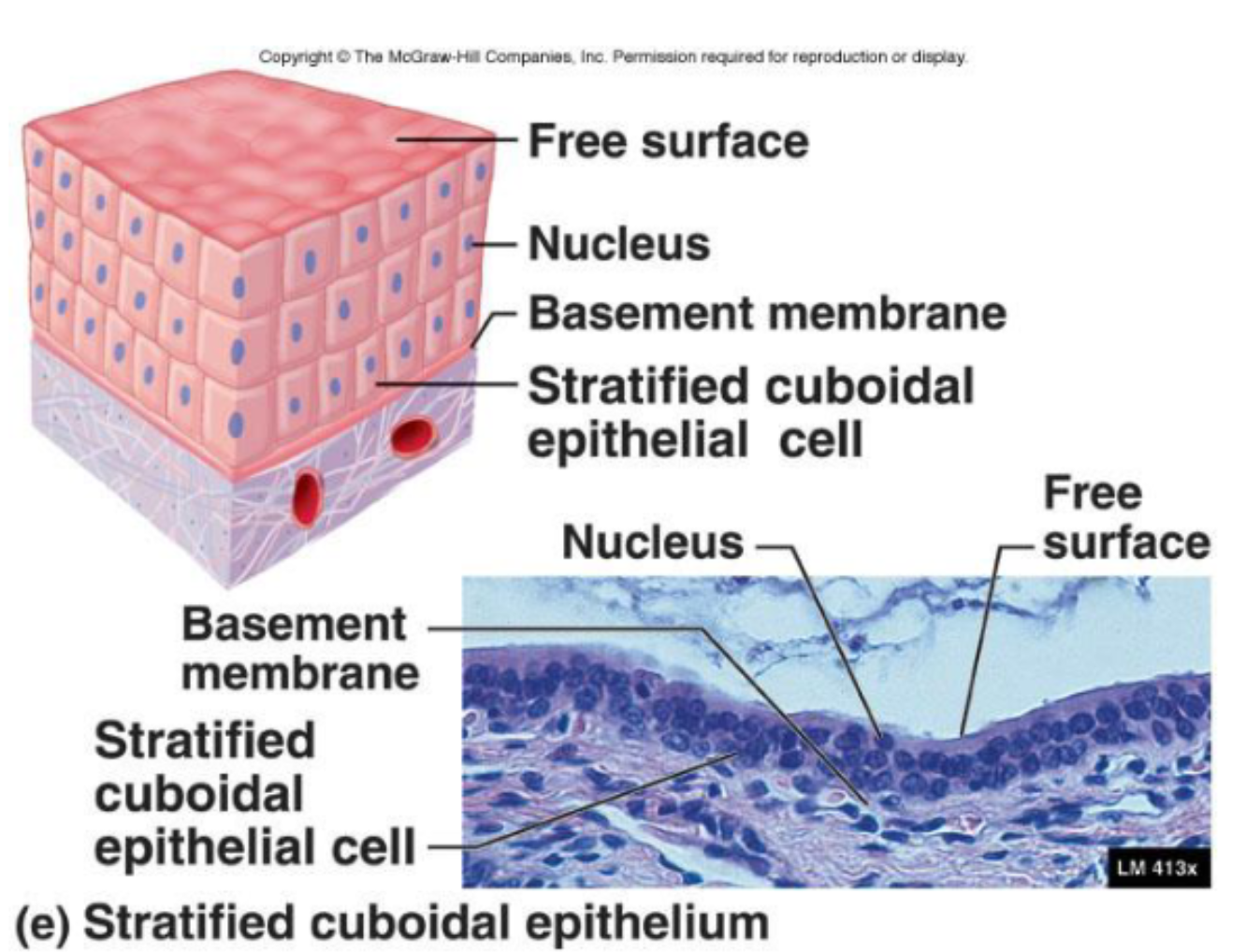
Rare
Function:
Movement and secretion
Location:
Glands
Ureter
Stratified Columnar
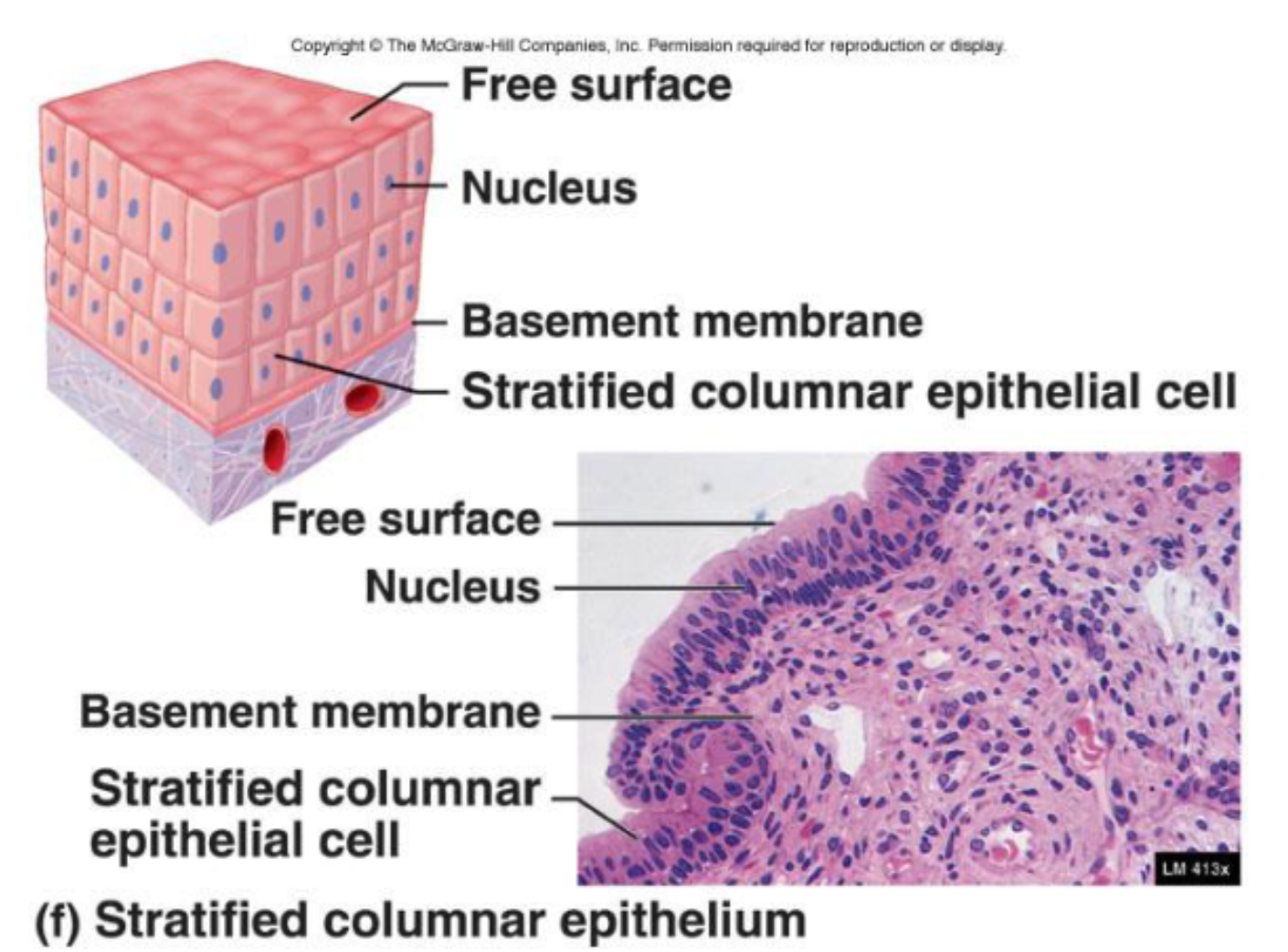
These are rare.
Function:
Protective and secretion
Location:
Location of eyelids
Urethra
Transitional Epithelia
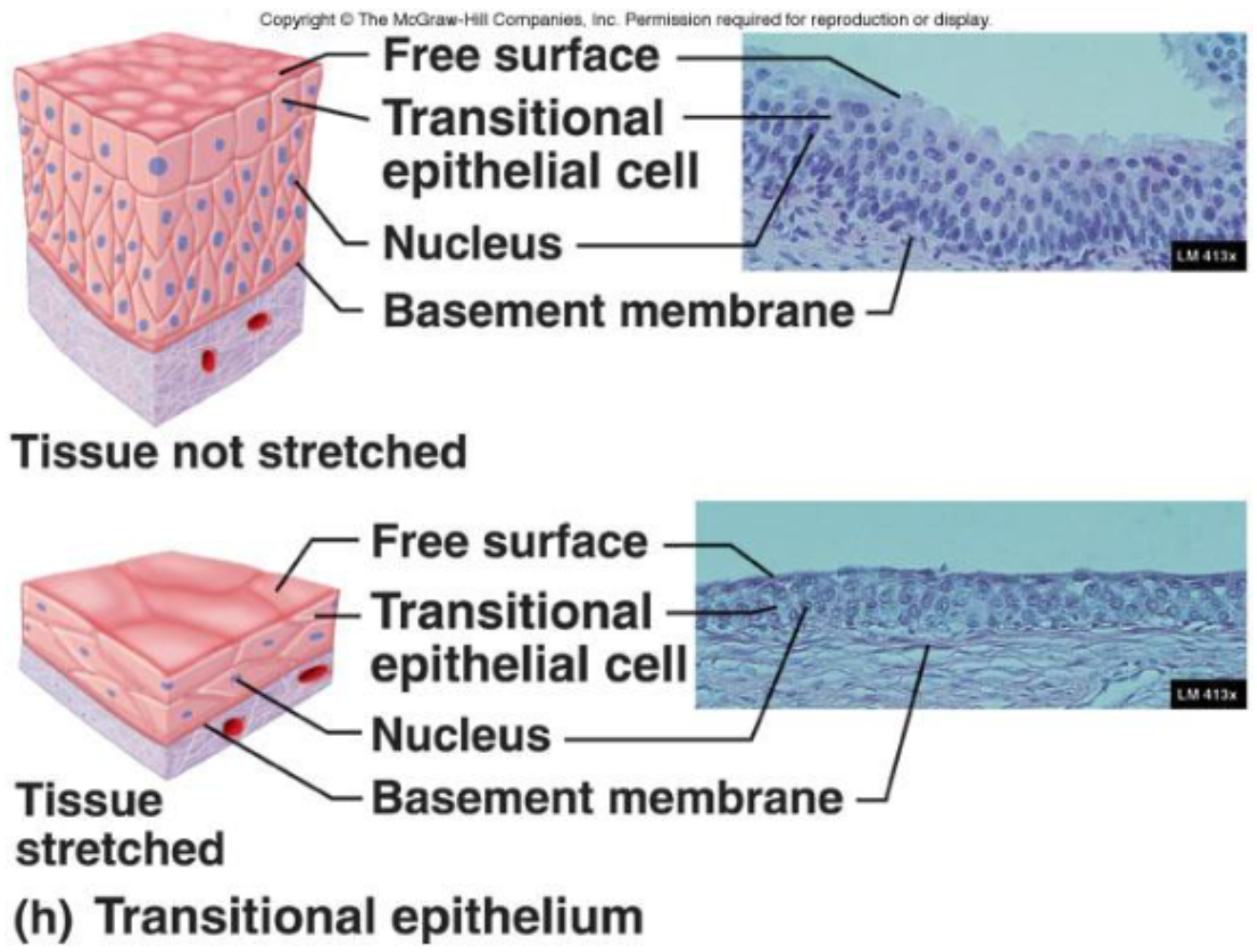
Function:
Accommodates fluctuations in the volume of fluid in an organ/tube
Need for more surface area
Location:
Lining of urinary organs
Apical cells can change shape to accommodate stretching
Classification of Glandular Epithelia
Epithelial tissue is capable of secretion. Specialized secretory organs called glands are responsible for secretion. They consist of one or more cells that make/secrete a product.
Secretion refers to the aqueous product of glandular cells and the process of making that product.
Formation involves active processes.
Made in ER, packed in Golgi, and secreted by exocytosis
There are two types of glands— exocrine and endocrine.
Exocrine
Secreted via ducts
Onto body surfaces or cavities
Endocrine
Ductless
Secrete directly into extracellular space
There are three specific distinctions of glands— duct structure, secretory structure, and mode of secretion.
Structure of Exocrine Glands
First, let’s distinguish between the duct structure and secretory structure.
The duct is the tube in contact with the epithelial tissue free surface, which transports secreted material.
The duct can be:
Simple— single, unbranched duct
Compound— branched duct
The secretory portion of the gland is found deeper within the epithelium, composed of cells responsible for producing the secreted material (secretory cells).
The secretory portions of the glands can be:
Tubular— straight, narrow tube with the same width as the duct
Acinar— a saclike structure whose width is greater than the width of the duct
They both are supported by connective tissue, which supplies blood and nervous fibers.
The fibrous capsule may penetrate the gland and divide it into lobes.
Three major categories of the exocrine glands are unicellular, simple, and compound.
Unicellular:
Some exocrine glands are composed of a single cell, making them unicellular.
Goblet cells that secrete mucus are unicellular.
Simple:
Simple glands are multicellular glands with a single, unbranched duct.
Some example of simple glands are:
Simple tubular
Glands forming a straight tube with no branching
Simple branched tubular
Glands with several tubular secretory portions branching rom single duct
Simple acinar
Glands with a single saclike secretory portion
Simple branched acinar
Several acinar secretory proportions branching from single duct
Compound:
Compound glands are multicellular glands that have several branched ducts. The secretory portions can be tubular or acinar, or a mixture of both.
Some example of compound glands are:
Compound tubular
Glands with multiple ducts, each with a narrow tubular secretory portion
Compound acinar
Glands with multiple ducts, each with several saclike secretory portions
Compound tubuloacinar
Glands with multiple ducts, each with several tubular and acinar secretory portions
Modes of Secretion by Exocrine Glands
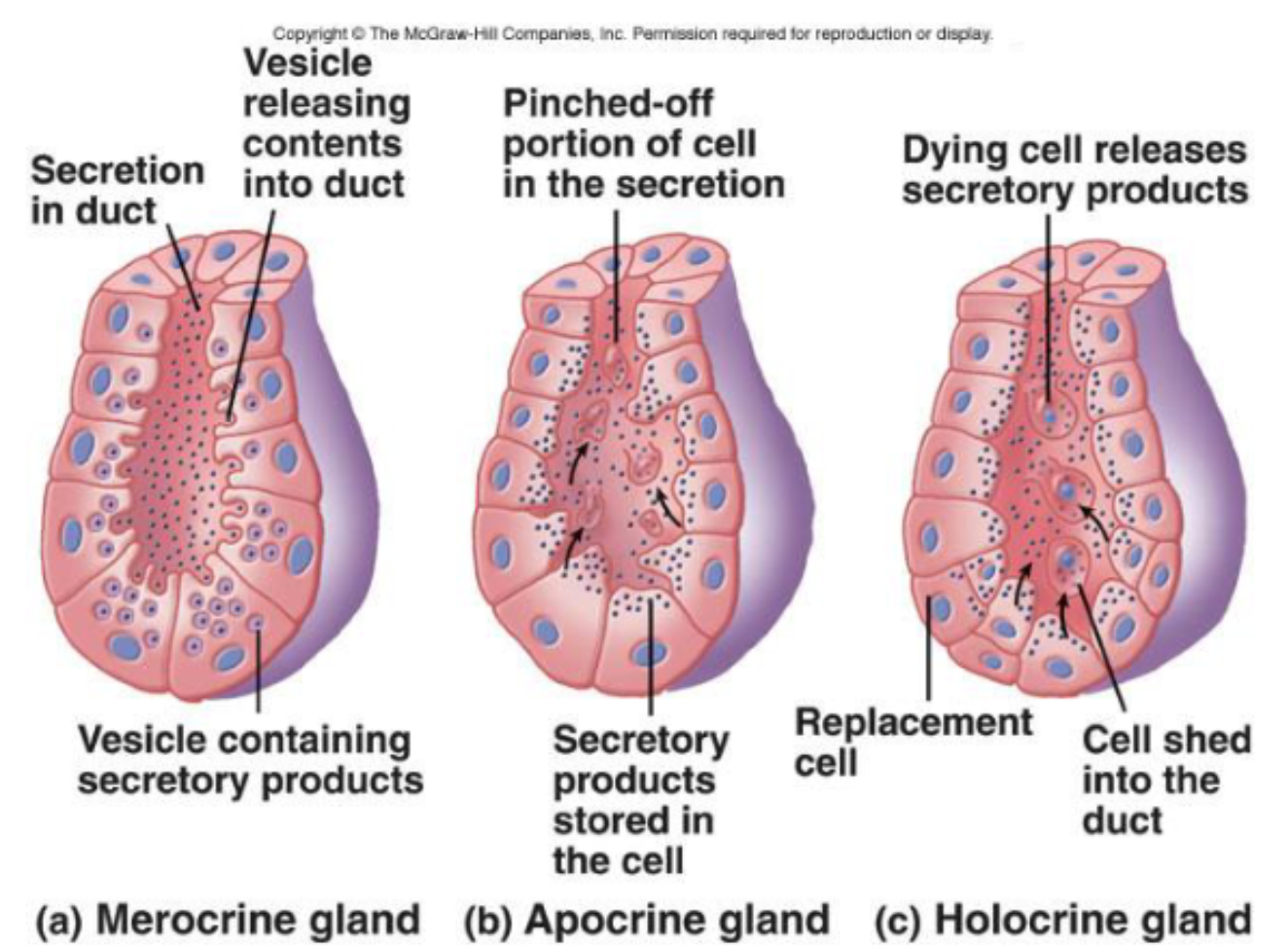
The cells of the secretory portion have three modes of secretion (or a combination). These three modes are merocrine, apocrine, and holocrine.
Merocrine glands secrete via exocytosis without altering secretory cell. It is the most common gland.
Apocrine glands accumulate products just beneath the free surface.
Top of the cell is removed, and products are released.
The cell is then repaired
Holocrine glands accumulate products until the cell bursts— releases secretory products, and then dies.
|