Unit G: Urinary System
Fun Facts
AKA the Excretory System
Performs the main part of the excretory function in the body- to urinate!
Most important organ of excretory system is the kidney
If kidneys fail, toxic wastes start to accumulate in the body which causes cells to “poison” the body.
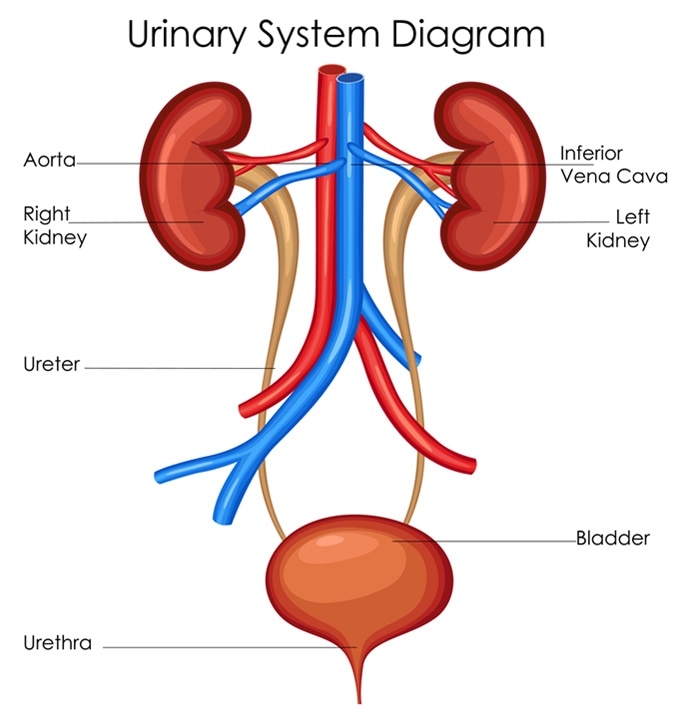
Gross Anatomy
2 Kidneys
2 Ureters
1 Bladder
1 Urethra
1 Urinary Meatus
Structures of The Urinary system
Kidneys
Most important excretory organ
Bean-shaped
Located between peritoneum and the back muscles (retroperitoneal)
Held in position by connective tissue
Enclosed in an adipose capsule
Protected by the floating ribs
External Structures
Renal Capsule
Renal Fascia
Renal Hilum
Internal Structures
Renal Cortex
Renal Medulla
Renal Pelvis
Renal Capsule
Kidney is enclosed within
Renal Fascia
Fibrous layer of connective tissue that covers the kidney
Renal Hilum
Indentation that gives the kidney its bean-shaped appearance (passageway for lymph vessels, nerves, renal artery and vein and ureter)
Internal Kidney
Renal Cortex: Outer layer
Composed of millions of microscopic functional units called nephrons
Renal Medulla: Middle layer
Inner, striated layer
RENAL PYRAMIDS are the striated cones.
Base of each pyramid faces cortex, while apex empties into cuplike cavities called CALYCES
Renal Columns
Located between the pyramids
Cortical tissue
Renal Pelvis: Innermost layer
Ureters
Muscular tube extending from each kidney to the urinary bladder
Lined by a mucous membrane
10-12” long
Urinary Bladder
Hollow muscular organ
Located in pelvic cavity
Made of elastic fibers and involuntary muscles
Urethra
Connects the bladder to the outside of the body
Female 1-2” long
Male 4-6” long
Urinary Meatus
Opening to the outside of the body
The external opening of the Urethra
Day 2: Functions of the Urinary System
Important
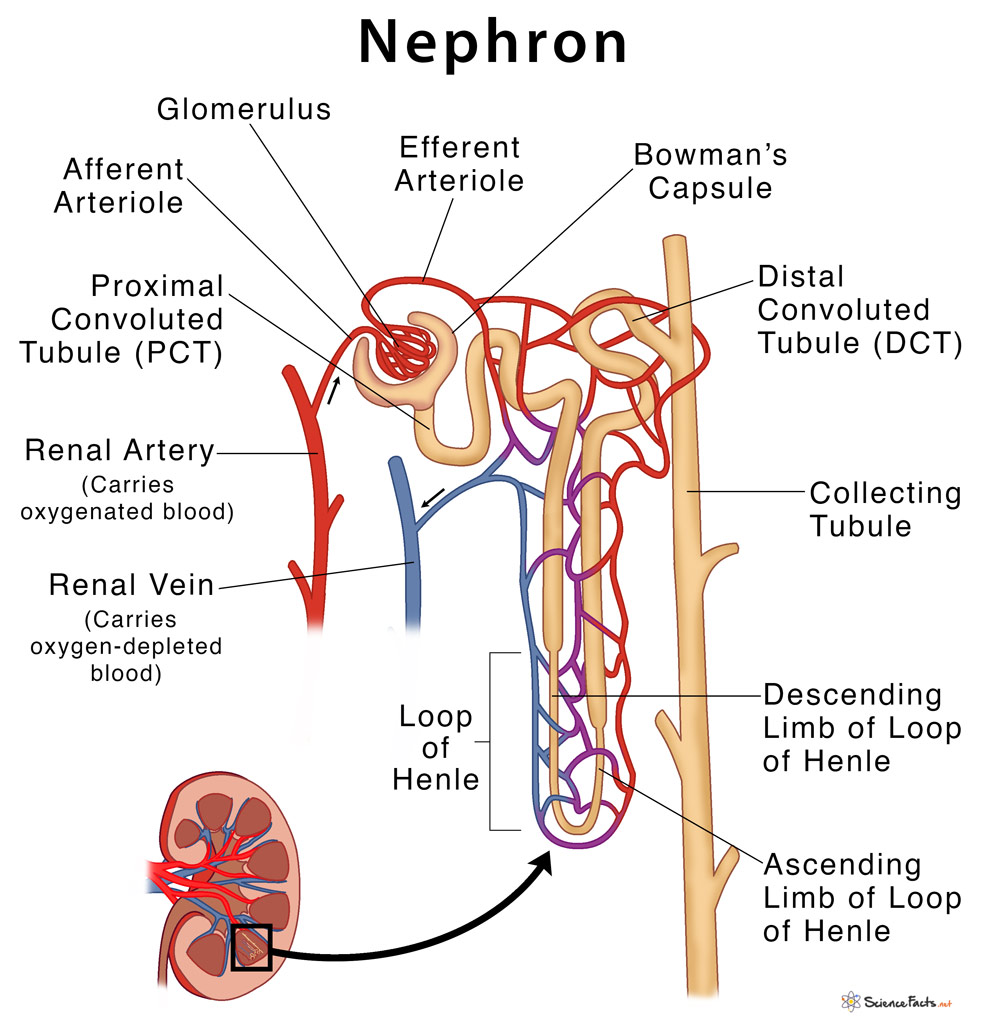
Proximal Convoluted Tubule
Distal Convoluted Tubule
Loop of Henle (nephron)
Bowman’s Capsule
Collecting Tubule
Glomerulus
(1,2,3 do the same function. 4,5,6 do different functions)
Functions
Excretion
Process of removing nitrogenous waste materials, certain salts and excessive water from the blood
Formation of Urine: Filtration → Reabsorption → Secretion
Filtration
Blood from the renal artery enters the glomerulus
High pressure in the glomerulus forces fluid into Bowman’s capsule, where it is filtered
Bowman’s Capsule
Bowman’s capsule filters out 125cc of fluid/min.
…how many cc’s per hour is this?
As the filtrate continues through nephron, 99% of water is reabsorbed—so only 1000-1500 cc (1-1.5 L)of urine are excreted daily
Reabsorption
Substances include water, glucose, amino acids, vitamins, magnesium, sodium and potassium
Reabsorbed by the capillaries in bloodstream around the TUBULES.
If blood levels of certain substances are high, the substances will not be reabsorbed.
They remain in the tubules and are excreted in the urine.
Ex- glucose in diabetics “spilling” glucose in urine
Ex – medications – hence why medications need to be taken frequently
Secretion: This process is the opposite of reabsorption.
Substances are secreted into the collecting tubules include ammonia creatinine, hydrogen ions, potassium and some drugs.
Elimination (Excretion) of urine
Bladder acts as a reservoir (storage tank) for urine.
Contains approximately 500 ml of urine.
Becomes distended and uncomfortable, letting us know it needs emptying.
Emptying the bladder (voiding) occurs through involuntary muscular contractions, which the nervous system can control to some extent.
Fluid and electrolyte balance
Electrolytes are selectively secreted to maintain body’s acid-base balance.
Chemical control: aid in the REABSORPTION process!
ADH – Antidiuretic hormone
Aldosterone
The amount of ADH produced is related to the level of body hydration
Under control of the hypothalamus
Aldosterone Secreted by the adrenal cortex of the KIDNEY.
Promotes the excretion of potassium and hydrogen ions.
Aldosterone release is the result of the renin-an enzyme in the kidneys that is released into the bloodstream.
Nervous control
Accomplished directly through action of nerve impulses on blood vessels within the kidney (and glomerulus)
Endocrine glands (Posterior Pituitary) hormonal secretions (Vasopressin and/or ADH) will also control urinary secretion.
Disorders and Dysfunctions
Cystitis
What is cystitis?
(cyst= medical term for ____ +itis =___ )
An inflammation of the mucous membrane lining of the urinary bladder.
The most common cause: is E. Coli (an organism found in the rectum)
Symptoms: Painful (dysuria) or frequent (polyuria) urination
More common in females—Why ??
The length of the female urethra is 1.5-2 inches long.
Organisms can easily enter the urethra and then into the bladder from the outside of the body.
Glomerulonephritis
Disease which injures the glomerulus of the nephron.
What will happen as a result of damaged glomeruli?
Filtration process is affected
ACUTE (one instance)
Sudden onset
Occurs after bacterial infection (usually strep throat in children)
Treated with antibiotics
Chronic (Long Term)
Filtration membrane is permanently affected
Causes diminished function of the kidney
May result in kidney failure.
Renal Calculi (Kidney Stones)
Can be calcium, uric acid or other substances
They grow larger and eventually fill the renal pelvis and possibly obstruct flow of urine.
First symptom – extreme pain in kidney area or lower abdomen (colon)
Nausea and vomiting are common
May have painful urination, frequency, chills or fever.
Possibility of blood in urine (hematuria)
Diagnosed with ultrasound or CT scan
Treat with increased fluids to flush stone out.
Possibility of lithotripsy (see page 429 medical highlight)
Meds for pain
Acute Renal Failure
Sudden onset
Caused by inflammation of the nephron (nephritis), shock, injury, bleeding, heart failure or poisoning
Symptoms
Oliguria (scanty or diminished production of urine)
Anuria (absence of urine) – could be dangerous because of build up of toxins
Chronic Renal Failure
Gradual loss of kidney functions.
Treat with Dialysis
Passage of blood through a device which rids the blood of harmful waste, extra salt, and water
These devices serve as a substitute kidney.
Two forms
Hemodialysis and Peritoneal Dialysis
Incontinence-Lack of voluntary control of urination
Enuresis-involuntary urination (bedwetting)
Treatment Options
Hemodialysis
Process for purifying blood by passing it through a thin membrane and exposing it to a solution which continually circulates around the membrane.
Uses a machine called a dialyzer
Peritoneal Dialysis
Uses the person’s own peritoneal lining instead of a dialyzer to filter the blood.
Kidney Transplants
Done in cases of prolonged chronic debilitating diseases and renal failure involving both kidneys.
Usually clients have been on dialysis for a long time waiting for a compatible organ.
Daily meds to prevent rejection
Improve quality of life
Urinalysis
An examination of urine
What does normal urine look like?
Clear, straw colored
What constitutes an abnormal urinalysis?
Presence of blood, bacteria, protein, pus, etc.