Wk 2B - Male and Female Reproductive System
Reproductive Development
Intrauterine Development
The sex of an individual is determined at the moment of conception by the chromosomes information supplied by the ovum and sperm
Week 5
formation of Mesonephric and Paramesonephric ducts
Week 7or 8
Males – Mesonephric ducts develops and give rise to epididymis, vas deferens, seminal vesicles
begins formation of testosterone and develops into male reproductive organs
Week 10
If testosterone is not present
Females – Paramesonephric ducts becomes dominant and develop into female reproductive organs
ovaries form
cells that will develop into eggs are already present (Oocytes)
Week 12
External genitals begins to develop
Males – penile tissue elongated
Females – uterus, labia minora and labia majora form
Pubertal Development
is the stage of life at which a person becomes capable of sexual reproduction
Secondary sex characteristics develop during puberty
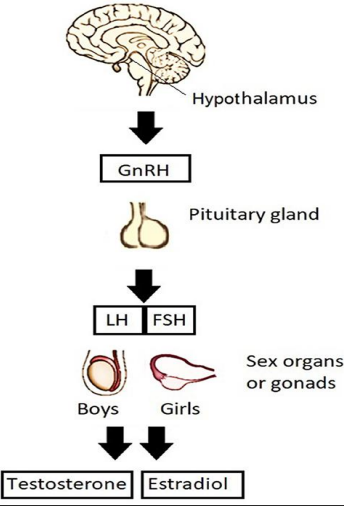
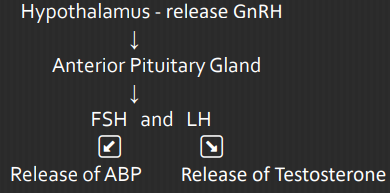
FSH and LH Function:
Initiate the production of androgen and estrogen
Initiate secondary sex characteristics
Production of eggs and influence menstrual cycles
Girls – age 9 to 12 years Hormones
Estrogen (Estrone E1, Estradiol E2, Estriol E3)
Boys – age 12 to 14 years Hormones:
Androgen (Testosterone)
Estrogen Function:
Development of the uterus, fallopian tubes, vagina
Female fat distribution
Hair patterns
Breast development (Thelarche) – starts 1-2 years before menstruation.
Secondary sex characteristics – are physical characteristics developing at puberty which distinguishes between sexes
Secondary Sex Characteristics
Girls
Growth spurt
Increase in transverse diameter of pelvis
Breast development (Thelarche)
Growth of pubic hair and axillary hair (Adrenarche)
Vaginal secretion
Onset of menstruation (Menarche 12.4 y/o)
Menarche - first menstrual period
Average Age – 12.4 years of age
Average Range – 9-17 years old
Delayed Menstruation Causes:
- Stress
- Extreme exercises
- Low body weight
- Polycystic ovary syndrome (PCOS)
Boys
Increase in weight
Growth of testes
Growth of face, axillary, and pubic hair
Voice changes
Penile growth
Increase in height
Spermatogenesis (production of sperm)
Spermatozoa produced in a cyclic pattern, produced in a continuous process.
Testosterone – primary androgenic hormone
Androgen Hormones are responsible for
1. Muscular Development
2. Physical Growth
3. Increase in Sebaceous gland secretions
Female Reproductive System
Gynecology - is the study of female reproductive organ
External Structures
Mons Veneris
a pad of adipose tissue, located over the symphysis pubis
Covered by a triangle of coarse curly hair that protects the pubic bone from trauma
Labia Mjora
are two folds of tissue, position lateral to the labia minora
Cover and protects the external genitalia, urethra, and vagina
Labia Minora
posterior to mons veneris spread two hairless folds of connective tissue.
Protect the clitoris, urinary and vaginal orifice
Clitoris
is a small rounded organ of erectile tissue (approximately 1-2 cm.)
serve as center of sexual arousal and orgasm
Vestibule
the flattened, smooth surface inside the labia minora that encloses the vaginal and urethral opening
Bartholin’s Gland
(Vulvovaginal Glands) located just lateral to the vaginal opening
Secretes mucus to lubricate the vagina during coitus.
Fourchette
is the ridge of tissue joining the labia minora and majora,
Serve as site of Episiotomy during childbirth
Hymen
a tough elastic semicircle tissue that covers the opening of the vagina
Hematocolpometra – imperforate hymen
Skene’s Gland
(paraurethral glands) lateral to the urinary meatus
secretes mucous which serve as lubricants during sexual intercourse
Perineum
muscular structure in between the vagina and anus. ▪ Support the genitourinary system
Internal Structures
Ovaries
approximately 4 cm. long by 2 cm. in diameter, 1.5 cm. thick and shape of almonds
secretes hormones
Functions:
Produce estrogen and progesterone
Produce mature and discharge egg cells
Initiate and regulates menstrual cycles
3 Principal Division of Ovaries
Protective layer of surface epithelium
Cortex – where the immature oocytes (Primordial) mature into ova
Central medulla – contains nerves, blood vessels, lymphatic tissue and smooth muscle tissue
Fallopian Tubes
provides a place for fertilization of the ovum by sperm. (approximately 10 cm. long)
Parts
Interstitial
is the part of the tube that lies within the uterine wall and site for ectopic pregnancy
Isthmus
is the distal portion of the tube that is cut or sealed in a tubal ligation or tubal sterilization procedure
Ampulla
is the third and the longest portion of the tube.
It is the portion that fertilization of ovum occurs.
Infundibular
distal segment of the tube. (2 cm. long and funnel shaped)
covered by fimbria (small hairs) that help to guide ovum into the fallopian tube
Uterus
Weight
Non-pregnant - 60 grams
Pregnant - 1000 grams
Size
5-7 cm. long
5 cm. wide
2.5 cm. thick (non-pregnant)
Function
Receive the ovum from the fallopian tube.
Provide a place for implantation and nourishment.
Furnish protection to a growing fetus.
Provide a place for menstruation, pregnancy, and labor.
3 Divisions of Uterus
Fundus
is the body of the uterus, uppermost part and forms the bulk of the organ.
During pregnancy, it is the portion of the structure that expands to contain the growing fetus.
Isthmus of the Uterus
is a short segment between the body and the cervix. In the nonpregnant uterus, it is only 1 to 2 mm in length.
It is the portion of the uterus that is cut when a fetus is born by a cesarean birth
Breast
are located anterior to the pectoral muscle and breast tissue extend into the axilla.
remain in halted stage of development until a rise in estrogen at puberty causes them to increase in size
Parts of Breast
Milk Glands (Lobules)
with approximately 20 lobes that produced milk by acinar cells and deliver it to the nipple via a lactiferous duct
Nipple
composed of smooth muscle capable of erection on manual or sucking stimulation
has 20 small openings through which milk is secrete
Areola
a darkly pigmented out to about 4 cm., the area appears rough on the surface and contains many sebaceous glands (Montgomery tubercles)
Ampulla
located just posterior to the nipple serves as reservoir for milk before breastfeeding
Cervix
is the lowest portion of the uterus.
Internal os – opening of the canal at the junction of the cervix into the uterus
External os – distal opening to the vagina (Estimating the level of the fetus in the birth canal)
Layers of Uterus
Endometrium
inner layers and important for menstrual function.
It becomes thick each month under the influence of estrogen and progesterone capable of supporting a pregnancy
If pregnancy does not occur, this is the layer that is shed as the menstrual flow
Myometrium
composed of smooth muscle that offers extreme strength to the organ
Function:
It prevent regurgitation of menstrual blood into the tubes
It holds the internal cervical as closed during pregnancy to prevent a preterm birth
Perimetrium
outermost layer, add further strength and support to the organ
Male Reproductive System
Andrology - is the study of the male reproductive system
External Structures
Scrotum
is a rugated, skin-covered, muscular pouch hanging below the penis containing the testes.
Support the testes and help regulate the temperature of sperm.
Testes
are two ovoid glands, that lie in the scrotum (2-3 cm. wide)
Produced and store sperm ▪ Produced hormones
composed of lobules containing interstitial cells
Lobules
Seminiferous tubules – produce spermatozoa
Leydig’s cells – responsible for the production of testosterone
Penis
is composed of three cylindrical masses of erectile tissue in the penis shaft
Corpus Cavernosa
two lateral columns of erectile tissue
Corpus Spongiosum
encases the urethra, located on the underside of the penis
Ischiocavernosus muscle
under stimulation, venous and arterial blood in erectile tissue leads to distention and erection of the penis
Internal Structures
Epididymis
seminiferous tubules of each testes
20 ft. long, takes 12-20 days for the sperm to travel the length of epididymis, 64 days to reach maturity
Serve as reservoir for sperm storage and maturation.
Conducting sperm from the tubule to the vas deferens.
A total of 65 - 75 days for the sperm to reach maturity
Aspermia – absence of sperm
Oligospermia – fewer than 20 million sperm per millimeter
Vas deferens (Ductus Deferens)
Hallow tube surrounded by arteries and veins
carries sperm from epididymis through the inguinal canal into the abdominal cavity.
Seminal vesicles
are pouches that lie along the bladder
Secretes viscous alkaline liquid portion of the semen.
Increase sperm motility
Prostate gland
a chest-nut size gland that lies below the bladder
Secretes a thin, alkaline fluid that protects sperm from being immobilized.
Reduces the acidity of the vagina
Benign Prostatic Hypertrophy
enlargement of the prostate gland
swelling interferes with both urination and fertility
Bulbourethral Glands
glands lies beside the prostate gland
Secretes an alkaline fluid to help ensure the safe passage of spermatozoa
Urethra
It is 8 inches (18-20 cm.) long
vessel of transport of urine and semen
Ejaculatory Ducts
two ejaculatory ducts pass through the prostate gland and join the seminal vesicles to the urethra.
Spermatozoa
ARE MALE SEX CELLS THAT CARRY A MAN’S GENETIC MATERIAL.
Sperm Count
33 - 46 million sperm per ml. of seminal fluid
50 million per ejaculation
50% of sperm are motile
30% are normal in shape and form
During ejaculation, semen receives contributions of fluid from
Prostate gland – 60%
Seminal vesicle - 30%
Epididymis - 5%
Bulbourethral glands – 5%
Spermatogenesis – the formation and development of sperm.
Testosterone - responsible for the development of the secondary male characteristics