Sciences of infection and disease
Introduction
Main cells of the immune system, their role and location
Cell type | Main role | Location |
Polymorphonuclear eosinophils | Release toxins that can kill bacteria and parasites | Blood vessels and can migrate to tissue during infection |
Polymorphonuclear neutrophils | Ingest and kill microorganisms (mainly bacteria and fungi). First responders at the site of infection. Release molecules that attract other immune cells at the site of infection | Blood vessels and can migrate to tissue during infection |
Polymorphonuclear basophils | Defence against parasites. Release molecules that can participate to the expulsion of an extracellular parasite | Blood vessels and can migrate to tissue during infection |
Mast cells | Release molecules involved into the destruction of pathogens | Connective tissue, mucous membranes |
Monocytes | Phagocytic cells that can engulf pathogens and cells and later differentiate into macrophages once they have left the blood circulation and entered a tissue | Blood vessels and can migrate to tissue during infection |
Macrophages | Phagocytic cells that can engulf pathogens and release molecules stimulating other immune cells | Migrate from blood vessels into infected tissues |
T-lymphocytes (Helper)/CD4 T helper cells | Specialised T-lymphocytes helping other T and B-cells perform their functions by interacting directly with them or releasing soluble molecules. Express CD4 antigen | Blood vessels and can migrate to tissue during infection |
T-lymphocytes (Suppressor) | Specialised T-lymphocytes (also called regulatory T-cells) that suppress various cellular and humoral mechanisms of the immune response. Express CD4 antigen | Blood vessels and can migrate to tissue during infection |
Cytotoxic T-lymphocytes/CD8 Cytotoxic T-cells | Kill infected cells. Express CD8 antigen | Blood vessels and can migrate to tissue during infection |
B-lymphocyte | Sub-type of lymphocyte that can present foreign antigens to other immune cells, secrete soluble molecules and produce antibodies when differentiated | Blood vessels and can migrate to tissue during infection |
Plasma cell | Differentiated B-lymphocytes that produce antibodies | Blood vessels and can migrate to tissue during infection |
Natural killer cells | Kill mainly virus-infected cells | Blood vessels and can migrate to tissue during infection |
Dendritic cells | Initiate antigen-specific immune responses | Resident cells of the skin, lung and digestive tract. Migrate to lymph nodes after activation by a pathogen |
Main notifiable infectious diseases affecting Australians from 2009–19
Gastrointestinal Infections
Campylobacteriosis — A common bacterial infection caused by Campylobacter bacteria, often transmitted through contaminated food, especially poultry.
Listeriosis — A serious bacterial infection caused by Listeria monocytogenes bacteria, often found in contaminated food, such as soft cheeses and deli meats
Paratyphoid — A bacterial infection caused by Salmonella paratyphi bacteria, similar to typhoid fever but often milder.
Salmonellosis — A bacterial infection caused by Salmonella bacteria, often transmitted through contaminated food or water.
Shigellosis — A bacterial infection caused by Shigella bacteria, often spread through contaminated food or water, or by person-to-person contact.
STEC (Shiga toxin-producing Escherichia coli) — A strain of E. coli bacteria that produces toxins that can damage the intestines.
Typhoid fever — A severe bacterial infection caused by Salmonella typhi bacteria, often transmitted through contaminated food or water.
Cryptosporidiosis — A parasitic infection caused by Cryptosporidium protozoa, often transmitted through contaminated water.
Rotavirus — A viral infection that affects the intestines, often causing severe diarrhea in infants and young children.
Hepatitis A — A viral infection that affects the liver, often transmitted through contaminated food or water.
Respiratory Infections
Legionellosis — A bacterial infection caused by Legionella bacteria, often found in contaminated water sources, such as hot tubs, air conditioning systems, and cooling towers.
Meningococcal disease (invasive) — A bacterial infection that can cause meningitis (inflammation of the lining of the brain and spinal cord) and septicemia (blood poisoning).
Tuberculosis — A bacterial infection that affects the lungs and other organs.
Haemophilus influenzae type b — A bacterial infection that can cause meningitis, pneumonia, and other serious illnesses, especially in young children.
Pertussis — A bacterial infection that causes whooping cough, a severe respiratory illness that can be fatal in infants.
Pneumococcal disease (invasive) — A bacterial infection that can cause pneumonia, meningitis, and other serious illnesses.
Influenza (laboratory confirmed) — A viral infection that causes flu, characterized by fever, cough, sore throat, and other symptoms.
Measles — A highly contagious viral infection that can cause fever, rash, and other symptoms.
Mumps — A viral infection that causes swelling of the parotid glands (located near the ears).
Rubella — A viral infection that can cause rash, fever, and joint pain.
Varicella zoster (chicken pox) — A viral infection that causes a rash and blisters.
Sexually Transmitted Infections (STIs)
Chlamydial infection — A bacterial infection caused by Chlamydia trachomatis, often asymptomatic in women but can lead to pelvic inflammatory disease.
Gonococcal infection — A bacterial infection caused by Neisseria gonorrhoeae, often asymptomatic in men but can lead to pelvic inflammatory disease in women.
Syphilis — A bacterial infection caused by Treponema pallidum, characterized by a chancre sore at the site of infection, followed by a rash and other symptoms.
Hepatitis B (newly acquired) — A viral infection that affects the liver, transmitted through blood or bodily fluids.
Hepatitis C (newly acquired) — A viral infection that affects the liver, transmitted through blood or bodily fluids.
Vector-Borne Infections
Dengue virus infection — A viral infection that can cause fever, rash, and other symptoms.
Flavivirus infection (unspecified) — A general term for a group of viruses that includes dengue, Zika, and West Nile viruses.
Ross River virus infection — A viral infection that can cause fever, rash, joint pain, and fatigue.
Malaria — A parasitic infection caused by Plasmodium parasites, transmitted by infected mosquitoes.
Barmah Forest virus infection — A viral infection that can cause fever, rash, joint pain, and fatigue.
Zoonotic Infections (transmitted from animals to humans)
Brucellosis — A bacterial infection caused by Brucella bacteria, often transmitted through contact with infected animals or their products, such as milk or meat.
Leptospirosis — A bacterial infection caused by Leptospira bacteria, often transmitted through contact with infected animals or their urine.
Ornithosis — A viral infection caused by Chlamydia psittaci bacteria, often transmitted through contact with infected birds, particularly parrots and parakeets.
Q fever — A bacterial infection caused by Coxiella burnetii bacteria, often transmitted through inhalation of airborne bacteria or through contact with infected animals or their products.
Pathogenic Microorganism
Microorganisms are unicellular organisms that are too small to be seen by the naked eye. They can be prokaryotic (simpler cells) or eukaryotic (more complex cells).
Pathogenic microorganisms can cause infections in humans and animals.
Prokaryotic cells — Bacteria and archaea. Only bacteria are known to cause human infections.
Eukaryotic cells — Fungi and protozoa.
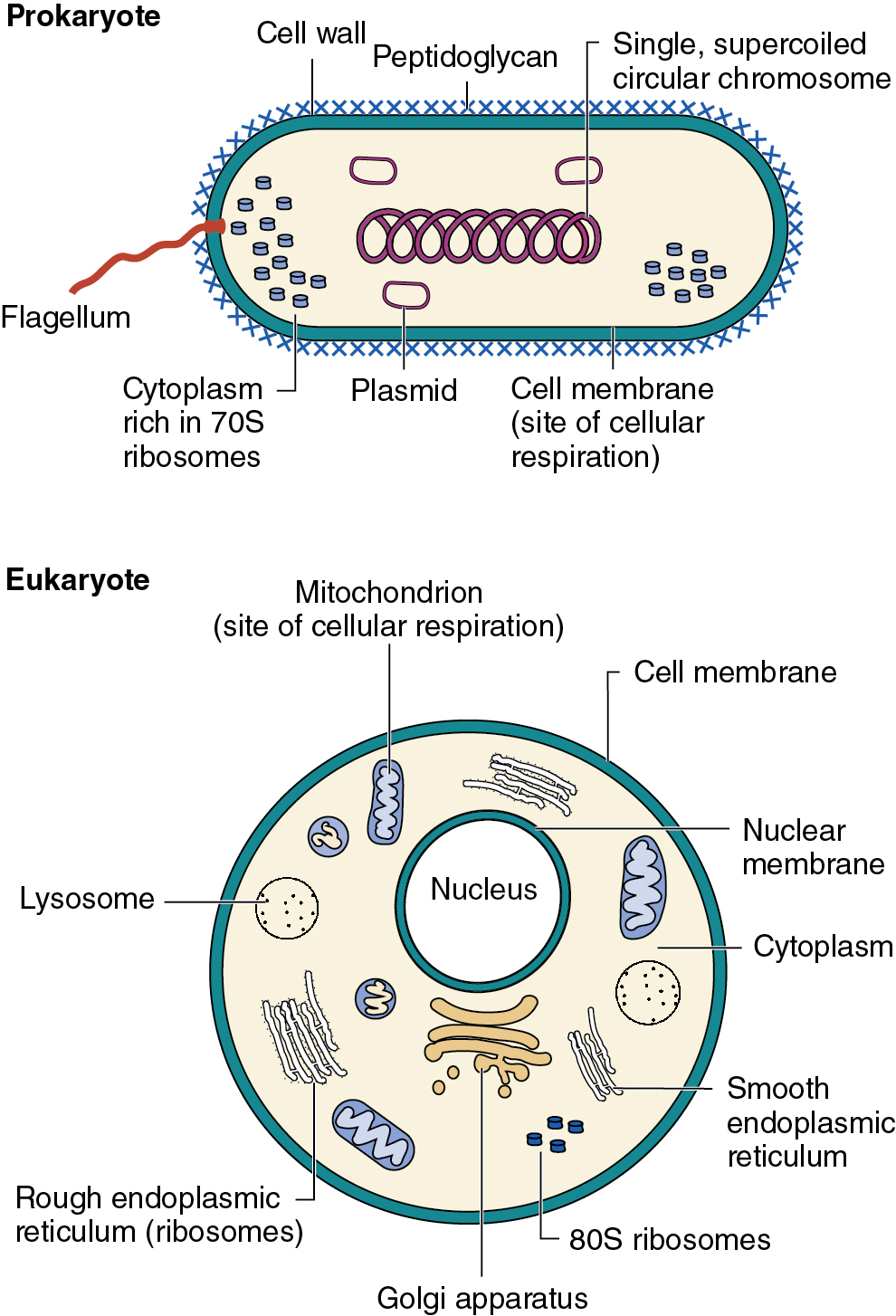
Prokaryotic cellular pathogens
Bacteria have diverse shapes, with bacillus (rod-shaped) and coccus (sphere-shaped) being most common.
Gram staining — a laboratory technique used to differentiate bacteria based on their cell wall structure.
Gram-positive bacteria stain purple due to a thick cell wall.
Gram-negative bacteria stain pink due to a thin cell wall.
Cell Wall — a rigid layer outside the cell membrane that provides structural support, protection, and shape to bacterial cells.
It is a key structural component for gram staining, but some bacteria, like Mycoplasma and Chlamydia, lack it.
Mycobacteria have a modified cell wall with mycolic acids.
Bacterial ribosomes are smaller (70S) than eukaryotic ribosomes (80S).
Bacteria have various structures and factors that contribute to their ability to cause disease.
Some bacteria can form spores, which are highly resistant dormant structures.
Bacterial structures important for virulence:
Capsule: Protects bacteria from the immune system.
Fimbriae and pili: Adhere to host cells.
Flagella: Enable movement.
Endotoxins: Released by Gram-negative bacteria when they die.
Exotoxins: Secreted by bacteria.
Examples of Spore Formers:
Bacillus anthracis (anthrax)
Clostridium tetani (tetanus)
Clostridium botulinum (botulism)
Sub-cellular structures in bacteria important for survival and virulence
Structure | Details | Function(s) |
Membrane and surface-associated structures | ||
Fimbriae | Short hair-like appendage extending from the cell surface |
|
Pilus | Short appendage extending from the cell surface |
|
Flagellum | Thread-like appendage extending from the cell surface |
|
Capsule/slime layer | Made up of polymeric substances such as polysaccharide and found on the cell surface. A capsule is tightly adhered to the cell surface, whereas slime layers are easily washed off |
|
Lipopolysaccharide (LPS) | Found only in Gram-negative bacteria, LPS extends from the cell surface. Consists of a lipid portion (lipid A) embedded in the outer membrane connected to a variable polysaccharide component called the O antigen |
|
Teichoic acids | Found only in some Gram-positive bacteria, teichoic acids are a phosphorylated polyalcohol present in the cell wall |
|
Cell wall | Rigid peptidoglycan structure positioned outside the bacterial plasma membrane |
|
Internal structures | ||
Plasmid | Small, circular DNA that replicates independently of the bacterial chromosome |
|
Spores | Highly resistant dormant structure produced by some Gram-positive bacteria |
|
Eukaryotic Cellular Pathogens
Eukaryotic microorganisms are more complex than prokaryotic microorganisms, with various organelles performing specific functions.
Key Organelles:
Mitochondria: Produce energy (ATP).
Endoplasmic Reticulum (ER): Synthesizes and modifies cellular products (lipids, proteins).
Golgi Apparatus: Transports ER-produced products.
Lysosome: Digests cellular waste.
Some eukaryotic microorganisms have flagella (long, whip-like structures) or cilia (shorter, hair-like structures) for movement.
Fungi — can be unicellular (yeast) or multicellular (molds).
Some are dimorphic, changing between yeast and mold forms.
Example: Blastomyces dermatitidis
Protozoa — unicellular eukaryotes that feed on organic material.
Many can form cysts for survival and transmission between hosts.
Trophozoite — the active, feeding stage of a protozoan parasite.
It's the form that the parasite takes when it's actively growing and reproducing.
Often the stage that causes disease in the host.
Encystment — the process by which a trophozoite transforms into a cyst.
Cyst — a dormant, resistant form of the parasite.
Cysts have a thick wall that protects them from harsh environmental conditions.
Encystment allows the parasite to survive outside of a host, making it easier for it to spread to new hosts.
Excystment — the process by which a cyst transforms back into a trophozoite.
It occurs when the cyst finds itself in a favorable environment, such as inside a new host.
This allows the parasite to resume its active, feeding stage and reproduce.
Examples:
Plasmodium (malaria)
Trypanosoma (trypanosomiasis)
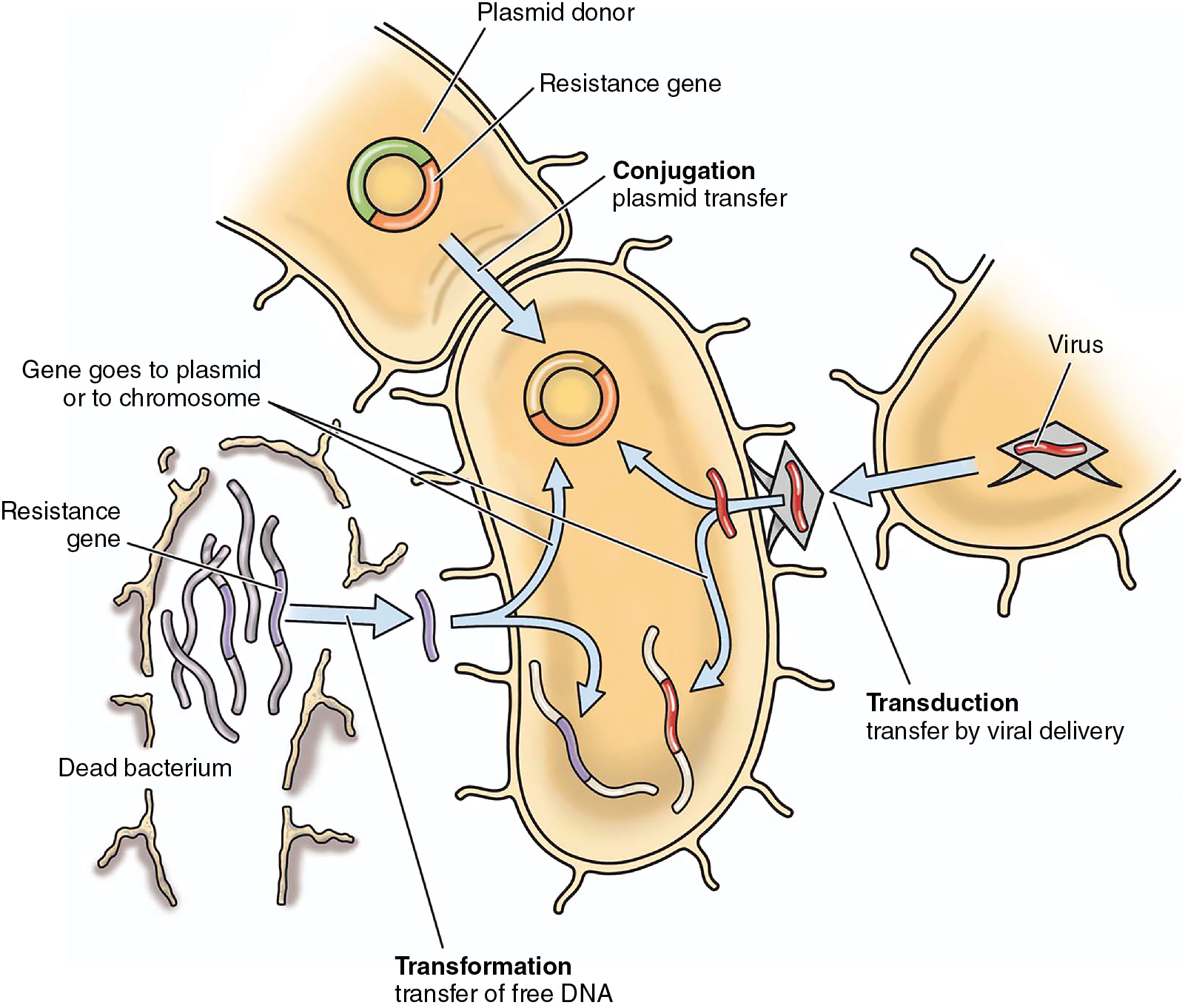
Horizontal gene transfer in bacteria
Horizontal Gene Transfer (HGT) — the process by which bacteria share DNA, contributing to the emergence of problematic pathogens and antibiotic-resistant strains.
Three mechanisms of HGT:
Conjugation — Requires cell-to-cell contact and a pilus for DNA transfer.
This involves the transfer of genetic material between two bacteria that are in physical contact. A specialized structure called a pilus connects the two bacteria, and DNA, often in the form of a plasmid, is transferred from one bacterium to the other.
It is a highly efficient way for bacteria to acquire new genes, including those that confer resistance to antibiotics or other antimicrobial agents.
Transformation — Uptake of naked DNA by competent bacteria.
This involves the uptake of free DNA from the environment. Bacteria that are competent, meaning they are in a physiological state that allows them to take up DNA, can undergo transformation.
It can be a way for bacteria to acquire genes that are beneficial for their survival, such as those that allow them to metabolize new nutrients or resist environmental stresses.
Transduction — Transfer of DNA by a bacteriophage (bacterial virus).
This involves the transfer of DNA from one bacterium to another by a bacteriophage, a virus that infects bacteria. The bacteriophage packages bacterial DNA into its capsid and can then transfer it to another bacterium when it infects it.
It can be a way for bacteria to acquire genes that they would not be able to obtain through conjugation or transformation.
Transferred DNA must integrate into the chromosome or a plasmid to be replicated and passed on to progeny.
Homologous recombination is a common method of integration.
It is a cellular process that involves the exchange of genetic material between two similar DNA sequences.
It is often used by bacteria to integrate transferred DNA into their chromosome. This allows the transferred genes to be replicated and passed on to the bacterium's offspring.
Antibiotic resistance is often due to horizontally acquired genetic elements.
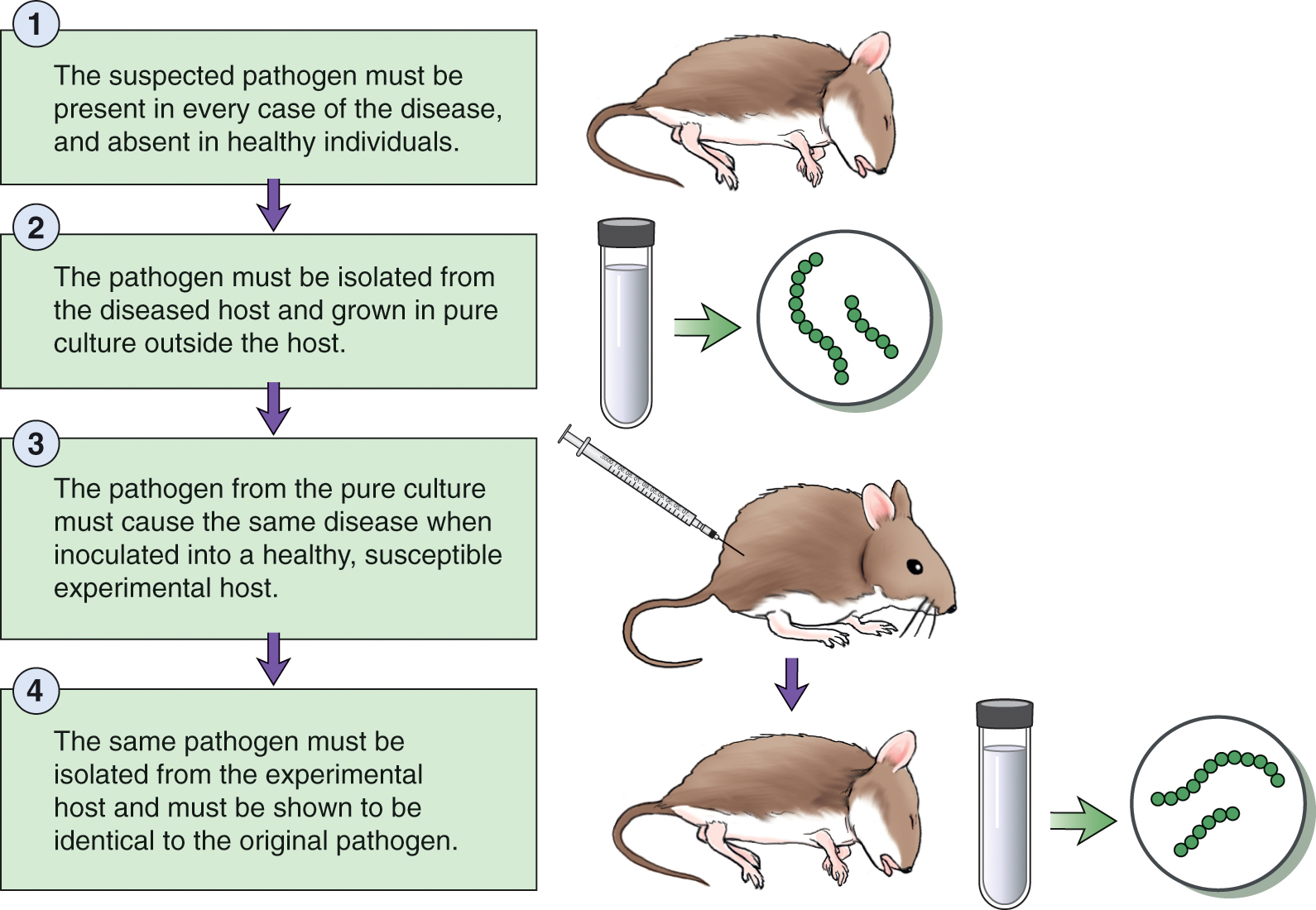
Koch’s Postulate
Koch's Postulates are a set of criteria used to establish a causal link between a pathogen and a disease. They require:
Isolation: The pathogen must be isolated from the diseased host.
Culture: The pathogen must be cultured in a laboratory.
Infection: The pathogen must be able to infect a healthy host.
Re-isolation: The pathogen must be re-isolated from the newly infected host.
Limitations of Koch's Postulates:
Culturability: Some pathogens may be difficult or impossible to culture.
Host Models: Suitable animal models may not be available for all diseases.
Complex Diseases: Some diseases are caused by multiple pathogens or factors.
Opportunistic Infections: Some pathogens only cause disease when the host's microbiome or immune system is compromised.
Modern Research:
Tracking Pathogens: Techniques like PCR and sequencing can track pathogens without the need for culture or animal models.
Host Factors: Research focuses on how host factors, such as the microbiome and immune system, influence susceptibility to and severity of infectious diseases.
Microbiomes
Microbiome — A community of microorganisms found in a particular environment.
Human Microbiome — The collective of microorganisms found on and in the human body, including skin, gastrointestinal tract, nose, mouth, and vagina.
Importance of the Human Microbiome:
Digestion: Aids in digestion of nutrients.
Vitamin Synthesis: Produces vitamins.
Protection: Protects against pathogens.
Immune Regulation: Stimulates and regulates the immune system.
Microbiome Composition:
High Diversity: The human microbiome contains a vast array of microorganisms.
Colon: The colon has a particularly high concentration of bacteria (10^11-10^12 per gram).
Dysbiosis: Imbalances in microbiome composition are linked to various gastrointestinal conditions.
Studying the Microbiome:
Metagenomic DNA: DNA extracted from an environment (e.g., feces) is analyzed to identify the composition of microorganisms and their genes.
Disease Correlation: Comparisons between healthy and diseased samples help identify microorganisms or genes associated with disease.
Challenges: Substantial inter-individual variation makes identifying trends difficult.
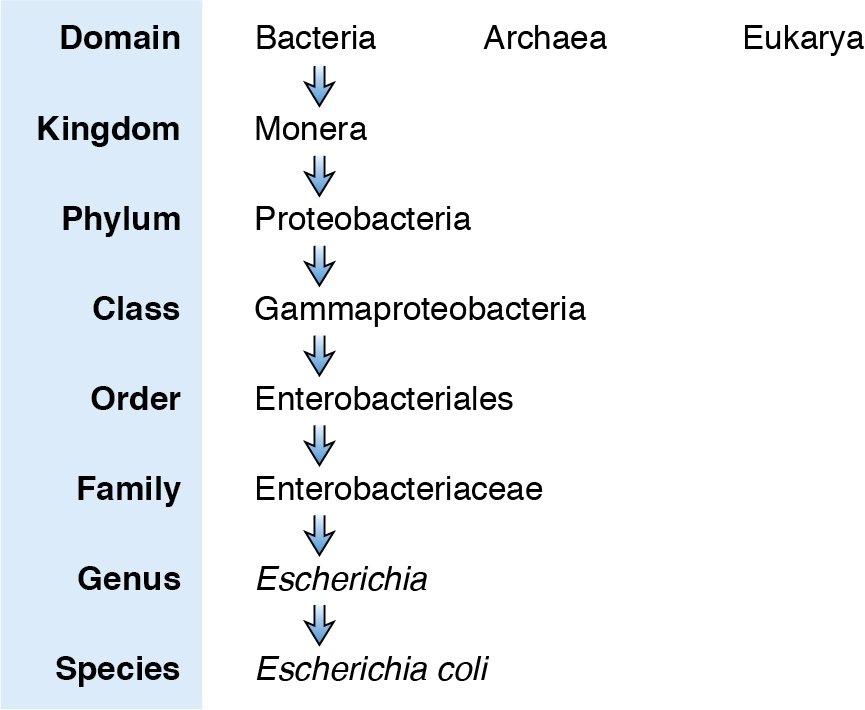
Taxonomy of microorganisms
Taxonomy — the classification and naming of organisms.
Microorganisms — These classified into groups based on shared characteristics, which helps in understanding and addressing them (e.g., prescribing treatments, quarantine).
Historical Classification: Phenotypic characteristics (e.g., morphology, metabolism) were used.
Modern Classification: Genetic-based methods compare SSU rRNA sequences to determine phylogenetic relationships.
Classification Levels:
Three Domains of Life:
Archaea — These are prokaryotesthat are distinct from bacteria.
They are often found in extreme environments, such as hot springs, salt lakes, and deep-sea vents.
They have unique cell walls and ribosomes that differentiate them from bacteria and eukaryotes.
Bacteria — They are found in a wide variety of environments, including the human body, soil, water, and air.
They can be both beneficial and harmful.
Eukarya — These are organisms with cells that contain a nucleus and other membrane-bound organelles.
This domain includes animals, plants, fungi, and protists.
They are generally more complex than prokaryotes and have a greater diversity of cell structures and functions.
Binomial Naming System — also known as scientific nomenclature, is a standardized way of naming organisms.
This was developed by Carl Linnaeus in the 18th century.
Each organism is given a unique two-word name. The first word is the genus name, which is capitalized. The second word is the species name, which is lowercase. For example, the scientific name for humans is Homo sapiens.
Strain: Microorganisms within a species with different phenotypic characteristics, often due to HGT.
Core Genome and Pan Genome:
Core Genome: Genes shared by all strains within a species.
Pan Genome: Genes that are uncommon and often acquired through HGT.
Pathogenic Biological Particles
Viruses
Viruses — are pathogens responsible for pandemics like influenza, COVID-19, and AIDS.
Size: Very small (20-400 nm).
Virion — A single viral particle consisting of a nucleocapsid (nucleic acid surrounded by a protein coat).
Capsid — Protects the nucleic acid and aids in host cell adhesion.
Envelope: Many viruses have a membrane envelope acquired from the host cell.
Nucleic Acid: Can be DNA (double-stranded or single-stranded) or RNA (double-stranded or single-stranded).
Taxonomy: Based on virion structure, nucleic acid type, replication mode, host range, and disease caused.
Prions
Prions — are infective proteins linked to neurodegenerative diseases.
Prions are transmissible spongiform encephalopathies (TSEs) due to their effect on the brain resulting in a spongy appearance when brain slices are observed histologically.
Transmission: Spread through consumption of contaminated meat.
Pathology: Take years to develop after exposure.
Resistance: Highly resistant to standard infection control methods.
Examples: Kuru, vCJD, BSE, scrapie.
Multicellular parasites
Helminths
Helminths — are wormlike macroparasites. Also known as parasitic worms.
Common in regions with poor sanitation and limited access to clean water.
Intestinal infestations: Often cause diarrhea and other gut symptoms.
Serious complications: Can migrate to other organs, causing more severe issues.
Nutrition: Heavy worm loads can lead to nutritional deficiencies and growth retardation, especially in children.
Mortality: Some worms, like Schistosoma, can be fatal.
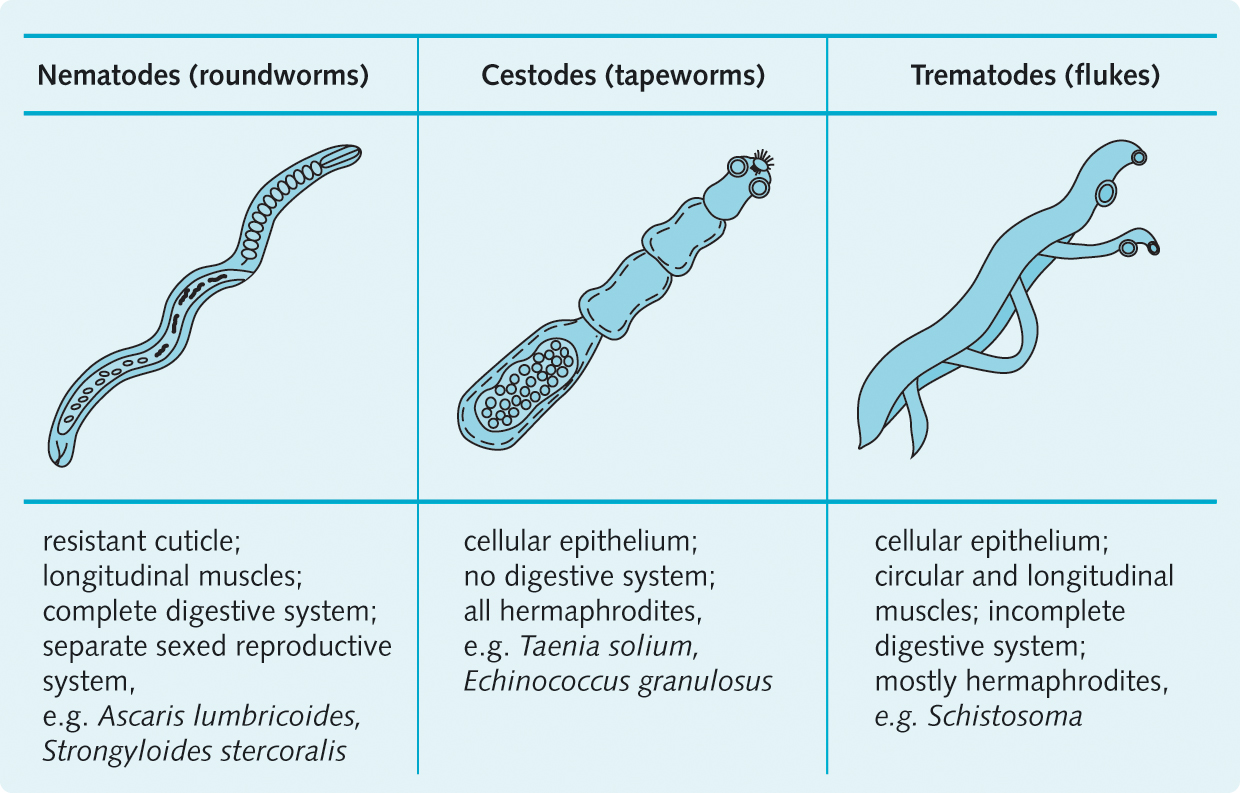
Types of Helminths:
Cestodes (Tapeworms) — Segmented worms with a scolex (head) and proglottids (segments).
Trematodes (Flukes) — Flattened worms with incomplete digestive systems.
Nematodes (Roundworms) — Cylindrical worms with tapered ends.
Examples of Helminth Infections
Helminth | Disease and symptoms | Transmission |
Tapeworms | ||
Taenia saginata | Larvae attach to intestinal gut and mature into adult worms. May be asymptomatic but high worm loads in the gut may result in weight loss and other gut-related symptoms such as abdominal pain and diarrhoea | Consumption of undercooked beef containing larvae |
Hymenolepsis nana | Eggs hatch in intestine maturing into adult worms. May be asymptomatic but high worm loads in the gut may result in weight loss and other gut-related symptoms such as abdominal pain and diarrhoea | Consumption of eggs |
Flukes | ||
Schistosoma species | Schistosomiasis occurs when larvae invade skin, migrating through blood to liver and urinary bladder, maturing into worms in blood vessels. Complications occur from eggs becoming trapped in tissues causing severe inflammatory reactions | Exposure to water environments containing larvae |
Fasciola hepatica | Excystation in duodenum then burrow through the lining of the intestine and migrate to the bile ducts causing inflammation and blockage | Consumption of cysts |
Nematodes | ||
Wuchereria bancrofti | Filariasis occurs when larvae in the bloodstream enter tissues and mature into adults. The worms reside in the lymph system causing blockages and fluid accumulation, possibly leading to lymphedema and elephantiasis | Transmitted from the bite of a mosquito |
Strongyloides stercoralis | Larvae migrate through blood to lungs where they are coughed up and swallowed into the digestive tract where they develop into adults. Symptoms are gut-related with infection in children affecting growth and mental retardation | Larvae in soil penetrate through skin |
Ancylostoma duodenale and Necator americanus (hookworm) | Similar disease and symptoms to S. stercoralis | Larvae in soil penetrate through skin |
Ectoparasites
Ectoparasites — are arthropods, parasites that live on the skin, causing irritation and allergic reactions.
Examples: Scabies, fleas, lice, bedbugs, ticks.
Non-lethal: But can transmit other pathogens or lead to secondary infections.
Vectors: Fleas (bubonic plague), lice (typhus), ticks (Lyme disease).
Scabies: Endemic in Australia's northern Indigenous communities and urban areas.
Secondary Infections: Can cause serious skin infections.
Examples of ectoparasites affecting humans
Ectoparasite | Disease and symptoms | Transmission |
Scabies ( Sarcoptes scabei ) | Female mite burrows under skin to lay eggs causing irritation. May occur anywhere on the body but tends to affect hands and forearms | Direct contact with infected individuals or by coming into contact with their bedding or clothing |
Fleas (Siphonaptera) | Minor irritation from bite | Contact with animals, usually pets, that carry fleas |
Lice
| Bite causes irritation. Different lice affect different parts of the body including head (head louse), body (body louse) and pubic (crab louse) regions | Direct contact with affected individuals or coming into contact with their bedding or clothing |
Bedbugs ( Cimex lectularius ) | Intense itching and irritation from bite which may develop into a painful welt | Bedbugs do not live on human skin. Instead, they infest unhygienic environments, mainly coming out at night to feed on the blood of sleeping individuals |
Ticks (Ixodidae) | Minor irritation from bite | Live in humid bush areas and colonise passing humans |
Transmission of Pathogens
Infection proceeds through six interconnected steps called the ‘chain of infection’ that describes the transmission of a pathogen from its natural reservoir, through a portal of exit, and transmission to a susceptible host through an appropriate portal of entry.
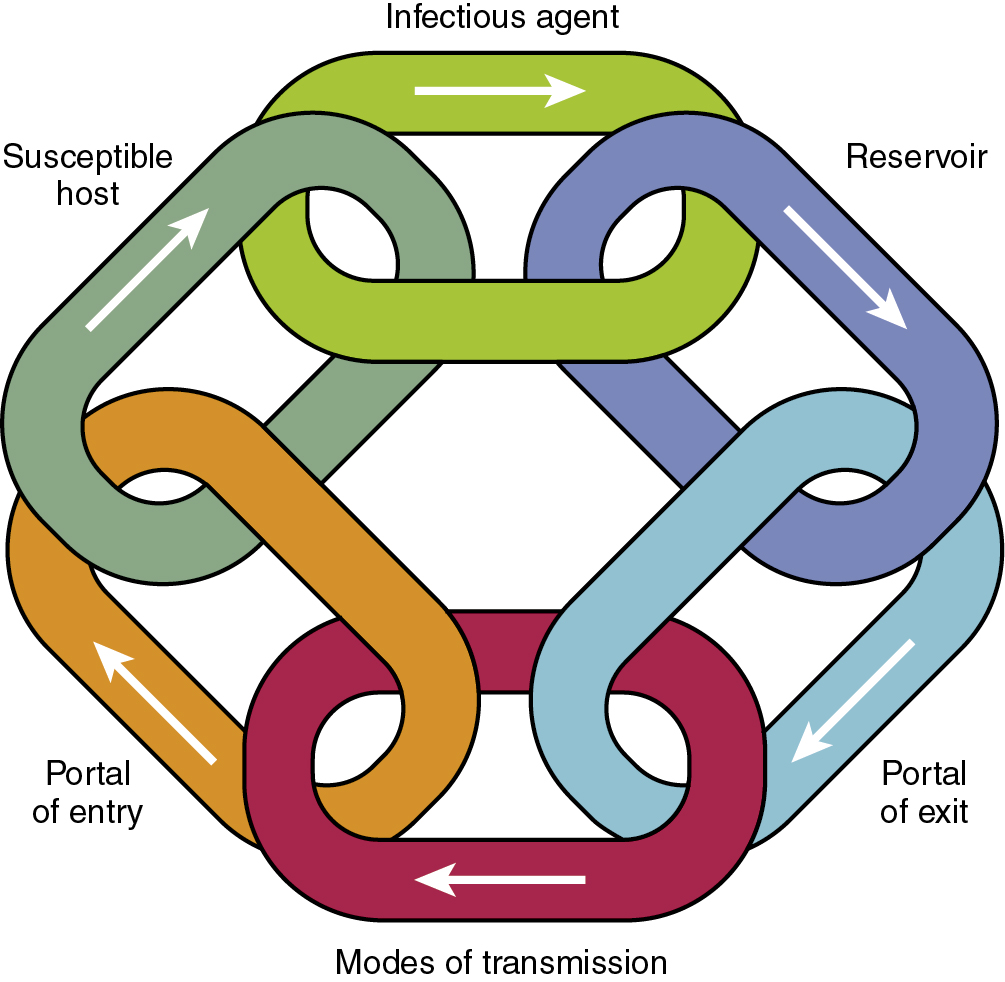
Reservoirs
Reservoirs — settings where pathogens naturally grow.
Types: Human, animal, environment.
Source of Infection: May not always be the direct source of infection (e.g., Legionnaire's disease, C. botulinum).
Eradication: Possible for human-only reservoirs through vaccination (e.g., smallpox).
Control: Isolation of infectious individuals.
Asymptomatic Carriers: Can spread infections unknowingly.
Zoonosis — infections from animals.
COVID-19: Likely a zoonosis from bats.
Other Examples: Influenza (pigs and birds), HIV (non-human primates), Ebola virus (bats).
Environmental Reservoirs:
Plants, soils, water.
Examples: Vibrio species (cholera, diarrhea, wound infections), fungal pathogens.
Reintroduction: Can be consistently reintroduced into the human community.
Portals of Exit
Portals of Exit — How infectious agents leave their reservoir.
Human Portals: Upper respiratory tract (saliva, respiratory droplets), blood, gastrointestinal tract (vomit, diarrhea/feces), urogenital tract (urine, genital fluids), skin (wounds, mucous membranes).
Animal Portals: Similar to human portals.
Environmental Portals: Depend on the environment.
Example: Vibrio bacteria in marine/estuarine waters exit through water.
Modes of Transmission
Modes of Transmission:
Direct Transmission: Infectious agent directly transfers from reservoir to host.
Contact: Skin-to-skin, kissing, sex.
Animal Bites: Contact with animal feces, water, soil, or plants.
Droplet Spread: Short-range transmission through aerosols from coughing, sneezing, talking, breathing.
Vertical Transmission: Mother to unborn child.
Example; Influenza, HIV, STIs.
Indirect Transmission: Infectious agent transfers through an intermediary.
Airborne: Suspended air particles (droplet nuclei).
Fomites: Inanimate objects (food, water, bedding, equipment).
Vectors: Arthropods (mosquitoes, fleas).
Example: Measles, Legionnaire's disease, malaria, plague.
Portal of Entry
Portals of Entry — Method by which a pathogen enters a susceptible host.
Specific Tissue Infection: Pathogens infect specific tissues.
Common Portals: Gastrointestinal, respiratory, urogenital tracts.
Examples:
Gastrointestinal: Consumption of contaminated food or water.
Respiratory: Droplet spread.
Urogenital: Sexual contact.
Blood-borne: Intravenous drug use, blood transfusions.
Skin: Wounds, mucous membranes.
Susceptible Host
Susceptible Host — A person or animal that is vulnerable to infection by a particular pathogen.
Host Susceptibility is an important link in the chain of transmission.
Factors: Host genetics, microbiome, age, pregnancy, medications, health status, underlying conditions.
Age: Very young and very old are more vulnerable.
Other Factors: Nutrition, stress, environmental pollutants, genetic conditions, medical treatments.
Complexity: Multiple factors contribute to host susceptibility.
Breaking Links in the Chain of Infection
Breaking Links in the Chain of Infection:
Targeting multiple links: Provides better outcomes.
Link selection: Depends on the infectious disease, cost, and sociocultural factors.
Controlling Reservoirs:
Human reservoirs: Isolation, treatment, extensive testing.
Fomites: Waste disposal, disinfection, sterilization.
Animal reservoirs: Avoidance or culling (e.g., influenza in birds).
Environmental reservoirs: Source identification and control (e.g., contaminated food).
Protecting Portals of Entry:
Standard precautions: Minimize transmission to healthcare workers.
Personal protective equipment: Face masks, gloves.
Hand hygiene: Controls infectious agents on hands.
Ventilation: Modifying air flow to prevent airborne transmission.
Disrupting Transmission:
Waste disposal: Proper disposal of human waste.
Hygiene: Regular handwashing.
Vector control: Using insecticides, repellents, clothing, bed netting.
Increasing Host Defenses:
Treatment: Treating underlying diseases or using prophylactic antimicrobials.
Vaccination: Effective in decreasing transmission and achieving herd immunity.
Host–pathogen interactions
Bacterial Pathogens
Strategies for Infection
Exposure and Colonization:
Opportunistic pathogens —Cause infection when host conditions are favorable (e.g., weakened immune system, disrupted microbiome).
Normal flora: Bacteria that normally inhabit the body can cause infection if they are relocated to an inappropriate site.
Adhesion — Bacteria sticking to host tissues. They use fimbriae, pili, flagella, and capsular polysaccharide to adhere to host tissues, establishing a focal point of infection.
Invasion and Spread:
Tissue invasion: Bacteria can secrete toxins (exotoxins) to break down tissues and spread.
Exotoxins — Toxins secreted by bacteria.
Toxins:
Types:
cytotoxic (affect multiple cell types),
neurotoxin (nerve cells),
hepatotoxin (liver cells),
cardiotoxin (heart cells),
enterotoxin (enteric cells).
Examples: Cholera toxin, tetanus toxin.
Food intoxication: Bacteria can produce toxins that cause illness without infection (e.g., staphylococcal intoxication, botulism).
Injectosomes — needle-like structures used by bacteria to inject toxins into host cells (effector proteins).
Evasion of Host Defenses:
Bacteria can form biofilms, which provide protection against host defenses and antibiotics.
Capsules can protect bacteria from phagocytosis.
Phagocytosis — a process by which cells, such as white blood cells, engulf and ingest foreign particles or microorganisms.
Antibiotic resistance — the ability of bacteria to resist the effects of antibiotics through various mechanisms.
Examples of toxins produced by bacteria and mechanism of action
Bacterium | Disease | Toxin | Mechanism of action |
Secreted toxins | |||
Clostridium botulinum | Botulism | Neurotoxin | Blocks excitation of muscles causing flaccid paralysis |
Clostridium tetani | Tetanus | Neurotoxin (tetanus toxin) | Prevents inhibition of motor neurons blocking relaxation of muscles |
Corynebacterium diphtheriae | Diphtheria | Diphtheria toxin | Inhibition of protein synthesis |
Listeria monocytogenes | Listeriosis | Listeriolysin | Lysis of multiple host cells |
Shigella dysenteriae | Dysentery (Bloody diarrhoea) | Shiga toxin | Inhibition of protein synthesis. Mainly affects blood vessels |
Vibrio cholerae | Cholera diarrhoea | Enterotoxin (cholera toxin) | Disrupts ion flow in the intestine causing massive water loss and diarrhoea |
Injectosome delivered toxins | |||
Salmonella enterica Typhimurium | Inflammatory gastroenteritis | Multiple effector proteins delivered to intestinal cells by a Type III secretion injectosome system | Induces entry into host cell and manipulates multiple host cell pathways involved in actin arrangement, cytokine production and apoptosis |
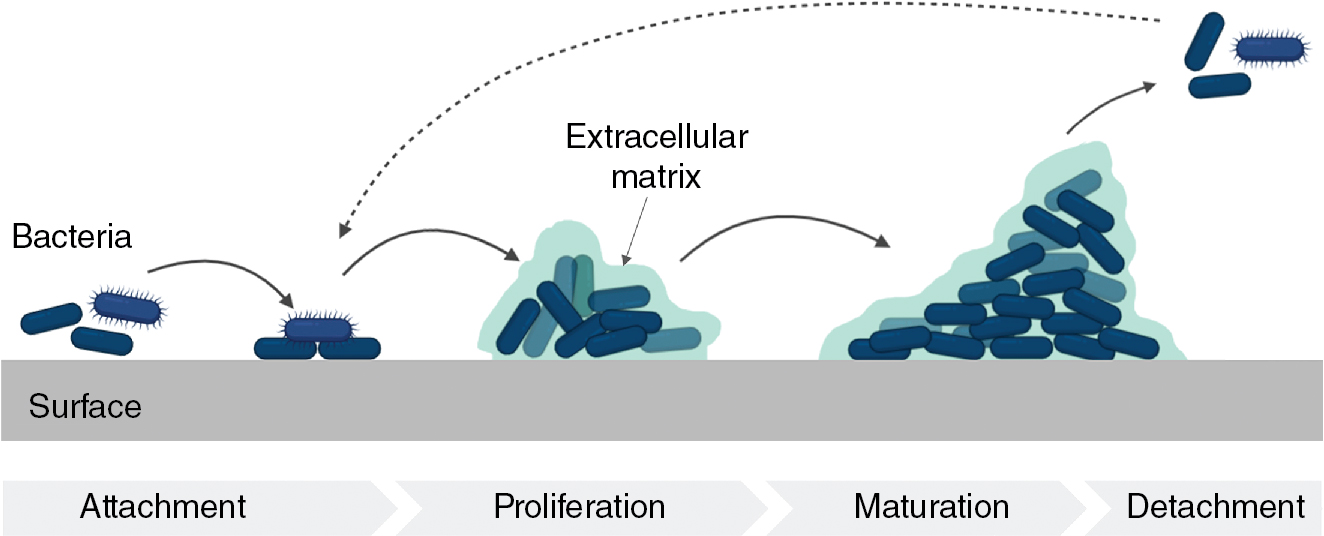
Biofilms
Biofilms — These are communities of bacteria that adhere to a surface and are encased in a protective matrix.
They are a natural mode of bacterial growth, forming on both animate and inanimate surfaces.
Advantages of Biofilms:
Coordinated activity: Bacteria in biofilms can work together to cause tissue damage.
Protection: The matrix acts as a barrier against host immune cells and antibiotics.
Clinical Significance:
Biofilms are often involved in chronic infections, such as Pseudomonas aeruginosa infections in cystic fibrosis patients and periodontal diseases.
Medical implants (e.g., hip joints, heart valves) are prone to biofilm formation, leading to infection.
Temporary implants (catheters) can also develop biofilms, increasing infection risk.
Biofilms on hospital surfaces and water pipes act as reservoirs for pathogens and antibiotic resistance genes.
Bacteria within biofilms are more resistant to disinfectants and antibiotics due to close cell-to-cell contact and horizontal gene transfer.
Antimicrobial Resistance (AMR):
Bacteria can evolve resistance through mutations.
Plasmids — circular pieces of DNA that can transfer resistance genes between bacteria.
Conjugative Plasmids — Contain genes for conjugation (transfer through a pilus).
Resistance plasmids provide an advantage in environments with antimicrobials.
Resistance plasmids spread through waste streams and re-enter the community.
Resistance plasmids are common in pathogens, commensals, and environmental bacteria.
Carriage of resistance plasmids increases the risk of developing a resistant infection.
Resistance plasmids often contain multiple resistance genes, limiting treatment options.
Controlling resistance plasmids is essential for effective infection prevention.
Intracellular Bacterial Pathogens
Some bacteria can invade host cells, evading the immune system and creating a replicative niche.
Obligate — pathogens that can only replicate within a host cell (e.g., Chlamydia, Mycobacterium tuberculosis).
Facultative — pathogens that can replicate both inside and outside host cells (e.g., Salmonella, Legionella, Yersinia).
Some pathogens are internalized by phagocytosis, while others induce host cells to take them in.
Subvert and control host cell functions, including escaping destruction by immune cells and manipulating host actin for cell-to-cell movement.
Fungal Pathogens
Superficial, Cutaneous, and Subcutaneous Mycoses
Dermatophytoses —also known as ringworm or tinea, are fungal infections that affect the skin, hair, or nails.
They are common in tropical regions, including Australia, and are influenced by various factors such as humidity, temperature, immune status, and socioeconomic conditions.
Types of Dermatophytoses:
Tinea capitis — Affects the scalp.
Tinea corporis — Affects the body.
Presentation:
Skin lesions: Circular, red, scaly lesions.
Nail infections: Discoloration, thickening, desquamation, separation from the nail bed.
Invasive infections: Can lead to ulcers and abscesses in immunocompromised individuals
Pathogenesis:
Adherence: Fungal cells attach to keratinized tissues using adhesins.
Penetration: Fungi secrete keratolytic proteases to penetrate the tissue.
Maintenance: Fungi obtain nutrients from the host tissue and adapt to host metabolic changes.
Biofilms: Dermatophytes can produce biofilms, which contribute to the persistence of infection
Systemic opportunistic fungal infections:
Systemic fungal infections — these infections are severe and life-threatening, often occurring in immunocompromised individuals.
Common causes include Candida, Cryptococcus, and Aspergillus species.
Risk Factors:
Immunocompromised individuals: People with HIV/AIDS or undergoing immunosuppressive therapy.
Opportunistic infections: These fungi can cause serious infections in immunocompromised individuals.
Pathogenesis:
Invasive pulmonary aspergillosis: Aspergillus spores enter the lungs, invade tissues, and spread to the bloodstream.
Cryptococcosis: Cryptococcus spores enter the lungs, spread to the bloodstream, and can infect the central nervous system.
Candidiasis: Candida species, normally part of the microbiome, can cause infection in immunocompromised individuals or those with disrupted anatomical barriers.
Virulence Factors:
Adhesins: Allow fungi to attach to host cells and abiotic surfaces.
Enzymes: Secreted enzymes break down host tissues and facilitate invasion.
Hyphae: Thread-like structures that help fungi penetrate tissues
Parasitic Pathogens
Intestinal protozoan parasites:
Intestinal protozoan parasites — these parasites are a common cause of foodborne infections, transmitted through contaminated food or water.
Common parasites:
Giardia lamblia — A flagellated protozoan that attaches to the intestinal wall.
Persistent diarrhea, fatigue, abdominal cramps.
Cryptosporidium parvum — A coccidian protozoan that invades intestinal epithelial cells.
Mild to acute diarrhea, nausea, vomiting, abdominal pain, low-grade fever.
Entamoeba histolytica — An amoeboid protozoan that can invade the colon and spread to other organs.
Bloody mucoid diarrhea, abdominal pain, fever, liver abscesses, life-threatening disseminated infection.
Life Cycle:
Ingestion of cysts: Through the fecal-oral route.
Excystation: Cysts transform into trophozoites in the stomach.
Attachment and proliferation: Trophozoites attach to intestinal epithelial cells and multiply.
Encystation: Trophozoites convert back into cysts for excretion.
Toxoplasma gondii:
Transmission: Ingestion of cysts.
Pathogenesis: Invades intestinal epithelial cells, multiplies, and spreads to other tissues.
Clinical presentation: Can cause flu-like symptoms, lymphadenopathy, encephalopathy, abortion, stillbirth, or congenital abnormalities.
Protozoan parasites acquired from insect bites:
Malaria:
Caused by: Plasmodium species (P. falciparum, P. vivax, P. malariae, P. ovale, P. knowlesi).
Transmission: Anopheles mosquito.
Life Cycle: Complex, involving multiple hosts and parasite stages.
Symptoms: Fever, chills, body aches, severe malaria (neurological syndrome, anemia, multi-organ failure).
Pathogenesis: Involves invasion of hepatocytes and erythrocytes, sequestration of infected erythrocytes in tissues.
American Trypanosomiasis (Chagas Disease):
Caused by: Trypanosoma cruzi.
Transmission: Triatome bug.
Life Cycle: Complex, involving multiple hosts and parasite stages.
Symptoms: Acute phase (fever, headache, enlarged lymph glands) and chronic phase (organ-associated symptoms).
Pathogenesis: Involves invasion of host cells, multiplication, and tissue damage.
Multicellular parasites:
Helminths are multicellular parasites that can infect humans, causing various diseases. They are commonly found in regions with poor sanitation and limited access to clean water. Indigenous populations in Australia are at higher risk for helminth infections.
Examples of helminth infections in Australia:
Strongyloidiasis: Caused by Strongyloides stercoralis.
Hookworm: Caused by Ancylostoma duodenale.
Echinococcosis: Caused by tapeworms.
Pathogenesis:
Tissue damage: Helminths can cause direct tissue damage and trigger inflammation.
Migration: Some helminths can migrate to various organs, causing systemic infections.
Immunological responses: The host may develop tolerance to helminths, limiting damage to both the host and parasite.
Life cycles:
Taeniasis: Humans are the definitive host for tapeworms (Taenia saginata, Taenia solium). Ingestion of raw or undercooked meat leads to infection.
Strongyloidiasis: Larvae penetrate the skin, migrate through the body, and can cause intestinal infections or disseminate to other organs.
Viral Pathogens
Cycle of Viral Infections
Attachment:
Virus adheres to specific receptors on the host cell.
Receptor specificity determines the range of host cells the virus can infect.
Penetration:
Virus enters the host cell through endocytosis or fusion.
Endocytosis is a natural process used by host cells.
Enveloped viruses can fuse with the host cell membrane.
Uncoating:
Viral nucleic acid is released from the capsid.
Mechanisms vary depending on the virus
Replication:
Viral nucleic acid dictates replication strategy.
Viral enzymes are often required for nucleic acid replication.
Viral mRNA is produced and directs protein synthesis.
Viral proteins are assembled into new virions.
HIV is a retrovirus that uses reverse transcriptase to convert RNA into DNA and integrate it into the host genome
Release:
Non-enveloped viruses are released through cell lysis.
Enveloped viruses bud out of the host cell membrane, acquiring their envelope.
Viral proteins are embedded in the host cell membrane during release.
Outcomes of Viral Infections:
Acute: Rapid onset, short duration (e.g., influenza, COVID-19).
Latent: Initial acute phase followed by a latent period (e.g., herpes simplex virus).
Persistent: Slow progression, ongoing replication without necessarily destroying host cells (e.g., Epstein-Barr virus).
Oncogenic: Can transform host cells into cancerous cells (e.g., human papillomavirus).
Immunological responses
Generality on the role of the immune system during infection
Immune system
Defense against pathogens.
Elimination of toxic or allergenic substances.
Differentiation between self and non-self to avoid attacking host cells or beneficial microorganisms.
Components:
Cells: A variety of cells with specific roles in different phases of the immune response.
Innate Immunity: Immediate, non-specific response involving barriers and soluble molecules.
Adaptive Immunity: More specific response involving T and B cells.
Innate Immunity:
Barriers: Epithelial cells, mucous layers, ciliated epithelial cells.
Soluble Molecules: Complement system proteins, defensins, inflammatory mediators, reactive free radical species, cytokines, and chemokines.
Pathogen Recognition: Recognizes general classes of pathogens but not fine distinctions.
Immediate Response: Aims to destroy pathogens or contain the infection until adaptive immunity activates.
Adaptive Immunity:
T-helper Cells:
Th1: Pro-inflammatory response for intracellular pathogens.
Th2: Anti-inflammatory response for extracellular parasites.
Cytokines and Chemokines: Regulate immune cell recruitment, differentiation, and activation.
Dendritic Cells:
Bridge between innate and adaptive immunity.
Phagocytosis: Engulf and process pathogens.
Antigen Presentation: Present antigens to T cells.
Pattern Recognition Receptors (PRRs): Recognize pathogen-associated molecular patterns (PAMPs).