W11: IMAGING THROUGH THE LIFESPAN - Specialised adolescent bone disease including scoliosis imaging
Specialised Adolescent Bone Disease Including Scoliosis Imaging
Introduction
MRTY3119 - Imaging through the lifespan, Week 11 - 2025.
Focusing on specialized adolescent bone disease, including scoliosis imaging.
Case Study
A 4-year-old patient who tripped and now has a sore tummy.
Several CT scan images are presented with various parameters:
Ex: 436, Se: 2, Im: 12-C to 17+C
XY coordinates ranging from 147.50 Ax to 166.25 Ax
DFOV 20.0cm, STND (Standard), KV 120, mA 180, A 87
Image dates: Aug 02 2007, 09:50:19 AM
512X512 resolution, Mag-1.00 magnification
Adolescence
Adolescence is derived from the Latin word "adolescere," meaning "to grow up."
It is a transitional stage of physical and psychological human development, generally occurring from puberty to legal adulthood.
Most closely associated with the teenage years.
Adolescents are still growing, and their bodies' response to injuries, infections, and deformities can differ significantly from adults.
The Age of Adolescence
Defines adolescence and its sub-stages according to age ranges:
Children, school-aged children, childhood. Adolescence can be divided into younger (or early) adolescents and older adolescents and teenagers. Emerging adults, young adults, adults.
The graphic illustrates the "New Adolescence,"
Common Causes for Limp According to Age
1-3 years:
Infection, occult trauma, neoplasia.
4-10 years:
Infection, transient synovitis, Perthes’ disease/avascular necrosis, rheumatologic disorder, trauma, neoplasm
Transient synovitis: temporary inflammation of the hip joint resulting from a viral infection or trauma, often presenting with hip pain and limping in children.
Perthes’ disease: a childhood condition where the blood supply to the head of the femur is temporarily disrupted, leading to bone death and subsequent hip pain, limping, and reduced range of motion.
Rheumatologic disorder: a group of diseases that cause chronic inflammation and pain in the joints, muscles, and connective tissues, often manifesting in adolescents as joint swelling, stiffness, and physical limitations.
Neoplasm: an abnormal growth of tissue that can be benign or malignant, which may arise in the bone and cause pain, structural deformities, or complications during adolescence.
10-19 years:
Slipped upper femoral epiphysis, rheumatologic disorder, trauma, neoplasm.
Adolescent Bone Pathology
Overview of various bone pathologies common in adolescents.
SUFE (SCFE) - Slipped Upper (Capital) Femoral Epiphysis
A Salter-I fracture of the upper femoral epiphysis.
Mostly idiopathic but possibly linked to growth spurts, hormonal factors, defective growth plate, genetics, and trauma.
Idiopathic: The exact cause is unknown, but it often occurs during periods of rapid growth in adolescents.
Females: Typically occurs between 11-14 years.
Males: Typically occurs between 13-16 years.
Affected patients are often overweight.
More common in boys.
Bilateral and asymmetric in 20-32% of cases.
Patients hold their leg in slight external rotation and have limited internal rotation.
Klein’s line should intersect with the outer portion of the femoral epiphyses; failure indicates SCFE.

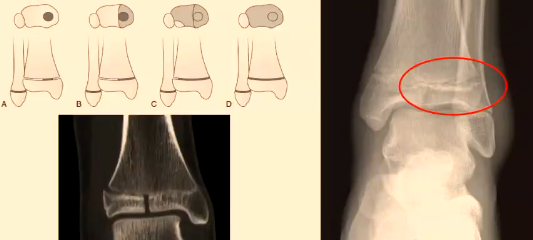
Tillaux Fractures
Occur in early teens during distal tibial physis fusion.
The distal tibial physis fuses in the medial central physis first.
Classified as transitional fractures due to this fusion process.
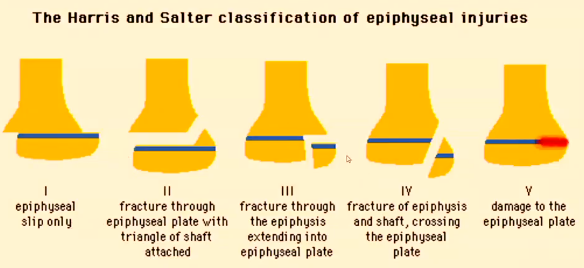
The Harris and Salter Classification of Epiphyseal Injuries
Type I: Epiphyseal slip only.
Type II: Fracture through the epiphyseal plate with a triangle of the shaft attached.
Type III: Fracture through the epiphysis extending into the epiphyseal plate.
Type IV: Fracture of epiphysis and shaft, crossing the epiphyseal plate.
Type V: Damage to the epiphyseal plate.
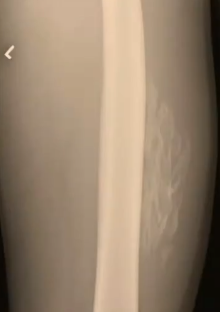
Myositis Ossificans
More common in adolescents, especially athletes, but not unique to them.
Clinical Features:
Pain, palpable mass, limited range of motion.
Often post-traumatic, secondary to direct injury.
Radiologic Findings (subacute phase, 5 weeks post-injury):
Dense, sheet-like calcifications within the muscle.
Distinct separation between the lesion and underlying bone.
Acute Osteomyelitis
Majority of cases in children are secondary to haematogenous spread or associated with a predisposing condition or penetrating injury.
Haematogenous spread: The infection is introduced into the bloodstream, allowing bacteria to infect the bone, which is particularly concerning in the growing skeleton during adolescence.
Osteomyelitis: Infection to the bone
In children over one year old, it usually affects the metaphysis due to reduced blood flow.
Presentation: pain, refusal to weight bear, systemic toxicity.
Tibial Osteomyelitis
Radiograph shows an aggressive lesion in the proximal left tibial metaphysis with a moth-eaten appearance, wide zone of transition, and periosteal reaction.
Bone destruction and periosteal reaction are usually evident on plain film by day 10-14.
Early treatment may prevent radiographic findings from developing.

Chronic Osteomyelitis
A low-grade, recurrent infection characterized by:
Bone sclerosis: This refers to an increase in bone density and is commonly seen in chronic osteomyelitis as the body attempts to wall off the infection.
Brodie abscess: Accumulation of pus in the bone
Sequestra: segments of necrotic bone that become separated from the surrounding healthy bone, often resulting from the infection.
Sinus tracts: These are channels that develop beneath the skin, allowing for the drainage of pus from infected areas of the bone to the surface.
Sequestrum: An area of devitalized bone surrounded by inflammation, appearing as a fragment in a region of bone sclerosis.

Brodie Abscess
A focal area of chronic osteomyelitis that may develop de novo or in a previous acute osteomyelitis site and contains fluid.
Radiograph shows an ill-defined osteolytic lesion with extensive reactive bone sclerosis.
Juvenile Idiopathic Arthritis (JIA)
A chronic inflammatory arthritis of unknown etiology.
Initial radiographs may be normal or show the acute inflammatory response accompanying synovial hypertrophy, leading to:
Soft tissue swelling.
Periarticular osteopenia.
Epiphyseal remodeling and widening.
Prolonged synovial proliferation leads to loss of cartilage and bone damage.
Progressive damage can lead to bony ankylosis.

Bone Tumours
Most common cancers in individuals < 20 years old:
Leukemia (30%).
Brain tumors (22%).
Lymphoma (11%).
Neuroblastoma (8%).
Soft tissue sarcomas (7%).
Nephroblastoma - Wilms tumor (6%).
Bone tumors (5%).
Most common malignant bone tumors: osteosarcoma (OS) and Ewing’s sarcoma (ES).
Osteosarcoma: A malignant tumor that primarily affects the long bones, particularly in adolescents, and is characterized by the production of osteoid tissue.
Ewing’s sarcoma: A highly aggressive malignant bone tumor that typically arises in the bones of the pelvis, legs, and arms, usually affecting adolescents and young adults, and is associated with a specific genetic translocation that promotes tumor growth.
Diagnostic imaging is critical for differentiating benign from malignant lesions and staging tumors.
Cancer is the most common non-traumatic cause of death in infants and adolescents.
Approximately 1000 children and adolescents are diagnosed with cancer annually in Australia.
The survival rate for childhood cancer is generally 80%.
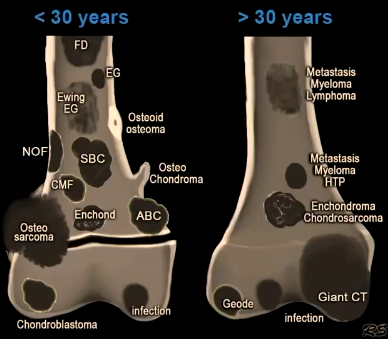
Seven Questions to Ask When Assessing Bone Lesions
Where is the lesion located?
How large is the lesion?
What is the lesion doing to the bone?
How is the bone responding?
Is the lesion producing a matrix?
Is a soft tissue mass evident?
How old is the patient?
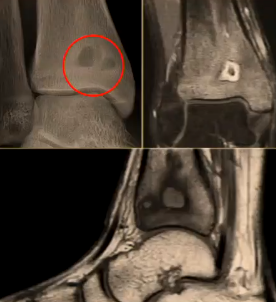
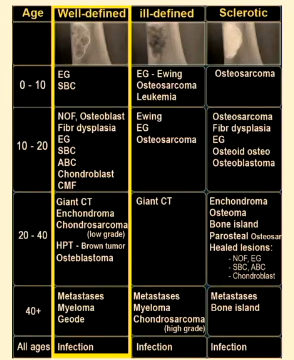
Legend of Abbreviations (Bone Lesions)
ABC = aneurysmal bone cyst
CT = cell tumour
FD = fibrous dysplasia
SBC = simple bone cyst
NOF = non-ossifying fibroma
EG = eosinophilic granuloma
Enchond = enchondroma
HTP = Browns tumours result of hyperparathyroidism
CMF = chondromyxoid fibroma
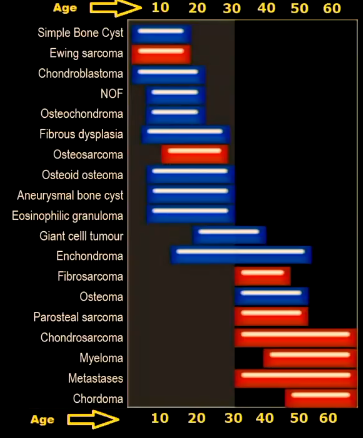
Bone Tumor Types & Age Distribution
Chart depicting the occurrence of various bone tumors across different age groups (10-60 years):
Simple Bone Cyst, Ewing sarcoma, Chondroblastoma, NOF, Osteochondroma, Fibrous dysplasia, Osteosarcoma, Osteoid osteoma, Aneurysmal bone cyst, Eosinophilic granuloma, Giant cell tumor, Enchondroma, Fibrosarcoma, Osteoma, Parosteal sarcoma, Chondrosarcoma, Myeloma, Metastases, Chordoma.
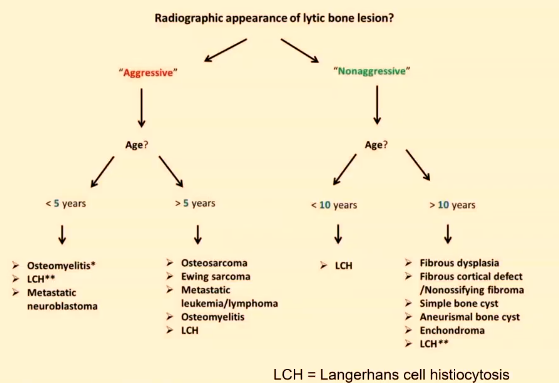
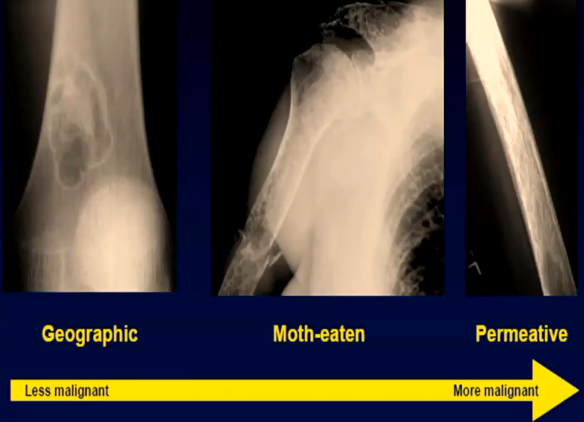
Radiographic Appearance of Lytic Bone Lesions
Algorithm for Assessing Lytic Bone Lesions:
"Aggressive" Lesion:
Age < 5 years: Osteomyelitis, LCH (Langerhans Cell Histiocytosis), Metastatic neuroblastoma.
Age > 5 years:
< 10 years: LCH, Osteosarcoma, Ewing sarcoma, Metastatic leukemia/lymphoma, Osteomyelitis.
> 10 years: Fibrous dysplasia, Fibrous cortical defect/Nonossifying fibroma
"Nonaggressive" Lesion:
Simple bone cyst, Aneurysmal bone cyst, Enchondroma.
Characteristics of Bone Lesions
Geographic:
Less malignant
Moth-eaten/Permeative:
More malignant.
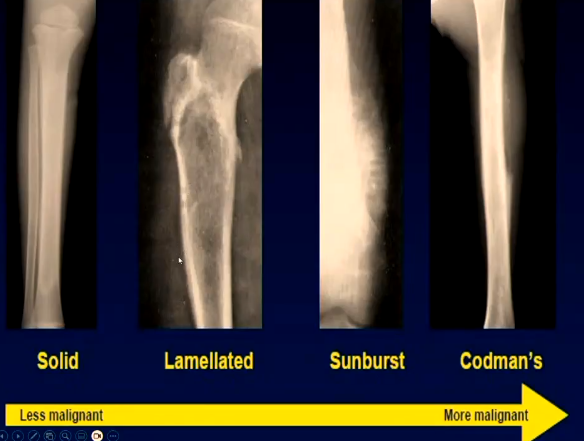
Periosteal Reaction
Periosteal reaction: a response of the periosteum to inflammatory processes, trauma, or tumor presence, often characterized by new bone formation.
Types:
Single layer
Onion skin (Lamellated)
Hair on end
Codman's triangle
Sun burst
Solid = Less malignant, sunburst/codman's = more malignant

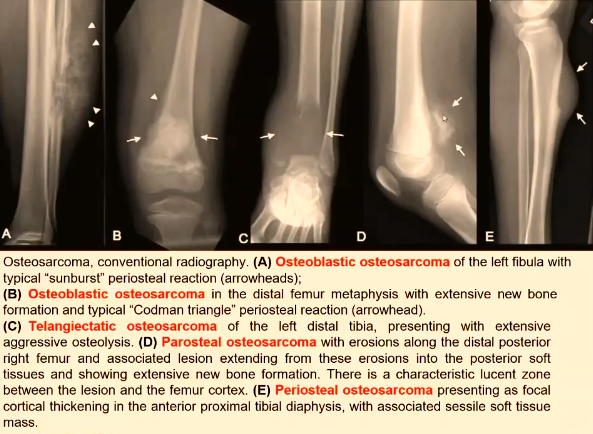
Osteosarcoma
Presents more often in adolescent boys.
20% have metastasized at discovery (60% to lung).
Symptoms:
Progressive pain.
Palpable mass.
Limping.
Pathological fracture.
Not very responsive to radiation (used palliatively).
Most common malignant bone tumour in children, typically presenting in teenagers, commonly develops in the metaphyses of long bones like the distal femur, proximal tibia, proximal humerus and proximal femur
Conventional radiography
Osteoblastic osteosarcoma will present with "sunburst" periosteal reaction
Osteoblastic osteosarcoma in the distal femur metaphysis presents with "Codman triangle" periosteal reaction.
Ewing’s Sarcoma
Arises in nerve tissue, bone marrow, & soft tissue.
Greatest occurrence between ages 4 & 25 (peaks between 10 & 20).
Highly malignant.
Metastasis approximately 33% at diagnosis, commonly spreads to the lungs, bone, and bone marrow.
Symptoms:
Pain, swelling, fractures.
Treatment similar to osteosarcoma.
More responsive to radiation.
Long term survival rate is about 65%.

Osteoid Osteoma
Common benign tumor of bone.
Predominantly in boys, usually in the second decade of life.
Composed of a nidus surrounded by dense sclerotic bone.
May develop in any bone; femoral neck most common, then tibia.
Aspirin relieves pain in 75% of patients.
Traditional treatment is surgical excision.
Osteogenesis Imperfecta
Four types with varying severity.
Type 1 is mild, Type 2 is perinatal lethal, Type 3 is progressively deforming, Type 4 is moderate-severe.
Hallmark: severe osteopenia and fractures.
Osteopenia: a condition characterized by lower than normal bone density, leading to an increased risk of fractures and skeletal deformities.
Bowing.
Blue sclera is an important clinical finding.
Hereditary Multiple Exostoses (Diaphyseal Aclasia)
Characterized by cartilage-capped exostoses – osteochondromas – that arise near the diaphyseal side of the physeal line.
Exosteses: bony growths that can cause pain and restrict movement, frequently leading to complications if they impinge on nearby structures.
Osteochondromas grow while growth plates are open and cease when growth plates fuse.
Affects long bones of arms and legs.
Grow adjacent to joints.
Osteochondromas point away from the joint.
Pts usually males.
Osteochondromas present in the first decade of life.
Patients have mild shortness of stature.

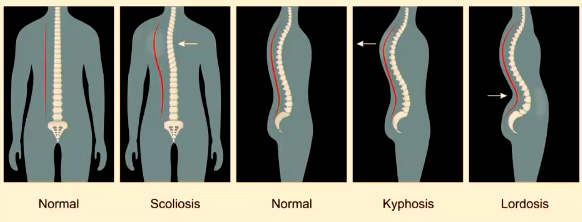
Spinal Disease
Conditions:
Normal.
Scoliosis.
Kyphosis.
Lordosis.
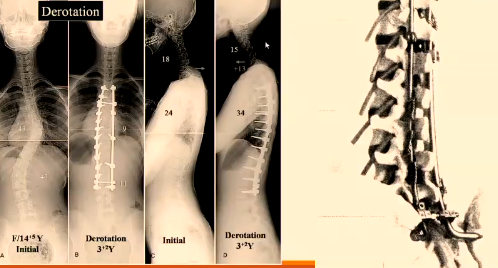
Scoliosis
Most common type: Idiopathic.
Adolescent Idiopathic Scoliosis (AIS): Occurs in adolescents (11-18yo), represents approximately 90% of all scoliosis in children.
AIS is 1.5-3 times more frequent with girls and increases in severity with age.
Other types of idiopathic scoliosis: infantile, juvenile, adult.
Other types of scoliosis: congenital, neuromuscular.
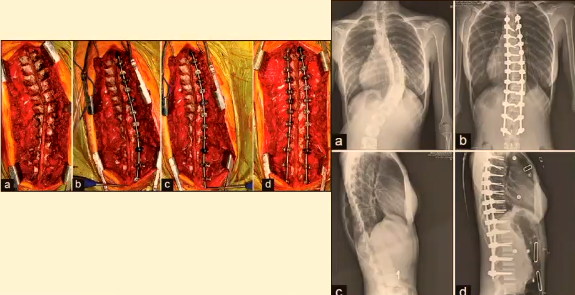
AIS is the most common presenting for surgery however the CONGENITAL SCOLIOSIS group have the largest complication rate following surgery.
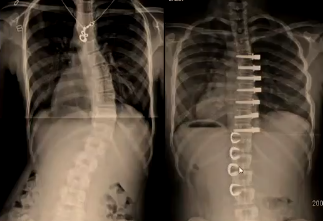
Surgery involves instrumentation (screws, rods, hooks) to reduce scoliosis and stabilize the spine to allow bone fusion.
Instrumentation is intended to be temporary and removed later and if bone fusion doesn't heal the rods will break.
Idiopathic Scoliosis
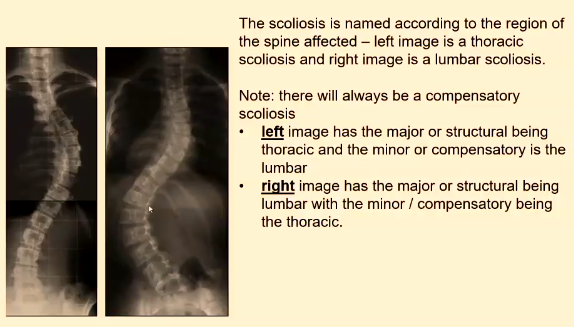
Named according to the region of the spine affected (thoracic, lumbar).
Always has a compensatory scoliosis.
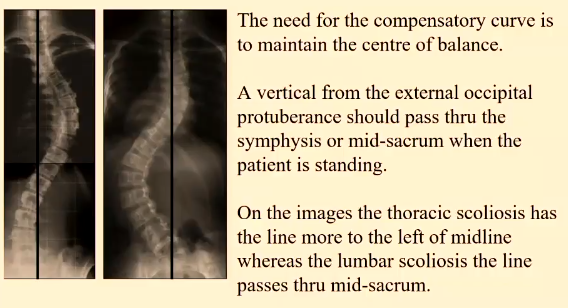
Compensatory curve maintains the center of balance.
A vertical line from the external occipital protuberance should pass through the symphysis or mid-sacrum.
Scoliosis Clinical Appearance
A noticeable Rib hump on the right side is visible on forward bend test due to vertebral rotation.

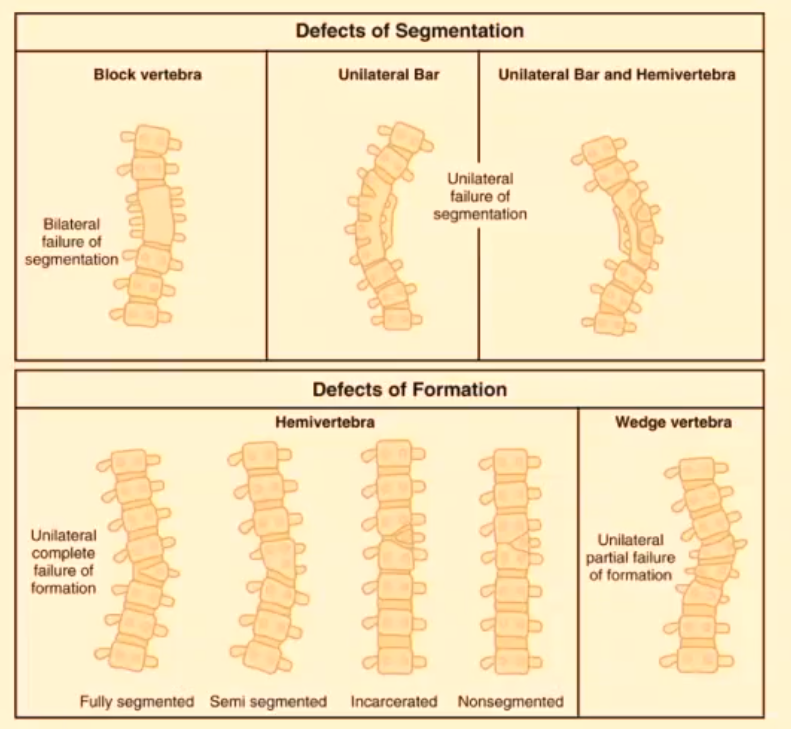
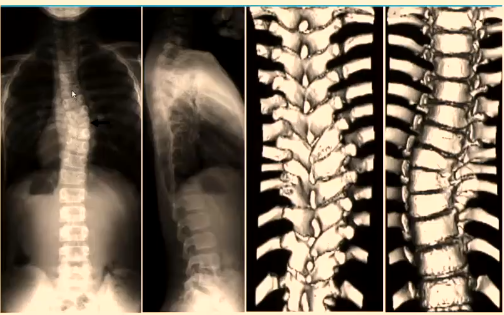
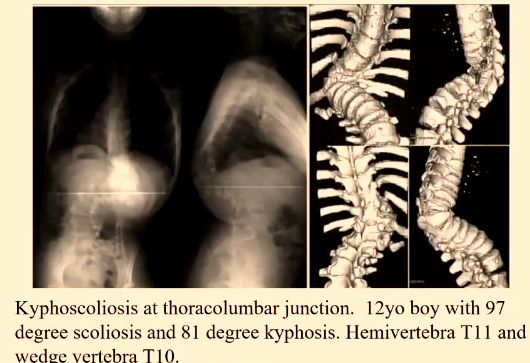
Congenital Scoliosis
Caused by an in-utero developmental defect in the spinal column.
Examples: unsegmented bar, wedge vertebra, hemivertebra, kyphoscoliosis.
Imaging Modalities for Scoliosis
Plain DR or CR PA and lateral images with image stitching.
Performed standing or sitting.
Grid must be used.
Performed PA with breast shielding.
Needs to include thoracic and lumbar plus the iliac apophysis.
Lateral may not be required for subsequent imaging and arms extended at 90 degrees to body.
EOS 2D/3D Imaging system.
Performs simultaneously an AP and lateral.
Can perform spinal imaging or entire body (leg length).
Uses scanning slit technology without a grid.
Software can produce 3D reconstruction.
EOS imaging is performed at a much lower dose due to the product configuration and the unique detection technology.

CT:
Defines involved anatomy with congenital scoliosis.
Determines the degree of vertebral rotation.
Is not used a progress imaging modality.
MRI:
Used predominantly for scoliosis due to a neuromuscular condition or a congenital scoliosis.
Ultrasound vs. X-ray:
Spine ultrasound used with Scolioscan system
The correlation between Ultrasound Coronal Angle (UCA) and Radiographic Cobb Angle (RCA).
Measuring Angle of Scoliosis
Define the upper and lower end vertebrae.
Identify Apical vertebra.
Determine Major/primary curve.
Identify Compensatory/secondary curve.
Cobb gives the angle measurement in degrees.
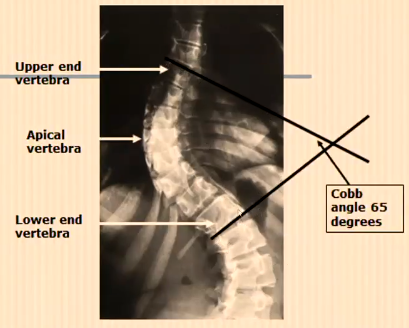
Cobb Angle and Severity of Scoliosis
A 10-degree Cobb angle is the threshold for scoliosis.
Most people are unaware of their scoliosis even when it exceeds 30 degrees.
There can be up to a 14-degree difference in Cobb angle between standing and lying.
RISSER SCORE and Relationship to Progression of Scoliosis
Indicates iliac apophysis appearance (1-5) and fusion with ilium (5).
Risser 0-1 = curves between 20-29 degrees have a > 65% risk of progression.
Risser 2-4 = curves between 20-29 degrees have a > 20% risk of progression.
Instrumentation Systems in Chronological Order
Harrington system (Distraction-compression) mid-late 1980s.
Luque instrumentation system.
Cotrel-Dubousset method (CD instrumentation system) - 1980s onwards (Simple rod rotation).
Rod Translation.
Cantilever bending technique.
Direct vertebral rotation.
Vertebral co-planar alignment.
Simultaneous double rod rotation.
Uncar convex rod rotation.
Types of Instrumentation
Harrington rods: Prone to failure due to pedicle hooks becoming detached or rods breaking.
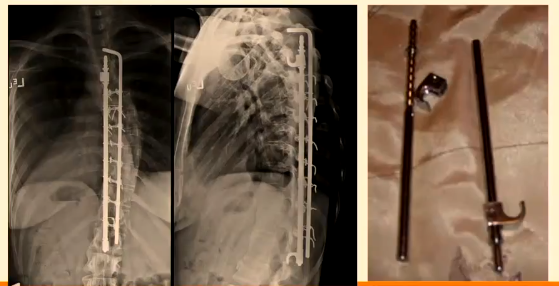
Luque or Luque-To: Used more for correcting neuromuscular scoliosis and uses wire loops around pedicle rather than pedicle hooks.

CD Instrumentation: Uses pedicle screws rather than wire loops and also employs rods, and transverse stabilizing bars that can be bent (contourable) and works on rotating the vertebra. Failures are due to infection.
Uncar convex rods rotation uses multiple pedicle screws
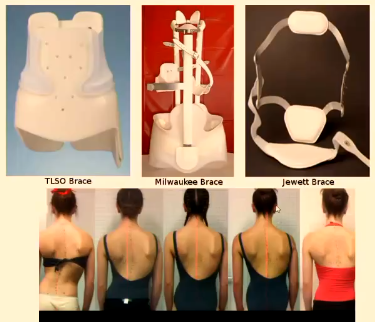
Managing a Patient with a Growing Spine
Stabilize the patient's spine until skeletal growth has completed.
Conservatively using a brace.
Surgical, allowing a flexible restraint that will stabilize the amount of curvature BUT it does not involve bone fusion.
Braces
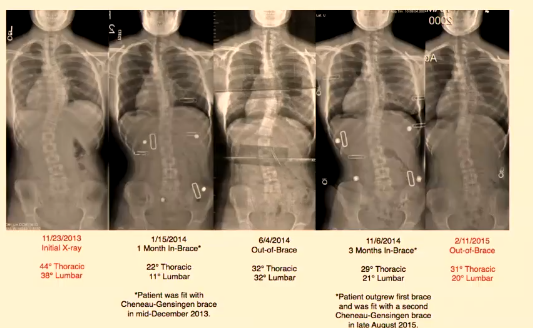
Example of a patient's scoliosis management using braces.
Patient was fit with Cheneau-Gensingen brace.
Initial X-ray: 44° Thoracic, 38° Lumbar.
1 Month In-Brace: 22° Thoracic, 11° Lumbar.
Months In-Brace: 29° Thoracic, 21° Lumbar.
Vertebral Flexible Tethering
A flexible restraint that will stabilize the amount of curvature BUT it does not involve bone fusion.
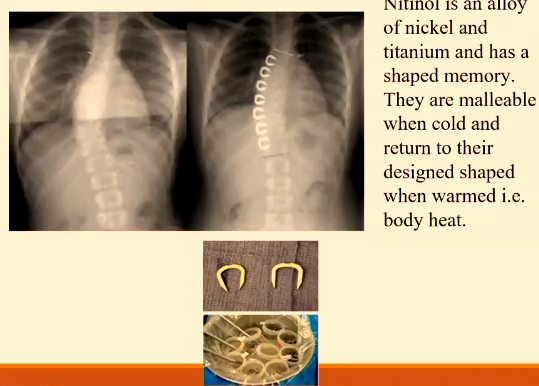
Vertebral Stapling Using Nitinol
Nitinol is an alloy of nickel and titanium and has a shaped memory.
They are malleable when cold and return to their designed shape when warmed i.e. body heat.