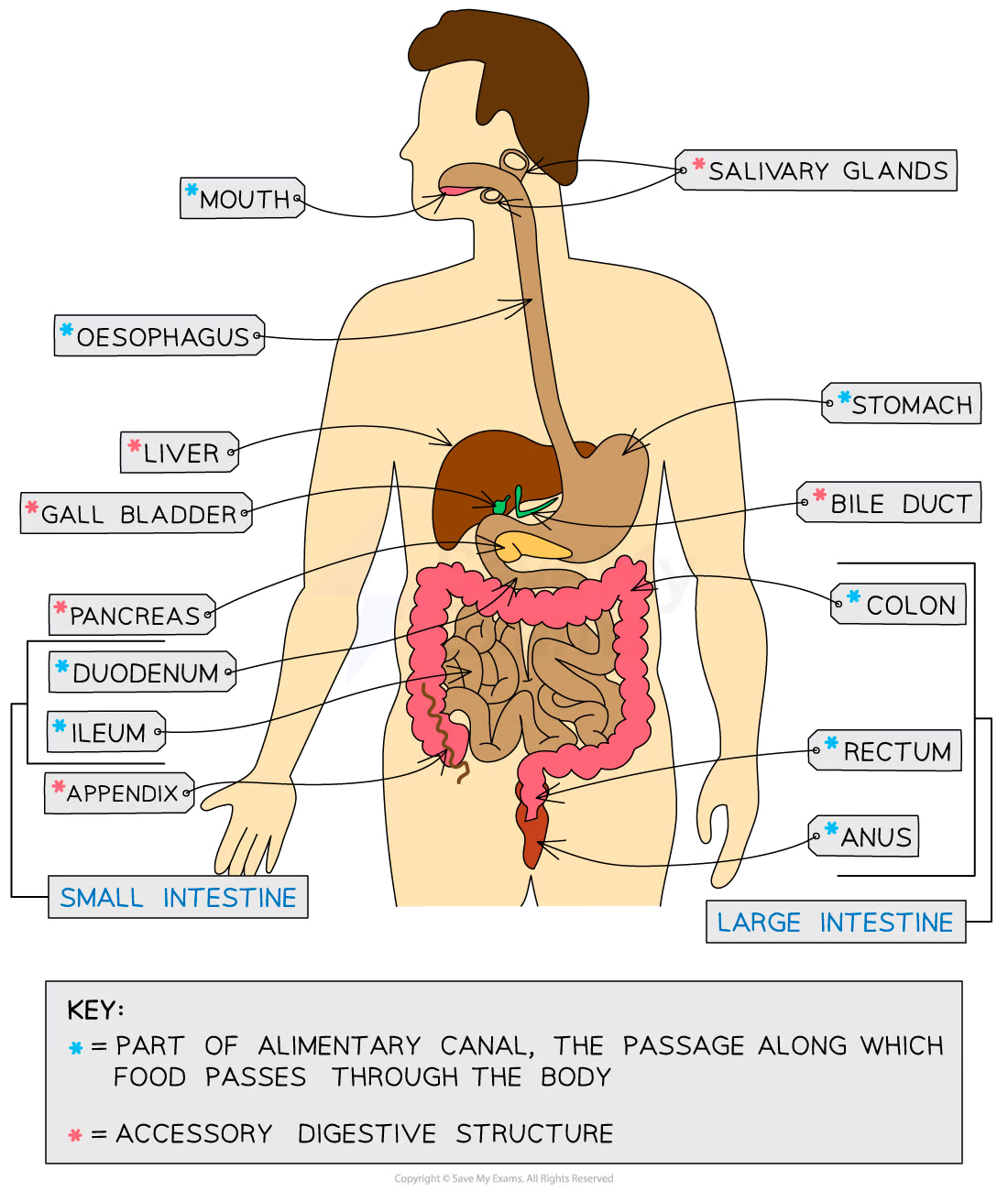
Gastrointestinal Physiology
GI anatomy
Gastrointestinal Physiology
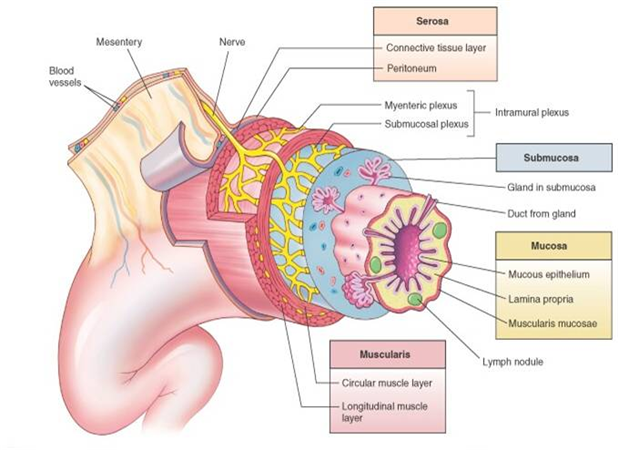
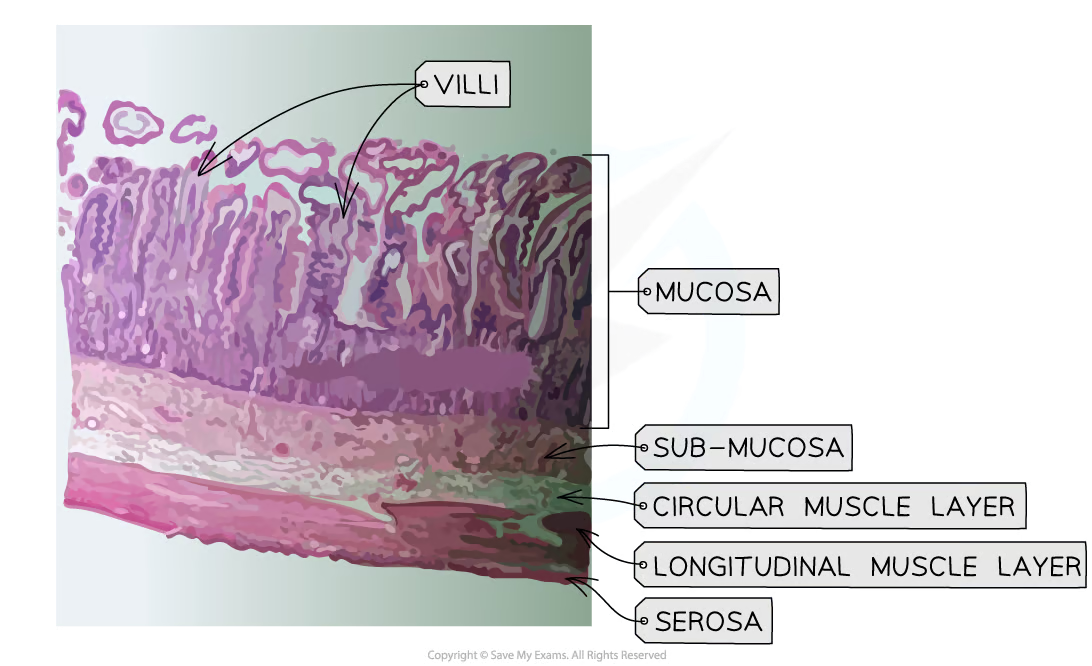
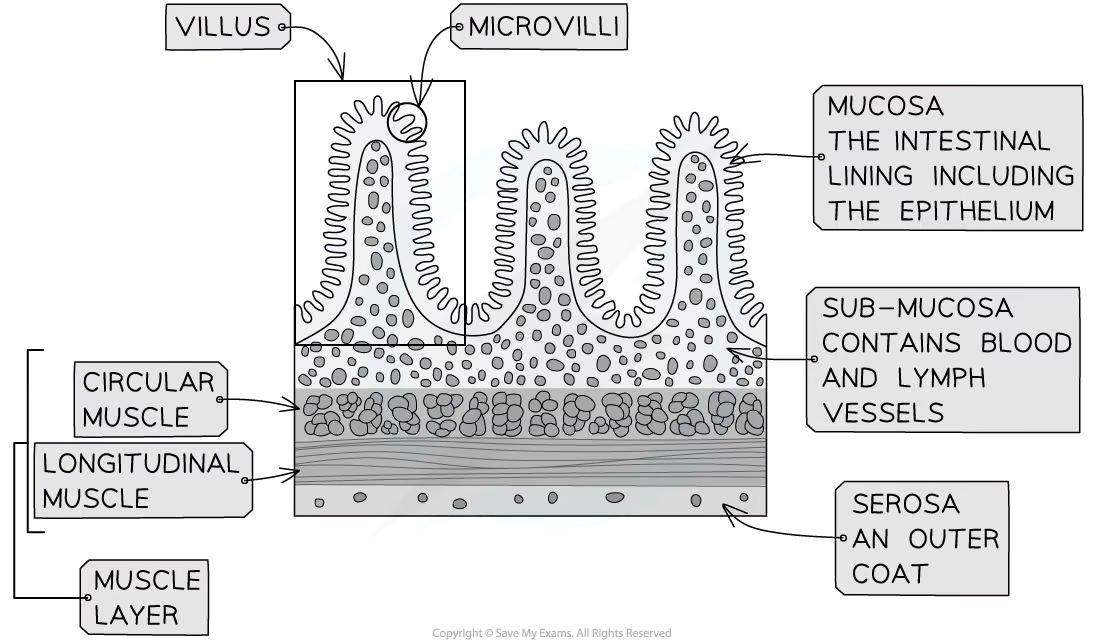
General histological organization of the GI tract
5 layers (from inner most to outermost layers)
Mucosa
mucous epithelium
lamina propia
muscularis mucosae
Submucosa
Muscularis
circular muscle layer
longitudinal muscle layer
Serosa
connective tissue layer
peritoneum
What modulates the GI track?
Enteric nervous system (ENS) → nerve network located in the GI tract and controlls the motility and secretory functions of it
also known as the “little brain of the gut”
contains sensory mechanoreceptors and chemoreceptors
Composed of 2 plexuses:
Myenteric plexus (Auerbach’s plexus)→ found in the muscularis externa
controls motility function of the GI track
Submucosa plexus (Meissner’s plexus)→ found in the submucosa (duh)
controls glandular secretions
Autonomic Nervous System (ANS) → composed of two systems
Parasympathetic nervous system → stimulates GI activity
Sympathetic nervous system → inhibits GI activity
Diffuse neuroendocrine system (DNES) → composed gastroendocrine and enteroendocrine cells
secretes endocrine hormones that modulate GI activity
General functions of the GI tract and their locations
Motility → esophagus, stomach, sphincters, small & large intestine
Secretion → mouth, stomach
Digestion → mouth, stomach & small intestine
Absorption → small & large intestine
Excretion
Motility
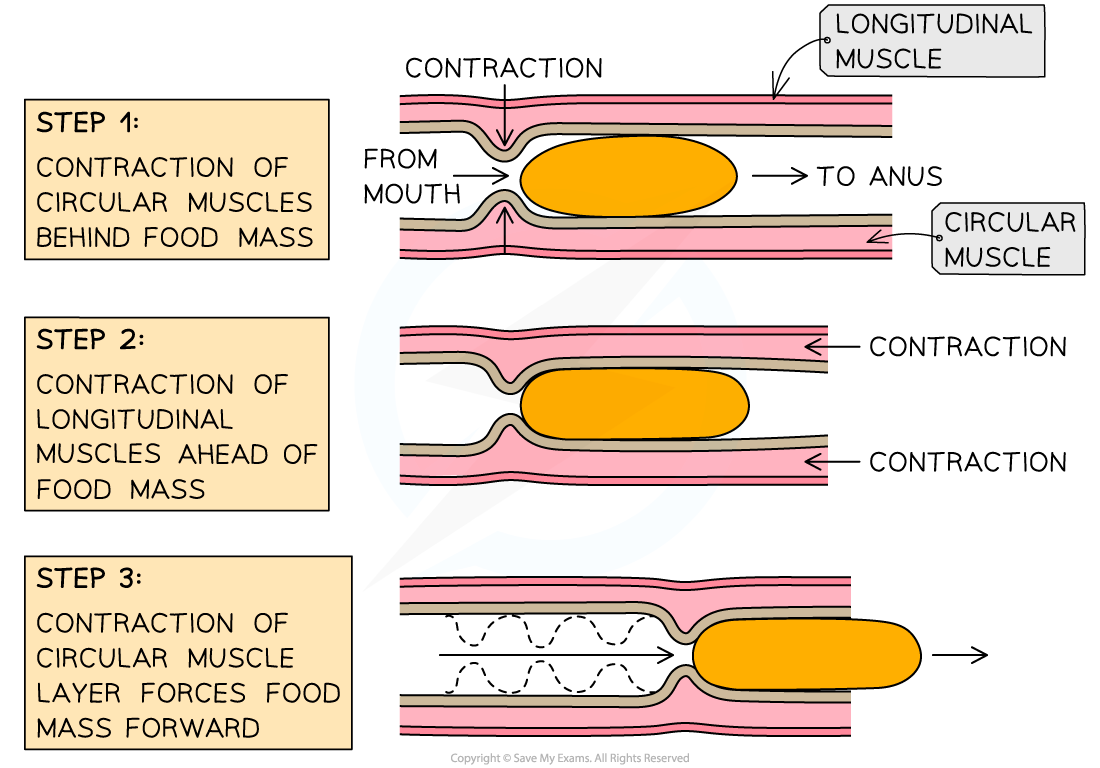
Peristalsis → wave-like contractions that push the bolus down the esophagous to the large intestine
Sties → esophagus, distal stomach, small & large intestine
Main function → propulsion
driving or pushing forward
![]()
Rhythmic segmentation → contractions on either side of the intestines that aid in mixing of foor
Sties → small & large intestine
Main function → mixing
Tonic contractions → consists of prolonged contractions that segment off in the sphincters
Sties → sphincters & proximal stomach
Main function → propulsion
Digestion overview
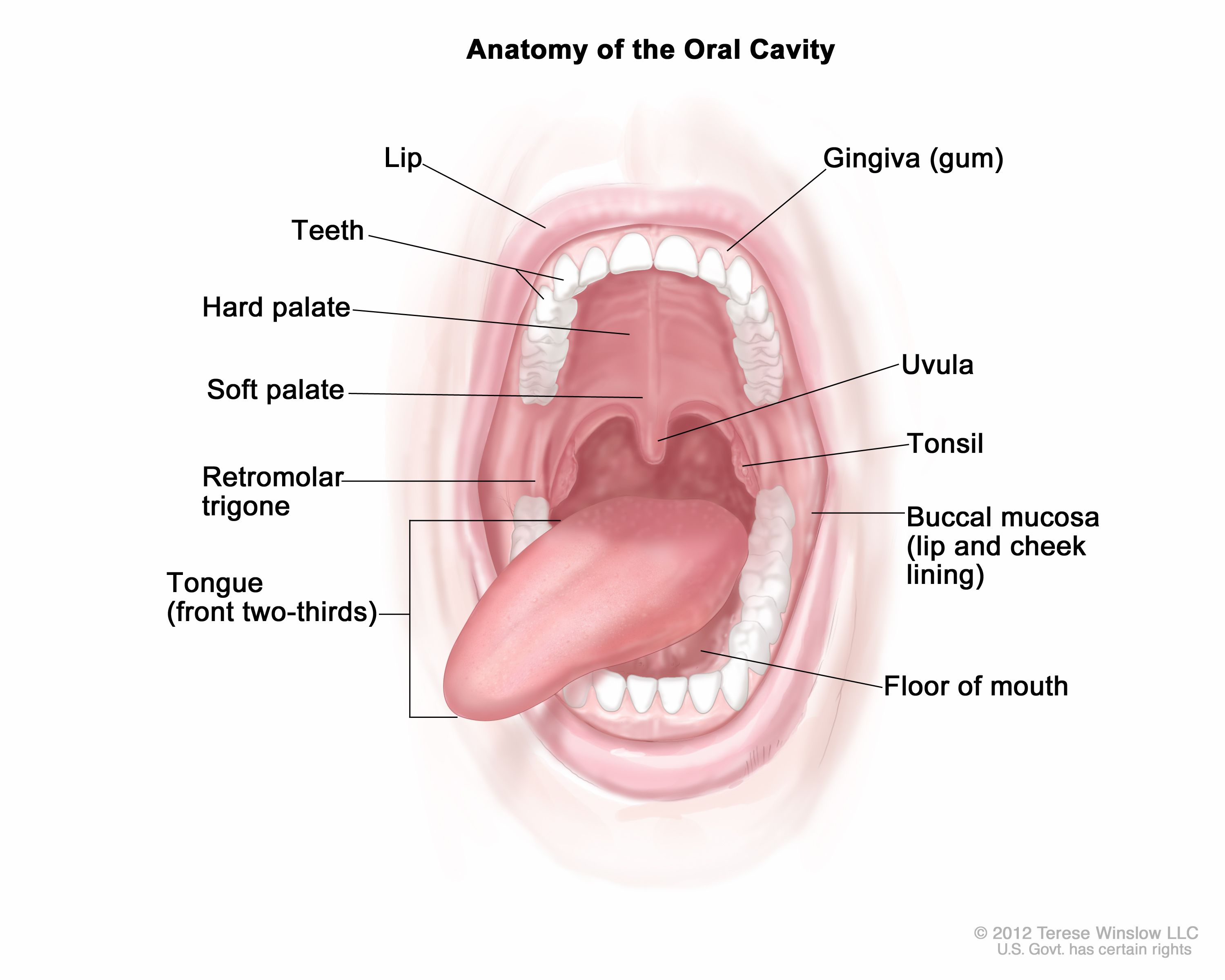
Oral cavity
Anatomy
Mouth
Salivary glands
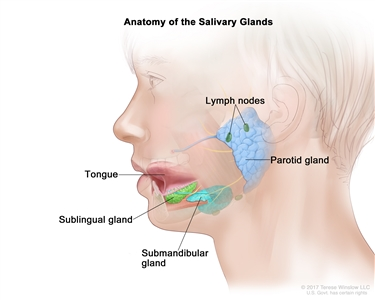
innervated by the ANS
largely induced by feedforward and visceral receptors
Function
Ingestion → the concious placement of food in the oral cavity
Deglutition → conscious process of swallowing.
The tongue pushes bolus against the soft plate and the back of mouth, triggering the swallowing reflex
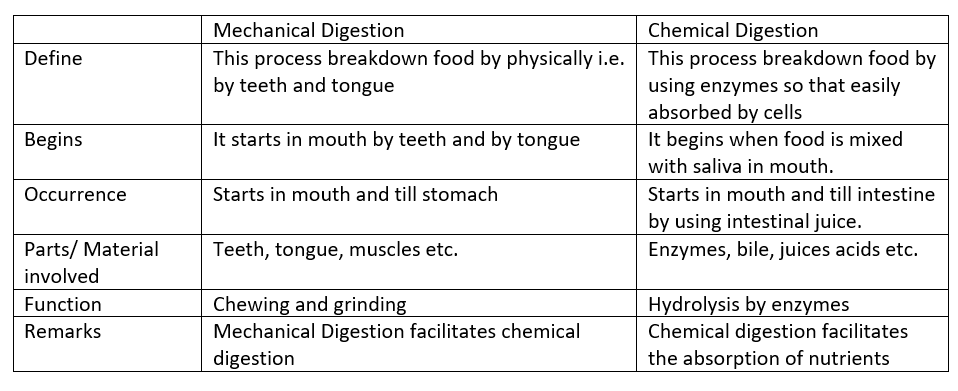
Diggestion
Mechanical
hewing (mastication) and smashing food against the hard palate with the tongue increases its surface area for digestive enzyme activity
Chemical
paired salivary glands secrete the constituents of saliva (water, mucus, ions, buffers, antimicrobics (IgA, lysozyme), enzymes (lingual lipase, salivary amylase))
Oprimum pH in oral cavity → 7.4
What is diggested in the oral cavity?
Carbohydrates with salivary amylase
Salivary glands
gland → secretory product
parotid gland → serous fluid
sublingual gland → mucous
submandibular glands → serous & mucous
Components of salive → water, mucus, buffers, antimicrobics, lysozymes. iodine, and enzymes
Pharynx & Esophagus
Pharynx
What passes through it?
Food, liquid, and air
Esophagus
Anatomy
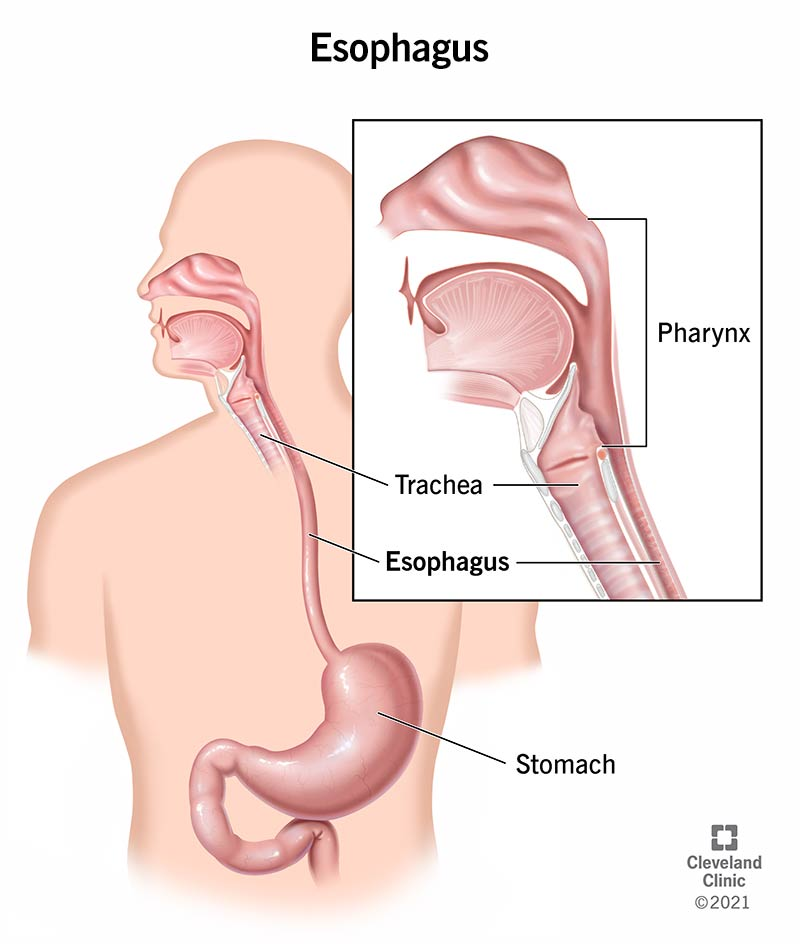
Functions
Primary function is to move the bolus towards the stomach
secretes mucous to lubricate the esophagus reducing friction to Protect the mucosa of the esophagus.
Two esophageal sphincters
Upper esophageal sphincters (UES) → located in the uper part of the esophagus
In charge of preventing air from entering the stomach during respiration
Lower esophageal sphincters (LES) → located below the diaphragm
Prevents reflux of chum into the esophagus
Pathologies
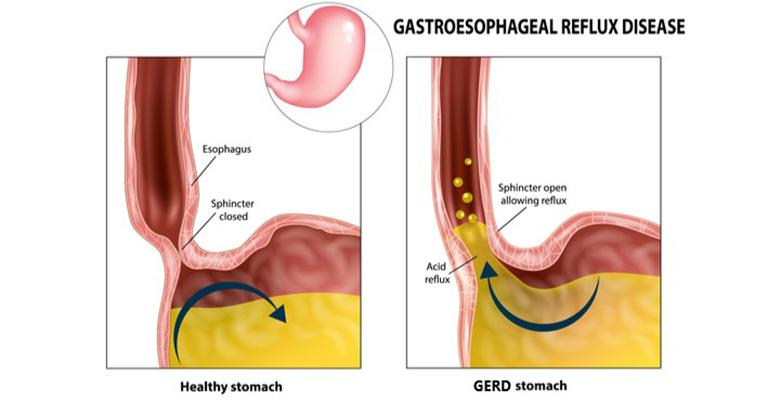
Gastroesophageal reflux disease (GERD) → chronic form of acid reflux caused by abnormal/weakened/relaxed LES or increased intra-abdominal pressure
Can develop in obesity, pregnancy, hiatal hernia*, gastroparesis
Can be treated with…
Anti-acids → TUMS
H2RAs → Pepcid, Zantac
PPIs → Proliosec
Surgery
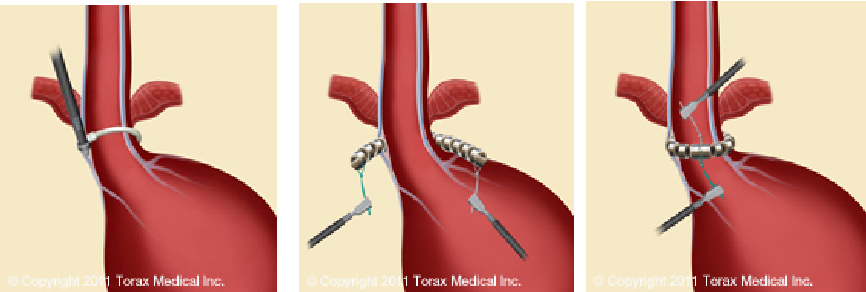
MSAD (LINX system) → a small flexible band of interlinked titanium beads with magnetic cores designed to restore the body's natural barrier to reflux
Nissen Fundoplication → procedure, where a surgeon wraps the top of the stomach around the lower esophagus (LES)
this reinforces the LES sphincter, decreasing the possibility of acid reflux.
Nissen Fudoplication:
![]()
MSAD (LINX system)
Hiatal Hernia* → occurs when part of the stomach protrudes up into the chest through the diaphragm (LES).
The hernia itself can play a role in the development of both acid reflux and GERD.
Weak supportive tissues and increased abdominal pressure can contribute to the condition.
Chronic Heart burn → chronic erosion of the esophagous and can lead to esophageal cancer
It can be treated with anti-acids and proton pump inhibitors
Esophagitis → inflammation of esophageal lining
Caused by GERD, infection, certain medications (e.g., NSAIDs)
“Pill-induced” Esophagitis → occurs when capsules or tablets get stuck in the esophagus and cause tissue damage (resulting in inflammation)
Barrett’s esophagus → metaplasia of the glandular cells of the lower 1/3 of esophageal lining to a simple columnar epithelium w/goblet cells
Caused by chronic Esophagitis (normally due to GERD)
Cells can become dysplastic and eventually precancerous
Dysplastic → term used to describe the presence of abnormal cells within a tissue or organ
Dysplastic ≠ Cancerous
can be mild, moderate, or severe, depending on how abnormal the cells look under a microscope and how much of the tissue/organ is affected
Esophageal cancer → 6th most common cancer related rate, only a 15% 5-year survival rate
Two forms…
esophageal adenocarcinoma → occurs in the esophageal glands
esophageal squamous cell carcinoma → occurs in the squamous epithelium
May be caused by tabacco (any form), GERD, poor diet, and obesity
The stomach
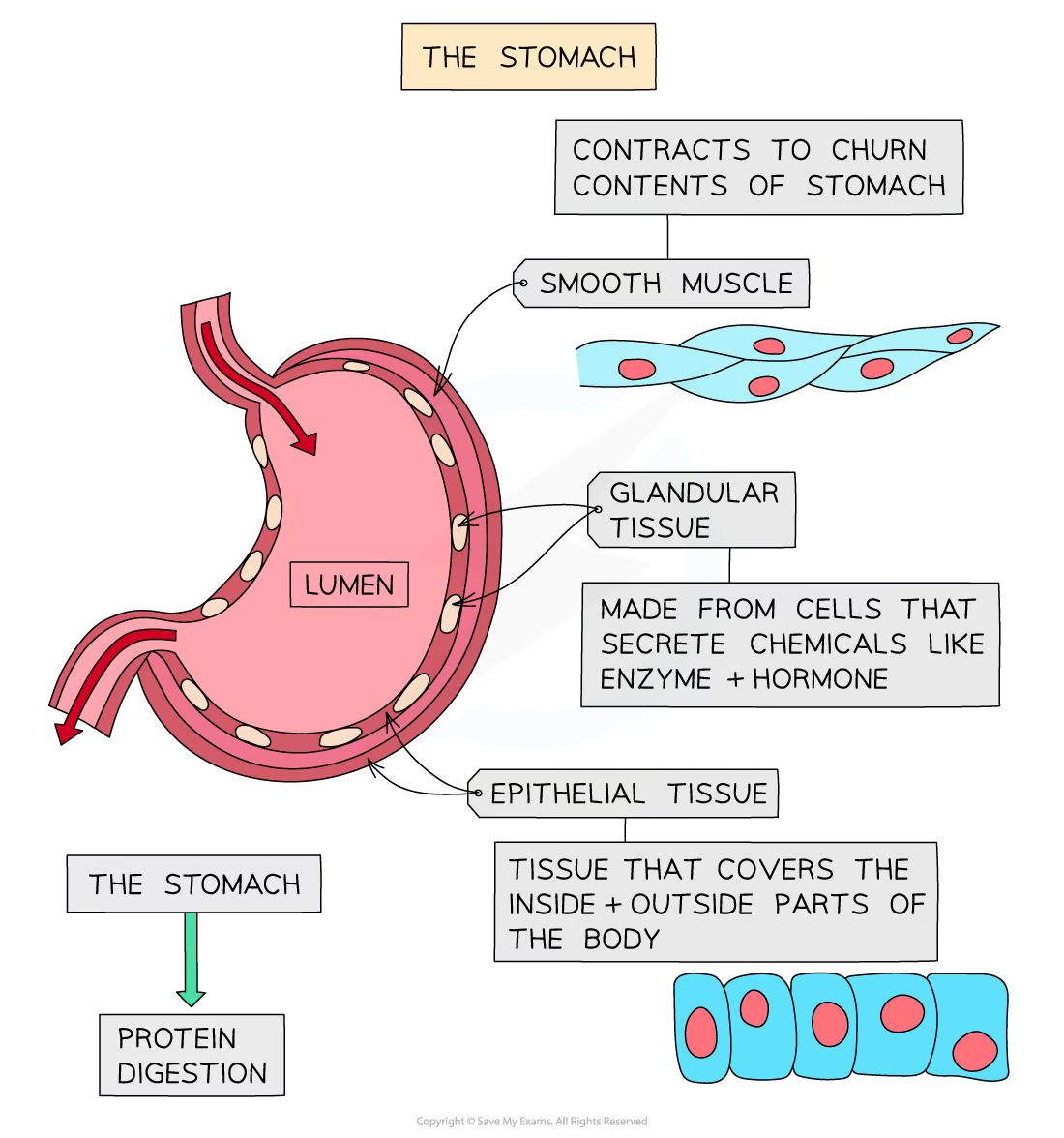
Anatomy
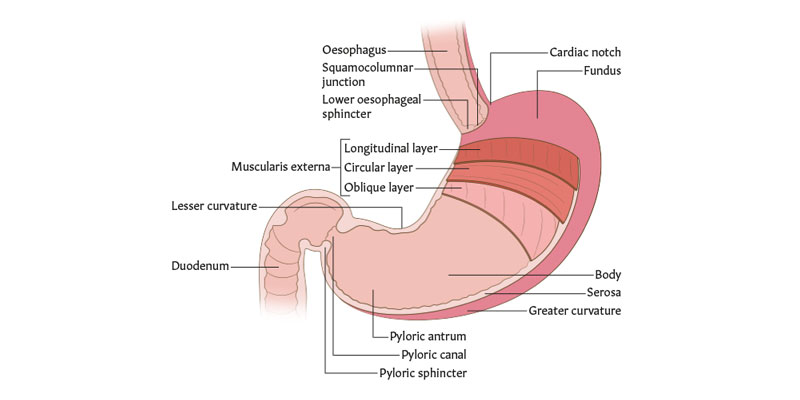
Why is the histological organization of the stomach unique from the rest of the GI tract?
stomach has 3 layers of smooth muscle in the muscularis externa
inner oblique
middle circular
outer longitudinal layer
this allows the stomach to contract in an additional plane and therefore impart a churning effect on the food
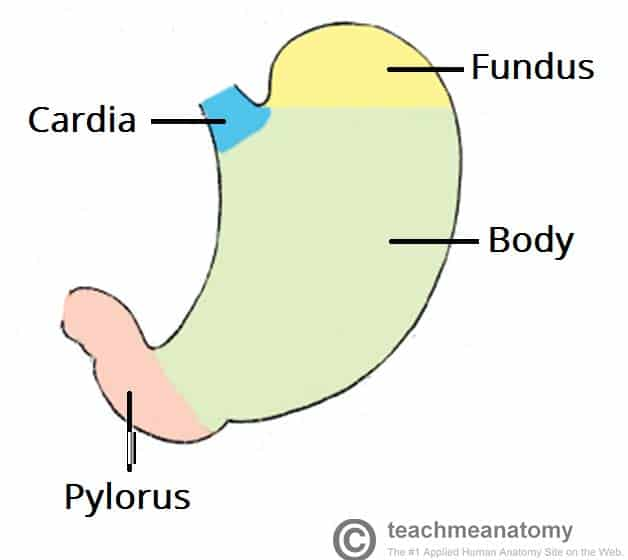
4 regions of the stomach
cardiac (cardia), corpus (body), pyloric (pylorus), fundic (fundus)
Histology
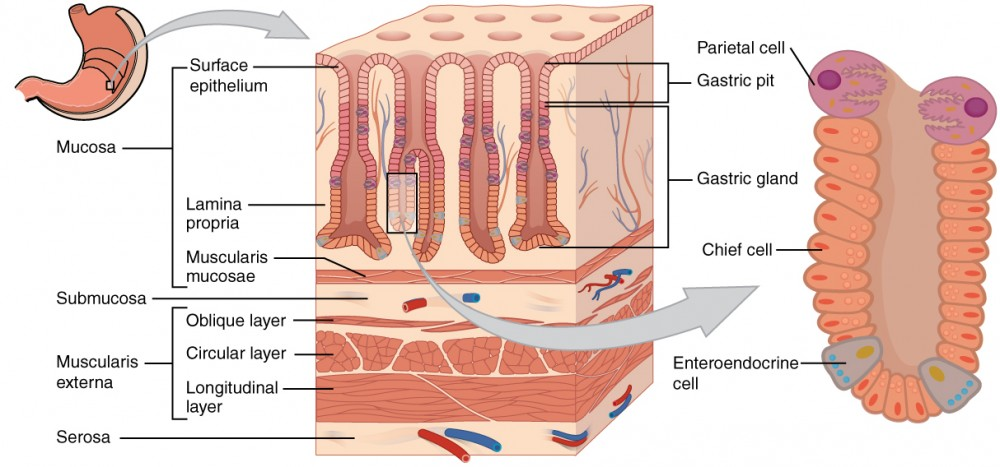
Gastric glands → located at the bottom of the gastric pits
composed of…
Parietal cells
Pumps H into the lumen & Cl follows (HCl)
pH of stomach → ~2-5
the acidity of the stomach lills microbes, denatures protein and activates pepsinogen
Secretes gastric intrinsic factor (GIF)
essential of vitamin B12 absorption
Chief cells
Secretes pepsinogen and gastric lipase
pH optima → ~2 and ~5, respectively
pepsinogen autoclaves to pepsin (peptidase) at low pH
Gastroendocrine cells
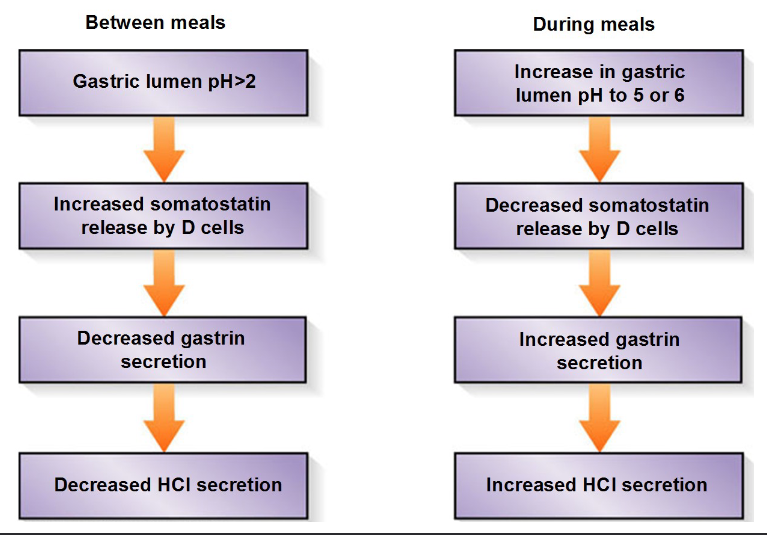
G cells
↑ gastric activity (mechanical and chemical)
induced by AAs, distension, and vagal stimulation
D cells (somatostatin)
inhibits parietal cels
induced by low luminal pH
Gr cells (ghrelin)
↑ neuropeptide Y (NPY) in hypothalamus, stimulating appetite
Surface lining cells
Function
Digestion
Mechanical → peristaltic wave contractions mix the bolus with digestive juices and periodically “squirt” chime into the duodenum
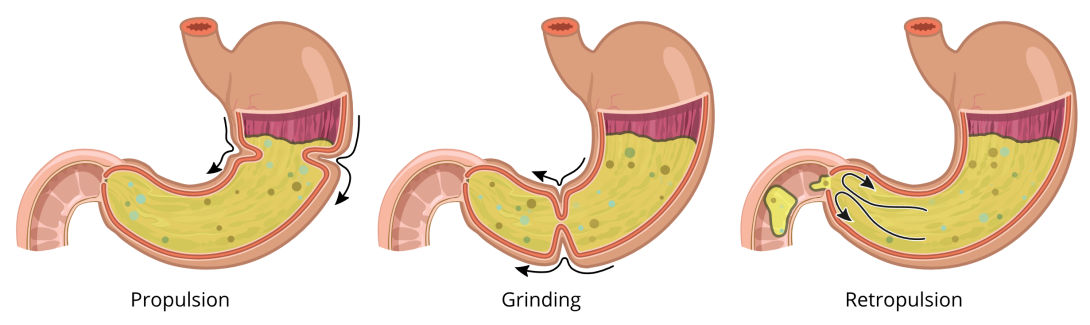
Steps of mechanical digestion:
Propulsion → peristaltic waves move from the fundus toward the pylorus
Grinding → the most vigorous peristalsis and mixing action occur close to the pylorus
Retropulsion → the pyloric valve* act as a pump that delivers small amounts of chyme into the duodenum. simultaneously forcing most of its contained material backward into the stomach
Pyloric valve* → located at the end of the stomach
opens during retropulsion
closes during propulsion and grinding
Chemical → gastric glands produce digestive enzymes and
gastroendocrine hormonesEnzymes (and other gastric juices) are mixed with food forming chyme