Implant Maintenance and Management
Patient Journey - The Role of the GDP (**and Dental Therapist)
Patient assessment and advice on tooth replacement
Establishing oral health**
Referral
Detailed planning*
Implant surgery*
Implant restoration*
Monitoring implant health and function, providing supportive care**
* Training required
Survival vs Success
Success Criteria
Albrektsson et al 1986
Clinical immobility of the implant
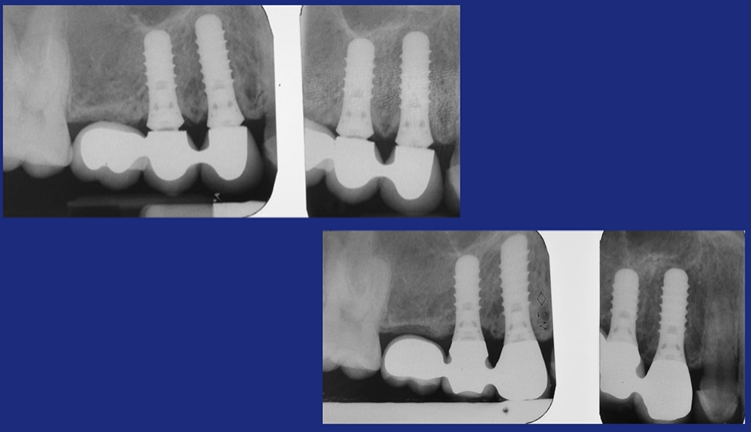
No peri-implant radiolucency
Vertical bone loss of less than 0.2mm annually after the first year
Absence of pain, infection, neuropathy, etc
In the context of the above, minimum success rates of 85% after 5 years and 80% after 10 years.
Success → Failure
Success → Complications → Failure
Biological
Mechanical
Aesthetic
Multifactorial
Monitoring Implant Health
Symptoms
Visual inspection of peri-implant soft tissues
Probing depth
Bleeding
Suppuration
Mobility
Peri-Implant Soft Tissues
Normal healthy gingiva
No inflammation, no recession, etc
Probing
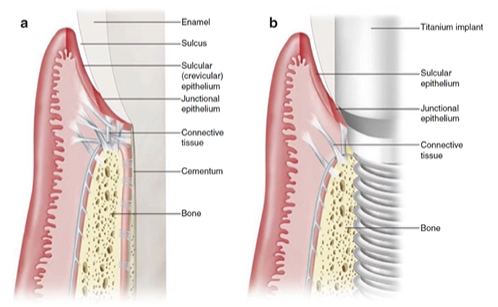
No collagen fibres are attached to the implant surface, they run parallel
No PDL, there is a direct connection between the bone and the implant
Can have equal probing depths all the way around the implant depending ont he implant design
Interpreting Clinical Signs
“Normal” probing depths around anterior implants can be deeper than expected around teeth
Increasing probing depth is significant
Small amounts of BOP are not uncommon, however brisk BOP should be regarded as a sign of inflammation
Suppuration is always significant
Implants should be immobile
Clinical mobility may be due to loss of implant integration or a prosthetic failure
Biological Complications
Peri-implant mucositis
Inflammation in the peri-implant soft tissues, no bone loss
Peri-implantitis
Inflammation in the peri-implant soft tissues, bone loss
These conditions result from the presence of biofilm adjacent to the peri-implant mucosa
It doesn’t always occur but is very common
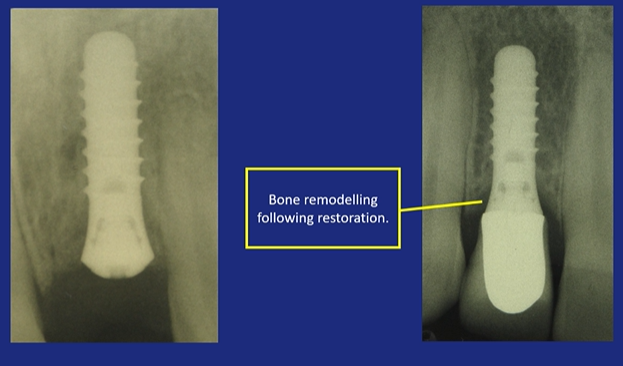
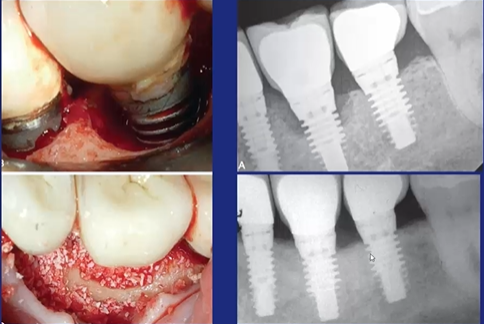
Peri-Implantitis
Use the threads to measure bone loss
Prevention of Peri-Implant Disease
Control of risk factors
Oral hygiene
Periodontal disease
Smoking
Regular supportive visits
Prosthesis design
Cement
Keratinised tissue?
“Implants placed in patients treated for periodontal disease are associated with a higher incidence of biological complications and lower success and survival rates than those placed in periodontally healthy patients. Severe forms of periodontal disease are associated with higher rates of implant loss.”
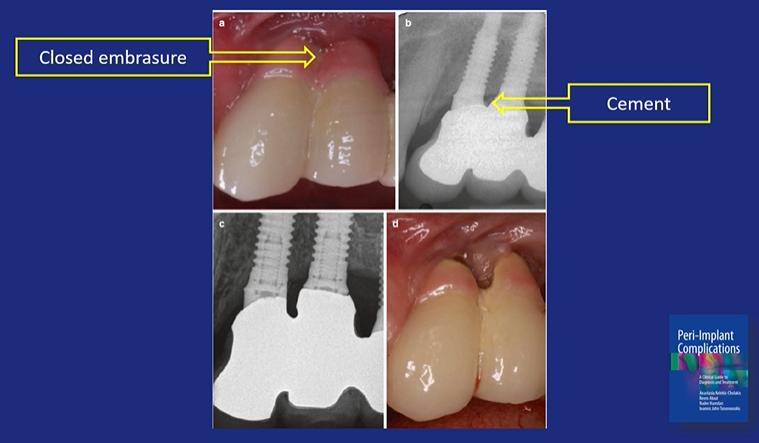
Impossible to clean
A large gap between restorations that increases the risk of caries and bone loss
Management of Peri-Implant Mucositis
Patient-performed plaque control
Professional debridement
Restoration modification
Which Instrument?
Not steel?
Can scratch
Plastic tip
Specific implant instruments
Titanium instruments
Management of Peri-Implnantitis
Surgical access
Granulation tissue removal
Implant surface decontamination
Implant surface modification?
Bone regeneration?
Implant removal
Implant Surface Decontamination
Titanium brush
Damp gauze
Implantoplasty
Smooth the surface
Reduced its thickness which may reduce its strength

Bone Regeneration
Implant Removal
Unscrew
Trephine Bur
Mechanical Complications
The implant breaks (not often)
The screw breaks
The abutment breaks
Aesthetic Complications
Soft tissue deficiencies
Pre-existing
Labial recession/uneven contour
Lack of papillae
Prosthetic errors
3D implant position
Has to be completely surrounded by bone, especially on the labial surface
Can bulk out the labial surface with Bio-Oss (a bone replacement material) for stabilising this bone
Black Triangle
Have sufficient distance between the implant and the adjacent tooth
>1.5mm means the remodelling will not extend through the full thickness of the bone and you will retain that bone on the adjacent tooth
Supports the interdental papilla
<6mm between the bone crest height and the contact point, there’s a good chance that it will fill up with papilla.
It may take several years in some cases
Failure of Integration
Rapid and complete loss of integration
Early (before loading)
Intra-operative trauma?
Later
Overload?
Host factors?
Conclusions
Implant complications are common
Mechanical complications are a nuisance but can usually be managed
The peri-implant disease can be prevented with excellent plaque control and regular supportive care
Peri-implant mucositis can often be managed with simple measures
Peri-implantitis requires specialist input