skeleton and bone tissues and types
Axial and Appendicular skeleton
The aging skeleton
Primary ossification centre is first place where bone forms
Secondary ossification is later forms
Function of the skeleton
Stability and movement
Supported by skeletal muscles and their attachments to both axial & appendicular skeleton
• Maintains posture to enable bodily functions
• Enables movement at joints by pulling the bone
Mineral storage
• Bone is made of organic and inorganic material
• Our body produces organic substances
>example: collagen fibres
• Receive inorganic substances from diet/development
>Minerals such as calcium & phosphorous
• Our body uses minerals for physiological & biochemical processes
• Example: calcium ions/electrolytes
• Signal transduction, neurotransmitter release, muscle contraction, protein synthesis, etc.
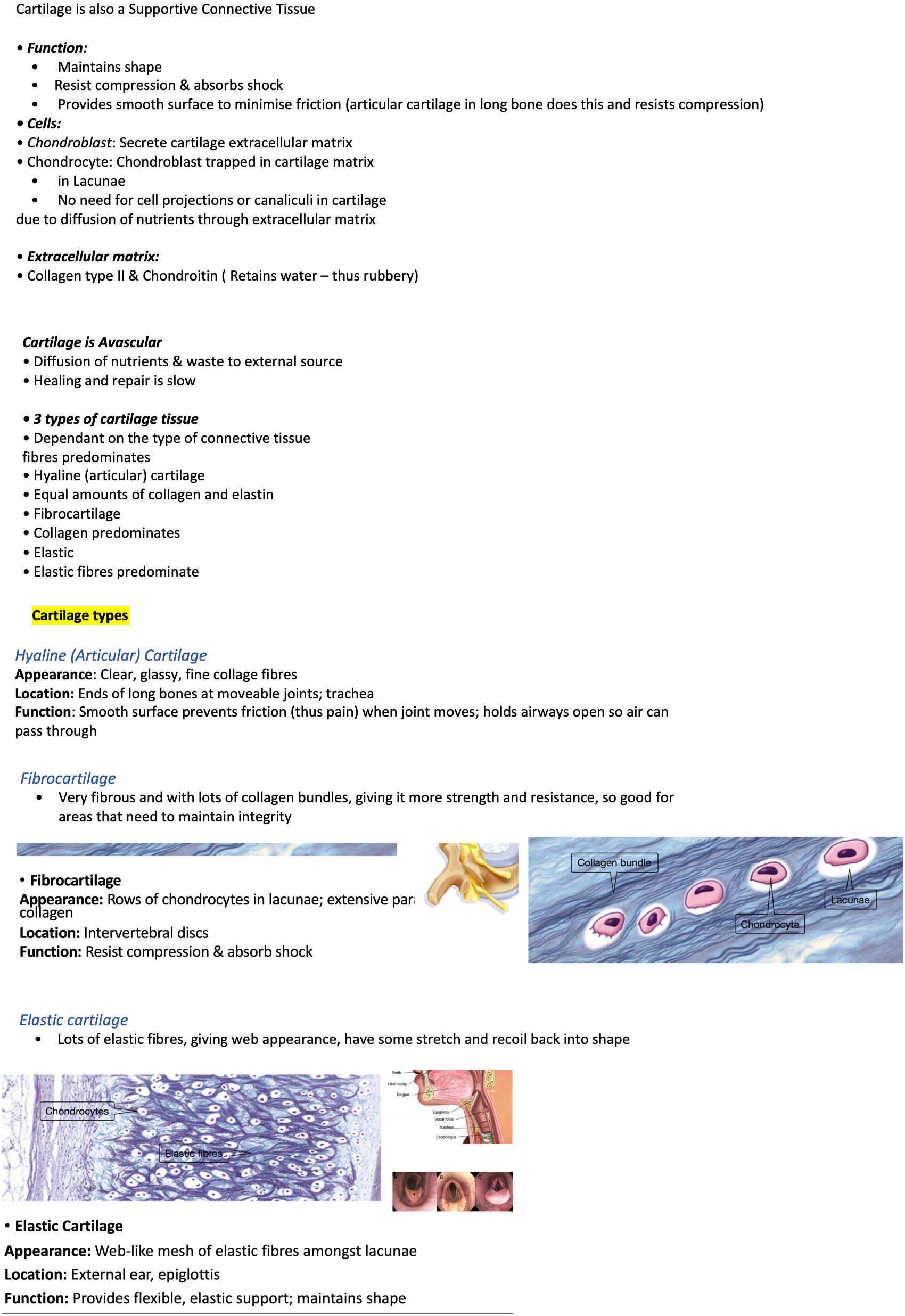
Blood Cell production and energy storage
Bone Marrow is a dynamic semi-solid tissue found within bone
Red Marrow: high number of haematopoietic stem cells (blood cell formation)
• Erythrocytes, monocytes, neutrophils, etc
• Located in spongy/trabecular bone, in ends of bones or flat bones
• Yellow Marrow: high number of adipocytes (fat cells) for energy/fat storage
> Located in medullary cavity of long bones
Bone types
Describes bone shape and not length
Long bones in arms or legs
Short bones mainly in wrist and hands or ankle
Skull bones and ribs/sternum are flat
Sesamoid bones form from within tendon, eg is patella
Irregular is vertebra
Long vs short bones
Flat, sesamoid and irregular bones
Osteology intro
Cortical vs trabecular bone (compact and spongey bone)
Compact (cortical) Bone = Outer edge of bone
• Prominent composition/type in diaphysis (shaft of long bone)
• Contains Osteons (how bone is built)
> Main unit of compact bone microstructure
• Strength in uniform direction due to being compact
Spongy (trabecular) Bone = Internal bone latticework that looks like sponge
• Prominent composition/type in heads of long bone & other bone structures (flat, irregular, etc)
• Contains Trabeculae (bony struts)
• Strength in multiple directions bc of latticework and space In/ around it, has red bone marrow which is essential for the making of blood cells (haematopoiesis)
Long bone vs others
Long bones =
share many common features
Irrespective of location as function is similar…
All assisst with Mobility!
Other bones =
Each Irregular, Short, Sesamoid, and Flat bone is unique…
Structure & features are based on location & function
No common features on the bone
Macroscopic appearance of bone and their functions
Bone Surface Features
• Rough areas, elevations, processes, grooves, depressions & openings
Provide a Functional Purpose
• Site of attachments
> Tendons/Muscles, Ligaments (stabilise a joint), Joint Capsule (structure that surrounds a whole joint)
• Articular surfaces
>Joint architecture determines movement
• Passageway for nerves & vessels
Gross anatomy of the long bone
Diaphysis = Shaft/ hollow structure
• Made of Cortical (compact) bone
Epiphysis = Ends of bone
• Contains Trabecular (spongy) bone
>epiphysial line if an adult and become bone or a plate that is made of cartilage if person is till growing
Metaphysis = Between Epiphysis & Diaphysis
• Contains Trabecular (spongy) bone
Medullary Cavity = Marrow cavity in diaphysis
>hollow except for yellow bone marrow where fat and energy is stored
Articular Cartilage = Covers epiphyses
• Smooth frictionless movement at joint
Fibrous tissues/membranes that cover the inside or outside of the bone
Periosteum only surrounds the actual bone not the joint, and will end where the articular cartilage begins (this cartilage allows for smooth frictionless joint)
Bone as a connective tissue
Bone is continuously changing, it is strong and semi-rigid in order to hold us and maintain our structure, but also be flexible and have some bend (as a result of fibres)
Suppourtive connective tissues
Bone is a supportive connective tissue
Supportive Connective Tissue = provide structural strength and protect soft tissue; few distinct cell types with densely packed fibres
• Bone – matrix is rigid & calcified (deposition of calcium mineral salts)
• Cartilage – matrix is firm but gelatinous (deposition of chondroitin polysaccharides)
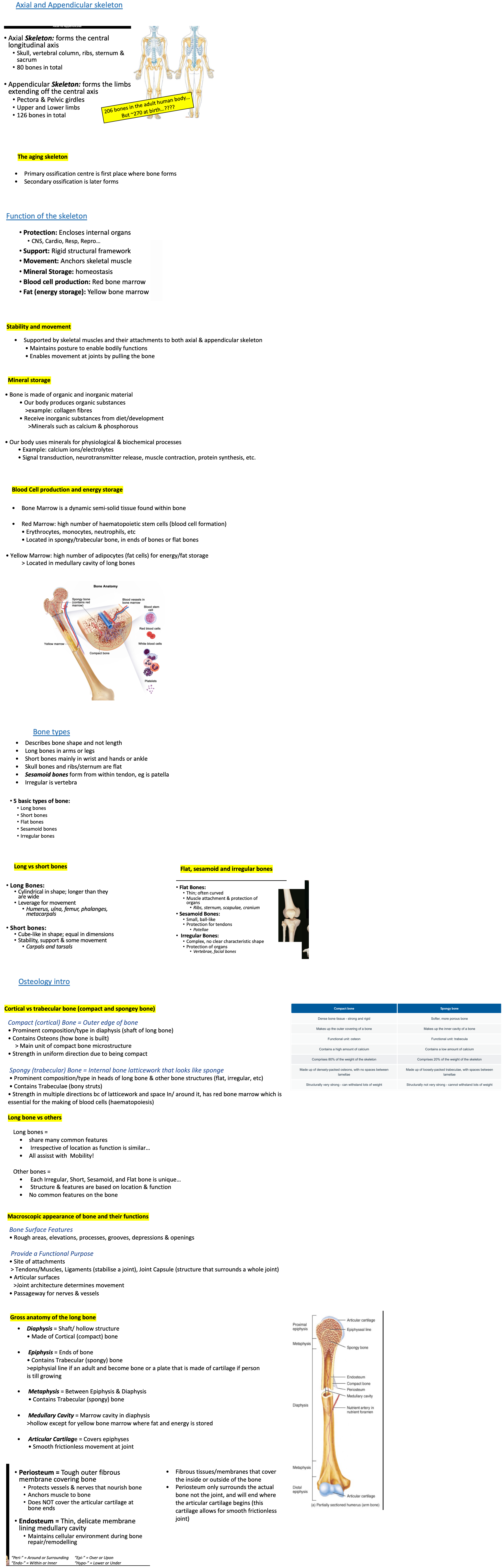
Bone tissue
Bone is a Supportive Connective Tissue
• Cells: Osteoprogenitor, Osteoblasts, Osteocytes & Osteoclasts
• Extracellular matrix:
> Organic components (material cells are making) = Collagen fibres
> Inorganic components (body/ DNA doesn’t create or code for, get them thru diet) = Mineral salts, make bone hard
Bone extracellular matrix
Organic components (osteoid):
• Synthesized and secreted by Osteoblasts (secretes material for basic soft model of bone)
Collagen type I
Inorganic Matter:
• Harvested from surrounding blood
• Calcium and Phosphorous Mineral Salts
Mineralization (Calcification):
• Hardening of bone extracellular matrix from the soft bone formed by osteoblasts
• Mineral salts bind to collagen, forming crystals that make bones physically hard
Bone cells
The first THREE cells are from one bone cell that grows over time (one cell lineage)
Osteoprogenitor Cell (osteogenic cell)
• Mesenchymal stem cell ( stem cell means cell that has the ability to turn into something else, mesenchymal means it has ability to turn into 3 distinct pathways, either bone, fat (adipocyte) or chondrocyte in cartilage)
• Only bone cell to undergo mitosis (i.e. divide) meaning it has being relied on to keep replenishing bone cells
• Some will become osteoblasts (a process called differentiation)
• Location: lines the surface/edges of bone
• Under Periosteum & Endosteum
Osteoblast
• Bone forming cell, after osteoprogenitor cells have received signal
• Synthesises and deposits the organic bone matrix (collagen fibres)
• Initiates calcification – impregnation of inorganic substances into bone matrix (hardens bone)
• Become (differentiate) osteocytes when encased/trapped in own bone deposits and needs branches to go through crystal matrices in bone to get nutrients
• Location: lines the surface/edges of bone, like osteoprogenitor cell
• Under Periosteum & Endosteum
Osteocyte
• Maintain bone microenvironment
• Delicate cellular projections (fingers) create a sensory network through bone matrix
• Regulate other bone cells
• Location:
• Cell Body = inside small cavities in bone (Lacunae) that were made when the bone was being formed
• Cellular Projections = travel through small canals (Canaliculi) that are extension of cells cytoplasm
Osteoclast
• Differentiate from haematopoietic stem cell (NOT from the same family as the previous 3 bone cells) as they are white blood cells
• Fusion of monocyte/macrophage type cells that come together to make a giant macrophage, that when told to live on a bone becomes an osteoclast
• Large multinucleated cell as it forms from many cells coming together with ruffled basal surface
• Creates a suction (sealing zone) to attach to bone to break down bone matrix (i.e. Resorption)
• Releases lysosomal enzymes and acids
• Location: Edge of bone in resorption pits
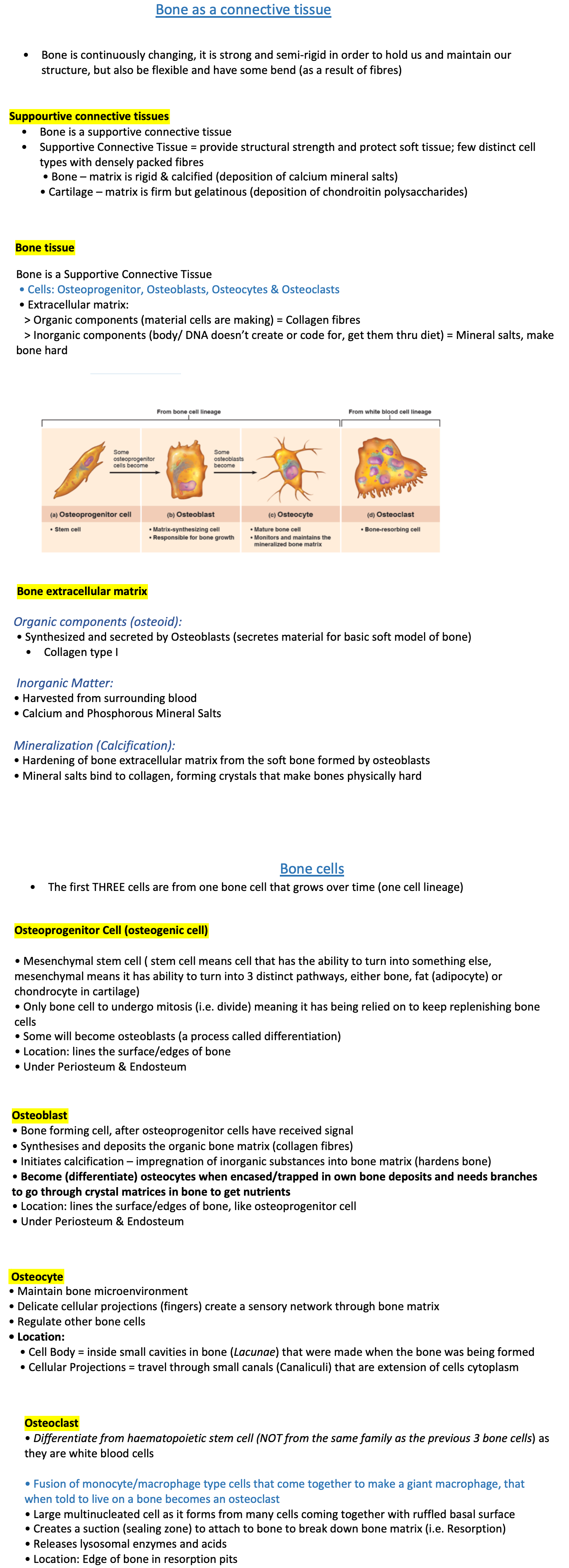
Osteon Components (A.K.A. Haversian System) from compact bone
Osteons are vertical tube-like bony constructs arranged in parallel
• You will ONLY find Osteons in Compact Bone
• Compact bone is a construct of multiple osteons
Each Osteon contains:
• Haversian (central) canal
A single canal for vessels
Supply of nutrients/removal of waste for bone cells
• Concentric Lamellae
‘Layers’ of bone ‘rings’ around the Haversian canal
• Lacunae
Cavities in lamellae containing the osteocyte cell body
• Canaliculi
Canals through lamellae containing osteocyte cellular
Compact bone also contain:
• Volkmann's canals – ‘Horizontal’ canals for vessels connecting adjacent osteons for carrying nutrients and waste
• Interstitial lamellae – Old osteons no longer containing a Haversian canal
> No longer layered around a central canal
> You will find only ‘interstitial lamellae’ in spongy/trabecular bone
How osteons form
Osteons are created during the process of bone formation and maintained or updated during the bone remodelling process
Starts with Vessels (blood and lymph), nerves
Osteoblasts come to the area around vessels due to growth factor being released into the local environment
Osteoblasts begin to lay down bone
Osteoblasts lay down more bone…Osteoblasts lay down so much bone they trap themselves in small cavities The small cavity is called a Lacunae THEN Osteoblasts now must differentiate into Osteocytes to survive
Osteoclasts exit the blood stream and resorb (remove) bone around vessel = Forms the Central / Haversian canal
An Osteoblast enters the Harversian Canal and fills in a single ring/layer of bone (lamellae)
Another Osteoblast creates another layer of bone within Haversian Canal (Concentric lamellae) Old osteoblast trapped in ‘Lacunae’ differentiates to form Osteocyte
Osteoblasts lay down so much bone they trap themselves in small cavities The small cavity is called a Lacunae -> Osteoblasts now must differentiate into Osteocytes to survive
Osteocyte projections form and tunnel through the bone to receive nutrients, remove wastes & communicate = Canals in bone are “Canaliculi”
Trabeculae (main functional unit of spongey bone)
Trabeculae is found in spongey/ trabecular bone, in the heads of bones
• Trabeculae are individual “strut” like bony units
• Spongy (i.e. Trabecular) bone is a latticework of
trabeculae
• You will ONLY find trabeculae in spongy bone (as cortical bone is too dense with no space for struts)
• Each Trabeculae contains:
Lamella (layers of bone) arranged in plates or sheets
Much like interstitial lamella
Lacunae & Canaliculi for osteocytes
• Trabeculae do NOT have
Concentric lamella (layered rings of bone)
A Haversian (central) canal as the cells can grab on the blood vessels from the surrounding area
Bone cell nutrition
Osteoprogenitors, Osteoblasts and Osteoclasts
• Located at edge of bone
• Diffusion of nutrients from local fluid Environment
• Osteocytes
• Located in lacunae (encased in solid bone matrix)
• Nutrients do NOT diffuse through calcified matrix
• Delicate Osteocytes projections travel through canals in bone (canaliculi) connecting with blood vessels outside of bone (red bone
marrow) or within the Haversian (central) canal
Cartilage is also a Supportive Connective Tissue
• Function:
Maintains shape
Resist compression & absorbs shock
Provides smooth surface to minimise friction (articular cartilage in long bone does this and resists compression)
• Cells:
• Chondroblast: Secrete cartilage extracellular matrix
• Chondrocyte: Chondroblast trapped in cartilage matrix
in Lacunae
No need for cell projections or canaliculi in cartilage
due to diffusion of nutrients through extracellular matrix
• Extracellular matrix:
• Collagen type II & Chondroitin ( Retains water – thus rubbery)
Cartilage is Avascular
• Diffusion of nutrients & waste to external source
• Healing and repair is slow
• 3 types of cartilage tissue
• Dependant on the type of connective tissue
fibres predominates
• Hyaline (articular) cartilage
• Equal amounts of collagen and elastin
• Fibrocartilage
• Collagen predominates
• Elastic
• Elastic fibres predominate
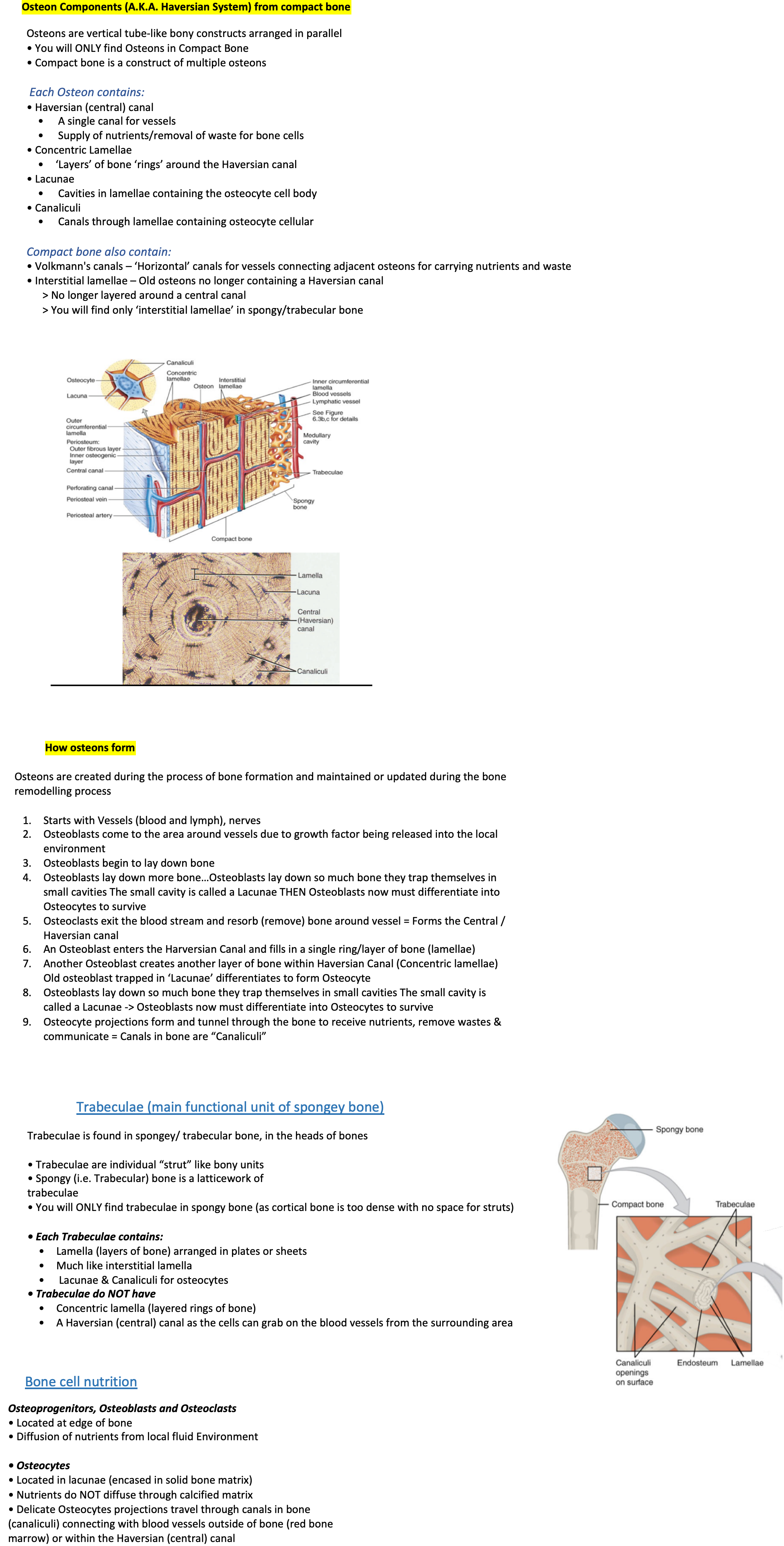
Cartilage types
Hyaline (Articular) Cartilage
Appearance: Clear, glassy, fine collage fibres
Location: Ends of long bones at moveable joints; trachea
Function: Smooth surface prevents friction (thus pain) when joint moves; holds airways open so air can pass through
Fibrocartilage
Very fibrous and with lots of collagen bundles, giving it more strength and resistance, so good for areas that need to maintain integrity
Elastic cartilage
Lots of elastic fibres, giving web appearance, have some stretch and recoil back into shape