Circulatory system potential SAQ questions
Principles of Hemodynamics
The relationship among blood pressure, flow and vascular resistance across the cardiovascular system.
Vascular histology
The cardiovascular system is a transport system of blood pumping.
Type of blood vessels
Arteries → Blood distribution at high pressure
Arterioles → Flow and resistance regulation
Capilalries → O2 nutrient, CO2 and fluid exchange
Venules and Veins → Capacitance vessels (high capacity to store blood and ready to accomodate changes in blood volume)
Structure follows function
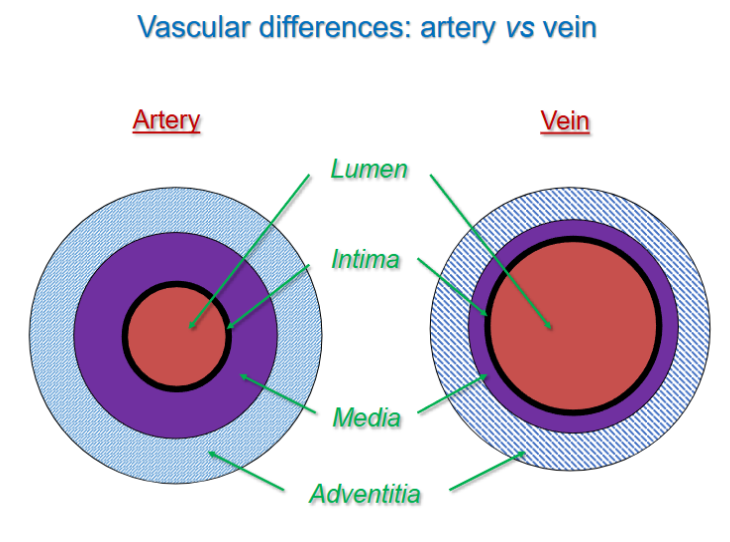
SUMMARY
Arteries:
Thick walled, musuclar, high pressure (large elastic, windkessels)
Regulate pressure and flow (small arteries and arterioles)
Veins:
Valves to prevent backflow, thin walls, collapsible
Low pressure capacitance system
Capillaries:
Extremely thin walls
Exchange vessels
Maximixed transmural diffusion
Cardiac anatomy recap
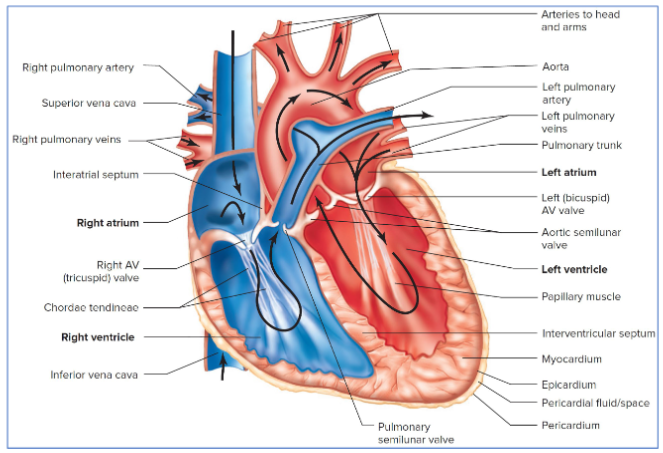
SUMMARY heart pump 1
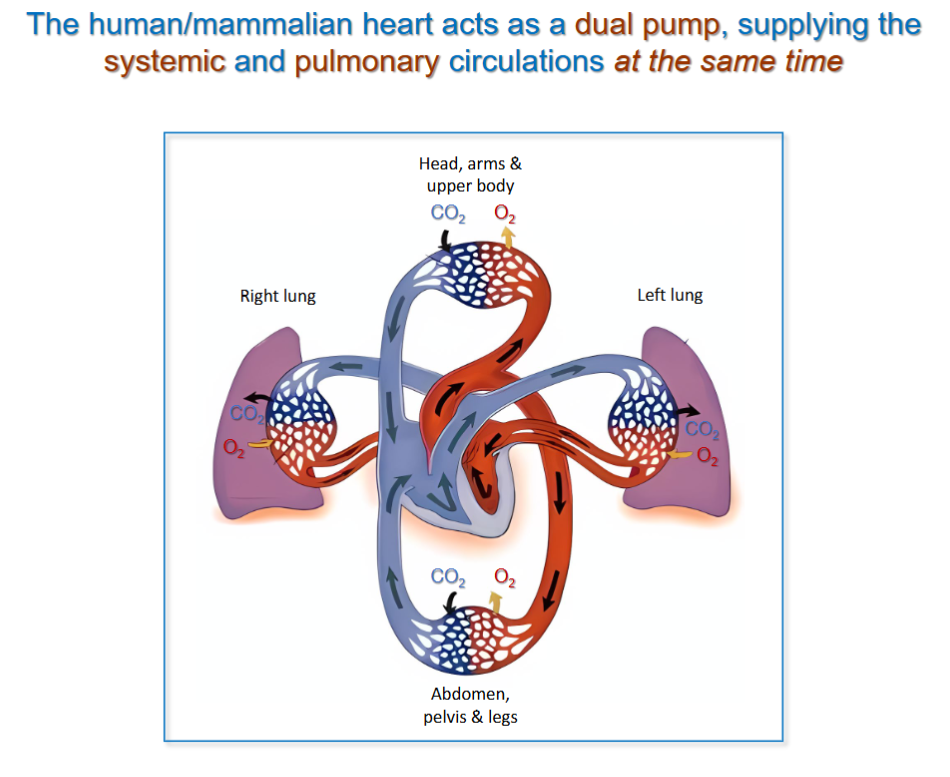
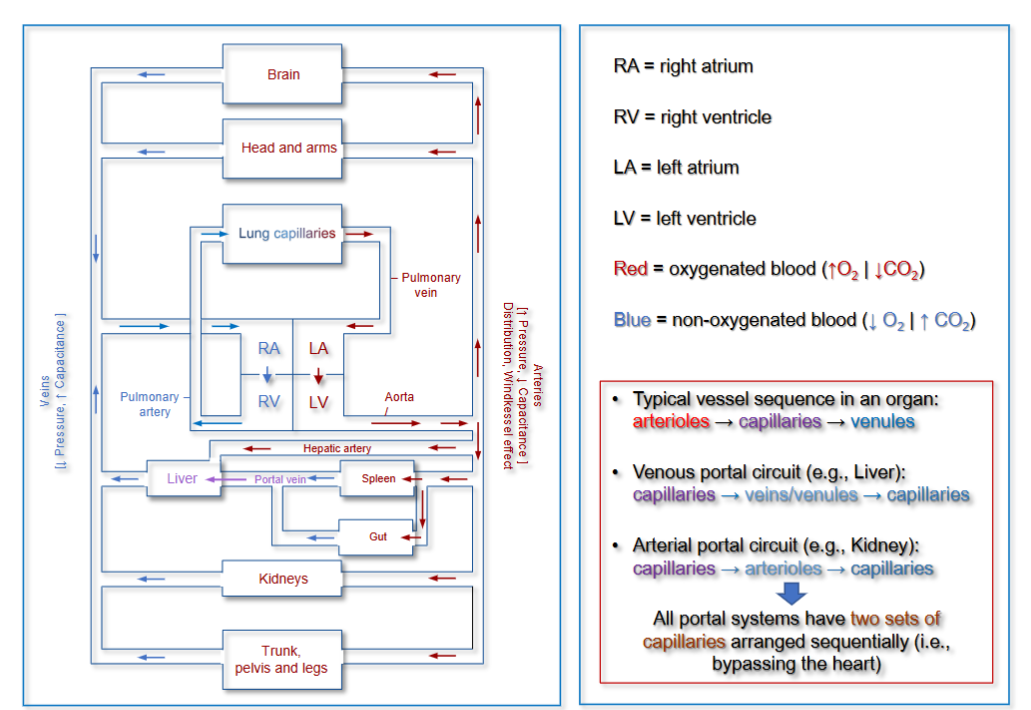
Heart functions as a dual pump linking systemic and pulmonary circuits.
Pump function depends upon the coordinated contraction (systolic function) and blood flow throughout the four cardiac chamgers (two atria and two ventricles).
Cardiac cycle descibes a coordinated sequence of electircal and mechanical events allowing efficient blood flow through the circulatory system
Cardiac output depends upon stroke volume and heart frequency, allowing a flow equaling the full blood volume to flow throughout the system in one min under resting condition.
What does this region of the CS do the blood? | How is the structure linked to the function? | What role is played for oxygenation / deoxygenation? | |
Blood vessels: Artery, Veins, Capillaries | → Artery= Carries oxygenated blood from the heart to the body. → Veins= Return deoxygenated blood to the heart. → Capillaries= Exchange of gases, nutrients, and waste between blood and tissues. | → Artery - Thick, muscular walls to withstand high pressure → Veins - Thinner walls than arteries → Capillaries - Very thin walls: Single layer of endothelial cells for efficient diffusion | → Artery - Carry oxygenated blood from the heart to the body (except pulmonary artery which carries deoxygenated blood to the lungs). → Veins - Carry deoxygenated blood back to the heart (except pulmonary veins which carry oxygenated blood from the lungs). → Capillaries - Exchange of gases (oxygen and carbon dioxide) between blood and tissues. |
The heart structure: ventricles, atrium, pulmonary vein, pulmonary artery, vena cava (superior and inferior) | → Ventricles - Left ventricle pumps oxygenated blood to the body via the aorta. → Atria - Right atrium receives deoxygenated blood from the body via the vena cava. → Pulmonary vein - Carries oxygenated blood from the lungs to the left atrium. → Pulmonary artery - Carries deoxygenated blood from the right ventricle to the lungs for oxygenation. → Vena cava - Superior vena cava carries deoxygenated blood from the upper body to the right atrium. | → Ventricles - Left ventricle: Thick muscular walls to generate high pressure. → Atria - Thin-walled, less muscular than ventricles. → Pulmonary vein - Endothelium: Simple squamous epithelium. → Pulmonary artery - Thick muscular walls to withstand pressure from the right ventricle. → Vena Cava - Thin-walled, large lumen for low-pressure blood return. | → Ventricles - Left ventricle pumps oxygenated blood to the body via the aorta. → Atria - Right atrium receives deoxygenated blood from the body via the vena cava. → Pulmonary vein Carries oxygenated blood from the lungs to the left atrium. → Pulmonary artery - Carries deoxygenated blood from the right ventricle to the lungs for oxygenation. → Vena cava - Superior vena cava brings deoxygenated blood from the upper body to the right atrium. |
Cardiac pacemaker activity refers to the electrical impulses generated by specialized cells in the heart, primarily located in the sinoatrial (SA) node. These cells have automaticity, meaning they can initiate action potentials without external stimuli. The SA node sets the pace of the heart, triggering contraction by stimulating the atria, followed by the atrioventricular (AV) node, bundle of His, and Purkinje fibers. This coordinated electrical activity ensures rhythmic heartbeats, maintaining proper heart rate and circulation.
Principles of hemodynamics?
Hemodynamics refers to the principles governing blood flow in the circulatory system. Blood flow is driven by a pressure gradient, moving from areas of high to low pressure, and is opposed by vascular resistance. According to Ohm’s Law, blood flow (Q) is directly proportional to the pressure difference (ΔP) and inversely proportional to resistance (R), expressed as Q = ΔP / R. Resistance is mainly determined by vessel diameter, with small changes causing large effects due to the Poiseuille’s Law, where resistance is inversely proportional to the fourth power of the radius. Blood flow can be laminar (smooth and efficient) or turbulent, which increases resistance and occurs in conditions like high velocity or vessel narrowing. Viscosity and vessel length also influence resistance. Hemodynamics ensures effective tissue perfusion and is regulated by neural, hormonal, and local mechanisms.
Starling principle?
describes the movement of fluid across capillary walls and explains how fluid exchange is regulated between the capillaries and interstitial space. It is governed by the balance of hydrostatic pressure (which pushes fluid out of capillaries) and oncotic pressure (which pulls fluid back into capillaries due to plasma proteins). At the arterial end of a capillary, hydrostatic pressure is higher than oncotic pressure, leading to filtration of fluid into the interstitial space. At the venous end, oncotic pressure exceeds hydrostatic pressure, resulting in reabsorption of fluid back into the capillaries. Any imbalance in these forces can lead to edema, such as increased hydrostatic pressure or decreased plasma proteins. The revised Starling model also emphasizes the role of the glycocalyx layer in regulating this exchange.
The cardiac cyle (heart as a pump)
The cardiac cycle is a series of events that occur during a single heartbeat, consisting of systole (contraction) and diastole (relaxation). It begins with atrial systole, where the atria contract, filling the ventricles with blood. During ventricular systole, the ventricles contract, raising pressure and forcing the AV valves (mitral and tricuspid) to close, causing the first heart sound (S1). This is followed by ventricular ejection, where blood is pumped into the aorta and pulmonary artery once ventricular pressure exceeds arterial pressure. In ventricular diastole, the ventricles relax, and the semilunar valves (aortic and pulmonary) close, causing the second heart sound (S2). The ventricles then fill with blood during ventricular filling as the AV valves open. Throughout this cycle, ventricular pressure rises during contraction and falls during relaxation, while atrial and venous pressures reflect changes in blood volume and flow. Heart sounds, S1 and S2, correspond to the closing of the AV and semilunar valves, respectively.
Describe the structure and function of different types of blood vessels.
Arteries carry blood away from the heart under high pressure and have thick, elastic walls. Veins return blood to the heart under lower pressure and have valves to prevent backflow. Capillaries are thin-walled and allow exchange of gases, nutrients, and waste between blood and tissues.