★ Highlighted is what we NEED to know
NURS-1550: Week 11: Therapeutic Drug Levels and Risks of Medication Use
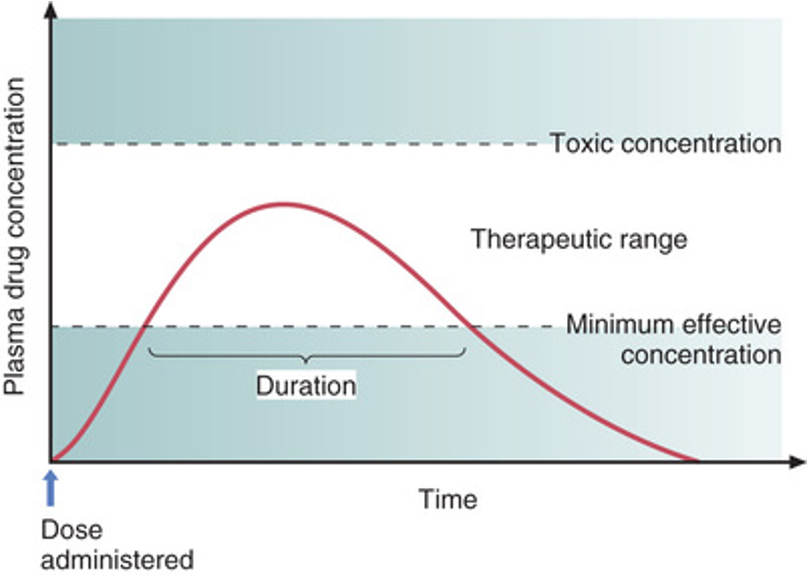
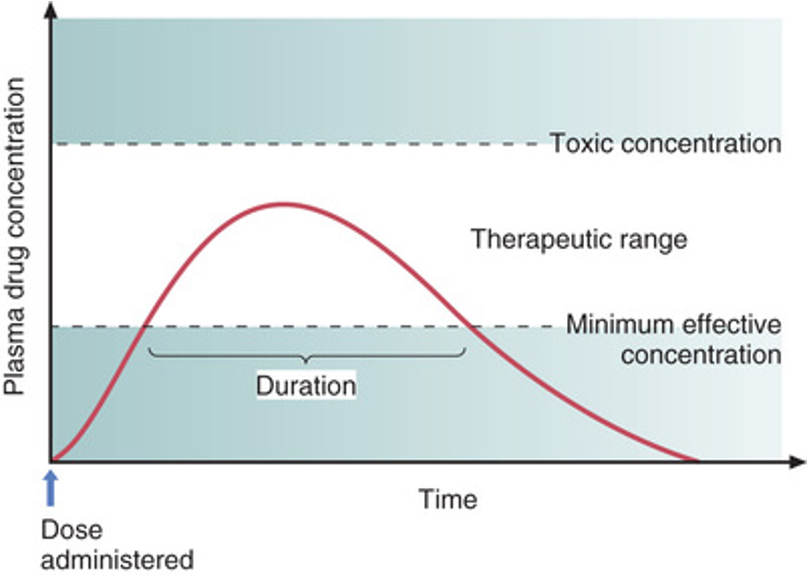
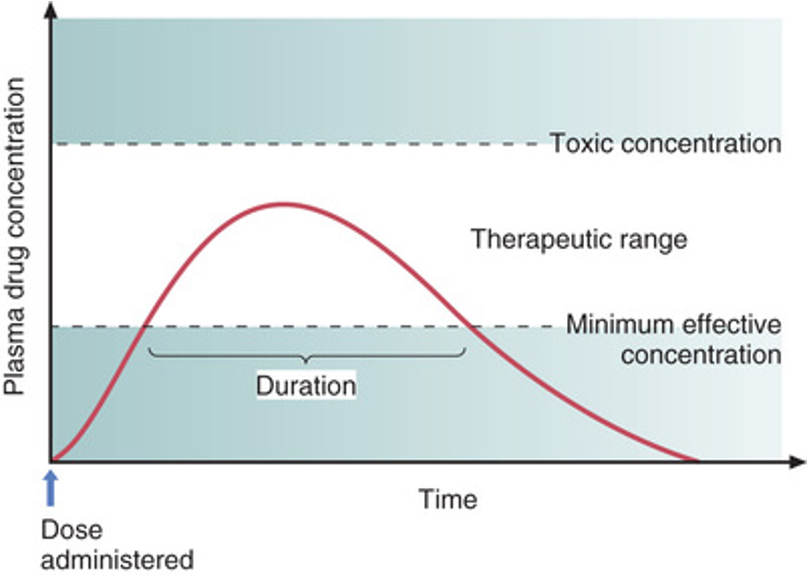
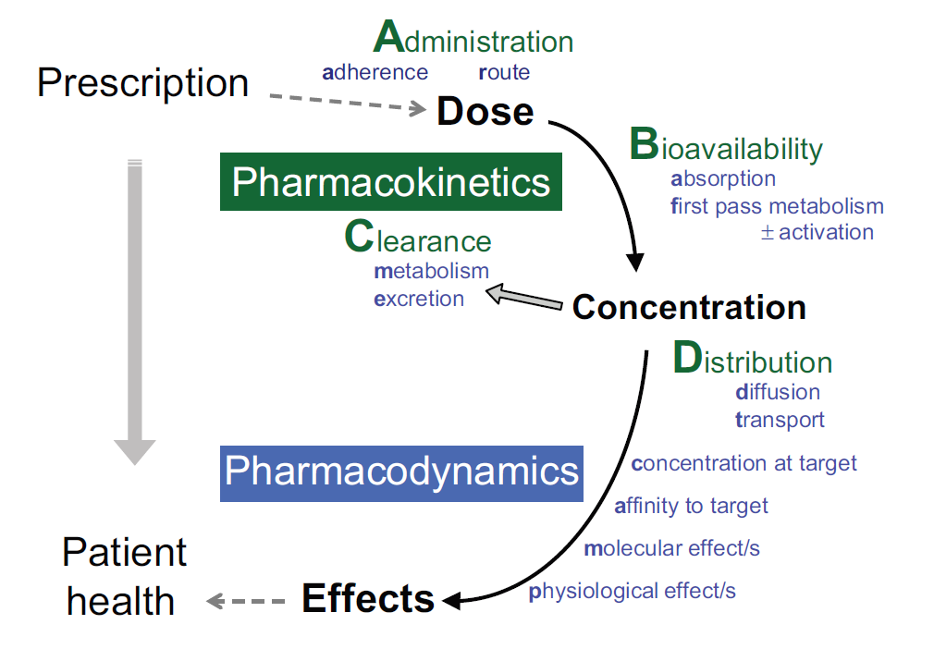
- Time course of drug responses:
- Plasma drug levels
- Single-dose time course
- Drug half-life
- Drug levels produced with repeated doses
- Remember peak, onset, & duration
- Peak = highest point
- Onset = when the drug takes effect
- Duration = for how long the drug is present in the body
- Case study:
- You are the emergency department nurse caring for a 72-year-old man who sustained a fracture to his right femur and left ankle when he fell off the roof of his two-story home. Your patient is complaining of pain that is a 9 on a scale of 0 to 10. You note that he has no medications ordered for pain.
- What steps would you take to address the patient’s pain level?
- Find a medication and prescribe something for the pain: morphine, tylenol, ibuprofen
- Get vitals, med history, pain level
- Stabilize leg
- Which route of administration for the medication might be best for this patient?
- What precautions should you take regarding the specific route of drug administration?\
- Question 1:
- A nurse is preparing to administer epinephrine to a patient who is having a severe allergic reaction. Which route of administration should the nurse use to provide the fastest and most complete absorption of epinephrine?
- Intravenous
- Intermuscular
- Subcutaneous
- Oral
- Question 2:
- When preparing to administer a sustainable-release capsule to a patient, the nurse understands what is true for a sustained-release capsule.
- They are usually more costly than pills.
- They are rapidly absorbed.
- They need to be crushed for appropriate absorption to take place.
- They need to be taken at regular intervals throughout the day.
- Question 3:
- The nurse identifies which patient as being at highest risk for slow drug metabolism?
- A 2-year-old boy who is prescribed an oral antibiotic
- A 14-year-old girl who takes four prescription drugs
- A 56-year-old man who has chronic hepatic disease
- A 76-year-old woman who has an elevated temperature
- Question 4:
- Digoxin has a half-life of 36 to 48 hours. Because of the length of the half-life, the nurse expects dosing to occur how often?
- 4 times per day
- 3 times per day
- 2 times per day
- Once a day
- Drug-drug interactions:
- Basic mechanisms of drug-drug interactions
- Can amplify each other
- Antagonize each other
- May have no interaction
- Clinical significance of drug-drug interactions
- Randomized control trials
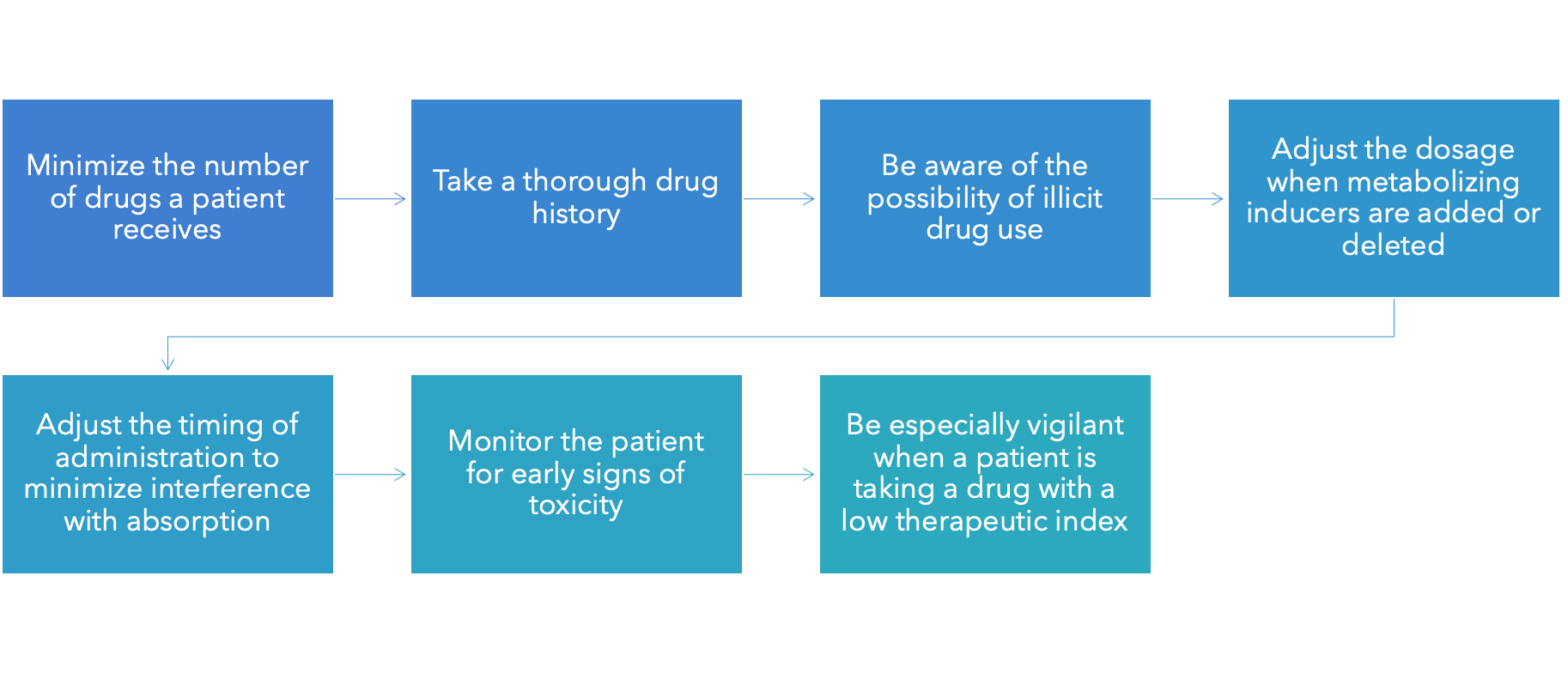
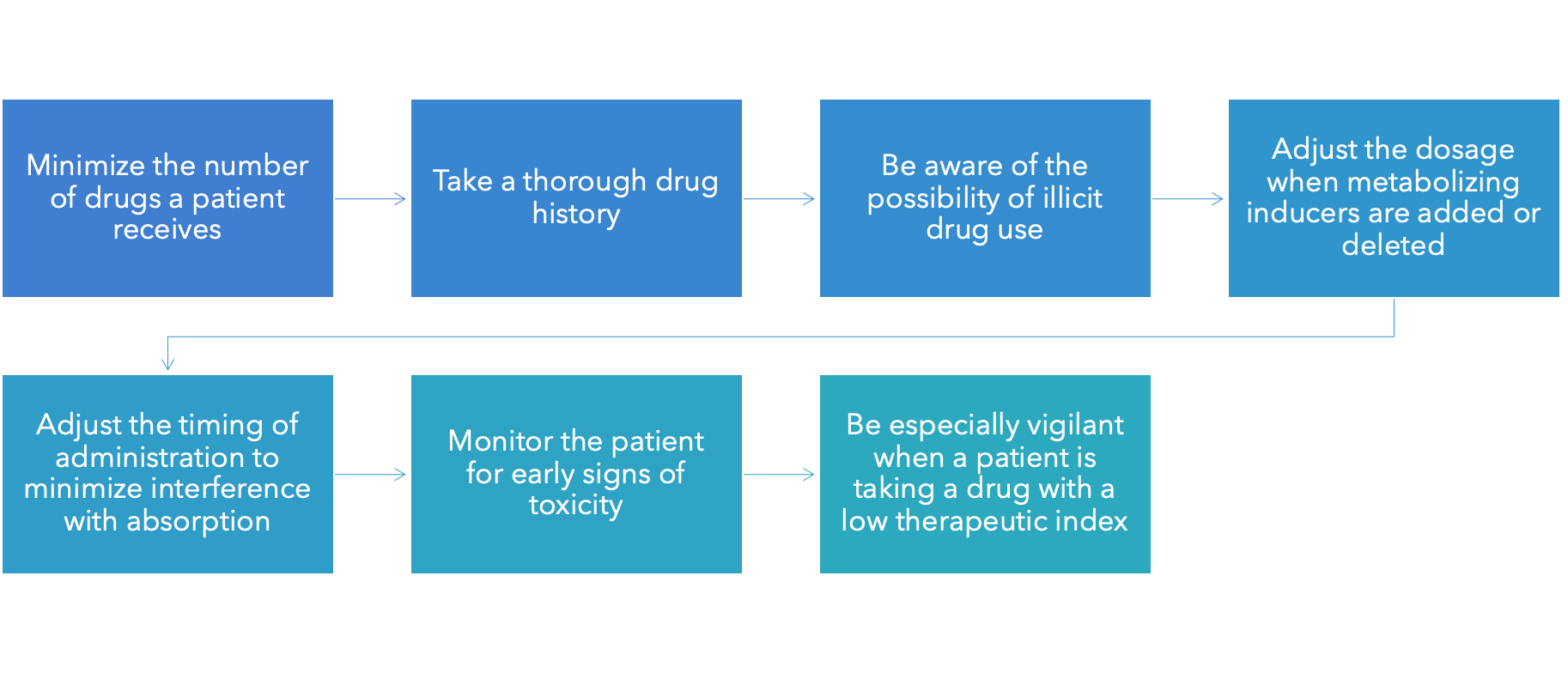
- Minimizing adverse drug-drug interactions
- Interactions can occur whenever a patient takes more than one drug
- Some interactions are intended and desired or unintended and undesired
- Patients frequently take more than one drug
- Multiple drugs to treat one disorder
- Multiple disorders requiring different drugs
- Over-the-counter medications, caffeine, nicotine, alcohol, and so on
- Consequences of drug-drug interactions:
- Intensification of effects
- Increased therapeutic effects
- Increased adverse effects
- Reduction of effects
- Reduced therapeutic effects
- Reduced adverse effects
- Creation of a unique response
- Basic mechanisms of drug-drug interactions:★
- Drugs can interact through four basic mechanisms:
- Direct chemical or physical interaction
- Pharmacokinetic interaction
- Ex. two drugs that increase ability to urinate so your excreting more of one of the drug than you should be
- Pharmacodynamic interaction
- Combined toxicity
- Direct chemical or physical interaction:
- Never combine drugs in the same container without establishing compatibility
- IV
- Mixing medications in IV is not done often because of crossovers or meditation making the tube sticky
- Some meds crystalize in IV line (don't want that in vein)
- Most common in intravenous solution
- Precipitate: Do not administer
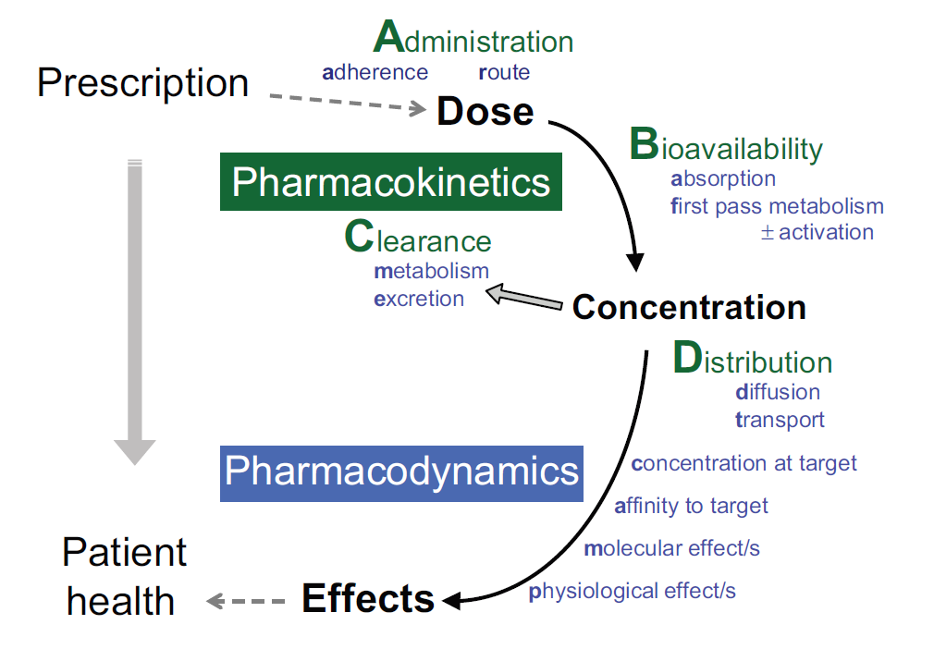
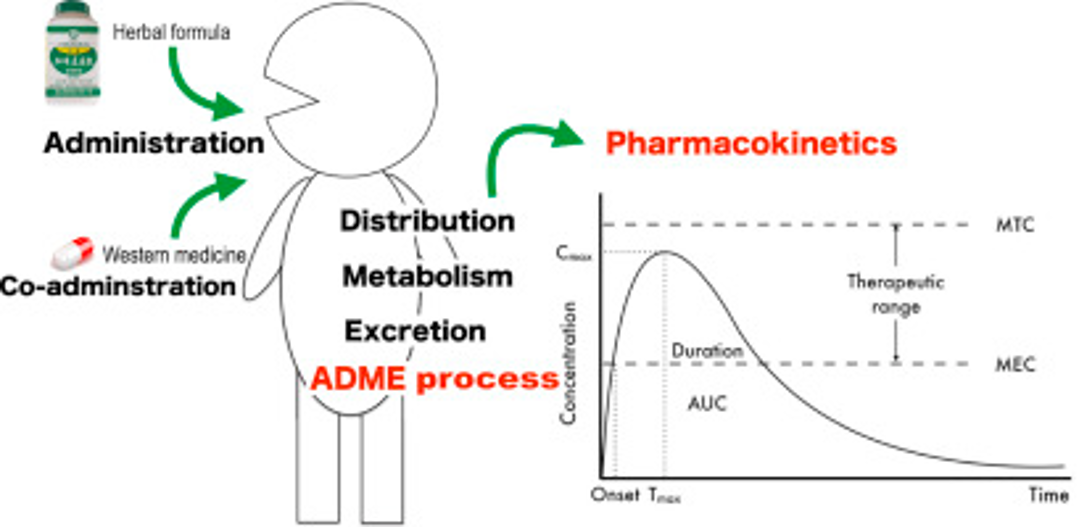
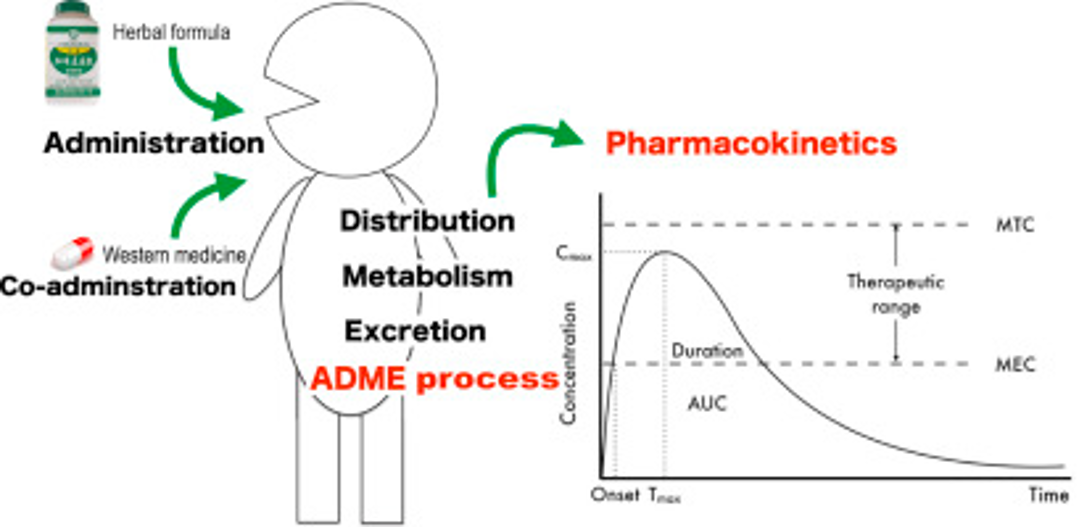
- Pharmacokinetic interactions:
- Alter absorption
- Alter distribution
- Alter renal excretion
- Alter metabolism
- Cytochrome P450 (CYP) group of enzymes (important for metabolizing)
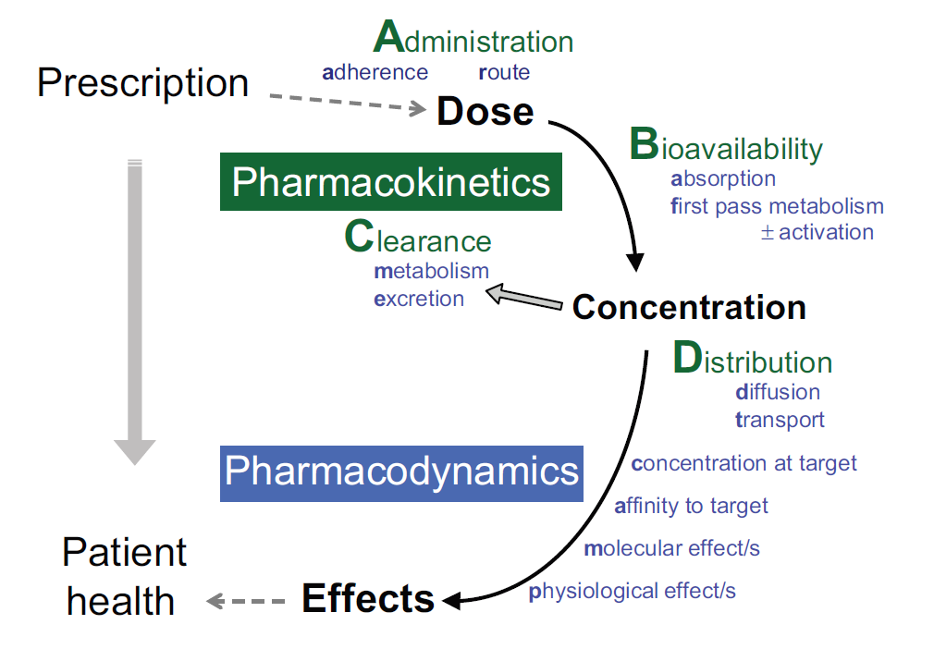
- Pharmacodynamic interactions:
- At the same receptor
- Almost always inhibitory (antagonist/agonist)
- At separate sites
- May be potentiative (morphine and diazepam)
- OR
- Inhibitory (hydrochlorothiazide and spironolactone)
- Combined toxicity
- Drugs with overlapping toxicities should not be used together
- Minimizing adverse drug-drug interactions:
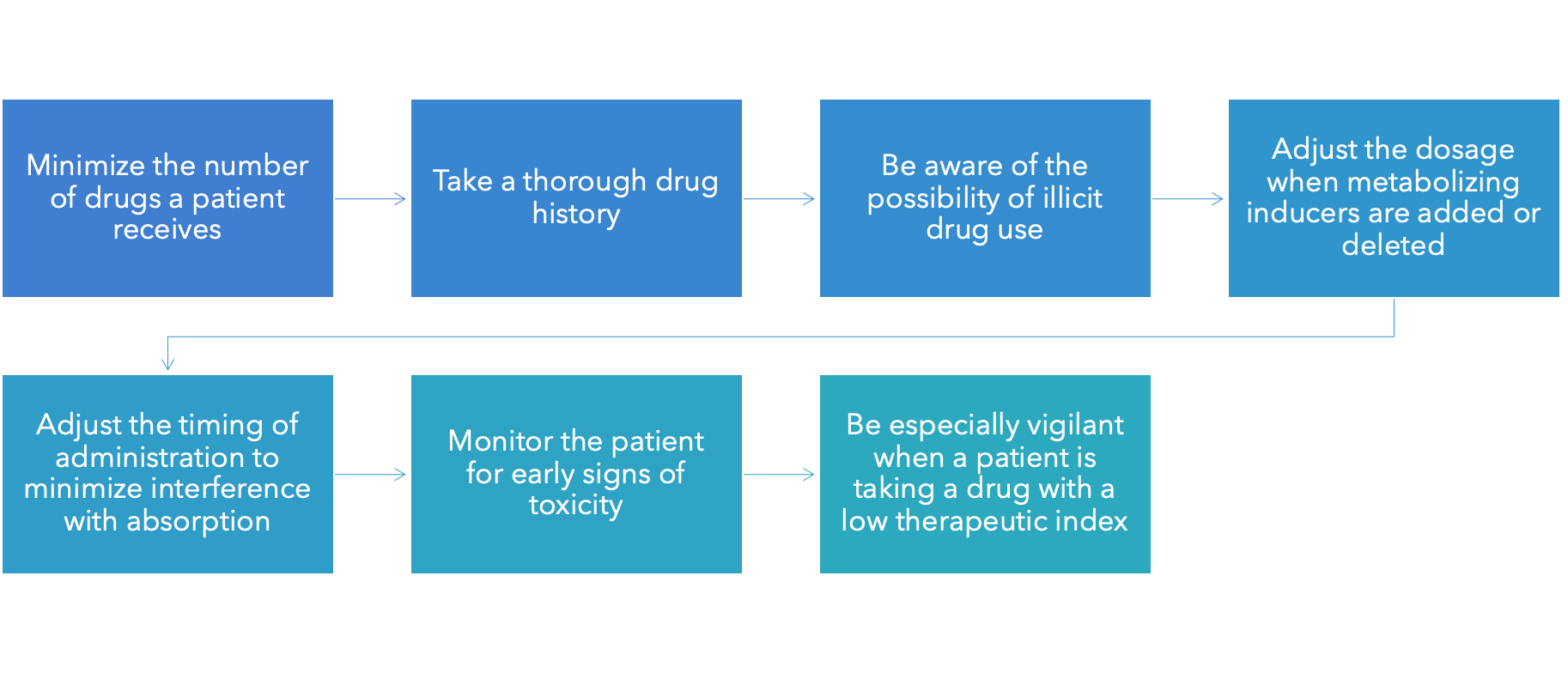
•Drug absorption
•Decreased absorption
•Rate
•Extent of absorption (occasionally)
•Milk and tetracycline don't go together
•Fiber and digoxin don't go together
•Increased absorption
•High-calorie meal and saquinavir
•Without food, not enough is absorbed
•Drug metabolism
•The grapefruit juice effect (not occurring with other citrus fruits or juices)
•Inhibits the metabolism of certain drugs
•Raises the drugs’ blood levels
•Increase in felodipine
•Others: Lovastatin, cyclosporine, midazolam, and so on
•Drug toxicity
•Monoamine oxidase inhibitors (MAOIs) and tyramine-containing foods tyramine like cheese, wine, cured meats
•Theophylline and caffeine TOXIC together
•Potassium-sparing diuretics and salt substitutes
•Aluminum-containing antacids and citrus beverages
•Drug action
•Warfarin and foods rich in vitamin K antidote to warfarin is vitamin K
•Timing of drug administration
•Some drugs are better tolerated on an empty stomach
•Others should be taken with food, especially for nausea
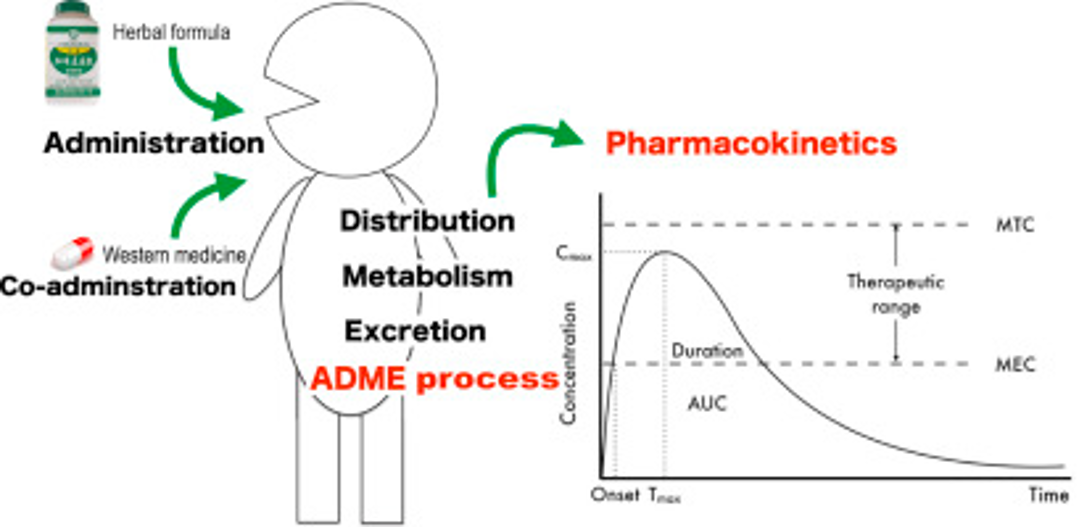
- Drug-herb interactions:
- Conventional drugs can interact with herbal preparations
- Interactions with herbal medicines are just as likely as they are with prescription medications
- Reliable information about drug-herb interactions is lacking
- Example of known interaction:
- St. John’s wort induces drug-metabolizing enzymes and reduces the blood levels of many drugs
- Question 5:
- A patient is taking two prescription medications that both cause bradycardia. The nurse should monitor the patient for which type of effect?
- An increased therapeutic effect
- An increased adverse effect
- A reduced therapeutic effect
- A reduced adverse effect
- Question 6:
- Which individual is at the highest risk for a drug-drug interaction?
- A toddler who is prescribed two antibiotics for a serious infection
- An adolescent who takes over-the-counter medications for menstrual cramping
- An adult who takes eight prescription medications for a chronic condition
- An older adult who takes two prescription medications and a dietary supplement for anxiety
The nurse cares for a patient who is taking a calcium channel blocker for hypertension. The nurse should be most concerned if the patient makes which statement?
- “I take my medication with a glass of water.”
- “I eat foods high in fiber to prevent constipation.”
- “I drink a glass of grapefruit juice each evening.”
- “I avoid foods such as broccoli and cabbage.”
•A patient is prescribed a medication to be taken on an empty stomach. Which statement should the nurse include when providing patient teaching?
- “Take the medication 1 hour before eating.”
- “Take the medication with a small glass of water.”
- “Take the medication before going to bed at night.”
- “Take the medication 1 hour after a meal.”
Rationale: To administer a drug on an empty stomach means to administer it at least 1 hour before or 2 hours after a meal.
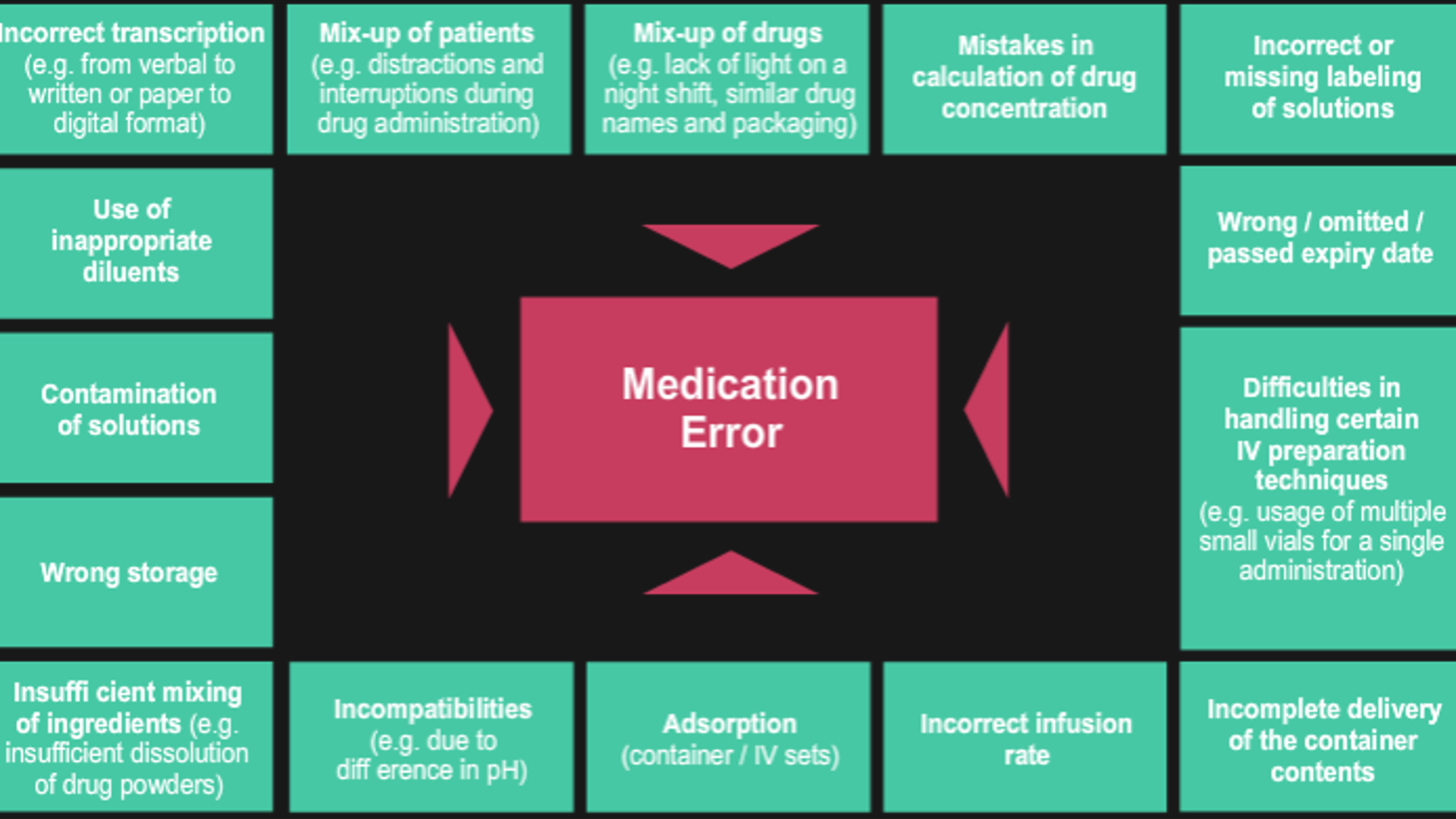
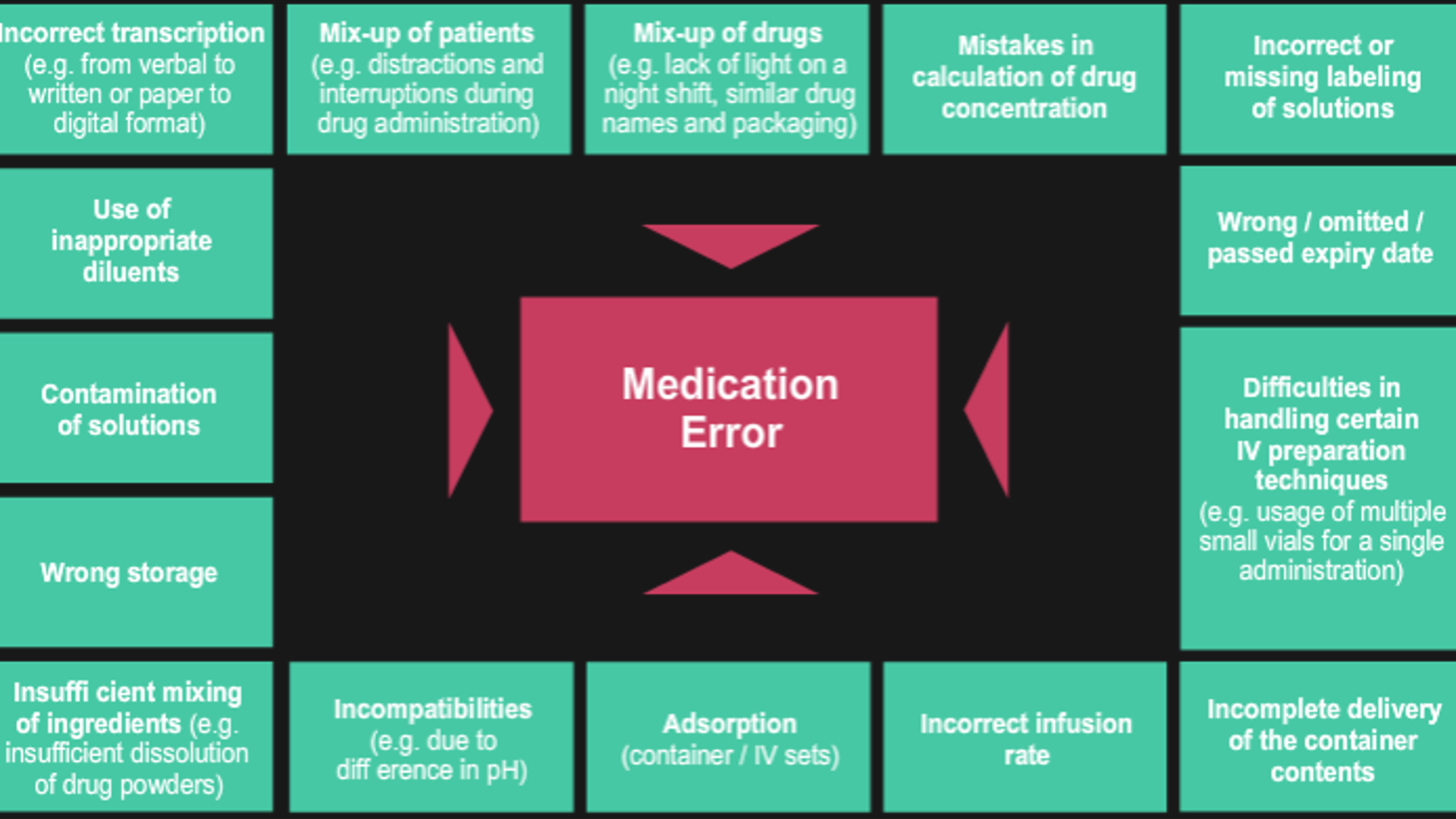
- Two issues related to drug safety:

- Adverse drug reactions (ADRs)
- Also known as adverse drug events (ADEs)
- Medication errors
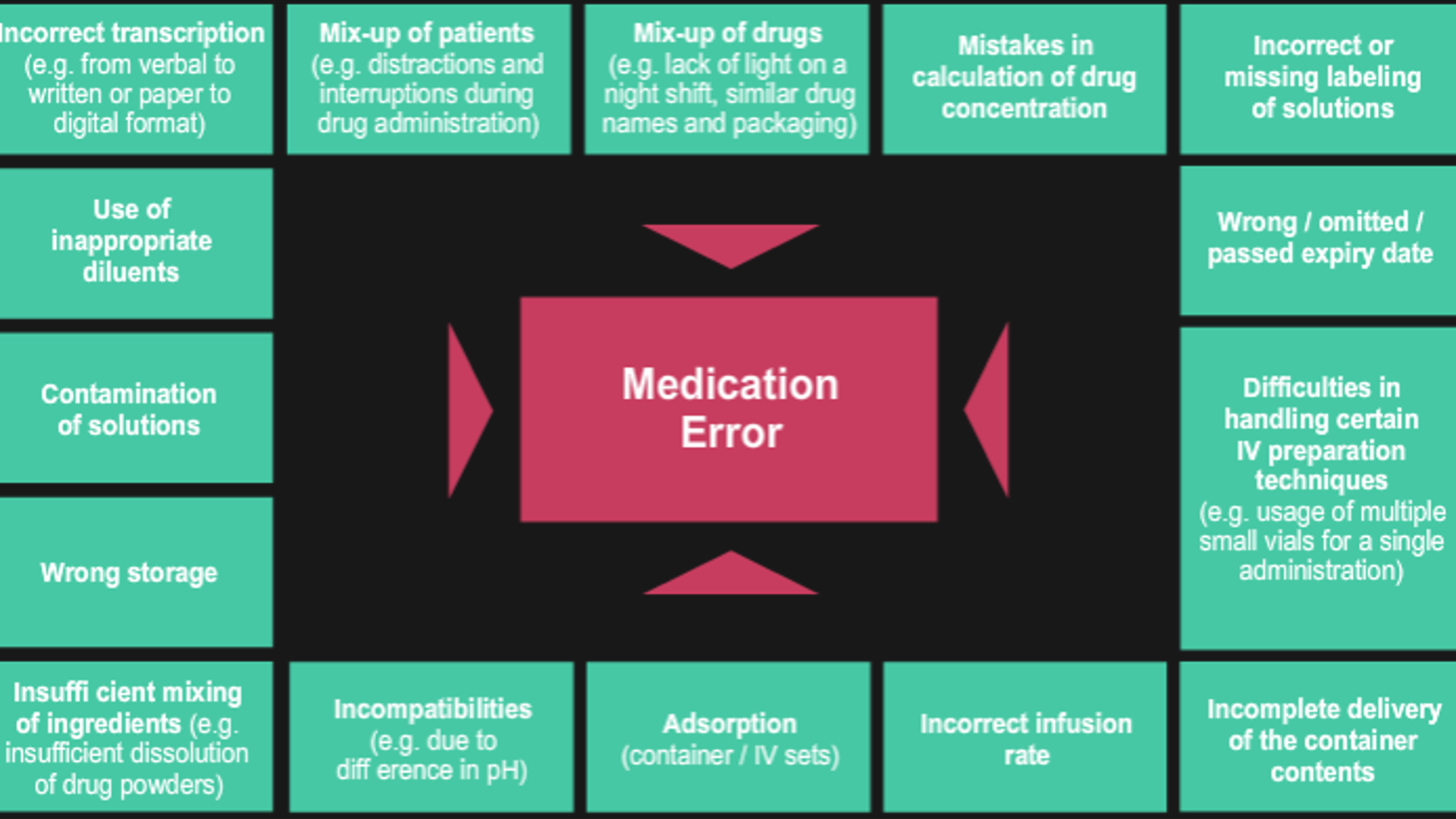
- Medication errors
- Wrong dose
- Wrong person
- Wrong time
- Wrong way route
- No consent
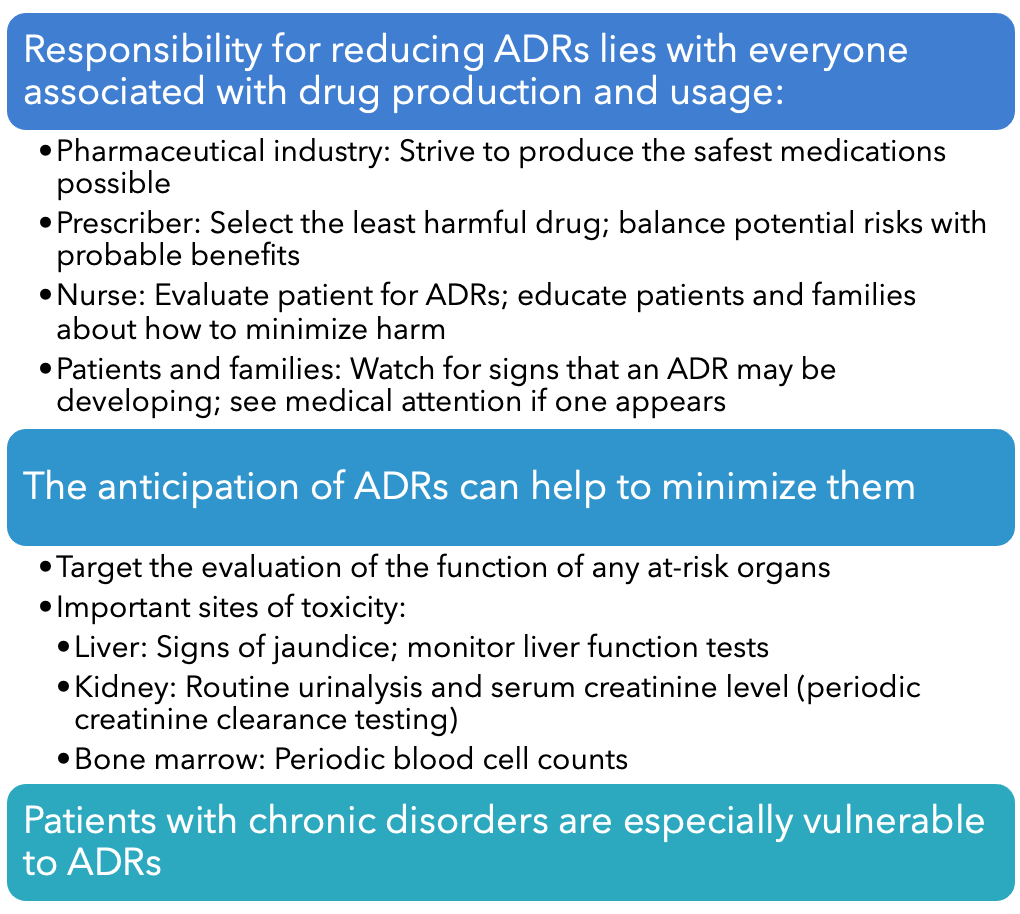
- Adverse drug reactions:
- Defined by the World Health Organization:
- Any noxious, unintended, and undesired effect that occurs at normal drug doses
- Excludes excessive dosages
- Can range from annoying to life-threatening
- Scope of the problem
- Mild reactions
- Drowsiness, nausea, itching, and rash
- Severe reactions (potentially fatal)
- Respiratory depression, neutropenia, hepatocellular injury, anaphylaxis, and hemorrhage
- Most common in the elderly and the very young
- Risk increased by severe illness
- AHRQ (2011): Dramatic rise in adverse drug reactions
- Adverse drug reactions: More than 800,000 outpatients sought emergency treatment for adverse drug reactions
- Hospitalized patients: 1,735,500 experienced adverse outcomes as a result of drug reactions and medical errors
- Of these 1,735,500, more than 53,800 died
- Terms related to adverse drug reactions:
- Side effect
- Toxicity
- Excessive dosing can also be caused by normal dosing though
- Allergic reaction
- Immune response
- Penisilin most common
- Hypoglycemic agents
- Idiosyncratic effect
- Uncommon response from genetic
- Paradoxical effect
- Opposite of drug intended response
- Some insomnia drugs can cause excitement
- Iatrogenic disease
- Physical dependence
- Long time use of certain drugs
- Ex. Opioids, alcohol, amphetamines
- Don't immediately stop the drugs. It can lead to seizures and death
- Carcinogenic effect
- Drugs to treat cancer are carcinogenic
- methotrexate for arthritis but it's carcinogenic and needs to be stored properly.
- Teratogenic effect
- If taken while pregnant = leads to birth defects.
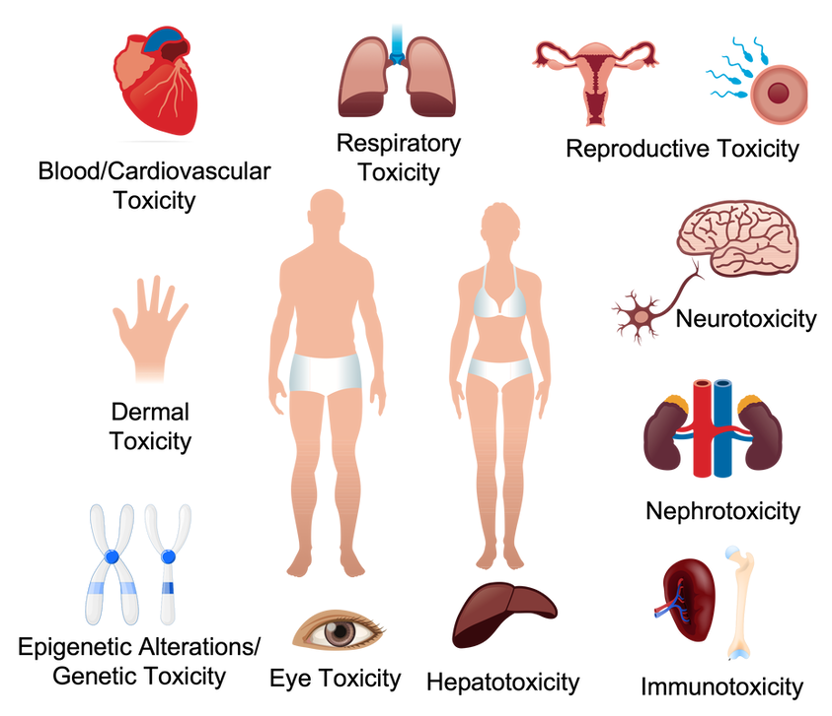
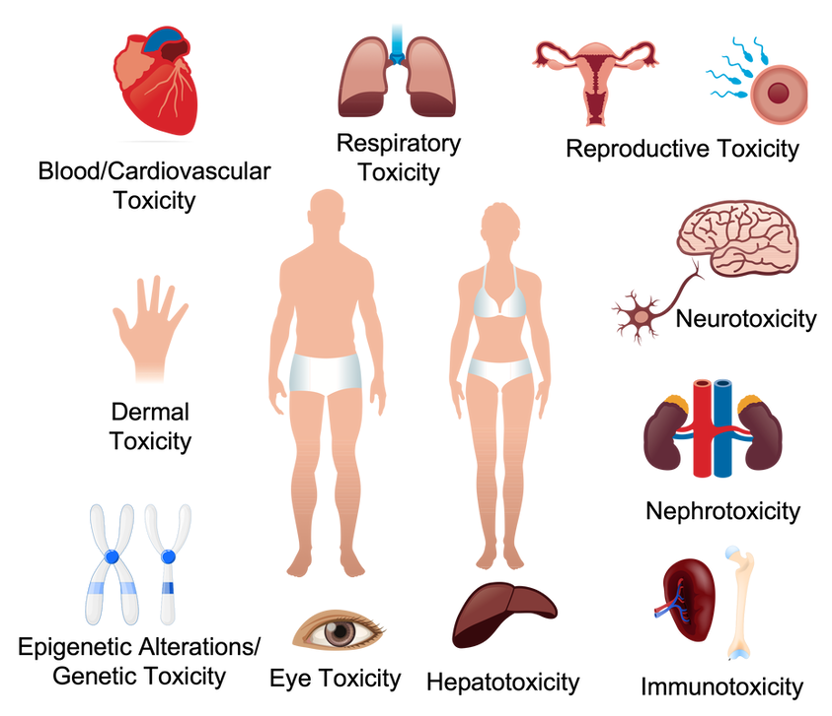
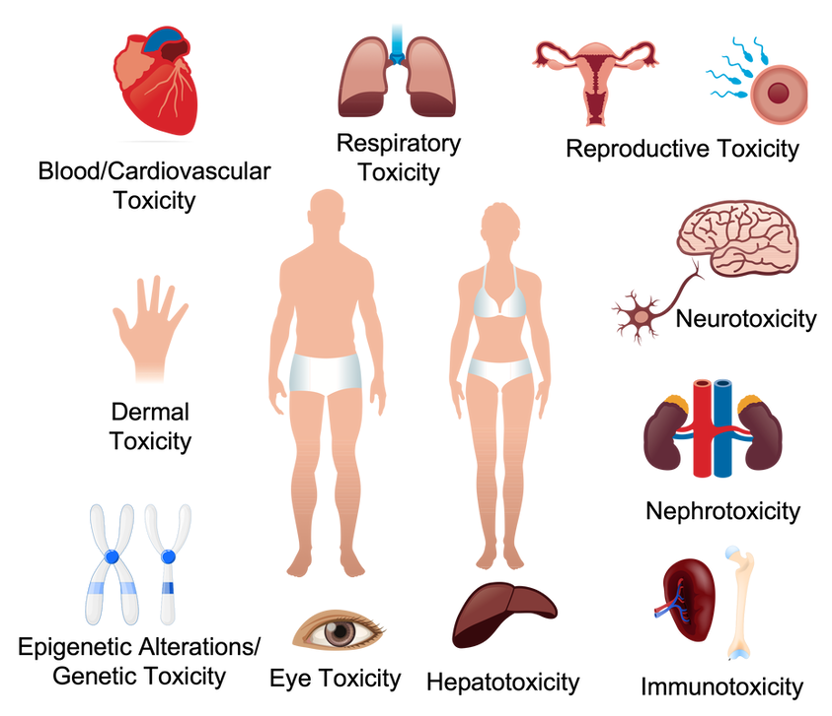
- Organ-specific toxicity:
- Many drugs are toxic to specific organs
- Common examples include:
- Kidneys: Amphotericin B (antifungal)
- Heart: Doxorubicin (anticancer)
- Lungs: Amiodarone (antidysrhythmic)
- Inner ear: Aminoglycoside (antibiotic)
- Hepatotoxic drugs
- QT interval drugs
- QT = cardiac symbol on the ECG
- PQRST = shape
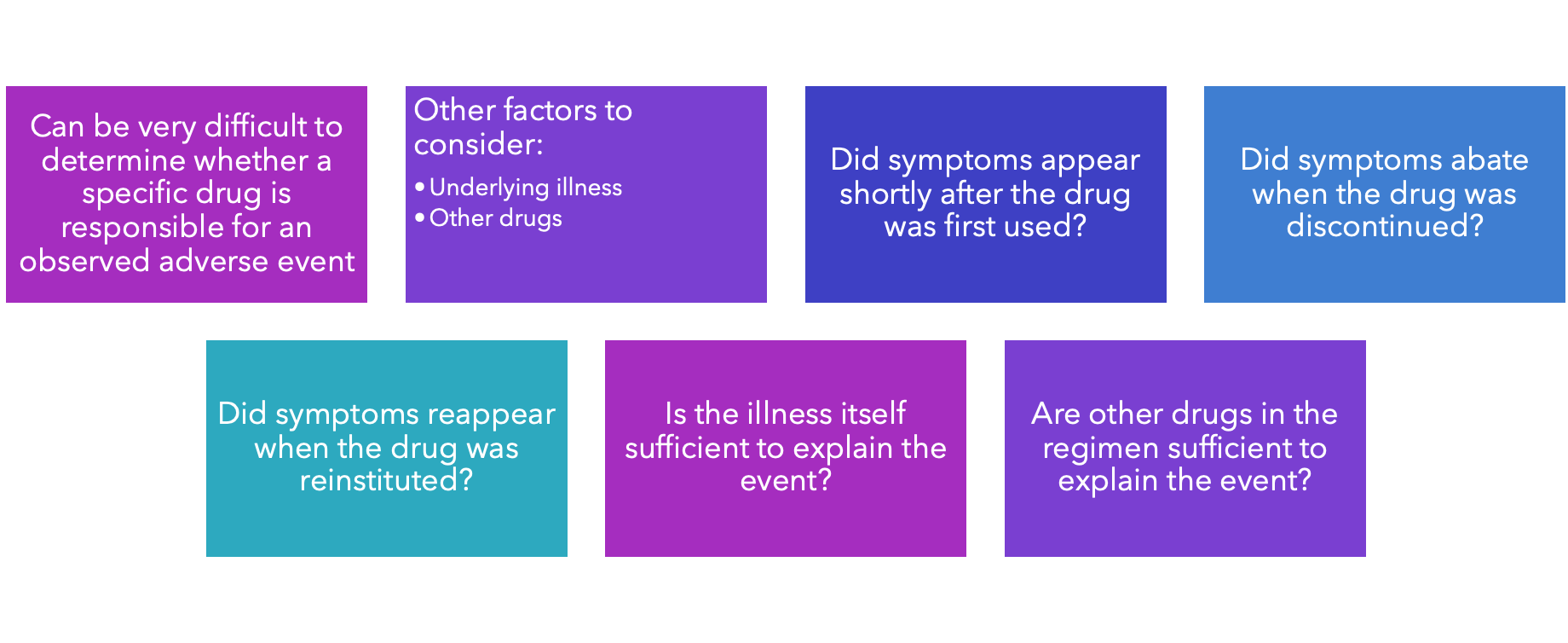
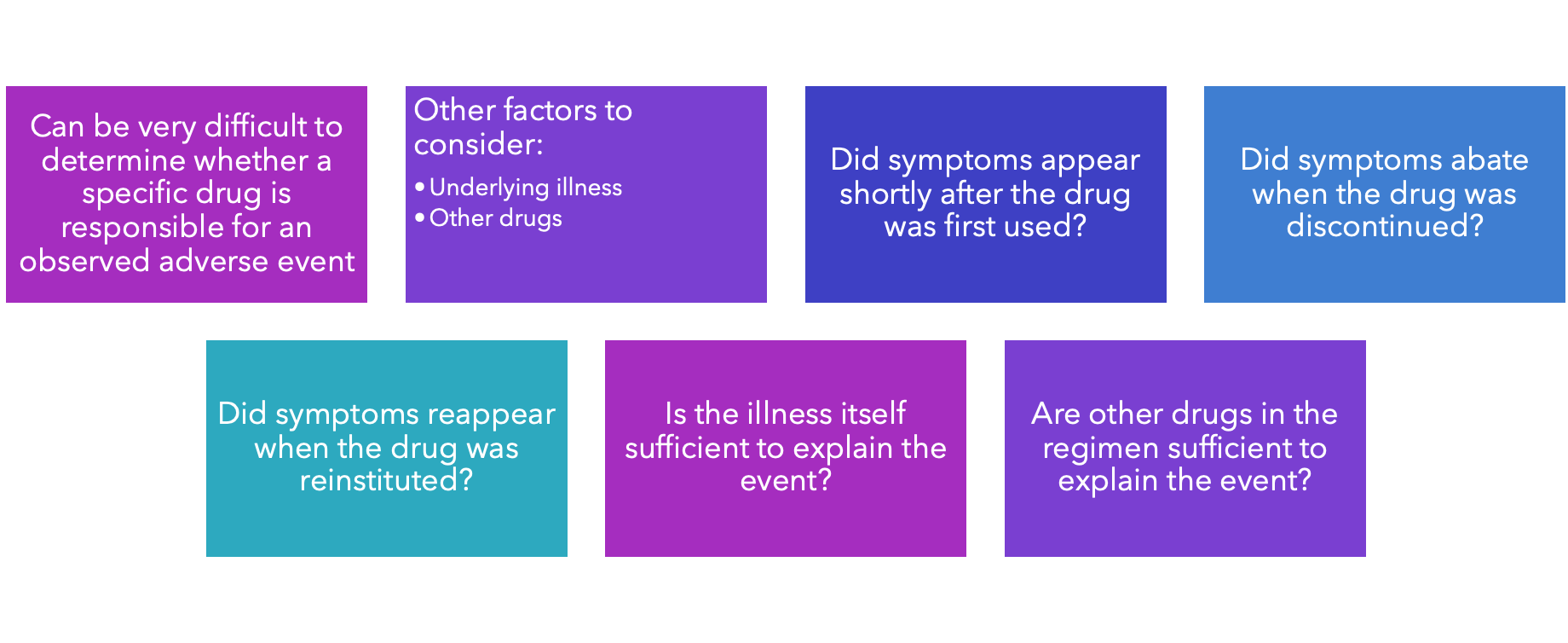
- Identifying adverse drug reactions:
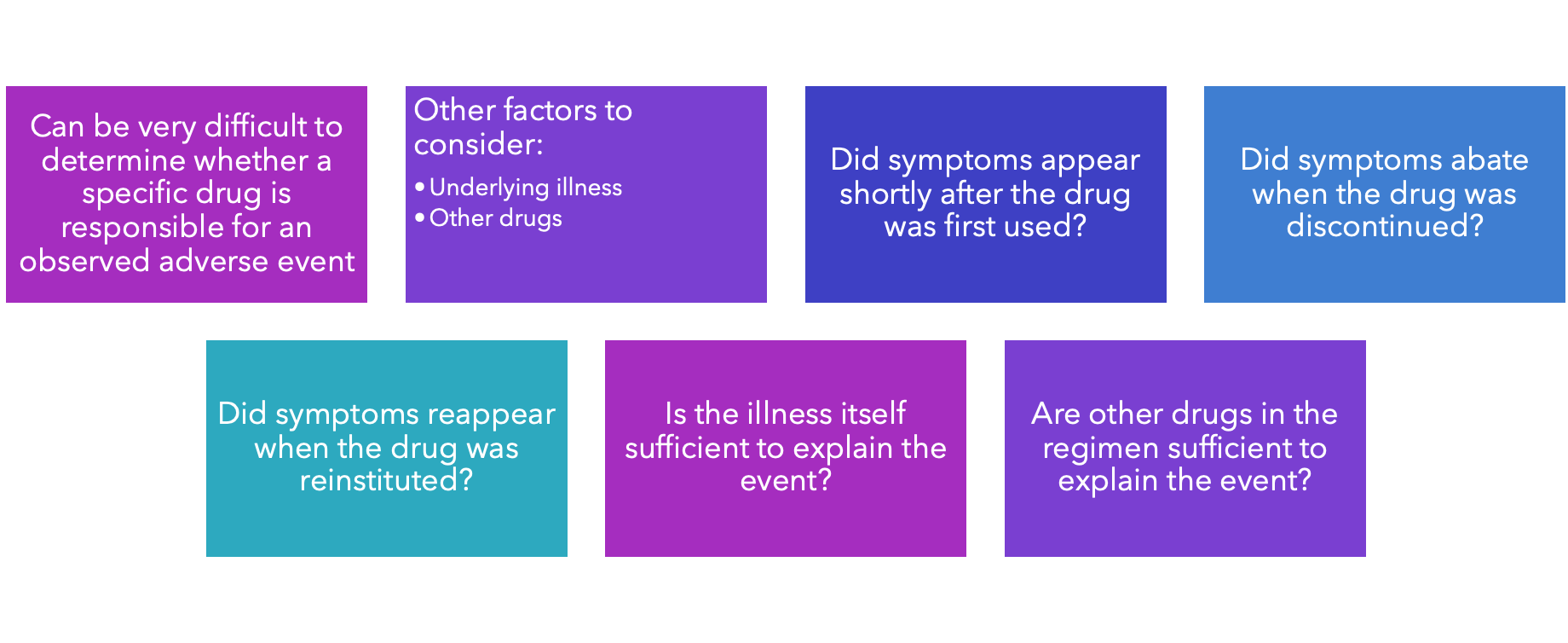
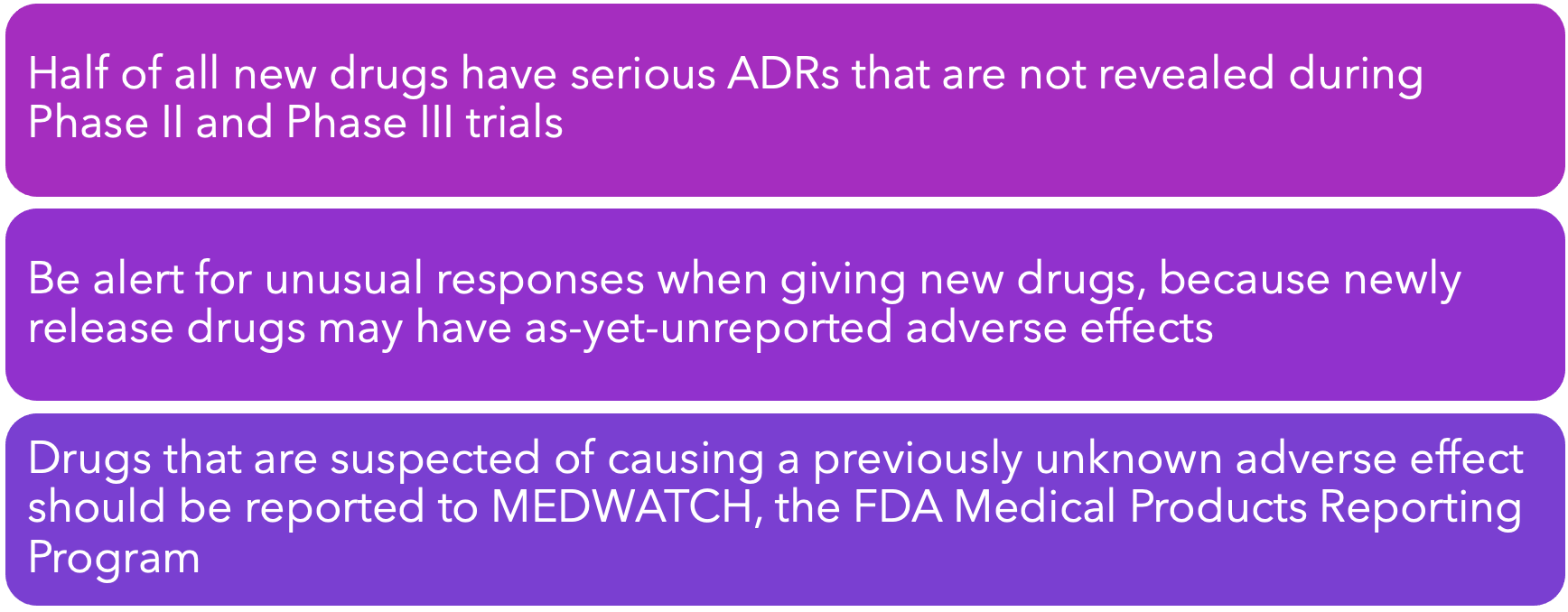
- Adverse reactions to new drugs:
- One way to minimize adverse drug reactions
- know patient history
- Recognition and conciliation
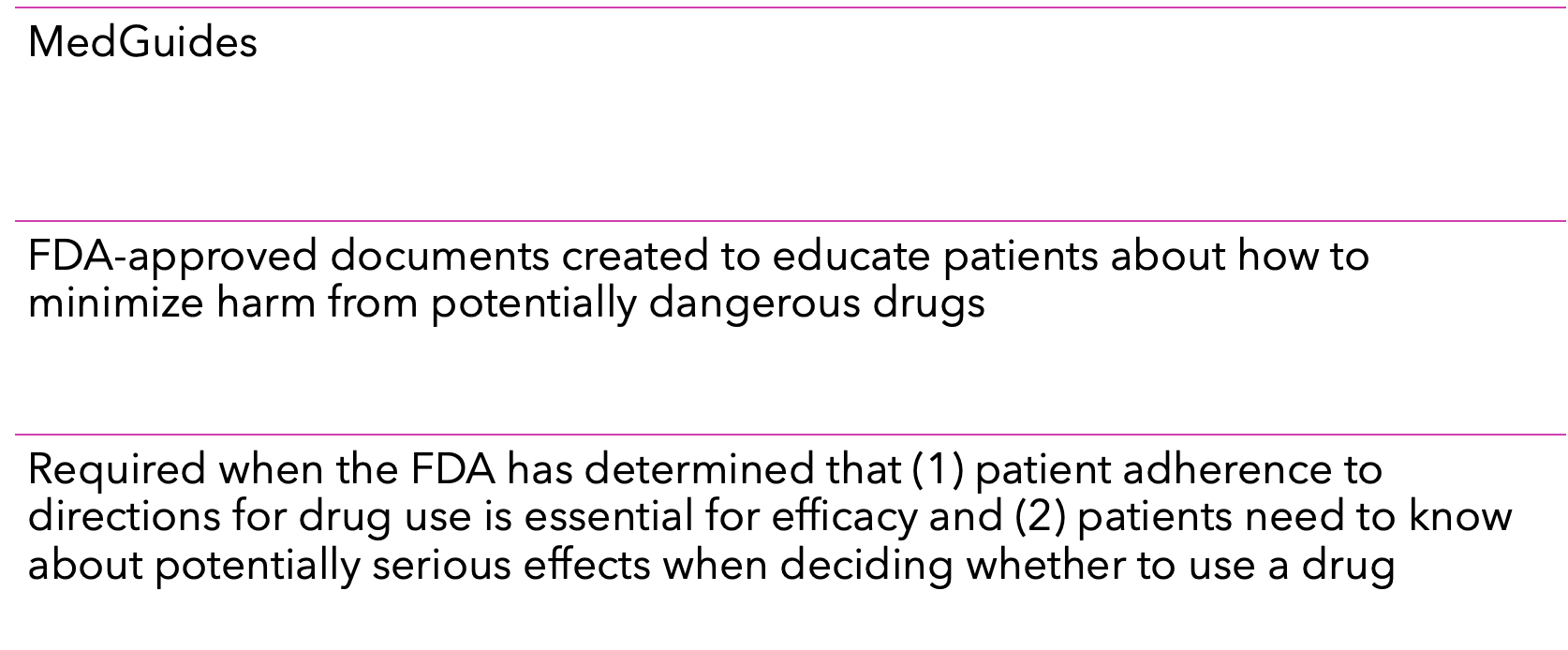
- Ways to minimize adverse drug reactions:
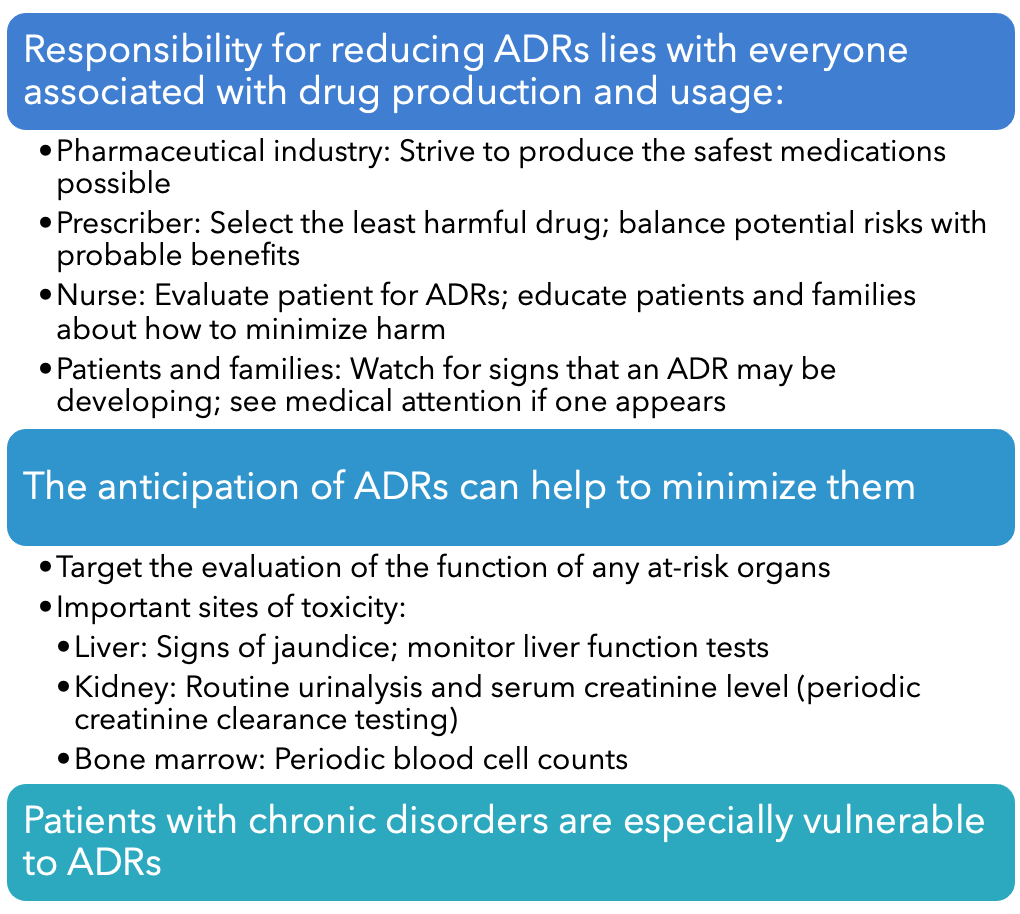
- Boxed warnings:
- Also known as black box warnings
- Strongest safety warning a drug can carry and still remain on the market
- Purpose of this warning is to alert prescribers to:
- Potentially severe side effects (eg, life-threatening dysrhythmias, suicidality, major fetal harm)
- Ways to prevent or reduce harm (eg, avoiding a teratogenic drug during pregnancy)
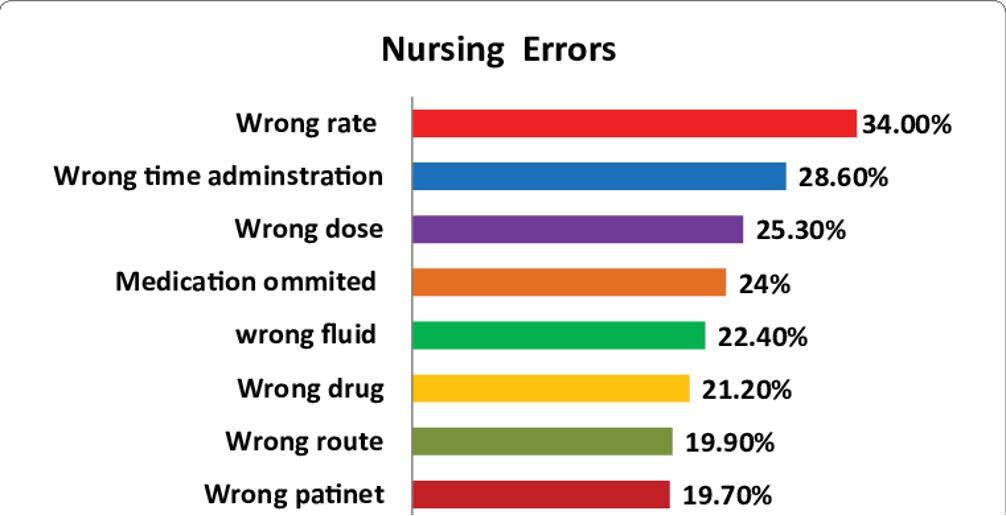
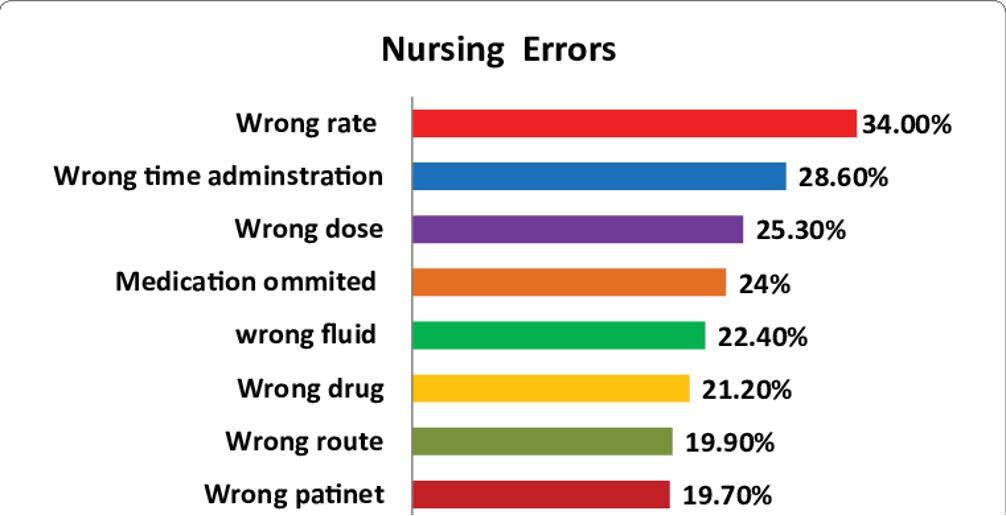
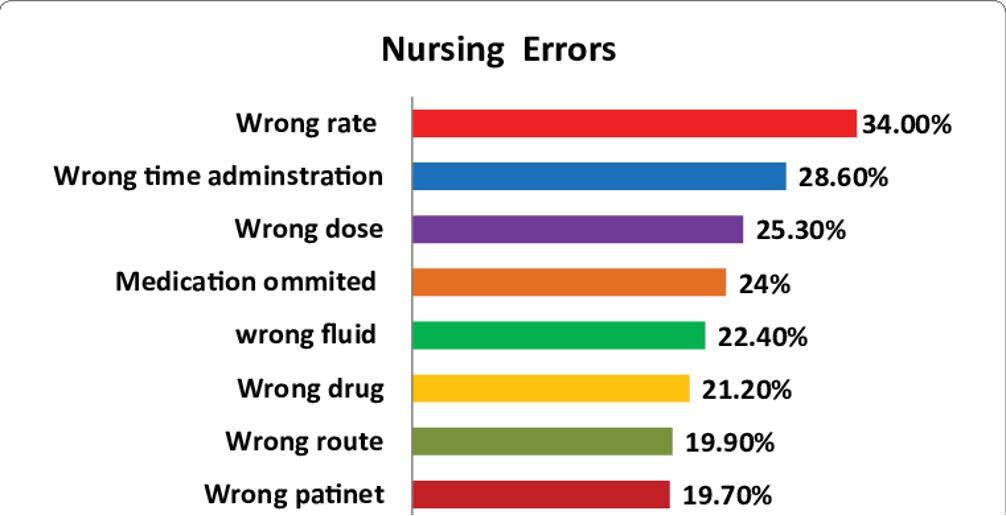
- Most common medication error
- Window: 30 mins before and 30 mins after
- Wrong time
- Wrong dose
- Misdose
- Wrong person
- Medication errors:
- Wrong rate
- Major cause of morbidity and mortality
- Documented in two landmark reports from the Institute of Medicine:
- To Err Is Human, 1999
- Preventing Medication Errors, 2006
- It is estimated that medication errors:
- Injure 1.5 million people per year
- Kill 7000 people per year
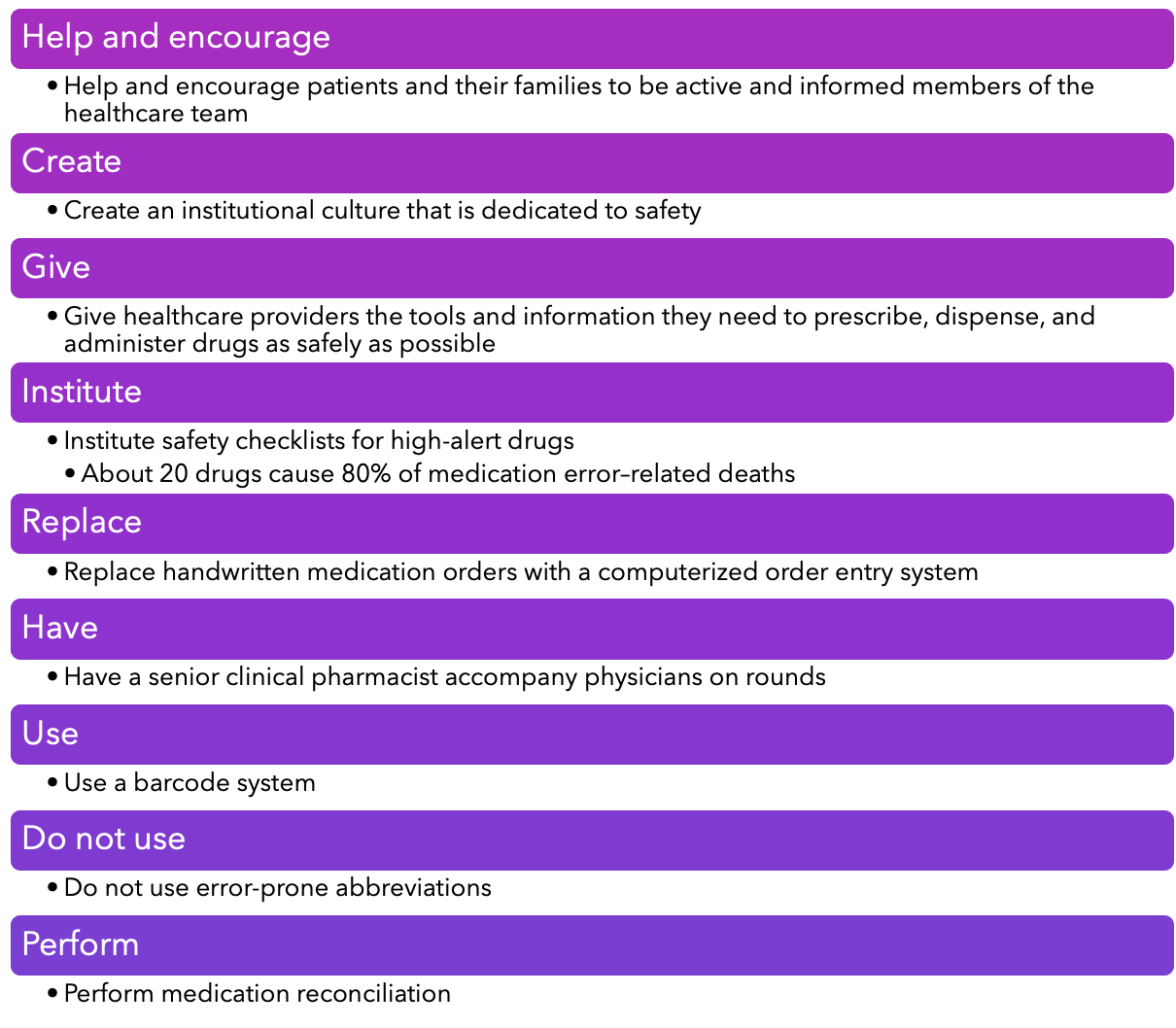
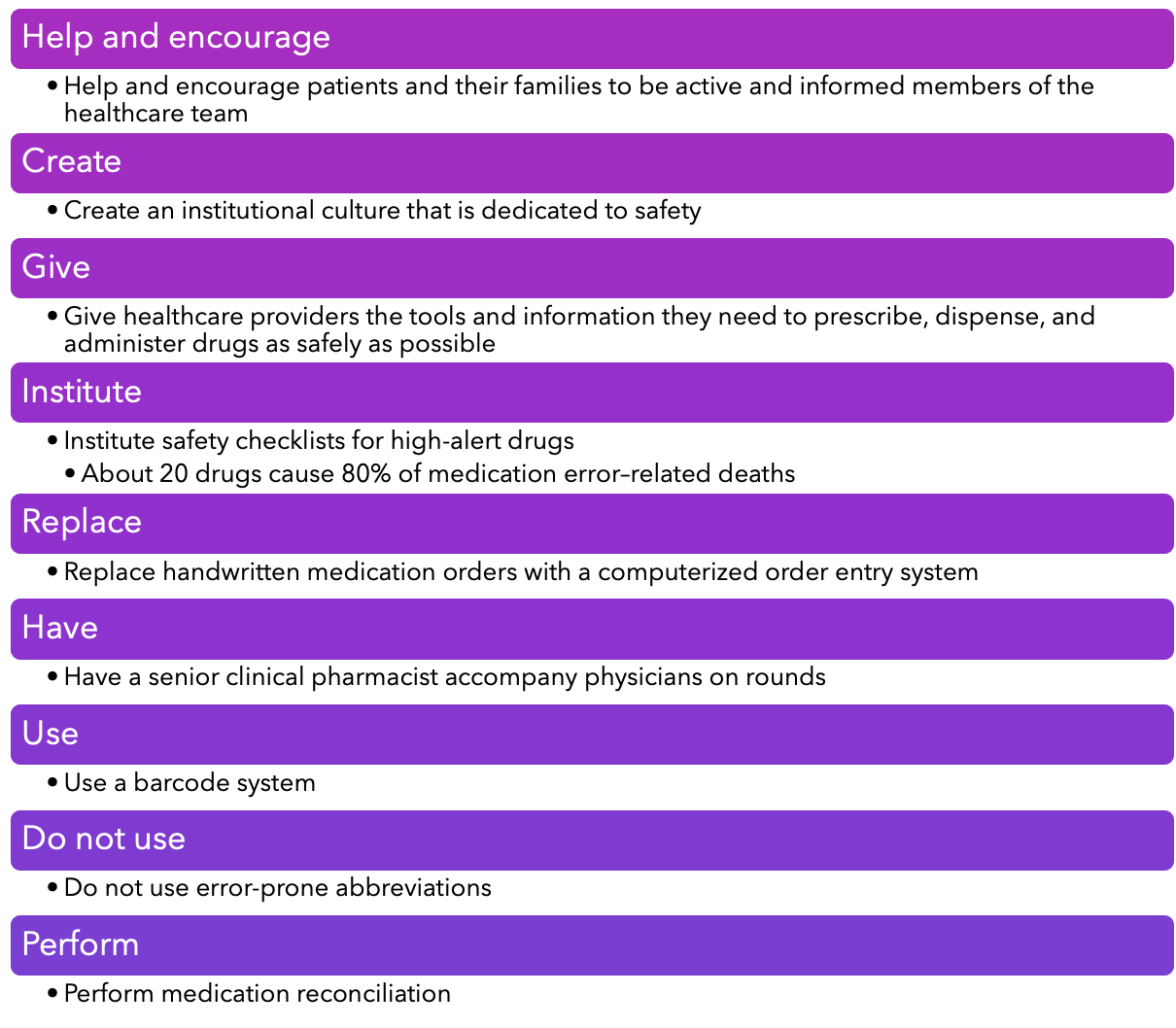
- Ways to reduce medication errors:
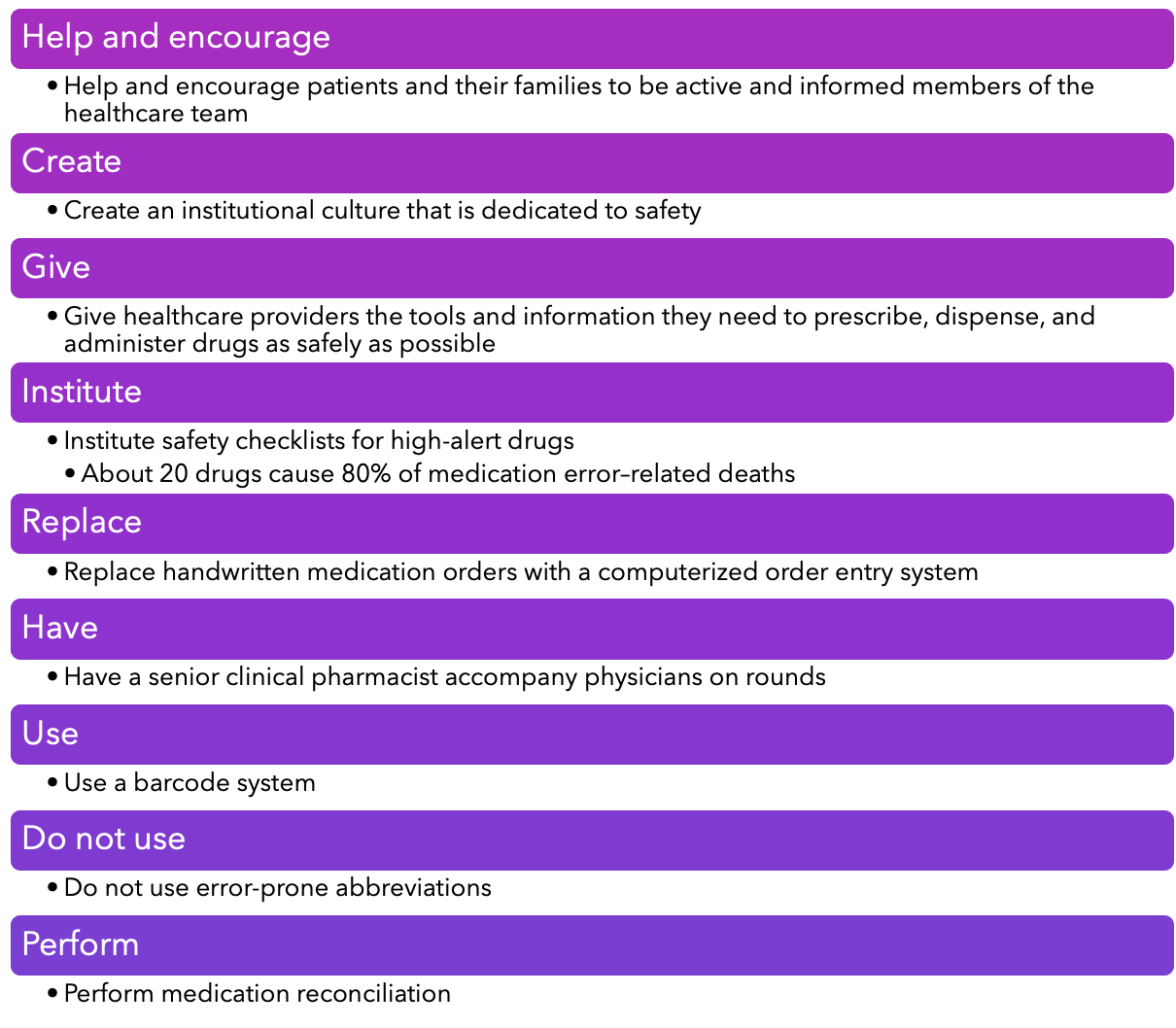
- How to report a medication error:
- Medication Errors Reporting (MER) Program:
- Reporting is confidential
- Reporting can be done by phone, fax, or Internet
- Program encourages all healthcare providers—including pharmacists, nurses, physicians, and students—to report errors
- https://www.ismp.org/orderforms/reporterrortoismp.asp
- All information is forwarded to the U.S. Food and Drug Administration (FDA), the Institute for Safe Medication Practices (ISMP), and the product manufacturer
- Case study:
- You are a new nurse who recently completed orientation on the medical/surgical unit. Your first patient of the day was prescribed ampicillin 1 g/100 mL to infuse over 30 minutes to be administered 1 hour before a colonoscopy. You review your medications in your mobile application and find that ampicillin is an antibiotic and should not be administered to patients allergic to penicillin. You review the patient’s history and see that the record reveals an allergy to penicillin and shellfish. You decide to review this history with the patient.
- 1. What questions would you ask this patient?
- Case Update: Your patient states that he or she has nausea and vomiting when he or she takes penicillin.
- 2. How would you proceed with caring for this patient?
- Case Update: You are asked to cover for a colleague who has stepped off the unit. The patient has intravenous (IV) ampicillin infusing. You check the patient’s chart and see that the record reflects that this patient is allergic to penicillin.
- 3. You go into the patient’s room, and the patient is having difficulty breathing. How do you handle this situation?
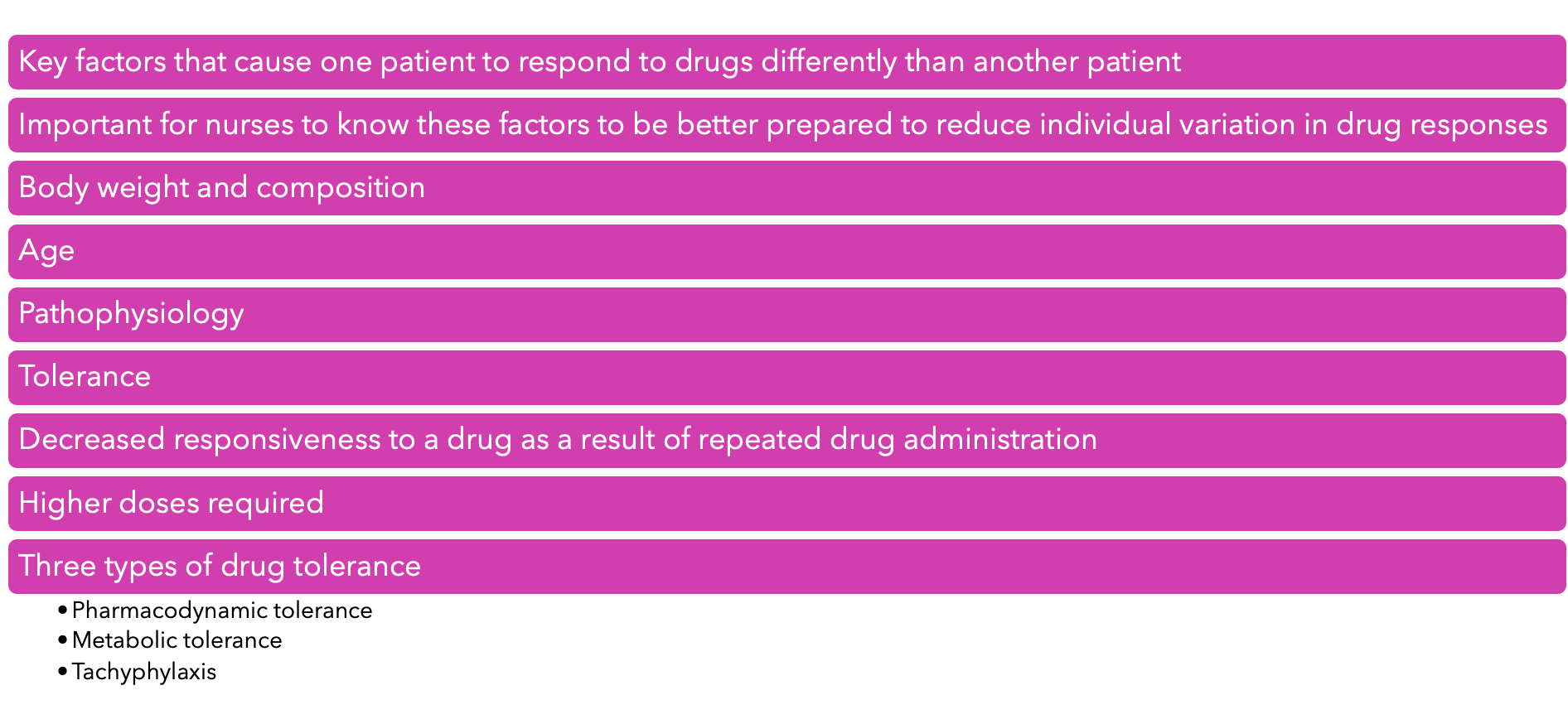
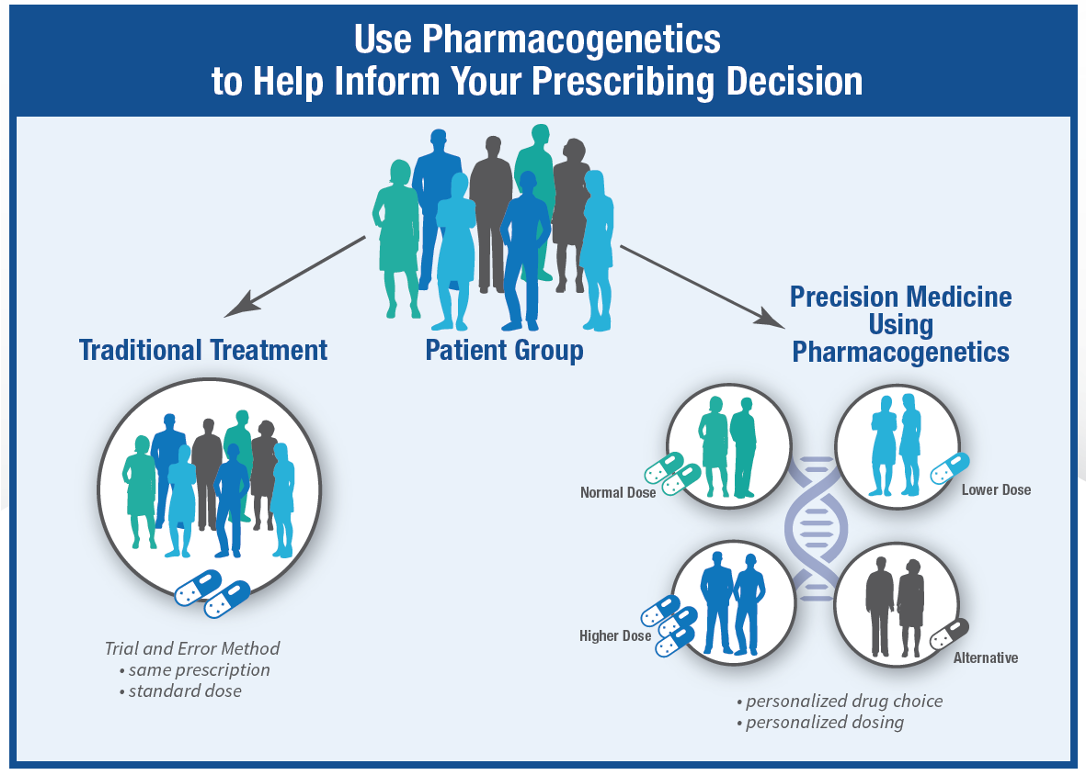
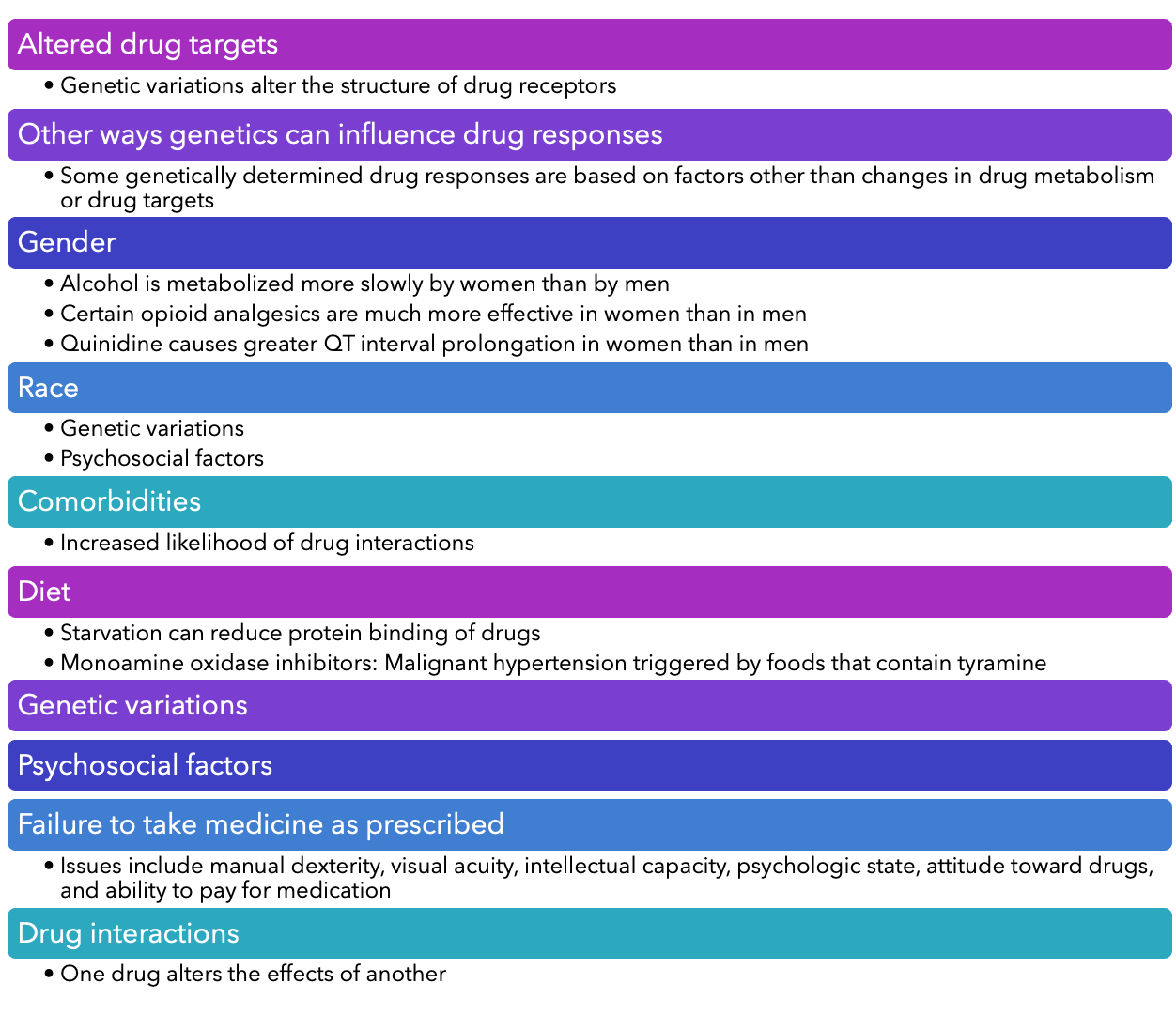
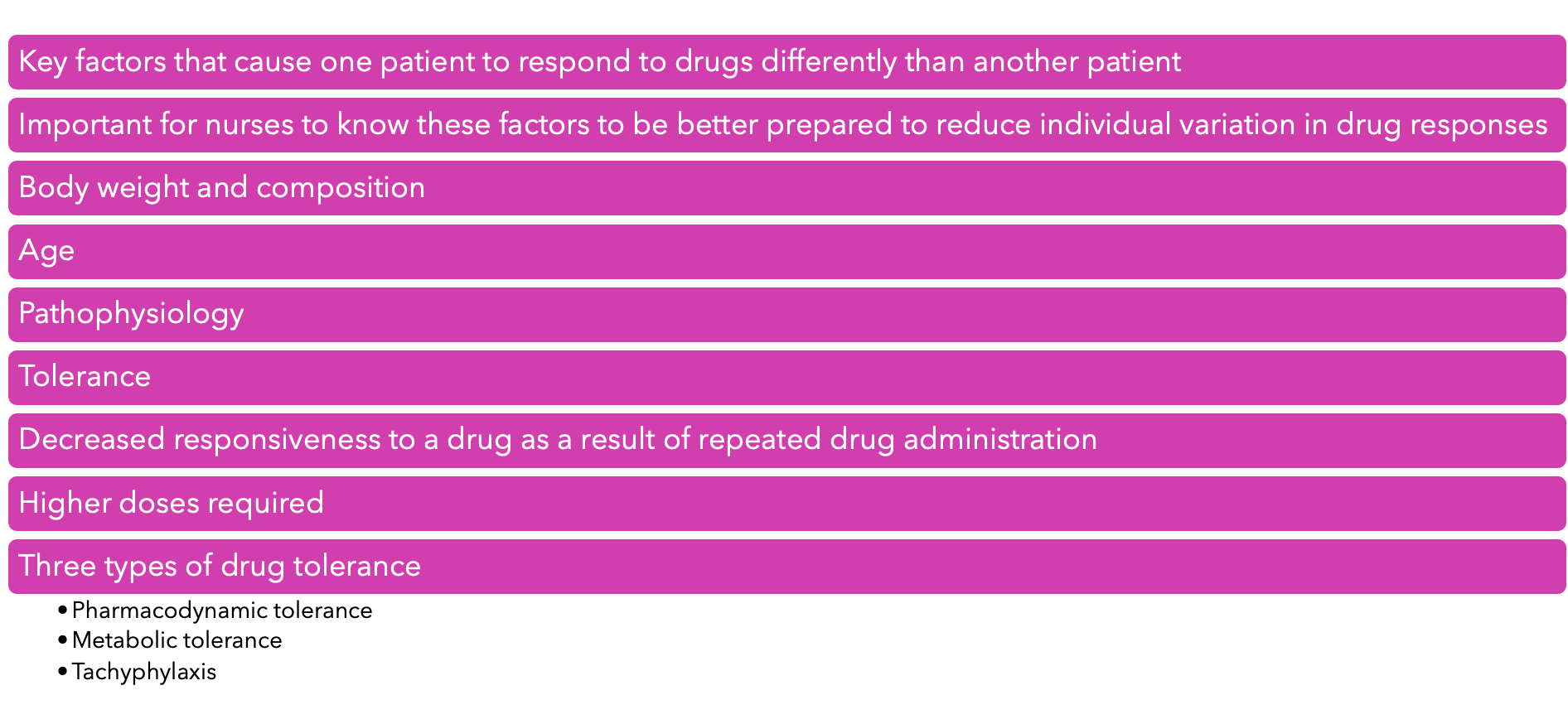
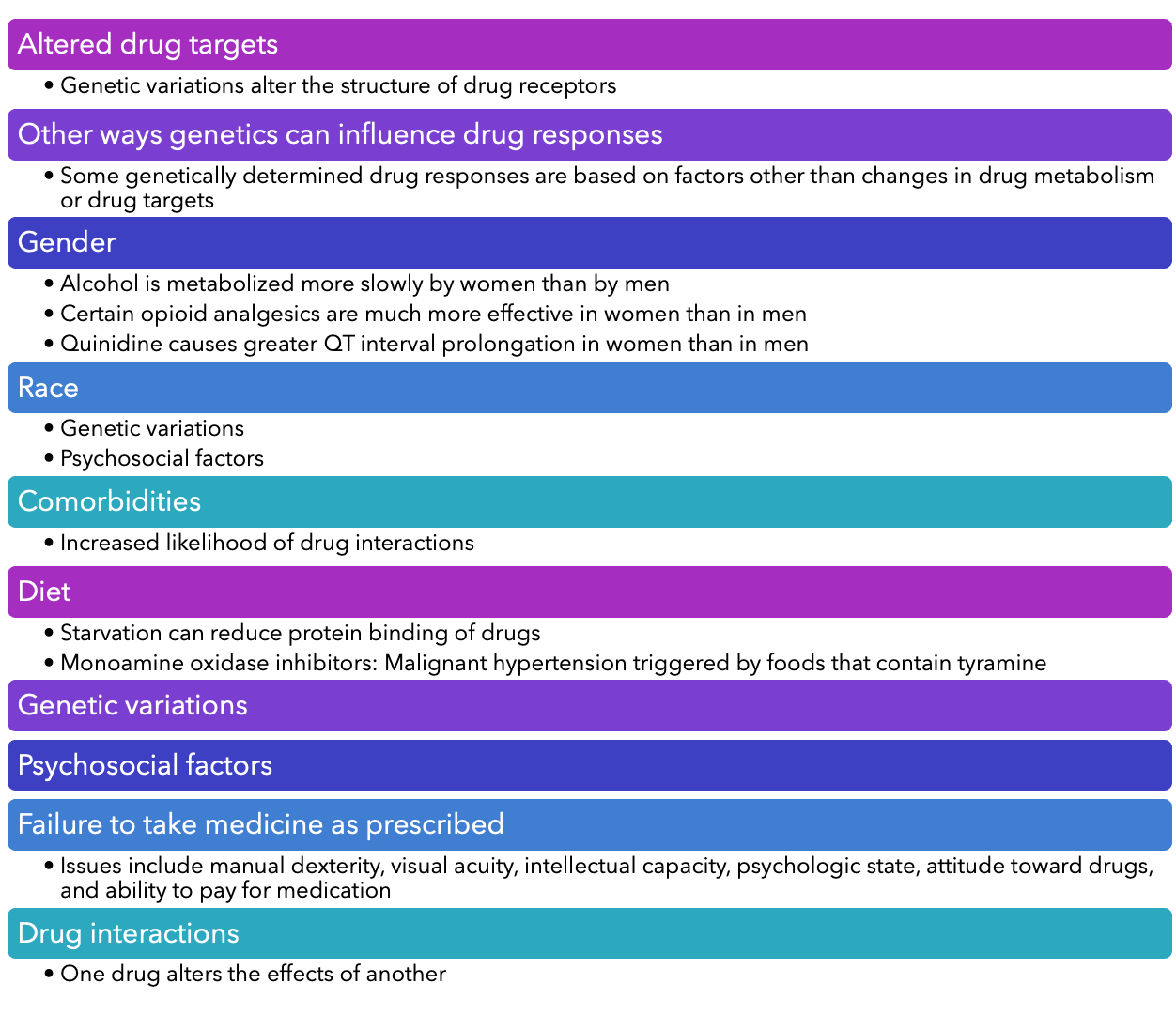
- Individual variation in drug responses:
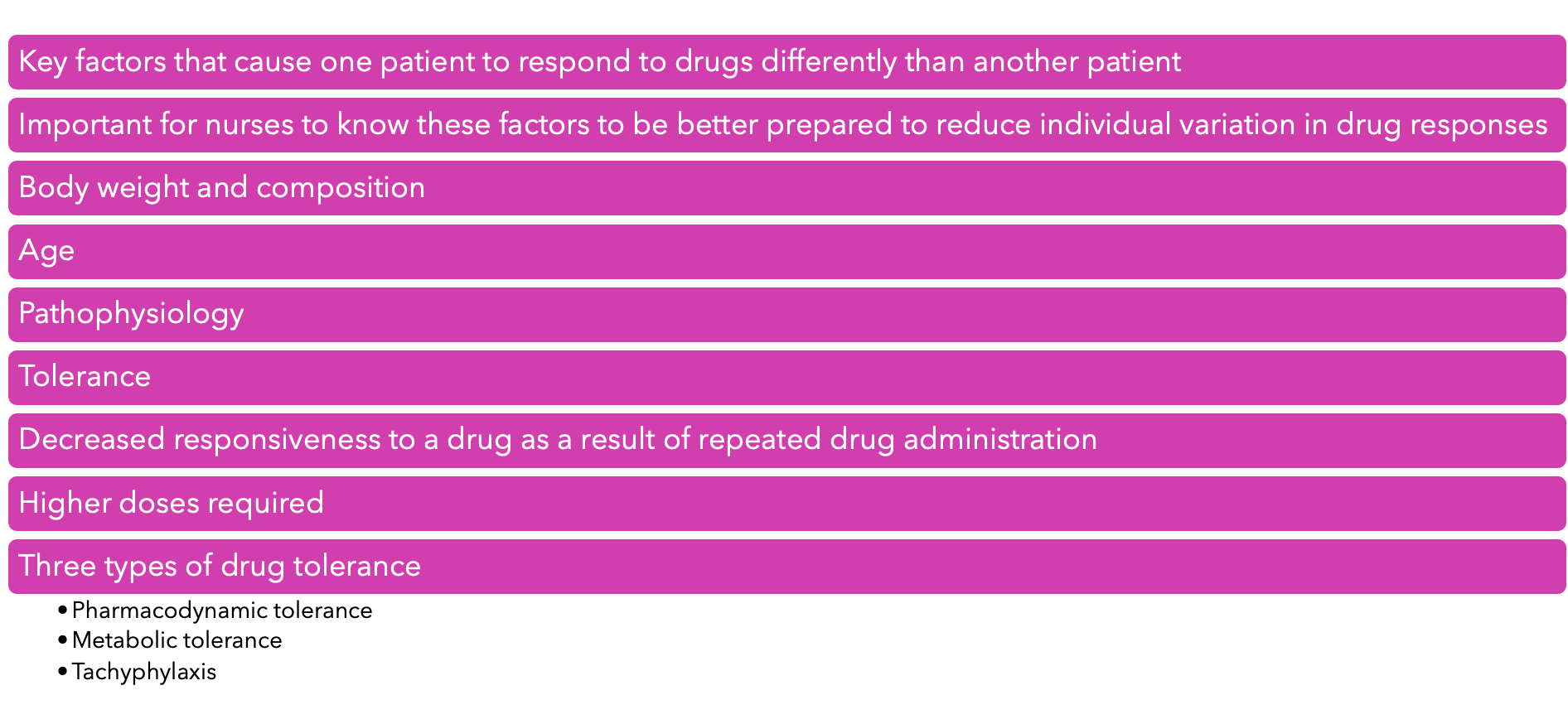
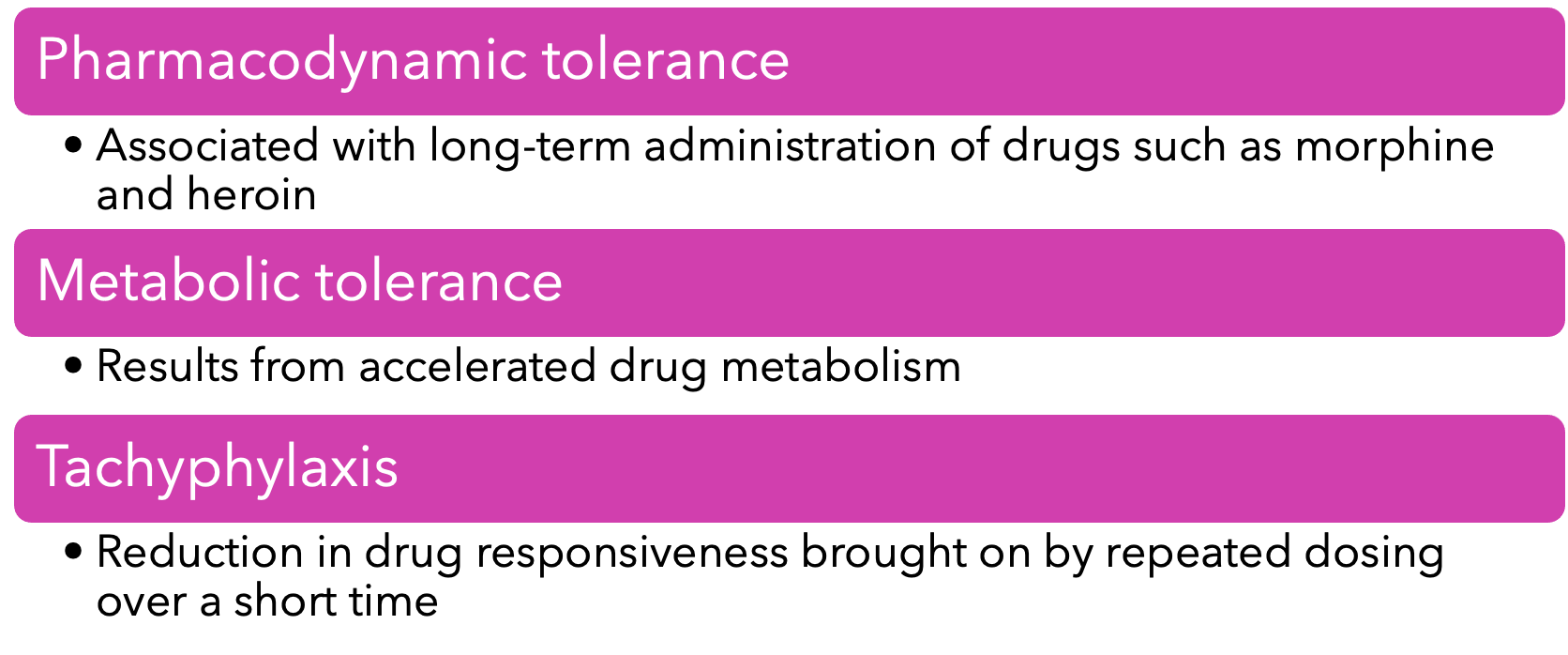
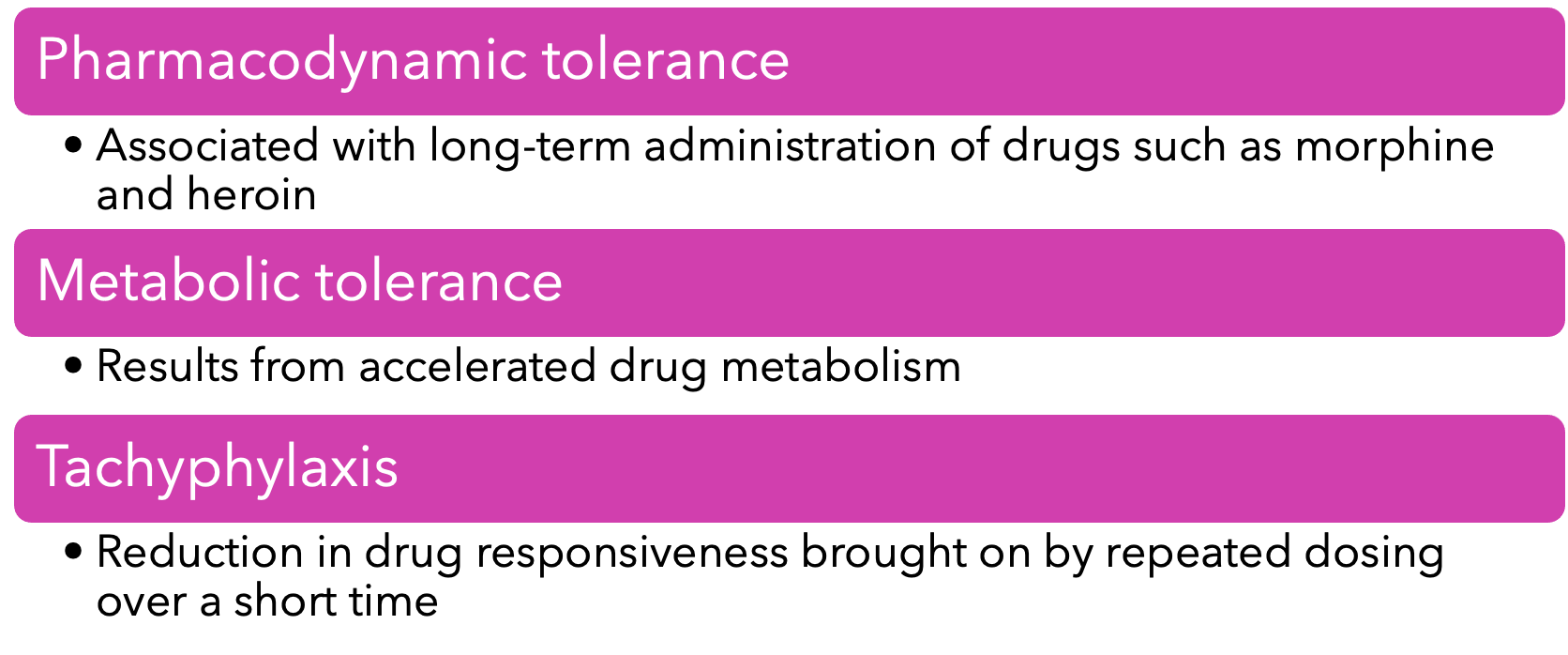
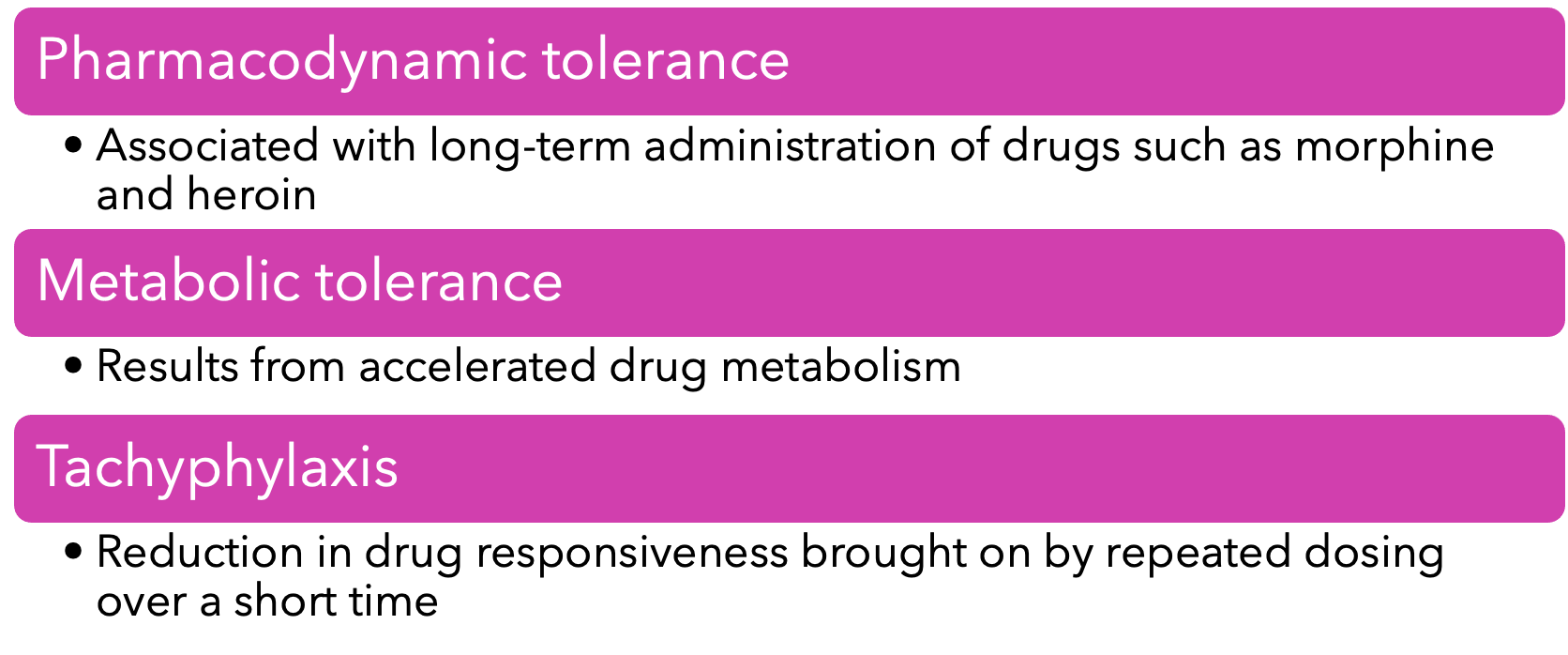
- Three types of drug tolerance:
Psychosomatic: brain controlling what's happening in body
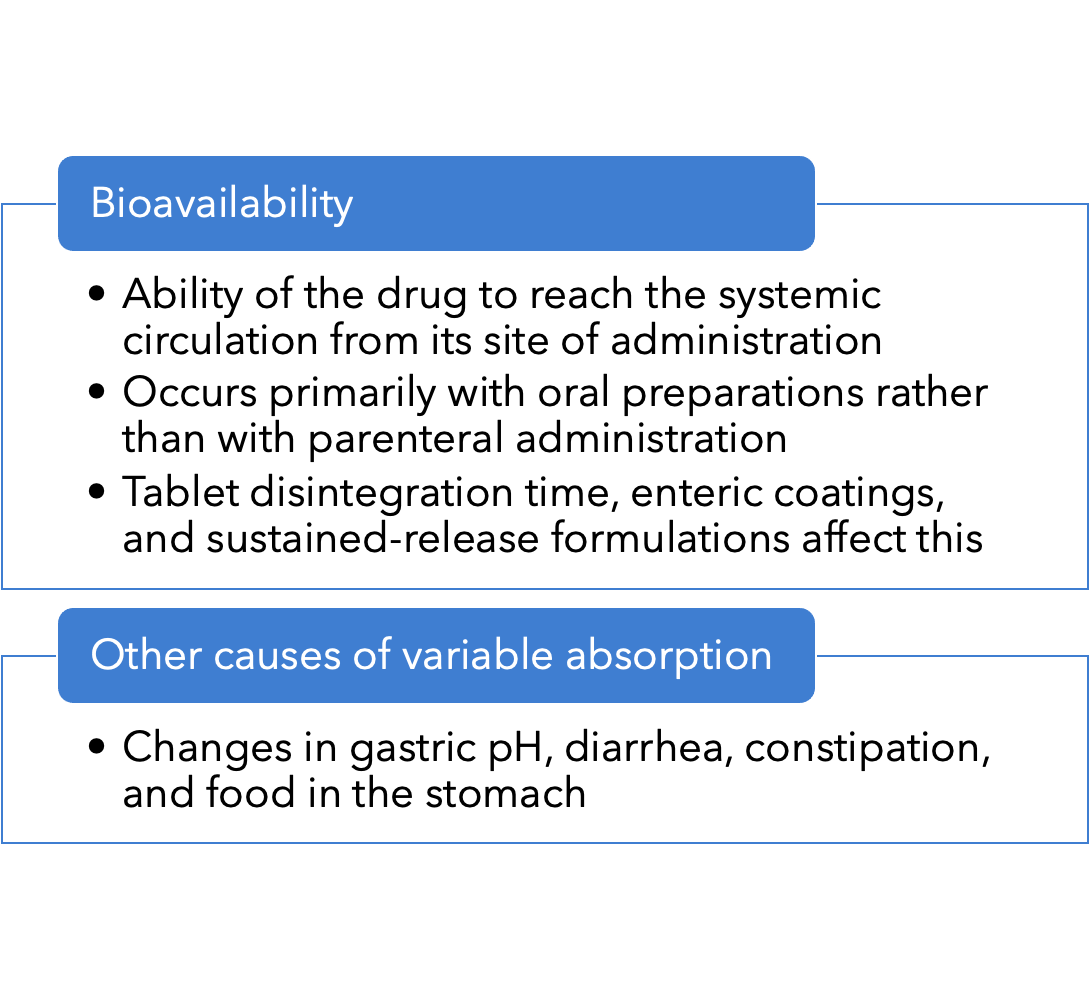
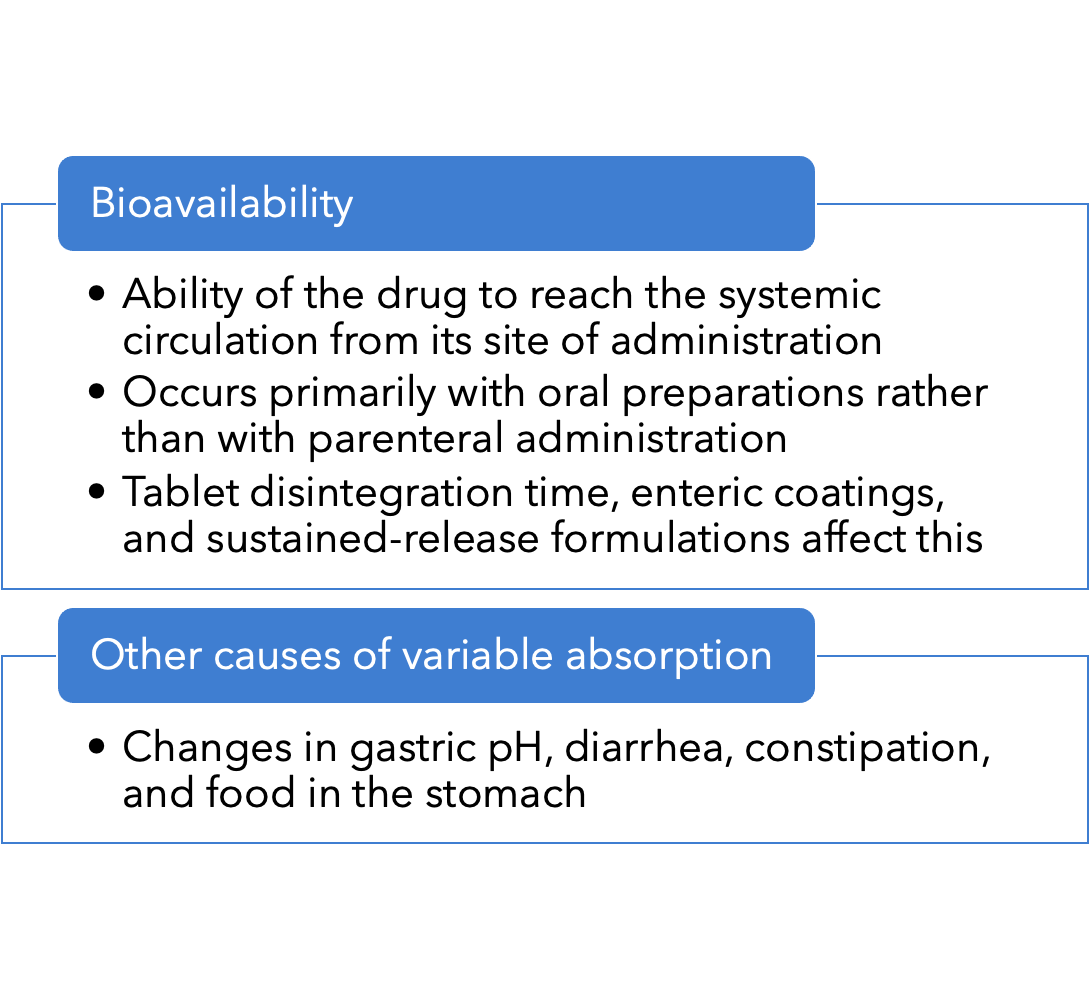
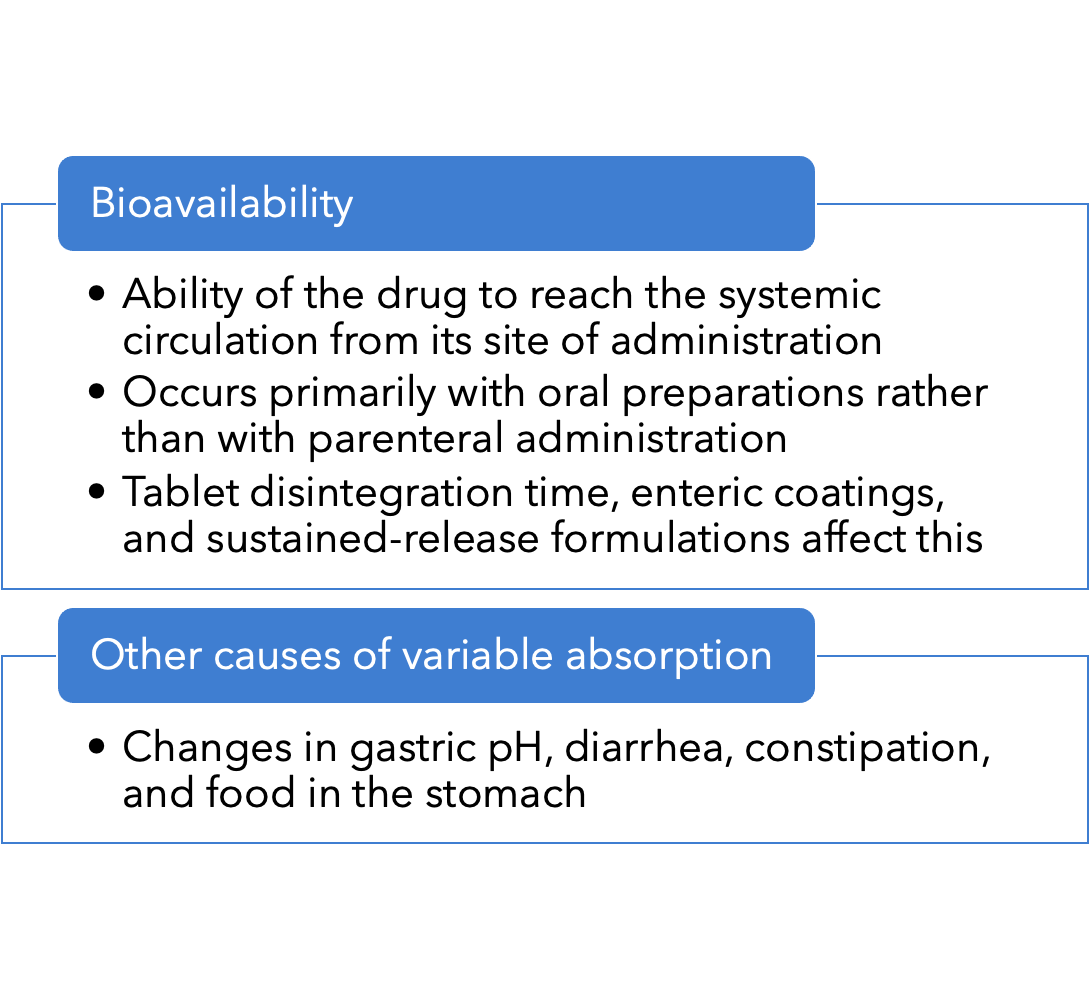
- Variability in absorption:
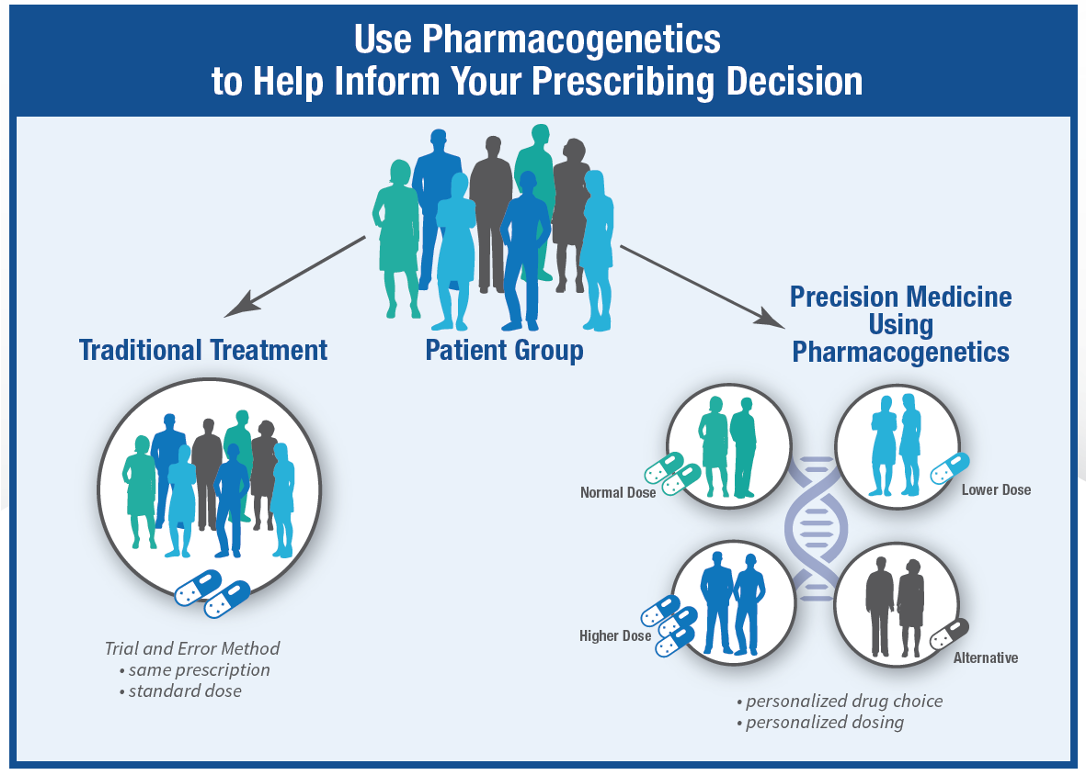
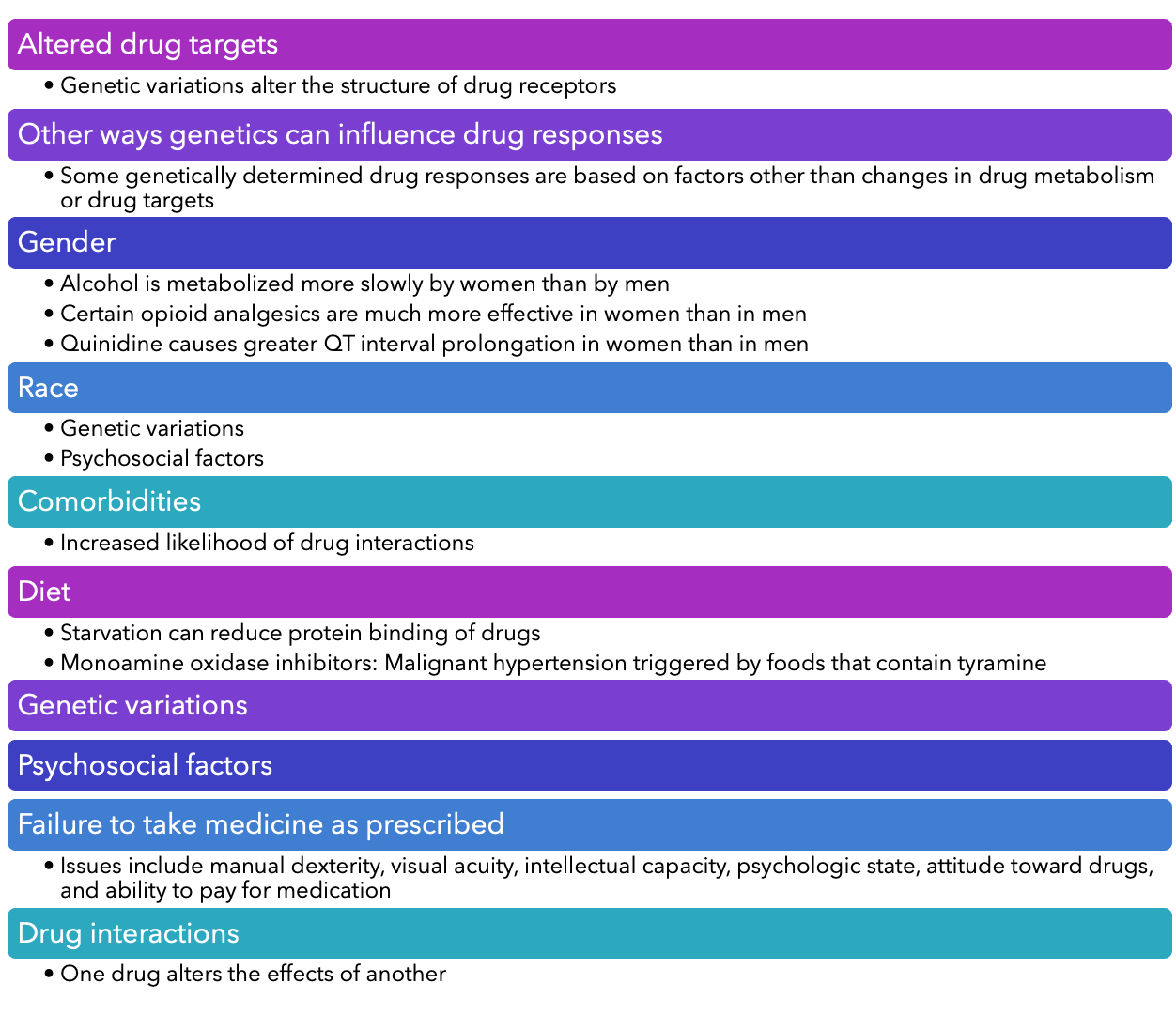
- Genetic and pharmacogenomics:
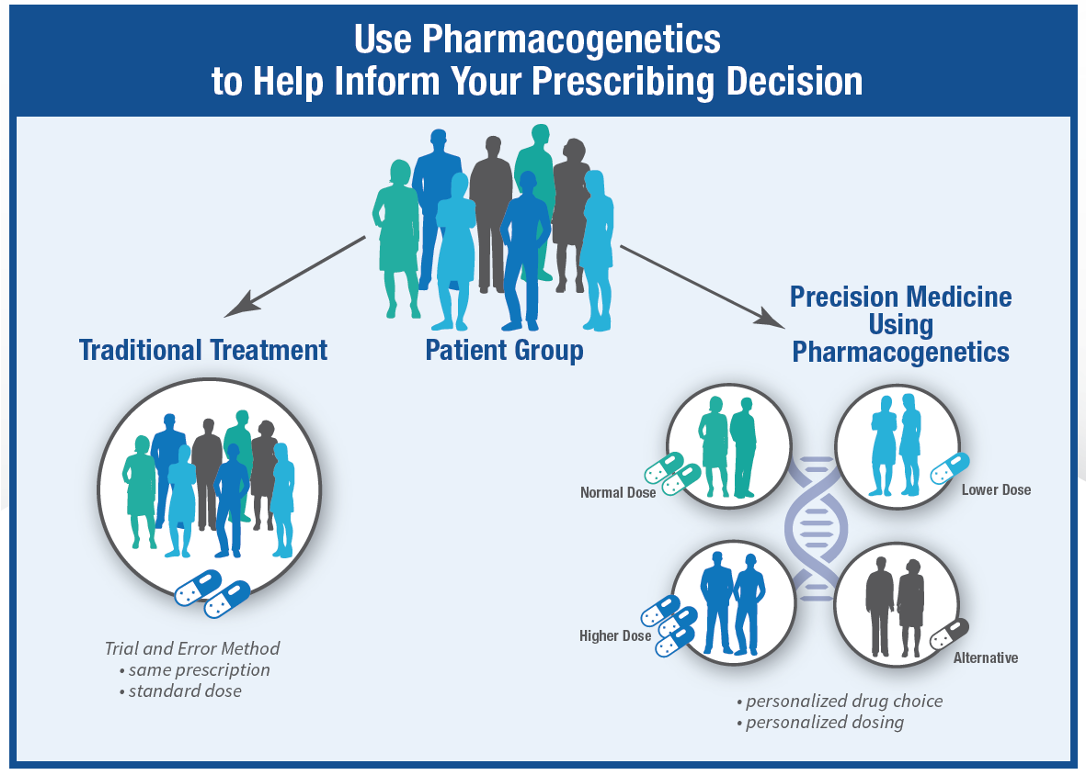
- Pharmacogenomics: Study of how genes affect individual drug responses
- Altered drug metabolism
- May accelerate or delay the metabolism
- Warfarin, succinylcholine, isoniazid, cytochrome P450
- Variations:
Nurse researcher working pahrma compnay
- What is best response
- What does bioavailabolty mean and why is it important to me
- The amount that gets absorbed and used for therapeutic use
- What s your best response can you please epakun what is meant by variants that may alter drugf metabolism