ACLE
Key Points
ACLE is a type of cutaneous lupus erythematosus (CLE) characterized by transient skin lesions.
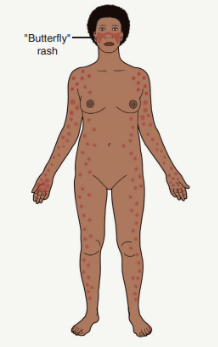
The lesions of ACLE are exemplified by the development of bilateral malar erythema (“butterfly rash”).
ACLE lesions tend to follow sun exposure and resolve without scarring.
ACLE is the cutaneous phenotype with the strongest association with systemic disease.
Epidemiology
The sources do not provide specific epidemiological data for ACLE.
Pathogenesis
ACLE pathogenesis is believed to be triggered by UVR exposure.
UVR exposure initiates an immune response with cytokine, chemokine, and antimicrobial peptide production by keratinocytes, as well as endothelial cell activation.
This leads to a complex cascade, including activation of dendritic cells, release of IFN, activation of T cells, and production of chemokines, resulting in a lichenoid tissue reaction.
Rash Description and Clinical Features
Malar Erythema ("Butterfly rash"):
The classic presentation of ACLE.
May range from mild erythema to intense edema.
May also present with telangiectasias, erosions, dyspigmentation and epidermal atrophy (poikiloderma).
May include a papular component or scaling.
Duration may range from a few hours to several weeks.
Typically spares the nasolabial folds.
The presence of small erosions can aid in the clinical differential diagnosis.

Distribution:
Most commonly affects the face, particularly the malar area.
Can sometimes be more widespread, including the arms.
When lesions occur on the hands, the knuckles are typically spared.
It is not unusual for patients with ACLE to also have oral ulcerations.
Other Variants:
A toxic epidermal necrolysis-like presentation has also been described as a form of acute syndrome of apoptotic pan-epidermolysis (ASAP).
Systemic association:
Has an association with anti-dsDNA antibodies and lupus nephritis.
Some patients with malar rash have neither anti-dsDNA antibodies nor lupus nephritis.
Diagnostic Criteria:
According to the Systemic Lupus International Collaborating Clinics (SLICC) classification system, ACLE is included as one of the clinical criteria. This includes:
Lupus malar rash (do not count if malar discoid).
Toxic epidermal necrolysis variant of SLE.
Photosensitive lupus rash in the absence of dermatomyositis.
Bullous lupus.
Maculopapular lupus rash.
The American College of Rheumatology (EULAR/ACR) classification criteria for SLE includes ACLE as a cutaneous finding that suggests the diagnosis of SLE.
Diagnosis and Investigations
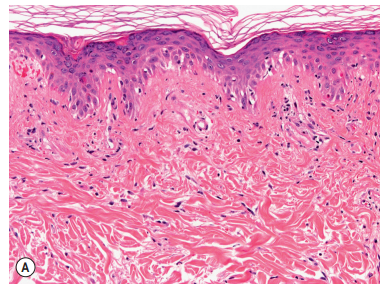
Histopathology:
Dermal changes can be relatively subtle.
Basal cell damage (vacuolar degeneration, hydropic change, or interface dermatitis) may be pronounced.
Mild interface dermatitis with vacuolization of basal keratinocytes and sparse superficial lymphoid infiltrates.
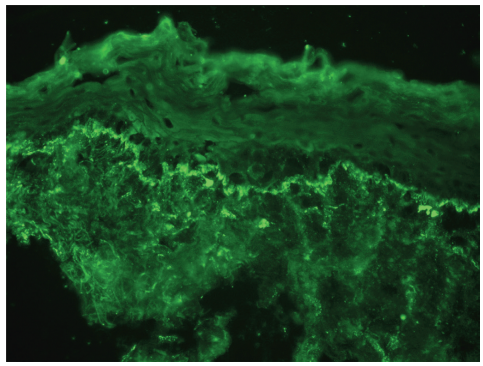
Direct Immunofluorescence (DIF):
In active lesions of ACLE, DIF of lesional skin is usually performed.
Granular deposits of IgM are present at the dermal–epidermal junction within lesional skin. Antibody deposits at the dermal–epidermal junction are the most characteristic immunohistologic finding in lesions of cutaneous lupus and normal skin of patients with systemic lupus erythematosus
Laboratory Tests:
ANA with profile (anti-dsDNA, -Sm).
Urinalysis.
CBC with differential, platelet count.
Chemistries (BUN, creatinine).
ESR, CRP.
Complement levels (C3, C4).
Antiphospholipid antibodies, PT/PTT.
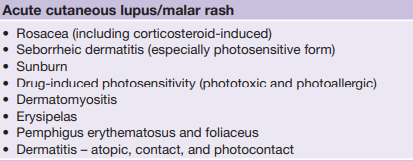
Differential Diagnosis
Seborrheic dermatitis.
Erythematotelangiectatic rosacea.
Sunburn.
Drug-induced photosensitivity.
Dermatomyositis.
Treatment/Management
General measures include avoiding photosensitizing medications and smoking cessation.
Sun protection is essential, including sunscreens, protective clothing and sun avoidance.
Careful attention should be given to vitamin D and calcium intake.
Complications
May resolve without scarring but can sometimes result in dyspigmentation.
Progression to systemic lupus erythematosus (SLE).
Additional Notes
The morphology of ACLE lesions can vary.
Telangiectasias, erosions, dyspigmentation and epidermal atrophy may help to distinguish ACLE from other facial eruptions.
ACLE is the cutaneous phenotype with the strongest association with systemic disease, but patients with any type of cutaneous LE may develop internal involvement.
A lesional biopsy for direct immunofluorescence (DIF) may be performed at the same time as a lesional biopsy for routine histology.
Less definitive histologic findings might sometimes be acceptable if the patient is already known to have SLE.