Hepatic System Part 2 (cholesterol)
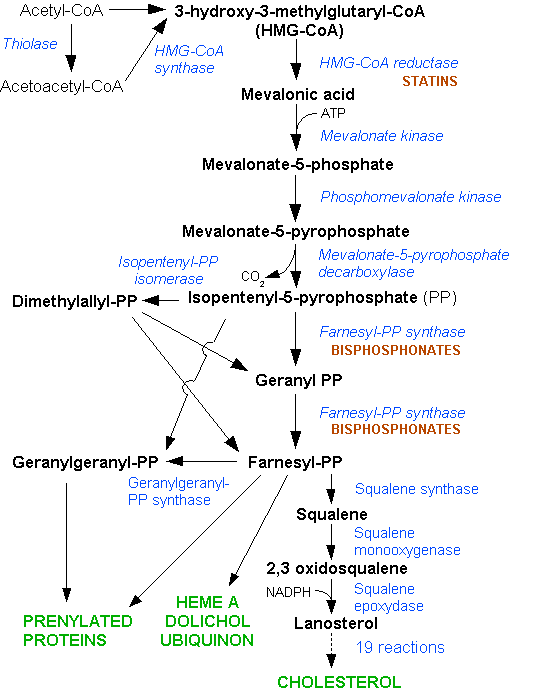
Cholesterol is found in all body cells as part of the cell membrane. 75% is synthesised in the body and the remaining 25% comes from the diet. Cholesterol is primarily synthesised in the liver, in the cytoplasm and endoplasmic reticulum. Small amounts are also synthesised by the lining of the small intestine and the individual cells of the body. The rate limiting step of cholesterol synthesis is the HMG-CoA reductase reaction. This reaction is highly regulated and is often the target of pharmacological intervention.
 Triparanol is a drug which inhibits a late step in the pathway, however it was withdrawn shortly after its introduction in the mid 1960s due to various cutaneous adverse effects and development of cataracts. These side effects were due to desmosterol accumulation, which is the substrate of the inhibited enzyme.
Triparanol is a drug which inhibits a late step in the pathway, however it was withdrawn shortly after its introduction in the mid 1960s due to various cutaneous adverse effects and development of cataracts. These side effects were due to desmosterol accumulation, which is the substrate of the inhibited enzyme.
Cholesterol reduces membrane permeability as its -OH group interacts with the polar heads of membrane phospholipids and sphingolipids while the steroid and hydrocarbon chain are embedded in the membrane, increasing packing together of the membrane.
Sex hormone production: cholesterol involved in producing progesterone, oestrogen and testosterone.
Adrenal hormones: cholesterol essential for production of hormones released by adrenal gland eg cortisol and aldosterone.
Cortisol increases blood sugar levels through gluconeogenesis and aids in fat, protein and carbohydrate metabolism.
Aldosterone control blood pressure by regulating sodium and potassium levels.
Digestion: cholesterol aids in bile acid production. Bile acids work to digest food in the intestines.
Insulation: cholesterol insulates nerve fibres.
Cholesterol is also involved in the process of synthesising vitamin D from sunlight.
High cholesterol levels can lead to heart issues.
Atherosclerosis is the narrowing of the arteries which increases risk of coronary heart disease. Coronary heart disease is an abnormality in the arteries supplying oxygenated blood to the heart.
Heart attacks occur when blood supply to the heart is blocked, usually by a clot in the coronary artery leading to death of heart muscle.
Angina is the chest pain/discomfort which occurs when the heart muscle doesn’t receive enough blood.
Stroke/mini-strokes occur when a blood clot blocks an artery/vein involved in blood supply to the brain. Also occurs as a result of a blood vessel breaking (aneurysm).
Plaques which build up in the arteries may rupture and enter the blood stream, which may lead to blockage of the coronary or carotid arteries in a worst case scenario.
There are several different classifications of lipoproteins: chylomicrons, very low density lipoproteins (VLDL), intermediate density lipoproteins (IDL), low density lipoproteins (LDL) and high density lipoproteins. The lower the density, the more the fat to protein ratio is increased.
Cholesterol is insoluble in the blood so is transported throughout the circulatory system via lipoproteins. LDLs carry cholesterol from the liver to cells and if more is carried than the cells can use, the LDL build up is harmful and can increase risk of arterial disease. Most human blood contains approx 70% LDL.
HDL carries cholesterol away from cells back to the liver, where cholesterol is either broken down or expelled from the body as waste.
Chylomicrons carry triglycerides from the intestine to the liver, skeletal muscle and adipose tissue.
VLDLs carry newly synthesised triglycerides from the liver to adipose tissue.
IDLs usually aren’t detectable in the blood.
Risk factors for high blood cholesterol include diet, medical conditions, genetics, sex, age, smoking, inactivity and obesity.
Diet: eating foods high in saturated fats and cholesterol raises levels of total cholesterol and LDLs
Diabetes: high blood sugar → higher LDL cholesterol and lower HDL cholesterol. Also damages artery linings.
Hypertension: increased pressure on artery walls causes damage which can increase accumulation of fatty deposits.
Sex: males have greater risk of high blood cholesterol than females.
Age: 55+ is a risk factor
Smoking: damages walls of blood vessels so they’re more likely to accumulate fatty deposits. May also decrease HDL levels.
Inactivity and obesity: physical inactivity can increase levels in LDL cholesterol. Cardio stimulates body to provide more oxygenated blood to meet body’s needs, keeping heart strong and clearing arteries. Obesity may increase triglycerides and LDLs and decrease HDLs.
Hyperlipidaemia may be familial (primary) or acquired (secondary). Secondary hyperlipidaemia results from another underlying disorder leading to alterations in plasma lipid and lipoprotein metabolism. May also be idiopathic.
Statins inhibit an early, rate limiting step in cholesterol biosynthesis.