Wk 8 - Drugs Acting on Central Nervous System
Central Nervous System
Brain & Spinal Cord
very important structure of the CNS is its protective mechanisms that not all chemicals can pass through it, this affects the pharmacodynamics of drugs because some of them cannot penetrate the CNS.
One vital protective structure is the Blood Brain Barrier (BBB). This represents therapeutic challenge to drug treatment of brain related disorders because a large percentage of drugs are carried bound to plasma proteins and are unable to cross the brain.
Anxiolytic and Hypnotic Drugs
Anxiety
a feeling of tension, nervousness, apprehension or fear that usually involves unpleasant reactions to a stimulus, whether acutal or unknown.
Is classified as mild, moderate, severe and panic
Mild Anxiety - Typically doesn't significantly interfere with daily life. Can be managed with coping mechanisms or stress-reduction techniques. (Worry, unease)
Moderate Anxiety - Can disrupt daily activities and make it challenging to function normally. May require professional help or medication. (fear, dread)
Panic Anxiety - Can be debilitating and significantly interfere with daily life. Often requires professional treatment to manage. (sense of impending doom)
Sedation
the loss of awareness and reaction to environmental stimuli
Hypnosis
Extreme sedation resulting in further CNS depression and sleep
These conditons occur due to increase excitatory neurotansmitters causing rapid brain impulse conduction causing restlessness, irritability, loss of concentration, loss of mental focus and sympathetic responses like palpitations, tremors, diaphoresis, increase breathing and increase blood pressure.
Classified into Three
Barbiturate
Benzodiazepines
Non-Benzodiazepines
Mechanism of Action
to enhance the effect of GABA (Gamma Amino Butyric Acid), therefore decreasing conduction of rapid impulses causing symptoms of anxiety.
GABA (Gamma Amino Butyric Acid) - an inhibitory neurotransmitter to decrease impulses in the synapses of the brain
Barbiturates
drug action is to enhance GABA effect.
CNS depressants
Inhibit neuroral impulse conduction in the ascending RAS
Depress cerebral cortex
Depress motor output
This used to be the drug of choice to manage anxiety but its depressant effect may cause severe respiratory depression that this is not primarily used for anxiety today
Indication
Relief of the signs and symptoms of anxiety
Sedation
Insomnia
Preanesthesia
Seizures
Pharmacokinetics
Barbiturates are absorbed well, reaching the peak levels in 20 to 60 minutes.
It is metabolized in the liver and excreted in the urine
Contraindications and Cautions
Barbiturates are more addicting than other anxiolytic drugs.
May cause severe CNS depression and respiratory dysfunction.
Contraindicated in pregnant women and clients with heaptic and renal dysfunction
Adverse Effects
CNS depression, paradoxical excitement, anxiety and hallucinations.
Gastrointestinal signs and symptoms like nausea, voimiting, constipation, diarrhea and epigastric pain.
Cardiovascular effects include bradycardia, hypotension and syncope
Drug-Drug Interactions
Increase CNS depression when given with alcohol, antihistamines, and other tranquilizers
Altered response to phenytoin
MAO cause increase serum levels and effect
Decrease effectiveness of the following drugs: anticoagulants, digoxin, tricyclic antidepressants, corticosteroids and oral contraceptives
Drug Samples (…barbital)
Phenobarbital
Secobarbital
Amobarbital
Benzodiazepines
drug action is to enhance GABA effect to cause inhibition of impulse transmission
Act in the limbic system and the RAS
Causes interference with neurons firing
Lower doses assist with anxiety o Higher doses cause sedation and hypnosis
Indications
Anxiety Disorders
Alcohol Withdrawal
Hyperexcitability and Agitation
Preoperative relief of anxiety and tension
Pharmacokinetics
this is well absorbed in the GIT with peak levels achieved in 30 minutes.
This is lipid soluble and well distributed in the body crossing the BBB, placenta and breast milk.
Metabolized in the liver and excreted in the urine
Contraindications and Cautions
Contraindicated in Clients with allergy to benzodiazepines, psychosis, clients with acute narrow angle glaucoma, shock, acute alcohol intoxication which may exacerbate the depressant effects of the drugs.
Contraindicated in pregnancy as this is known to possible cause cleft lip or palate, inguinal hernia, cardiac defects, microcephaly or pyloric stenosis if taken during the first trimester.
Caution should be used in the elderly or debilitated patients an those with hepatic and renal functions
Adverse Effects
Sedation, drowsiness, depression, lethargy
anticholinergic effects like drying of mount, constipation, orthostatic hypotension, urinary retention, dysrhythmias, blood dyscrasias and phlebitis.
Withdrawal syndrome may occur with abrupt cessation characterized by nausea, headache, vertigo, malaise and headache.
Drug-Drug Interactions
Increase CNS depression when taken with alcohol
Increase in effect when taken with cimetidine, oral contraceptives, or disulfiram
Decrease in effect if given with theophylline or ranitidine
Drug Samples (…zepam)
Diazepam
Lorazepam
Clonazepam
Non-Benzodiazepines
Other Drugs used for anxiety that do not fall under Benzodiazepine
Paraldehyde
Old drug used for Delerium Tremens, seizures, absorbed and metabolze in the liver.
It has a distinctve odor and cannot be stored in plastic containers
Meprobamate
An old drug used to manage anxiety for 4 months, works in the limbic system.
metabolized in the liver and excreted in the urine
Chloral Hydrate
Frequently used to produce nocturnal sedation or preoperative sedation. Unknown mechanis of action.
absorned in the GIT, metabolized in the liver and excreted in the urine
Zolpidem
Used to treat insomnia.
Metabolized in the liver and excreted in the urine
Anti-Histamines
Dipenhydamine (Benadryl)
Promethazine (Phenergan)
Used or its drowsiness effect in anxiety.
With anticholinergic effect. Used during preoperatively or postoperatively to decrease use of narcotics
Buspirone
No sedative,anticonvulsant, or muscle relaxant properties, unknown mechanism of action, reduces anxiety without many CNS effects.
Absorbed in the GIT, metabolized in the liver an excreted in the urine
Beta-Blockers
Propranolol
Metoprolol
Decreasing sympathetic effect to lessen signs nd symptoms of anxiety
Nursing Considerations
Do not administer intraarterially because of possible serius areriospasm and gangrene may develop
Do not mix IV drugs with other drugs
Give parenteral forms if oral forms are not feasible and switch to oral which is safer
Give IV drugs slowly to avoid hypotension effects
Promote safety measures
Monitor hepatic and kidney function
Taper dose of drugs gradually o
Provide comfort measures to help patient tolerate the effects of drugs
Provide thorough health teaching about drug effects and adverse reactions
Offer support and encouragement
For overdose of Benzodiazepine, Flumazenil must be ready as its antidote.
Antidepressant Drugs
Depression being an affective disorder is recognized by its clnical manifestations such as sleep disturbances, they have little energy, inability to perform daily activity.
Affect - People’s feelings in response to their environment
Affective Disorder - A person’s mood goes far beyond the usual, normal “ups and downs”
They may describe overwhelming feelings of sadness, despair, hopelessness and disorganization.
Pharmacology explains depression by Biogenic Amine Theory.
Biogenic Amine Theory
This theory explains that depression occurs due to decreasing neurotransmitters, norepinephrine, serotonin and dopamine.
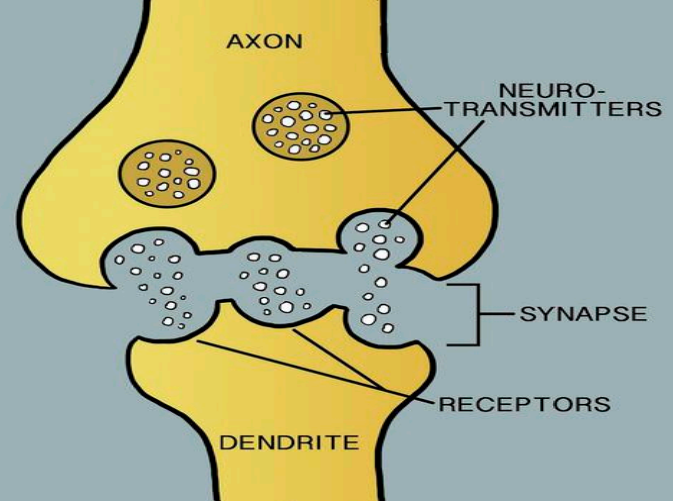
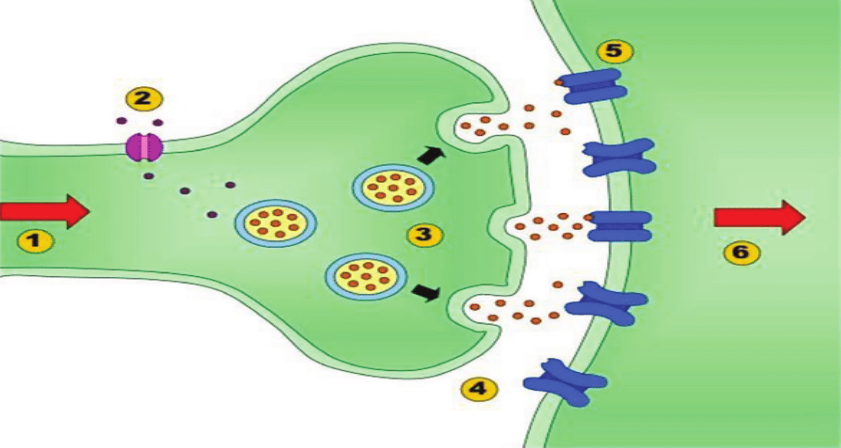
When impulses travel across the synapses, neurotransmitters are released into the symapse, they bind in the receptors in the post synaptic neural membrane and help impulse to be conducted. After which, neurotransmitters are removed by enzymes or they may go back to the presynaptic neuron:
Limbic System
area responsible for over all emotion and behavior
In the Limbic System, there are 3 neurotransmitters being released (Norepinephrine, Serotonin and Dopamine)
After impulse is transmitted across the synpase, and enzyme called Mono Amine Oxidase will remove them.
Some however may go back to the pre synaptic neuron the process called reuptake of Neurotrnasmitters. If they are not available in the synapse, there will be no more impulse transmission
depression results from decreasing neurotransmitter in the limbic system which may happen due possibly to:
Overused of neurotransmitters ( Norepinephrine, Dopamine and Serotonin)
Increase effect of Mono Amine Oxidase ( MAO ) enzyme
Increase reuptake of neurotransmitter back to presynaptinc neuron
Mechanisms of Action
Inhibit the enzyme Mono Amine Oxidase (MAO), leading to increased NE or 5HT in the synaptic cleft
Inhibit Reuptake of Neurotransmitters, leading to increased neurotransmitter levels in the synaptic cleft
Regulate receptor sites and breakdown of neurotransmitters, leading to an accumulation of neurotransmitters in the synaptic cleft
Tricyclic Antidepressants (TCA)
inhibit presynaptic reuptake of neurotransmitter, norepinephrine and serotonin, which leads to accumulation of these neurotransmitters in the synaptic cleft and increased stimulation of post synpatic receptors
Pharmacokinetics
it is abosrbed in the gastrointestinal tract, reaching the peak in 2 to 4 hours.
Widely distributed in the tissue including the brain.
Metabolized in the liver and excreted in the urine. They cross the placenta and the breast milk.
Contraindications and Caution
Contraindicated to those with known allergy to TCA.
Clients with recent myocardial infarction because of its cardiovascular effects.
Caution should be used in clients with Gastrointestinal and Genitourinary tract disorders.
The presence of hepatic and renal impairment increases toxicity of the drugs.
Adverse Effects
CNS effects like sedation, hallucinations, fatigue, cardiovascular effects, unstable blood pressure, abnormal rhtyhms, myocaridal infarction, anticholinergic effects like drying of the mouth, constipation, urinary retention
Remember Mnemonic
C - Cardiovascular Effects
A - Anticholinergic Effects
S - Sedation
H - Hypotension or Hypertension
Drug-Drug Interactions
The effects of TCA may increase if combined with Ranitidine, Fluoxetine and Cimetidine especially the anticholinergic effects
Oral anticoagulant level may increase if combined with TCA and risk for bleeding increases.
Increase effect with sympathomimetic drugs especially its cardiovascular effects
Drug Samples
Imipramine
Amitryptilline
Clomipramine
Mono Amine Oxidae Inhibitors
these drugs inactivate the enzyme MAO to increase the neurotransmitters in the synapses.
Pharmacokinetics
absorbed in the GIT, reaching peak levels in 2 – 3 hours.
metabolized in the liver and excreted in the urine.
They pass the placenta and breast milk and not used in pregnancy
Contraindications and Cautions
Contraindicated in clients with cardiovascular disease, hepatic and renal disease.
Caution should be used in psychiatric patients
Adverse Effects
More adverse effects than other antidepressant drugs.
Dizziness, excitement, nervousness, mania, hyperfexia, tremors, confusion, insomina, agitation and blurred vision.
Liver toxicity, Cardiovascular toxicity.
Anticholinergic effects
Drug-Drug Interaction
Drug interaction with other antidepressant drugs include hypertensive crisis, coma and severe convulsion.
A period of 6 weeks should elapse after stopping SSRI and beginning MAOI.
Drug-Food Interactions
Tyramine-rich food which normally broken down by MAO enzymes in the GIT maybe absorbed in high concentration in the resence of MAOI and may cause hypertensive crisis.
Fermented Foods
Aged Foods
Cured Foods
Overripe Foods
Drug Samples
Isocarboxazid - Used for patients who did not respond to or could not take newer, safer antidepressants
Phenelzine - Used for some patients who did not respond to newer, safer antidepressants
Tranylcypromine - Used for adult outpatients with reactive depression
Selective Serotonin Reuptake Inhibitors
these drug specifically block the reuptake of serotonin with little or no effect on Norepinpehrine. SSRIs do not have the many adverse effects of TCAs and MAOIs
Indications
Depression
Obsessive Compulsive Disorders (OCD) Panic attacks
Bulemia
Post Traumatic Stress Disorder (PTSD)
Pharmacokinetics
well absorbed in the GIT, metabolized in the liver and excreted in the urine or feces.
SSRIs are associated with congenital abnormalities. They passed the placenta and the breastmilk
Contraindications & Caution
Those with allergy to SSRIs
pregnancy and lactation.
Adverse Effects
CNS effects like headache, drowsiness, dizziness, insomnia, anxiety, tremor, agitation and seizures.
Anti cholinergic effects on the gastrointestinal tract and genitourinary tract
Drug Samples
Sertraline
Paroxetine
Fluoxetine
Nursing Considerations
Limit drug access to potentially suicidal patients to decrease the risk of overdose
Monitor the patient for 2 – 4 weeks to ascertain onset and full effects
Monitor blood pressure and orthostatic blood pressure carefully
Monitor liver function
Withold medication dose in client with severe headache that may due to severe hypertension and cerbrovascular effects
Have phentolamine or another adrenergic blocker for hypertensive crisis
Provide comfort measures to help the client tolerate drug effects
Provide list of food that is low or no tyramine to clients on MAOI therapy
Offer support and encouragement to help patients cope with the disease and drug regimen
Psychotherapeutic Drugs
Mental disorders have several classifications. For this course, discussion include only drugs used for Schizophrenia and Mania, two of the most common psychiatric disorders.
Schizophrenia
the most common type of psychotic disorders.
This prevents an individual in functioning in the society.
Some clinical manifestations include, hallucinations, delusions, paranoia, speech abnormalities and affcetive problems
Mania
associated with Bipolar illenss
Mania is characterized by periods of extreme overactivity and excitement
Narcolepsy
daytime sleepiness and sudden periods of loss of wakefulness
Caused by problems with stimulation of the brain by the reticular activating system (RAS)
problems with response to that stimulation
Attention Deficit Disorder (ADHD)
inability to concentrate on one activity for longer than a few minutes
state of hyperkinesis
usually diagnosed in school-aged children but can occur in adults
Drugs for mental disorders are called Psychotherapeutic drugs.
Drugs for Schizophrenia are called Anti Psychotic Drugs
Drugs for Mania are called Anti Manic Drugs
Antipsychotic Drugs
Mechanism of Action
Typical Antipsychotic Drugs
block Dopamine receptors in the limbic system, in the reticular activating system and the brain.
This group of antipsychotic may block all dopamine receptors including those not associated with psychoses
Atypical Antipsychotic Drugs
block Dopamine and Serotonin receptors.
This group will lock only the receptors of Dopamine and Serotinin which are responsible for occurrence of psychosis making them more specific drugs for Psychotic disorders
Drug Classifications
Typical Antipsychotic Drugs
once known as major tranquilizers
primarily dopamine receptor blockers
used to treat disorders involving thought processes
Older drugs, they are less potent and associated with more adverse effects
→ Chlorpromazine
→ Fluphenazine
→ Thioridazine
→ Haloperidol
Atypical Antipsychotic Drugs
block both dopamine receptors and serotonin receptors
may alleviate some of the unpleasant neurological effects and depression of typical antipsychotics
→ Clozapine
Pharmacokinetics
Antipsychotic drugs are erratically absorbed in the GIT, metabolized in the liver and excreted in the bile and urine.
Widely distributed in the tissues, being released up to 6 months after they are discontinued.
Drugs cross the placenta and breast milk so they are not given to pregnant and lactating mothers
Contraindications and Cautions
Contraindicated in patients with Parkinson’s disease, cardiovascular disease, severe hypotension and bone marrow suppresion
Adverse Effects
Anti cholinergic effects like drying of the mouthe, constipation and urinary retention, Sedation effect, Orthostatic hypotension and extra pyramidal symptoms.
Remember Mnemonic
A – Anti cholinergic effect
S – Sedation
H – Hypotension
E – Extra pyramidal Symptoms
Extra Pyramidal Symptoms
Parkinson’s like syndrome, Dystonia, Akathisia, Tardive dyskinesia (happen because of dopmaine blocking effect in the basal ganglia altering its function of coordination and fine motor function.)
Nursing Considerations
Do not allow patients to crush or chew the tablet as it decreases absorption of the drugs
Monitor for orthostatic hypotennsion
Consider warning the patient or the patient’s guardian on the risk of tardive dyskinesia
Monitor CBC to check signs of bone marrow suppression
Provide positioning of legs to decrease discomfort of dyskinesia
Provide sugarless candies for drying of the mouth
Encourage the patient to void before taking the dose if urinary retention is a problem
Provide safety measures such as side rails and assistance in ambulation if there are CNS effects
Provide vison examination to determine ocular changes
Conduct thorough health teaching on the effects and adverse effects of the drugs
Offer support and encouragement to help patients cope with their drug regimen
Anti Manic Drugs - Lithium
Mechanism of Action
Lithium alters sodium transport in the nerve and muscle, inhibit the release of norepinephrine and dopamine slightly and decreases intraneuronal content of second messengers.
The last action may modulate impulses to control hyperactive state in mania
Pharmacokinetics
Lithium is absorbed in the GIT. It slowly crosses the BBB.
Dehydration and sodium depletion may cause the kidneys to reabsorb more Lithim thus increasing serum levels and toxicity.
Lithium crosses the palcenta and breastmilk
Contraindications and Cautions
Contraindicated to those with allergy to the drug, dehydration, hyponatremia and leukemia
Adverse effects
Toxicity associated with serum level of Lithium. ( Therapeutic level 0.6 – 1.2 mmol/L)
Serum level less than 1.5 mmol/L
CNS problems including lethargy, slurred speech, muscle weakness, fine tremor; poluria, beginning gastric toxicity
Serum level 1.5 – 2 mmol/L
Intensification of the above plus ECG changes
Serum levels of 2.0 – 2.5 mmol/L
Progression of CNS symptoms to ataxia, hyperreflexia and seizure, hypotension
Serum levels more than 2.5 mmol/L
complex multi organ toxicity and death
Other Drugs for Mania
Aripiprazole – atypical antipsychotic drug
Lamotrigine – anti convulsive drug
Olanzapine – atypical antipsychotic drug
Quetiapine – atypical anti psychotic drug
Nursing Considerations
Daily monitoring of lithium serum levels
Give the drug with food to alleviate GI irritation
Ensure that the patient have adequate intake of salt nd fluid
Monitor closely especially during the initial stage of therapy
Arrange for small and frequent meals with sugarless lozenges for drying of mouth
Provide safety measure like siderails and assistance with ambulation if CNS effects occur to prevent potential injury
Offer support and encouragement ot help patient cope with drug regimen
Anti-Seizure Drugs
Seizure
collection of different syndromes characterized by abnormal and excessive impulse transmission in the brain
may be primary or secondary.
Primary Seizure - Disorder has no known cause this is often called Epilepsy
Secondary Seizure - may be caused by Cerebrovascular accident, Infections, Brain Tumor, Traumatic Brain Injury, Fever and a lot more conditions that may alter impulse transmission in the brain
Convulsion
seizure manifesting motor symptoms like tonic clonic seizure.
All convulsions are seizure but not all seizures are convulsions
Classifications of Seizure
Generalized Seizure - beigns in one area of the brain and rapidly spread to both hemispheres of the brain.
Tonic – Clonic Seizure (Grand Mal Seizure) - dramatic (loss of conscious)
Absence seizures (petit mal seizures) - brief (loss of attention)
Myoclonic seizures - brief muscle jerks often on limbs
Febrile seizures - in children usually when having a fever
Status epilepticus - medical emergency, seizure more than 5 mins
Partial Sezure - Partial seizures or focal seizures involve one area of the brain and do not spread throughout the entire organ
Simple partial seizures
Occur in a single area of the brain and may involve a single muscle movement or sensory alteration
Complex partial seizures
Involve complex sensory changes
Motor changes may include involuntary urination, chewing motions, diarrhea, etc.
The problems of seizure is excessive impulse transmission in the brain, so the action of the drug is to decrease impulse transmission, anti seizure drugs cause CNS depression.
Mechanisms Of Action
Suppressing sodium influx or deporalarization in the neuron
Suppressing calcium influx, preventing electric current generated by calcium ions
Increasing the action of the Gamma Amino Butyric Acid ( GABA ) an inhibitory neurotransmitter in the brain
Action potential happen by sodium influx and potassium efflux
calcium channels open causing release of calcium that generate electrical activity and nurotransmitters both excitatory and inhibitory regulate impulse transmission.
Excitatory neurotransmitters allow impulses to travel while inhibitory neurotransmitters stop impulses.
The mechanisms of action of anti seizure drugs occur in the neuronal synapse.
Drugs for Seizures are called Anti – seizure drugs or Anti – convulsive drugs (Anticonvulsant drugs) or Anti – Epileptic Drugs.
Drug Classifications
Hydantoins
inhibit sodium influx or depolarization along the nerve fiber.
Pharmacokinetics
Hydantoins are absorbed in the GIT.
It is higly protein bound up to 95%.
A decrease in serum albumin or proteins increases free phenytois serum levels.
Average half life is 24 hour.
Hydantoins are metabolized to inactive metabolites and excreted in the liver.
Hydantoins are less sedating than Barbiturates and Benzodiazepines.
Adverse Effects
Neurologic and psychiatric effect which include slurred speech, confusion, depression.
Low platelet count and WBC may happen and gingival hyperplasia (overgrowth of gum tissue or reddened gums that easily bleeds).
Hyperglycemia and less severe adverse effcts such as nausea, vomiting, constipation, drowsiness, headache and alopecia
Drug-Drug interactions
Hydantoins must not be taken with other anti seizure drugs because it may increase its CNS depressant effects.
Increase effects of Hydantoins happen in combination with Aspirin, anticoagulants, Barbiturates, Rifampicin and chronic ingestion of ethanol.
Decreased Hydantoins absorption occur when combined with Antacids, calcium preparations, sucralfate and some anti cancer drugs.
Drug Samples (…toin)
Phenytoin
Fosphenytoin
Ethotoin
Barbiturates
enhance GABA effect.
These drugs are highly sedating and they may cause severe CNS depression.
Indications
Anxiety, General Anesthesia and most commonly used for Generalized Tonic – Clonic Seizure
Benzodiazepines
enhanced GABA effect.
Indications
For status epilepticus and benign febrile seizure.
Diazepam is not used for long term treatment of seizure. Clonazepam is good for treatment of Petit Mal Seizure and Myoclonic Seizure
Succinimides
enhanced effect of GABA, an inhibitory neurotransmitter.
Drug Samples
Ethosuximide - the drug of choice for Petit – Mal or Absence Seizure (fewer adverse effects)
Methosuximide
Valproate or Valproic Acid
reduces electrical acivity by suppressing calclim influx and enhancing GABA effects the drug of choice for treating myoclonic seizure
Other Anti-seizure Drugs
Carbamazepine
Gabapentin
Lamotrigine
Levetiracetam
Topiramate.
Some of these drugs used for partial seizure may also be used for treatment of neuropathic pain
Carbamazepine is used for treatment of Trigeminal Neuralgia.
Nursing Considerations
Administer the drug with food to alleviate GI irritations
Monitor CBC to detect possible bone marriw suppresion
Evaluate therapeutic blood level to prevent toxicity
Provide safety measures
Provide thorough health teaching, including drug name, prescribed dosage and avoidance of adverse effects
Suggest that clients wear Medic Alert Bracelet to alert health care workers about the use of anti epiletpic drugs
Offer support and encouragement to help the partient cope with the drug regimen.
Anti-Parkinson Drugs
Parkinson’s Disease
a degenerative disorder of the central nervous system. There is no known cause.
This is common among elderly 60 years old and above.
The disease is characterized by degeneration of the substantia nigra in the midbrain. Therefore there is tremendous decrease of dopamine in the brain especially affecting the basal ganglia
Substantia Nigra
A dopamine secreting neurons in the brain.
Basal Ganglia
responsible for coordinating fine motor movement of the body
Alterations in the basal ganglia function results to lack of coordination, tremors, rigidity and bradykinesia
The neurons of the basal ganglia function normally when there is a balance between excitatory and inibitory neurotransmitters.
Dopamine in the basal ganglia acts as the inhibitory neurotransmitter
Acetylcholine produced by higher neuron in the cerebral cortex act as excitatory neurotransmitter.
In Parkinson’s disease an imbalance of neurotransmitters, decreased dopamine and increased acetylcholine
Results to clinical manifestions causing incoordination for unconscious muscle movements including those that control position, posture and movement
Anti – Parkinson’s drugs should balance the effects of the neurotransmitters.
These Drugs do not cure the disease but control the symptoms, hence the use is for palliative treatment.
Mechanism of Action
To increase dopamine effect
To supress acetylcholine effect
Drug Classifications
Dopaminergic Drugs
increase the effect of Dopamine at the receptor sites by increasing the levels of dopamine in the substantia nigra or directly stimulating the receptors
Pharmacokinetics
These drugs are absorbed in the GIT, metabolized in the liver and excreted in the urine.
They cross the placenta and the breast milk
Contraidication and Caution
Contraindicated to clients with allergy to the drugs and glaucoma as the drug can exacerbate glaucoma.
Caution should be used with any condition that could be exacerbated by dopamine receptor stimulation such as cardiovascular disease, bronchial asthma, peptic ulcer disease, urinary tract obstrution and psychiatric disorders.
Adverse Effects
CNS effects include anxiety, nervousness, headache, malaise, fatigue, confusion, mental changes, blurred vision, muscle twitching and ataxia.
Peripheral effects include anorexia, nausea, vomiting, diarrhea, constipation, cardiac arrythmias, urinary retention and bone marrow suppresion
Drug – Drug interaction
Dopaminergic drugs combined with MAOI may increase hypertensive crisis.
The combination of levodopa with Vitamin B6 and phenytoin and dopamine antagonists may lead to decrease effect of dopaminergic drugs.
Drug Samples
Levodopa
a precursor of Dopamine.
Once levodopa enters the BBB, it becomes dopamine and will replace the loss od dopamine.
When this drug was develop, there was a dramatic reduction in the signs and symptoms of Parkinson’s disease, however it was found out later that levodopa can be destroyed by and enzyme called dopa decarboxylase before they cross the BBB resulting to decreasing the level of levodopa that may cross the BBB.
Levodopa is combined with Carbidopa (Sinemet) to increase the level of levodopa entering BBB by inhibiting the enzyme
Best drug used for Parkinson’s
Amantadine
drug that can increase the release of dopamine.
This drug can be effective as long as there is a possibility of more dopamine release.
Bromocriptine
acts a direct dopamine agonists on dopamine receptor sites in the substantia nigra.
Anti-Cholinergic Drugs
oppose the effects of acetylcholine at receptor sites in the substantia nigra.
These anticholinergic drugs have greater affinity with the receptors of acetylcholine in the CNS than those in the periphery
However, they still block some receptors at the autonomic nervous sytem.
Blocking the acetylcholine effect help to normalize the dopamine – acetylcholine imbalance in the basal ganglia.
Pharmacokinetics
drugs absorbed in the GIT, metabolized in the liver and excreted by cellular pathways.
They pass the placenta and the breast milk
Contraindications and Cautions
Contraindicated in clients with Gastro intestinal or Genito urinary obstruction.
Caution should be used in clients with cadiovascular conditions because of its blocking effect of parasympathetic nervous system
Adverse Effects
Blocking CNS actylcholine may cause disorientation, confusion and memory loss.
Peripheral anticholinergic effect include drying of the mouth, constipation, urinary retention and orthostatic hypotension.
Drug-Drug interaction
These drugs should not be combined with other drugs with anti – cholinergic effects like anti – psychotic, anti – depressant drugs.
Drug Samples
Diphenhydramine ( Benadryl )
Benztropine ( Cogentin )
Biperiden ( Akineton )
Trihexyphenidyl ( Artane )
These drugs are famous by their brand names. Most often used for treatment of Parkinson’s like syndrome, an adverse effect of anti – psychotic drugs
Nursing Considerations
Provide sugarless lozenges to relieve drying of the mouth
Give the drugs with caution in hot weather or with exposure to hot environemtn because of increase risk for heat prostration
Give drugs with meals as they may cause GI irritation
Monitor bowel functions
Establish safety precautions
Ensure that the patient voids before taking the drugs if urinary retention is a problem
Provide thorough patient teaching about topics such as the drug name and prescribed dosage, measures help to avoid averse effects, warning signs that may indicate problems and need for pwriodic monitoring and evaluation to enhance patient knowledge about drug therapy and to promote compliance
Offer support and encouragement to help the patient cope up with the disease and drug regimen
Muscle Relaxants
Types of Spinal Reflexes
Simple - Involving an incoming sensory neuron and an outgoing motor neuron
Complex - Involving interneurons that communicate with the related centers in the brain
Mechanism
Most relaxants
Work in the brain and spinal cord
Interfere with cycle of muscle spasm and pain
Botulinum toxins and dantrolene
Enter muscle fibers directly
Work in the upper levels of the CNS to interfere with the reflexes that are causing the muscle spasm
Possible depression anticipated with their use
Lyse or destroy spasm - Often referred to as spasmolytics
Fibers in the CNS Controlling Different Types of Movements
Pyramidal tract - Controls precise intentional movements
Extrapyramidal tract - Modulates unconsciously controlled muscle activity - Allows the body to make automatic adjustments in posture, position, and balance
Neuromuscular Abnormalities
Muscle spasm
Often results from injury to the musculoskeletal system
Caused by the flood of sensory impulses coming to the spinal cord from the injured area
Muscle spasticity
Result of damage to neurons within the CNS
May result from an increase in excitatory influences or a decrease in inhibitory influences within the CNS
Baclofen
Prototype
Indication
Alleviation of signs and symptoms of spasticity; use in spinal cord injuries or diseases
Actions
GABA analog; inhibits monosynaptic and polysynaptic spinal reflexes; CNS depressant
Oral route
Onset 1 hour; peak 2 hours; duration 4–8 hours
Intrathecal route
Onset 30–60 min; peak 4 hours; duration 4–8 hours
T½
3–4 hours; excreted in the urine
Dantrolene
Indications
Treatment of spasticity directly affecting peripheral muscle contraction
Management of spasticity associated with neuromuscular diseases
Contraindications
Presence of any known allergy to the drug
Spasticity that contributes to locomotion, upright position, or increased function
Active hepatic disease
Lactation
Botulinum Toxin Type A
Prescription drug approved by the FDA in 2002
Temporarily improves the appearance of glabellar lines between the eyebrows
Four units of the drug are injected between eyebrows
Adverse effects include headache, respiratory infections, flu-like symptoms, and droopy eyelids
Nursing Considerations
Monitor patient response to the drug (improvement in muscle spasm and relief of pain; improvement in muscle spasticity)
Monitor for adverse effects (CNS changes, GI depression, urinary urgency)
Evaluate the effectiveness of the teaching plan
Monitor the effectiveness of comfort measures and compliance with the regimen
Neuromuscular Junction Blocking Agents
NMJ - point of communication between a nerve and a muscle
Sarcomere the functional unit of a muscle
Categories of NMJ Blockers
used when clinical situations require muscle paralysis
not broken down by acetylcholinesterase, hence longer effect than Ach
PREVENTS skeletal muscle function
Nondepolarizing
Act as antagonists to acetylcholine (ACh) at the NMJ
prevent depolarization ( contraction ) of muscle cells
eg. curare ( poison used to on tips of arrows or spears )
Tubocurarine
General anesthesia; skeletal muscle relaxation; reduce intensity of muscle contractions in ECT; management of mechanical ventilation
Occupies the muscular cholinergic receptor site, preventing ACh from reacting with the receptor; does not cause activation of muscle cells; causes a flaccid paralysis
Depolarizing
Act as an ACh agonist, causing stimulation of the muscle cell
causes prolonged contraction, hence prevents repolarization
Succinylcholine
Adjunct to general anesthesia; to facilitate endotracheal intubation; to induce skeletal muscle relaxation during surgery or mechanical ventilation
Combines with ACh receptors at the motor endplate to produce depolarization; this inhibits neuromuscular transmission, causing a flaccid paralysis
Action of NMJ Blockers
Both are used to cause paralysis (loss of muscular function)
For performance of surgical procedures
To facilitate mechanical ventilation
Similar in structure to ACh
Occupy the muscular cholinergic receptor site, preventing ACh from reacting with the receptor
Do not cause activation of muscle cells; muscle contraction does not occur
Not broken down by acetylcholinesterase; effect is more long-lasting than that of ACh
Used when clinical situations require muscle paralysis
Indications
As an adjunct to general anesthetics during surgery
To facilitate mechanical intubation by preventing resistance to the respirator
To facilitate electroconvulsive therapy
Evaluation of Patient Receiving NMJ
Monitor patient response to the drug (adequate muscle paralysis)
Monitor for adverse effects
Evaluate the effectiveness of the teaching plan
Monitor the effectiveness of comfort measures and compliance with the regime
Adverse Effects
Respiratory depression
Hypotension / cardiac arrythmias
Bronchospasm
→ due to histamine release of many NMJ blockers causing respiratory obstructionGI slowdown
Skin breakdown
→ Decubitus Ulcer = lost of reflex muscle movement that protects body from pressure soresFear related to helplessness and inability to communicate
Hyperkalemia
→ due to muscle membrane alterationsMalignant Hyperthermia
→ massive muscle contractions, sharply ↑ body temperature, severe acidosis and death
→ due to succinylcholine
Care for Patients
Support and reassurance – Communication is decreased with paralysis
Vigilant maintenance of airways and respiration
Prevention of skin breakdown
Monitoring for return of function
Pain relief as appropriate
Reassurance
Support
Orientation
Skin care and turning
Supportive care