Horse examination:
ARTERIES to palpate:
Transverse Facial Artery
Location: Caudal to the lateral canthus of the left eye.
Technique:
Use three fingers to gently stroke the area until the vessel is found.
Count the pulse for 15 seconds and multiply by 4 to get beats per minute (BPM), or count for 10 seconds and multiply by 6.
Importance: This artery is a good site for measuring pulse rate.
Facial Artery
Location: Alongside the ventral aspect of the mandible.
Technique:
Place fingers on the ventral aspect and stabilize between the index and ring fingers.
Again, count pulse for the same durations (15 sec = x 4, or 10 sec = x 6).
Note: Another effective location for pulse rate measurement.
Lymph nodes in Horse:
1. Submandibular Lymph Nodes
Location: Just caudal to the facial artery.
Technique:
Use hands in the same direction as when palpating the facial artery.
Apply pressure dorsally while allowing the lymph nodes to slide laterally between the fingers.
Grab with fingers upwards
Observation:
Make sure that both lymph nodes are symmetrical and check for any abnormalities.
2. Retropharyngeal Lymph Nodes
Location: Under the dorsolateral edges of the larynx; intermandibular space at the angle of the mandibles.
Technique:
Place hands under the dorsolateral edges of the larynx and move over the larynx to reset hand position.
Move hands laterally into the intermandibular space to isolate lymph nodes.
Observation:
Check for symmetry and any abnormalities in the nodes.
3. Parotid Lymph Node
Location: Caudal to the ramus of the mandible, near the ear.
Technique:
Place fingers caudal to the ramus and move fingers upward towards the ear.
Observation:
Typically palpated muscular attachments or tenderness in this area.
The lymph node may be felt here, but it can vary by individual anatomy.

Pre-scapular lymph node
located under muscle, we do not feel it unless swollen, or enlarged.

Pre-femoral lymph node
we cannot feel it unless swollen/enlarged
CARDIOVASCULAR SYSTEM
Looking at mucous membranes - color, CRT, mandibular artery, jugular furrow - filling of jugular vein.
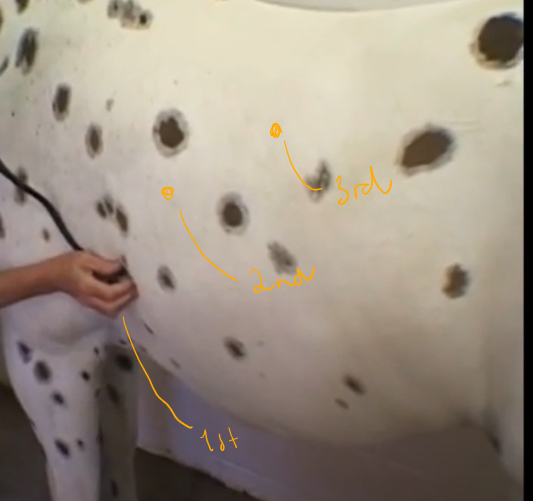
Landmarks:
Left side:
3rd ICS (at level of elbow) - pulmonic valve (furthest cranial)
4th ICS a little above - aortic valve
5th ICS - mitral valve
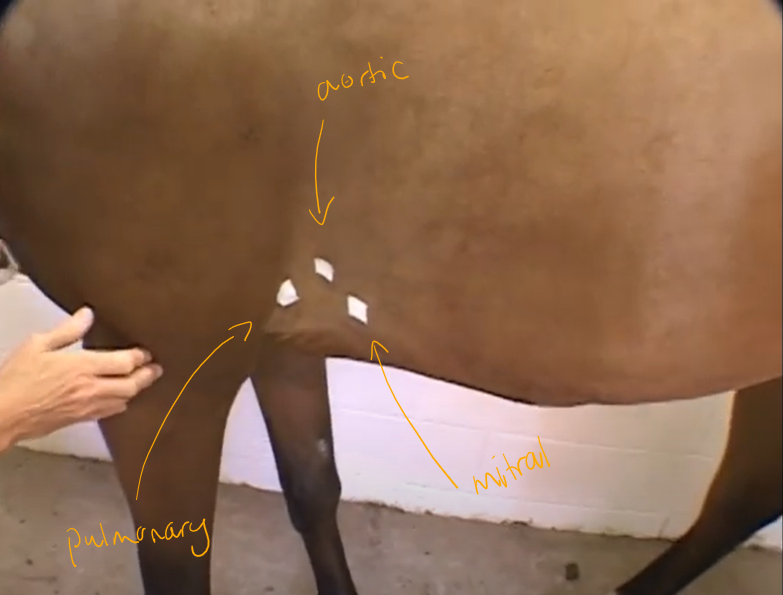

Right side:
tricuspid valve - at level just above elbow in armpit (3rd-4th ICS)

Rate
Rhythm
quality
Very much sound, volume of heart
A lot of physiological murmurs in horses!
The different heart sounds:
lub (S1)
dub (S2)
S3 + S4 (additional heart sounds, not as loud or intense) - but horses may have also these.
Most important is lub-dub sound!
RESPIRATORY EXAMINATION:
Looking at the effort of breathing, nostrils, overall thorax etc. Watch for nasal flaring, history.
Systematic Approach to Examination
Sequential Examination: Start from the front of the horse and move toward the back.
Nose Assessment:
Look for any nasal discharge or abnormal smells; certain infections may cause distinct odors.
Inspect nostrils for lumps or tumors using a finger or visual inspection.
Mucous Membranes:
Lift the upper lip to check color and refill time; a healthy horse should have pink membranes and normal capillary refill time (1-2 seconds).
Facial Examination
Symmetry is crucial; horses with sinus issues may present unilateral nasal discharge or facial asymmetry.
Percussion:
The technique is used to detect fluid or pus in sinuses by tapping on the skull and listening for dullness vs. hollow sounds.
Sinuses → tapping with fingers, getting hollow sounds
Palpation Steps
Check submandibular lymph nodes; swollen nodes can indicate respiratory infections.
Palpate larynx and thyroid gland; observation of any coughing or unusual lumps is critical.
Larynx → pinching, cranially to thyroid gland

Trachea Examination
Palpate the trachea and feel for the tracheal rings.
Important for procedures like tracheostomy, which is performed between specific tracheal rings.
Auscultation of the Respiratory System
Using the Stethoscope:
Proper orientation of earpieces - going forward from you.
Use the diaphragm side for furry animals.
Respiratory Rate Measurement:
Observe thoracic movement and abdominal muscle effort to gauge respiratory effort.
Count breaths via nostrils if necessary.
a lot of effort with abdominal muscles during breathing → can indicate allergic problems → problems with expiring the air
Auscultating:
auscultating trachea → breathing through pipe, if we hear anything wet → abnormal.
then proceed with lungs:
Techniques to Elicit Deep Breaths
Nostril Pinching: Encourages deep breathing for better sound assessment.
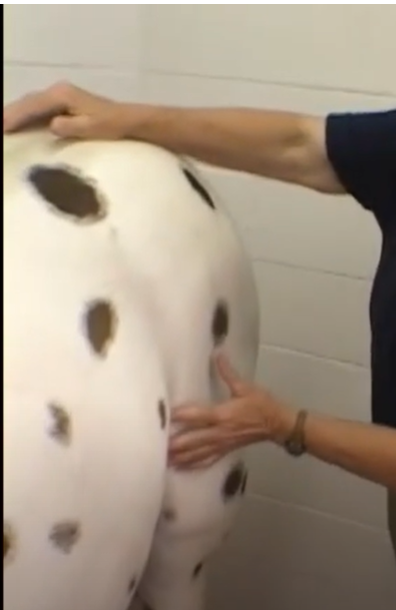
Rebreathing Bag: Using a large plastic bag to increase carbon dioxide and stimulate deeper breaths.
Additional Diagnostics
Other diagnostic techniques may include:
Transtracheal or Bronchoalveolar Lavage: Sampling fluid from the airways for testing.
Radiology: Useful for detecting issues in foals.
Ultrasound: Helps identify fluid in the chest.
Observing the horse during exercise may give insights into respiratory difficulties.