Microbiology Chapter 17: Adaptive Immunity
Adaptive Immune Response; specific, induced by antigen
Lymphocytes → B type, T type
Humoral Immunity: deals w/ extracellular pathogens
B type develop into plasma cells and memory cells
Plasma cells →
produce antibodies → bind into extracellular pathogens
Memory cells - can recall a particular antigen that activated them
Cell-mediated Immunity: deals with intracellular pathogens
T types develop into effector cells
Effector cells
Kills possessing intracellular pathogens → cytotoxic T cells
Activate other cells of the immune system → T helper cells
Some T helper cells will interact with B cells and help activate them
Antigens (Ag) are molecules that in the body, activate lymphocytes:
B cells: interact w/ antigen via surface immunoglobulins i.e, antibodies
T cells: interact w/ antigen via surface antigen receptors
Antigens are molecules on the surface of a pathogen
Epitope - part of the antigen that immune cells bind onto to detect it
Interactions with antigens occur with smaller segments called epitopes or antigenic determinants
Epitopes that elicit an immune response can be a protein, peptide, or complex polysaccharides
Antibody Structure and Diversity
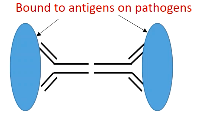
Antigens are proteins so they’re comprised of polypeptide chains
Variable regions of these chains possess variable amino acid sequences and are the antigen binding sites
Variable regions can change depending on the amino acid sequence
There are two of these regions on the end of each molecule. Variable regions is where antigen binding occurs
There are also Fc regions where the binding of the host cell occurs
Antibody classes - IgG, IgD, IgE are monomer forms; IgM and IgA are aggregates of 2 or more monomers.
All antibody classes are defined by the Fc region
Each class can differ in their variable regions
IgM and IgA can form polymers
IgA (15%): dimer; found mainly in mucosal surfaces & in secretions. Prevents pathogens attachment to surfaces
Two pathogens can connect to the FC portion of the antigens and so there’s four binding sites on the antigens
Found mostly in mucosal secretions and mucosal surfaces
Used to prevent attachment of pathogens to mucosal surfaces by binding them to the antigens
IgG (75%): monomer; most abundant in blood & tissue fluids; opsonization, activate complement; neutralize viruses
IgD (.2%): found on B cells & in blood, lymph
Found on the surfaces of B cells
Pathogen binds on the IgD on the surface of the B cell which can lead to the B cells creating antibodies
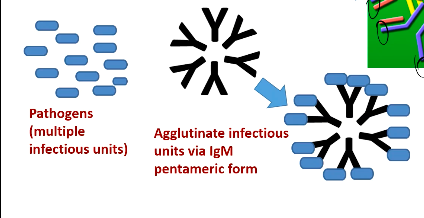
IgM (10%); circulating type is a pentamer; generally remains in blood vessels. First Ab detected in immune response; effective in agglutination & complement activation
Five antibodies come together with IgM
10 binding sites per aggregate
a group of pathogens will be clumped up due to the IgM as the pathogens binds onto the molecule and become one form
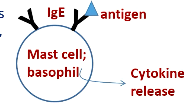
IgE (.2%): found on surface of mast cells & basophils; causes release of histamine, other chemicals by these cells in presence of antigen. Can attract complement, phagocytic cells
This molecule is sitting on these cells and is what allows them to interact with antigens. These cells are responsible for hypersensitivity responses, so allergic reactions, runny nose, watery eyes, ect.
Humor immune response to a microbe is a composite of responses to different epitopes by thousands of B cells; most effective against extracellular pathogens
B cells produce antibodies. Antibodies are incapable of going inside of a cell, thus making them more effective for extracellular pathogens
B cells possess surface immunoglobulins that bind to their specific epitope → B cells become activated
B cells usually require T helper cells (Th) that interact with each other
Called T dependent antigens
Typically for smaller antigens
The most common response involving B cells
Th cells bind antigen via MHC class II receptors on B cells
B cells typically need a T cell to help activate them
The key to the B cell response is clonal selection: proliferation of B cells that respond to a specific antigens
Different B cells present different antibody receptors and will respond to different antigens
When a B cell contacts its cognate antigen, it is stimulated to proliferate and differentiate into plasma cells (secrete antibodies) and memory cells.
When a B cell comes into contact with its matching antigen. it is stimulated or activated (usually with the help of a T cell) to clone itself or multiply. When these B cells multiply, they all recognize that same antigen but they’re then differentiated into plasma cells or memory cells
Plasma cells secrete the antibodies that will help fight off the pathogens but memory cells don’t secrete antibodies but instead stay in your body for a long time and remember that same antigen which allow for your immune system to respond and release antibodies much quicker than before.
Plasma cell antibodies last around 2 months
a clone population of plasma cells only match to one epitope, not multiple
Detecting Invaders: When a pathogen (like a virus or bacteria) enters the body, B cells help recognize these foreign invaders. Each B cell has unique receptors that can bind to specific parts of a pathogen, like a lock and key.
Activation and Division: When a B cell binds to its matching pathogen, it gets activated. This usually requires help from another immune cell called a T helper cell, which gives a signal for the B cell to start working. Once activated, the B cell multiplies to make many copies of itself.
Making Antibodies: The activated B cells turn into plasma cells, which act as antibody factories. These plasma cells produce tons of antibodies—proteins that specifically bind to the pathogen and mark it for destruction.
Neutralizing the Threat: Antibodies either neutralize the pathogen directly by binding to it (preventing it from infecting cells) or flag it for other immune cells to attack and destroy.
Memory B Cells: Some B cells don’t turn into plasma cells but instead become memory B cells. These cells "remember" the pathogen, so if it invades again, they can respond faster and more effectively, providing long-lasting immunity.
B cells sometimes internalizes a pathogen meaning when the antigen binds onto the B cell, the B cell takes a part of that pathogen and eats it. That pathogen is then broken down inside the B cell and those pieces are presented through MHC class II on its surface which allow the T helper cells to recognize it and activate the B cell to make antibodies. This process is more common in T dependent antigens.
T-independent antigen - B cells do not require Th cells for activation
Usually used for larger antigens
B cells can be activated on their own when encountering a large antigen
Same process occurs as T dependent antigen process, just without the need for a T helper cell to activate a B cell.
Antibody Responses
Primary antibody response
Following infection or vaccination; antibodies appear in serum after several days
During lag period, B cells that bind antigen differentiate into:
Antibody-producing plasma cells (first IgM → IgG)
Memory B cells
Secondary response
Via a second exposure to pathogen or booster dose
Due to memory B cells;
A much bigger response, with mostly IgG
Basis for immunization
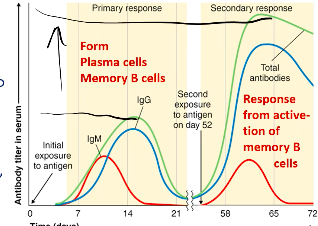
Less time lag and more antibodies produced in the second response
Protective Mechanisms of Binding Antibodies to Antigens:
Agglutination - seen with IgM, clumping up
reduces number of infectious units to be dealt with
Opsonization - enhances phagocytosis
Coating antigen with antibody enhances phagocytosis
Neutralization - seen with IgA antibodies, prevents adherence of viruses and bacteria
Blocks adhesion of bacteria and viruses to mucosa & blocks attachment of toxin
Activation of Complement
Causes inflammation and cell lysis
Antibody-dependent cell-mediated cytotoxicity (ADCC)
in response to large pathogens like parasites or large protozoans
Collective response that involves antibodies and different cell types that bind onto the Fc portion of the antibodies that are bound onto the large pathogen
brings together different cells and that binding brings about a release a collection of different chemicals from these cells
Cell-mediated immunity involves T cells; they recognize antigens that are presented to them on the surface of cells infected with intracellular pathogens.
T cytotoxic cells (Tc):
Differentiate into cytotoxic T lymphocytes (CTLs); target self-cells altered by infection with pathogen (virus & bacteria) - also target cancer cells
Recognize endogenous antigens combined with MHC class I molecules via CTL CD8+ co-receptor
Kill target cells via perforin proteins and induction of apoptosis by introduction of granzymes in to target cells.
Attacks infected cells directly
An infected cell will present antigen from pathogen using MHC class I molecules. The Tc cells will recognize that it’s infected and release perforin proteins to lyse the cell or activate cell death in the cell.
T helper (Th) - recognize antigens presented by antigen presenting cells (APCs), specifically dendritic cells & macrophages
Via their CD4+ co-receptors, Th cells bind antigen combined with MHC class II molecules on the APCs.
Activation of Th cells causes release of various cytokines
Th1 cells - cytokines activate macrophages, complement, promote inflammation & opsonization, & differentiation of CTLs.
When macrophages are activated, you increase the number of pseudopod folds which increases the ability for the cells to phagocytize material
Th2 cells - cytokines mainly for antibody production by B cells
T dependent antigen process
T helper cells involve macrophages, dendritic cells, and B cells
Classes of Adaptive Immunity:
Naturally acquired →
Active - antigens enter the body naturally; body induces antibodies
Passive - Antibodies pass from mother to fetus via placenta or infant
Artificially acquired →
Active - antigens are introduced in vaccines; body produces antibodies
Passive - performed antibodies in immune serum are introduced by injection