Palmar region of the Hand.
Palmar Region of the Hand: Anatomy, Muscles, Blood Supply, Innervation, and Clinical Significance
The palmar region of the hand is an essential area responsible for grip, dexterity, and various fine motor functions. It contains numerous structures such as muscles, tendons, blood vessels, and nerves that work together to perform intricate hand movements. The anatomy of the palmar hand is also important in understanding common hand injuries, conditions, and surgical interventions.
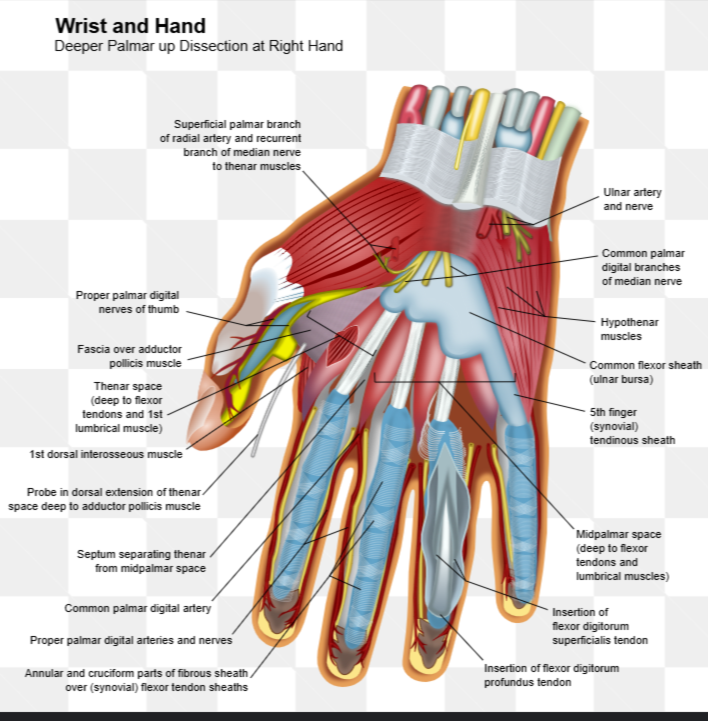
Anatomy of the Palmar Region
The palmar region is divided into several anatomical areas and is characterized by a dense arrangement of muscles, nerves, and vessels.
1. Layers of the Palmar Region
Skin: The skin on the palm is thick, and the palmar aponeurosis is found beneath it, which is a strong connective tissue structure providing support and protection.
Palmar Aponeurosis: A triangular fibrous structure that lies just beneath the skin. It protects the tendons of the long flexors and helps to anchor the skin to underlying structures.
Flexor Tendons: Tendons of the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) pass through the palmar region to insert on the fingers.
Muscles: The muscles of the palm are classified into three groups:
Thenar muscles: Located at the base of the thumb.
Hypothenar muscles: Located at the base of the little finger.
Midpalmar muscles: Include the lumbricals and interossei muscles.
2. Major Muscles of the Palmar Region
The muscles of the palmar region of the hand are responsible for the movement and function of the digits. These muscles can be categorized into three groups:
Thenar Muscles: The thenar muscles control the movements of the thumb and allow for thumb opposition, a critical movement for grasping and pinching.
Abductor Pollicis Brevis:
Origin: Flexor retinaculum and scaphoid, trapezium.
Insertion: Lateral side of the base of the proximal phalanx of the thumb.
Action: Abducts the thumb.
Innervation: Median nerve (recurrent branch).
Flexor Pollicis Brevis:
Origin: Flexor retinaculum and trapezium.
Insertion: Lateral side of the base of the proximal phalanx of the thumb.
Action: Flexes the thumb.
Innervation: Median nerve (recurrent branch).
Opponens Pollicis:
Origin: Flexor retinaculum and trapezium.
Insertion: Lateral side of the 1st metacarpal.
Action: Opposes the thumb (bringing it across the palm).
Innervation: Median nerve (recurrent branch).
Hypothenar Muscles: These muscles control the movements of the little finger and contribute to hand strength and dexterity.
Abductor Digiti Minimi:
Origin: Pisiform bone.
Insertion: Medial side of the base of the 5th proximal phalanx.
Action: Abducts the little finger.
Innervation: Ulnar nerve (deep branch).
Flexor Digiti Minimi Brevis:
Origin: Hook of the hamate and flexor retinaculum.
Insertion: Medial side of the base of the 5th proximal phalanx.
Action: Flexes the little finger.
Innervation: Ulnar nerve (deep branch).
Opponens Digiti Minimi:
Origin: Hook of the hamate and flexor retinaculum.
Insertion: Medial border of the 5th metacarpal.
Action: Opposes the little finger (bringing it across the palm).
Innervation: Ulnar nerve (deep branch).
Midpalmar Muscles:
Lumbricals:
Origin: Tendons of the flexor digitorum profundus.
Insertion: Extensor expansions of the 2nd to 5th fingers.
Action: Flex the metacarpophalangeal joints and extend the interphalangeal joints.
Innervation: Median nerve (lateral two lumbricals), Ulnar nerve (medial two lumbricals).
Palmar Interossei:
Origin: Sides of the metacarpals of the 2nd, 4th, and 5th fingers.
Insertion: Bases of the proximal phalanges and extensor expansions of the 2nd, 4th, and 5th fingers.
Action: Adduct the fingers (PAD - Palmar ADduction).
Innervation: Ulnar nerve (deep branch).
Dorsal Interossei:
Origin: Sides of two adjacent metacarpals.
Insertion: Bases of the proximal phalanges and extensor expansions of the 2nd, 3rd, and 4th fingers.
Action: Abduct the fingers (DAB - Dorsal ABduction).
Innervation: Ulnar nerve (deep branch).
Nerve Supply to the Palmar Region
The innervation of the palmar hand is provided by two major nerves: the median nerve and the ulnar nerve. These nerves ensure proper movement and sensation of the hand.
Median Nerve:
Function: The median nerve innervates most of the thenar muscles, the lateral two lumbricals, and provides sensory innervation to the palmar surface of the thumb, index, middle, and half of the ring finger.
Pathway: The median nerve passes through the carpal tunnel to enter the palm and innervates the thumb and the first three digits.
Ulnar Nerve:
Function: The ulnar nerve innervates the hypothenar muscles, the medial two lumbricals, all the interossei muscles, and provides sensory innervation to the medial part of the hand, including the little finger and half of the ring finger.
Pathway: The ulnar nerve enters the palm through the Guyon’s canal, located at the wrist, to supply the intrinsic muscles and skin of the little finger.
Blood Supply to the Palmar Region
The blood supply to the palmar region of the hand is provided by branches of the radial and ulnar arteries:
Radial Artery:
The radial artery passes through the anatomical snuffbox and contributes to the deep palmar arch. It supplies the thumb and index finger.
Ulnar Artery:
The ulnar artery enters the palm and contributes to the superficial palmar arch, which supplies blood to the medial part of the hand. It provides branches to the little finger and the medial part of the ring finger.
Both arteries form anastomoses in the palm, ensuring adequate blood supply and redundancy in case of blockage or injury.
Clinical Significance of the Palmar Region
1. Carpal Tunnel Syndrome
Carpal Tunnel Syndrome (CTS) occurs when the median nerve is compressed within the carpal tunnel, which can cause symptoms such as numbness, tingling, and weakness in the thumb, index, middle, and part of the ring fingers. It is often caused by repetitive hand movements and can result in loss of thumb opposition.
2. Ulnar Nerve Compression
Ulnar nerve entrapment at the Guyon’s canal (located at the wrist) can lead to claw hand deformity, where the affected fingers (typically the 4th and 5th fingers) remain in a flexed position due to the weakness of the lumbricals and interossei.
3. Dupuytren's Contracture
Dupuytren's contracture is a condition where the palmar aponeurosis thickens and contracts, causing the fingers (usually the 4th and 5th) to bend inward toward the palm. It leads to a decrease in hand functionality and may require surgical intervention.
4. Tendon Injuries
Injuries to the flexor tendons (such as flexor digitorum profundus and flexor digitorum superficialis) can impair finger flexion and lead to inability to make a fist. This can occur from trauma or lacerations in the palm.
5. Intrinsic Muscle Weakness
Damage to the median or ulnar nerves can result in weakness or paralysis of the intrinsic muscles of the hand, affecting the ability to grasp and manipulate objects. This may lead to conditions such as wrist drop or claw hand.
Summary
The palmar region of the hand plays a vital role in performing complex, coordinated movements. The thenar, hypothenar, and midpalmar muscles facilitate important functions such as grip, pinching, and fine motor skills. Proper nerve and blood supply are crucial for hand function, with the median nerve and ulnar nerve innervating the muscles and providing sensation to different parts of the hand. Conditions like carpal tunnel syndrome, ulnar nerve compression, and Dupuytren's contracture can significantly affect hand function, highlighting the importance of understanding the anatomy and clinical relevance of the palmar region.