Microbiology week 3
What is a pathogen?
A microorganism that can cause damage/ disease
Some organisms may have specific mechanisms that allow them to cause damage, known as virulence factors
What is a virulence factor?
A virulence factor is something that helps the organisms cause the damage/ disease to the host cell
Adhesins- Help the organism adhere to host epithelial cells
Evasins & Impedins- Help the organism evade the host immune system
Invasins-Help the organism invade host tissues
Toxins- Help the organism cause damage direct to the host tissues
Host defenses
Exterior defenses- most of the infectious agents encountered by an individua; are prevented from entering the body by a variety of biochemical and physical barriers. The body tolerates a variety of commensal organism which compete effectively against pathogens.
Respiratory tract
Nose- Specialised hairs vibrissae filter large particles
Abrupt airflow changes due to the structure of the nasopharynx
Cough reflex
Respiratory epithelium from nose to terminal bronchioles are covered with beating cilia, covered in mucus
Alveoli containing IgA, complement components and alveolar macrophages.
Different organisms found in the upper respiratory tract
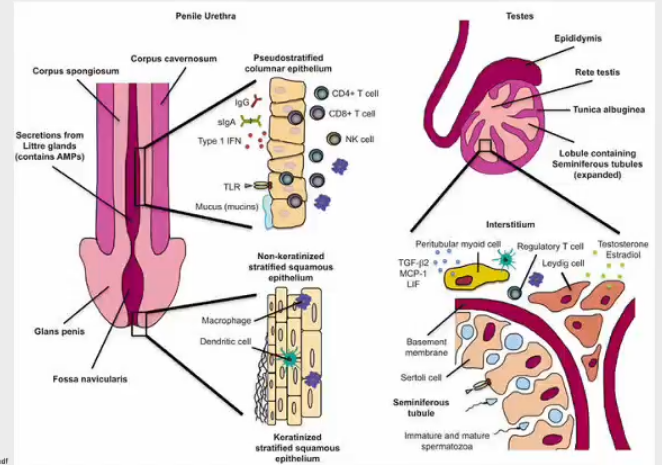
Urinary tract
Mucosal
Urothelial secretion of cytokines and chemokines
Mucopolysaccharide lining
Mucosal IgA
Men- prostatic secretions contain bactericidal zinc and urethra is longer
Urine
Acidic pH
High urine osmolality
Urinary inhibitor of adherence
Competitive inhibitor of attachment to urothelial cells
Flushing action of urine flow
GI tract
Mouth
Flow of liquids
Saliva - lysozyme
Normal bacterial flora
Oesophagus
Flow of liquids
Peristalsis
Stomach
Acid pH
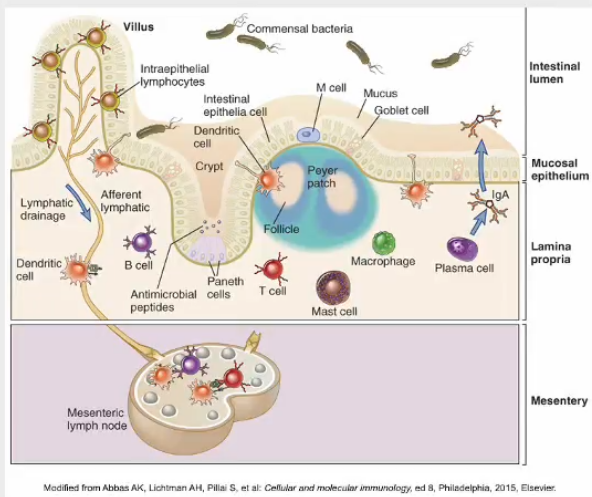
Small intestine
Flow of gut contents
Peristalsis
Mucus/ bile
Secretory IgA
Lymphoid tissue - Peyer’s patches
Shedding and replacement of epithelium
Normal flora
Large intestine
Normal flora
Peristalsis
Shedding and replication of epithelium
Mucus
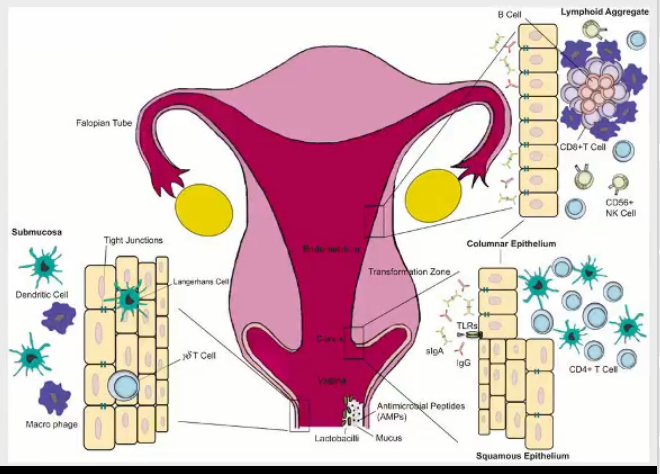
Vaginal flora- protects female reproductive tract
How do microorganism invade the body
1st line of defence- innate immune system
Skin
Mucosa membrane
2nd line
phagocytes
complements
3rd line- adaptive
lymphocytes
antibodies
Memory cells
How do they invade the 1st line of defence
Failures in the system- breaks to the skin, lack of normal flora
Number of pathogens are high= overwhelming
Resistance to pH changes
Adhesion despite flow of liquids
How do they invade the 2nd line of defence
Avoidance- physical barrier
Cryptococcus neoformans- thick capsule
Granuloma stops immune system detecting foreign body
Interference
CMV has a homologue of UL18- inhibits cytokine production
Cytokine- stimulate the immune response
How do they invade the 3rd line of defence
Concealment- the organism surrounds itself with host cells- stops antigens being detected, conceal their receptor antigens
Chlamydia- exist within the host cell- mimic host antigens- immune system won’t identify chlamydia cells
Antigenic variation- changes the shape of surface antigens the pathogen induces a series of innate responses in place of the host developing an effective adaptive responses
Influenza virus- changes surface antigens
Immunosuppression- organisms can supress the immune system
less monocytes - impaired lymph proliferation
Trypanosomes and Leishmaniasis- organism can change antigen on their surface
Defects in host defence mechanism
two types of immune deficiency states affect the host’s ability to fight infection
Primary immune deficiency- genetic origin. most are recognised during infancy
Acquired immune deficiency (secondary)- caused by another disease such as cancer, HIV infection or chronic disease. or exposure to a drug that is toxic to the immune system
Immune-mediated damage
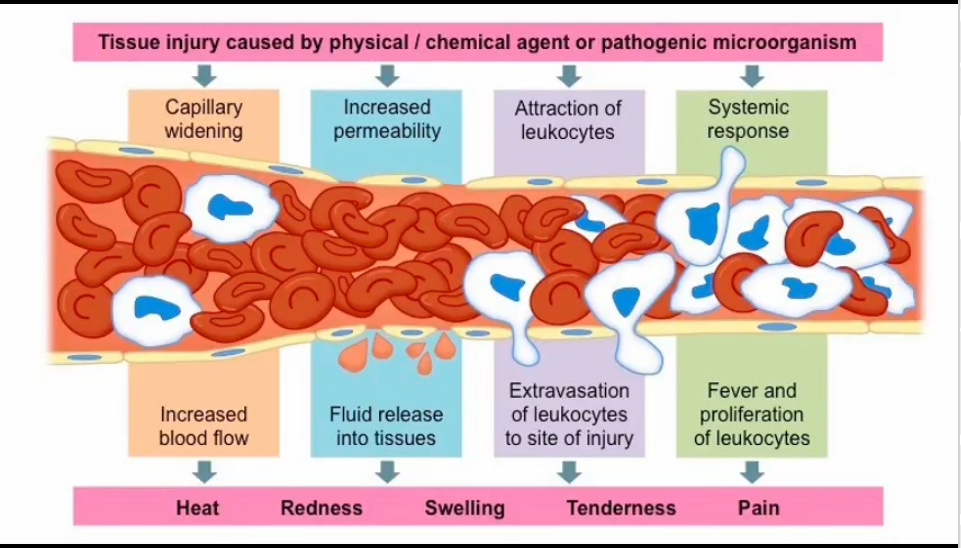
Damage/disease can be caused by the pathogen but can also be caused by the immune response.
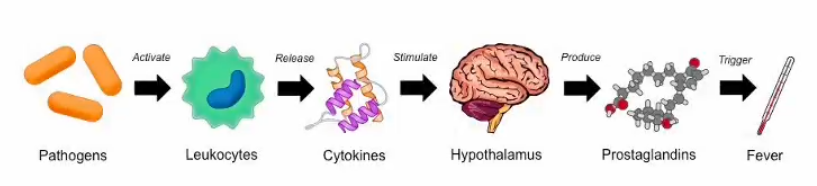
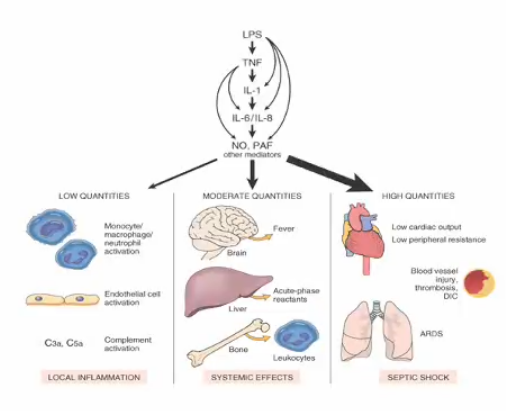
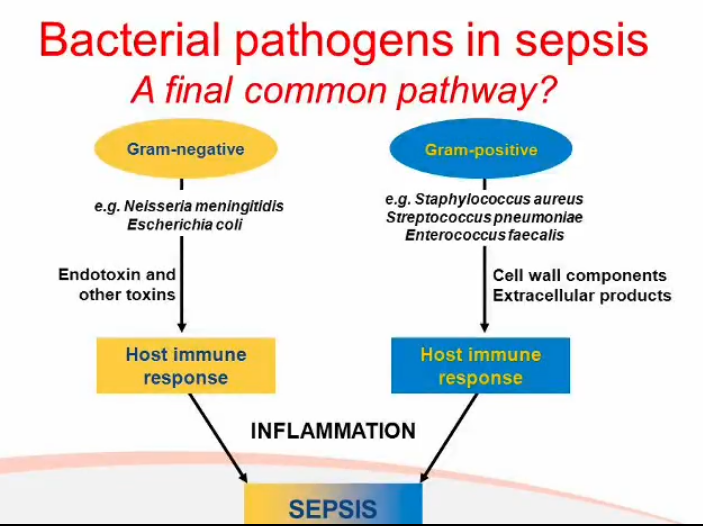
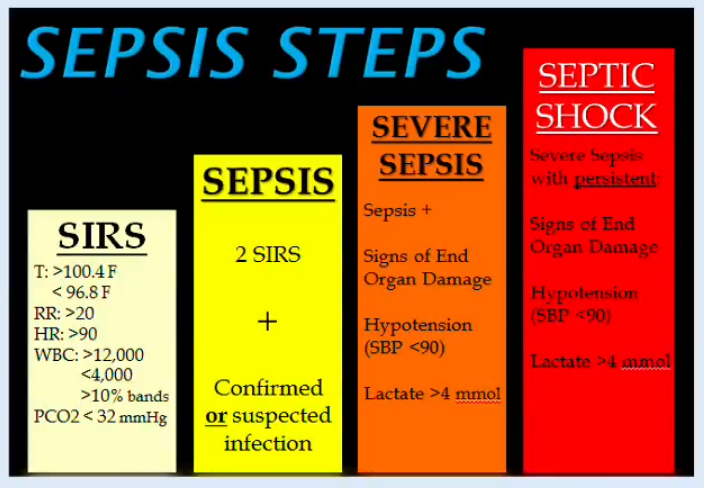
Excessive stimulation of the innate immune system can lead to dangerous or potentially fatal symptoms, a microbial-induced example of this is sepsis
Sepsis and septic shock
when some gram-negative bacterial lyse, a component of their cell wall- lipopolysaccharide (LPS) cause excessive cytokine secretion by macrophages
S- slurred speech or confusion
E-extreme shivering or muscle pain
P-passing no urine (in a day)
S-severe breathlessness
I-it feels like you’re going to die
S-skin mottled or discoloured
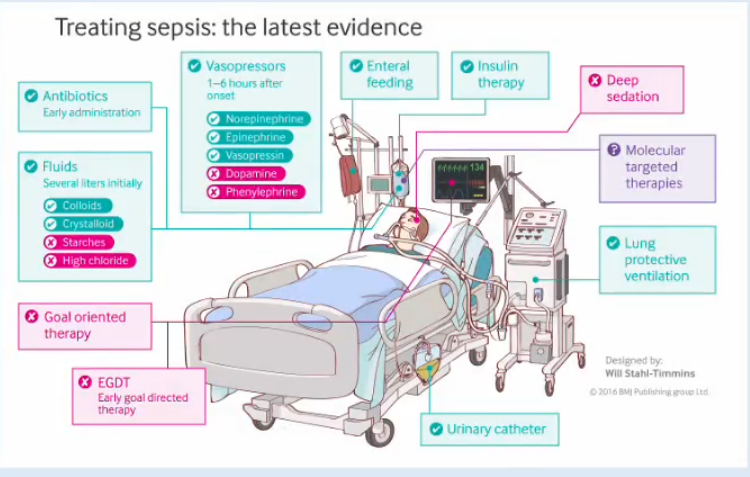
Treatment can bypass host defenses
Influenza virus
Antigenic variation
Principle is by constantly changing the shape of surface antigens the pathogen induces a series of innate responses in place of the host developing an effective adaptive response.
Hemagglutinin (HA)
Neuraminidase (NA)
Eight ribonucleotide segments each contain viral RNA surrounded by nucleoprotein and associated with RNA transcriptase
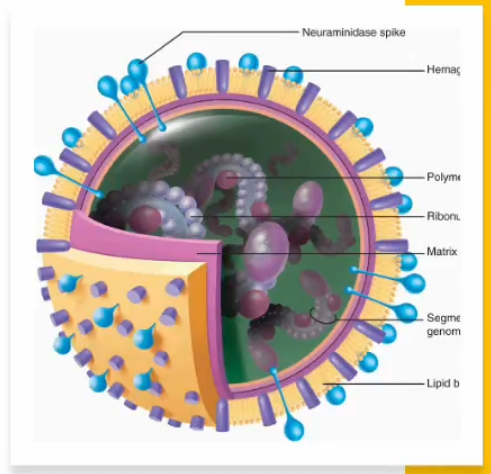
Antigen variation
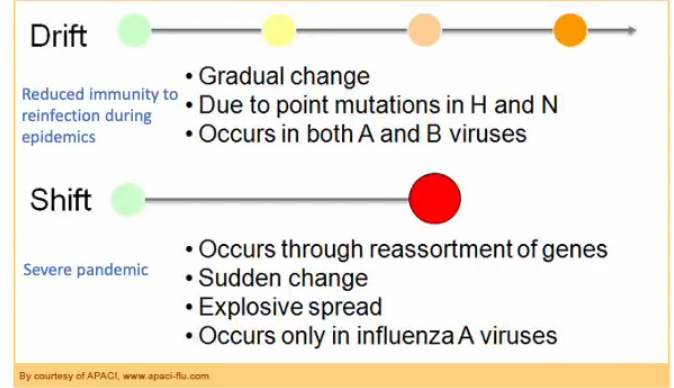
Two types of influenza virus, designated type A and type B- public health concern
Can not be differentiated by symptoms- differentiated in lab only
Many subtypes of flu A with different variants of HA and NA, most of these subtypes only circulate in birds
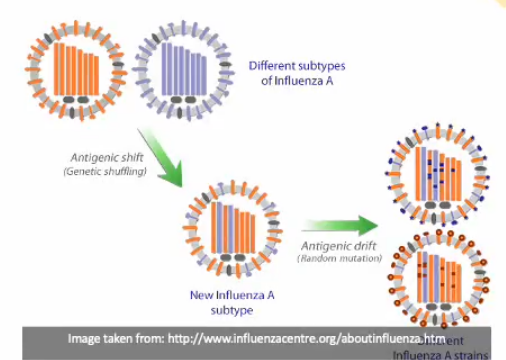
Occasionally a new subtype of flu A virus emerges that has a HA to which humans haven’t been exposed to previously - ANTIGENIC SHIFT
HA and NA of type A and type B viruses continually change by mutation to produce new strains- ANTIGENIC DRIFT