Week 15: High Risk Newborns and Associated Care
High Risk Newborn Overview
Location: Topic four in the OB learning modules
Introduction to High Risk Newborns
Topics include assessment and management of newborns with complications.
Pediatric nurses often encounter high-risk patients after stabilization.
Emphasis on parental emotional support and education regarding complications and care needs.
Common Types of Newborn Complications
Describe the assessment of risk factors and collaborative care approaches for newborns.
Importance of identifying complications early and intervening appropriately.
Emotional Aspects of High-Risk Infants
Parents may experience grief and difficulty bonding with infants that are not as expected (e.g., due to prematurity or anomalies).
Support includes education, emotional support, and allowing parental bonding time.
Definition of High-Risk Neonate
A neonate is classified as high risk if there is an increased chance of dying during or shortly after birth.
Advances in medicine have improved survival rates and outcomes for high-risk infants.
General trends in how families cope with the unexpected challenges of caring for high-risk infants.
Common Complications and Anomalies
Types of Anomalies:
Congenital defects
Cognitive delays
Maternal Infections and their adverse impact on fetal development.
Importance of Early Interventions to prevent or treat complications.
Assessment of Vital Functions
Follow ABCs in care:
A: Ensure oxygenation and ventilation
B: Thermoregulation
C: Nutrition and fluid/electrolyte balance
Prevention and control of infection are paramount.
Encouragement of parental bonding and providing developmental care.
Preterm Delivery
Risk factors:
Preeclampsia
Maternal diseases
Multiple pregnancy
Adolescent pregnancy
Lack of prenatal care
Substance use/smoking
Previous preterm delivery
Cervical incompetence
PROM (infection)
Placenta previa
Maternal HTN
Symptoms: temperature instability, inability to excrete urine, hypoglycemia, hyperbilirubinemia, and increased risk of infection.
Treatment: the top priority is supporting the cardiac and respiratory systems as needed
Daily weight
Maintain body temperature
3-5 days without apnea or bradycardia events
Complications: RDS, BPD, aspiration, apnea, intraventricular hemorrhage, retinopathy of prematurity (common, abnormal bleeding in the retina, which in turn affects oxygenation), PDA, or necrotizing enterocolitis. (NEC; stop feeding, place NGT to decompress, and measure abdominal girth q8 and remove necrosis, may require temporary ostomy).
Nursing Management: rapid/perform resuscitative measures and respiratory support as needed.
Preterm infants born before 34 weeks are not coordinated enough to maintain suck, swallow, and breathe necessary for oral feeds.
Nonnutritive sucks: Use of a pacifier during gavage feedings eases the transition to oral feeding later.
Newborn Infection, Sepsis
Infection can be contracted before, during, or after delivery.
Culture, nasal swab, and lumbar puncture.
Organisms: S. aureus, E. coli, H. influenza, S. epidermis, GBS.
GBS: on IV antibiotics for 21 days in the hospital.
Risk Factors:
PROM
TORCH infections
Preter
Low birth weight
Prolonged labor
Meconium aspiration
Maternal UTI & STIs
HIV
Expected Findings: Temperature instability, poor feeding, hypo/hyperglycemia, abd. distention, color change, N/V, lathergy, abnormal BI, drainage from eye, umbilical or stump.
Assessment at 24 Hours of Life
Difficulty establishing respirations
Irritability
Lethargy
Seizure activity
Tremulousness
Opisthotonos (hyperextension)
Poor sucking reflex
Abdominal distention
Flat philtrum (middle upper lip)
Wide-set eyes
Neonatal Substance Withdrawal
Maternal substance use (e.g., alcohol, drugs) can lead to Neonatal Abstinence Syndrome (NAS):
Involves withdrawal symptoms in newborns, leading to neurobehavioral and physical changes.
Dependence on the type of substance used, dosage, and timing of exposure.
Substances include (and are not limited to): Opioids, Barbiturates, Benzodiazepines, SSRIs, caffeine, and nicotine.
Intreauterine drug expose can cause neurobehavioral changes, anomalies, and evidence of withdrawal in the neonate.
Diagnostics: Obtain specimends of urine and meconium.
Meconium can detect drug use over a 20-week period and is currently the best method for detecting drug exposure.
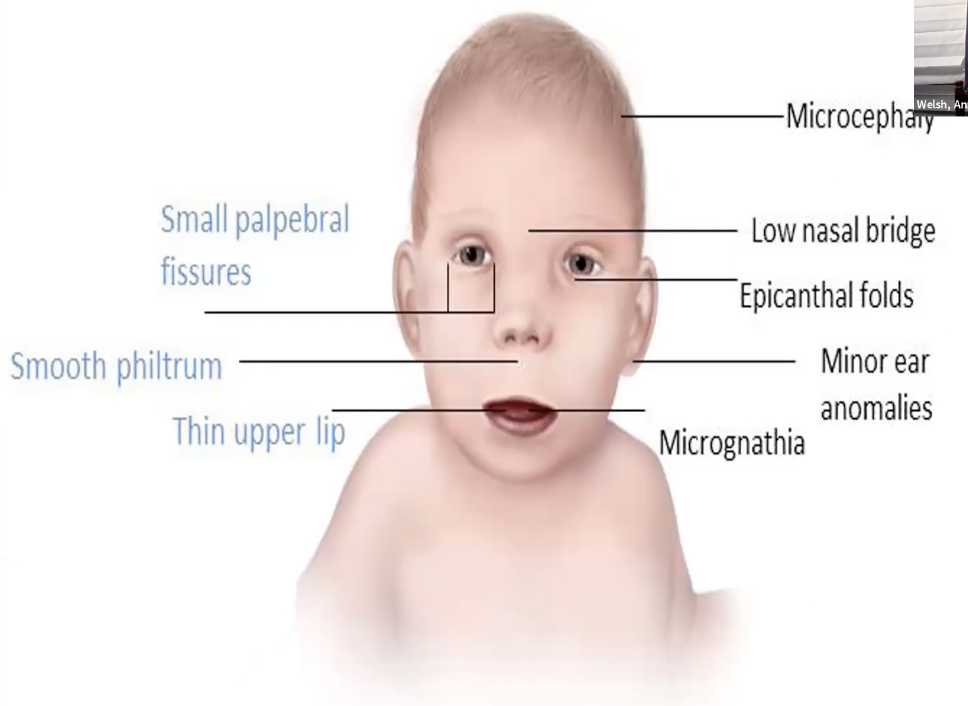
Fetal Alcohol Syndrome (FAS)
Caused by chronic or periodic alcohol intake during pregnancy.
NO alcohol consumption is safe during pregnancy.
Characteristics include:
High-pitched cry
Difficulty in soothing infants
Growth restriction
Craniofacial structure anomalies
CNS dysfunction
Long-term risks: Congenital defects (ADHD, poor speech, low IQ), neurological impairments.
CNS Problems: Mental retardation, microcephaly, poor coordination, decreased muscle tone, small brain, behavioral abnormalities, irritability, tremors, and poor feeding.
Alcohol is for tetragenic substance; therefore, the daily intake of alcohol can lead to this.
It can reduce the amount of oxygen to the baby and cause developmental impairments.
Diagnosis: Identify and document all 3 facial abnormalities, growth deficits, and CNS abnormalities, including structural/functional abnormalities.
Complications:
Cardiac murmurs
Limited joint movement
Finger and toe deformities
Single palmar creases
Kidney defects
Labial hypoplasia
Difficulty with memory, attention, and problem-solving
Learning disabilities
Problems with mental health
Difficulties with social interactions
Treatment is supportive
Prevention
Respiratory problems:
Place the neonate on a cardiac monitor
Assess breath sounds frequently- alert for respiratory distress
Nutrition
Emphasis on weight gain
Assess feeding behaviors
Encourage feeds and bonding
Elevate the head during and after feeding
Signs and Symptoms of NAS
Symptoms observed 24-72 hours post-birth include:
CNS hypersensitivity: Shrill/High-pitched cry, hyperactivity, seizures
Autonomic dysfunction: Temperature instability (typically higher), respiratory distress
Poor feeding behaviors, GI disturbances (loose stool)
Increased Risks
Pregnant Women who use addictive drugs are at higher risk for:
Abruptio placentae
Spontaneous abortion
Preterm labor
Precipitous labor
Mental health issues
Neonatal Complications may include:
Urogenital malformations
Cerebrovascular complications
Low birth weight
Decreased head circumference
Respiratory complications
Sezuires
Failure to thrive
Death
Monitoring and Assessment Tools
Use of the Finnegan Scoring System to assess the severity of withdrawal every four hours (the higher the score, the higher need for medication).
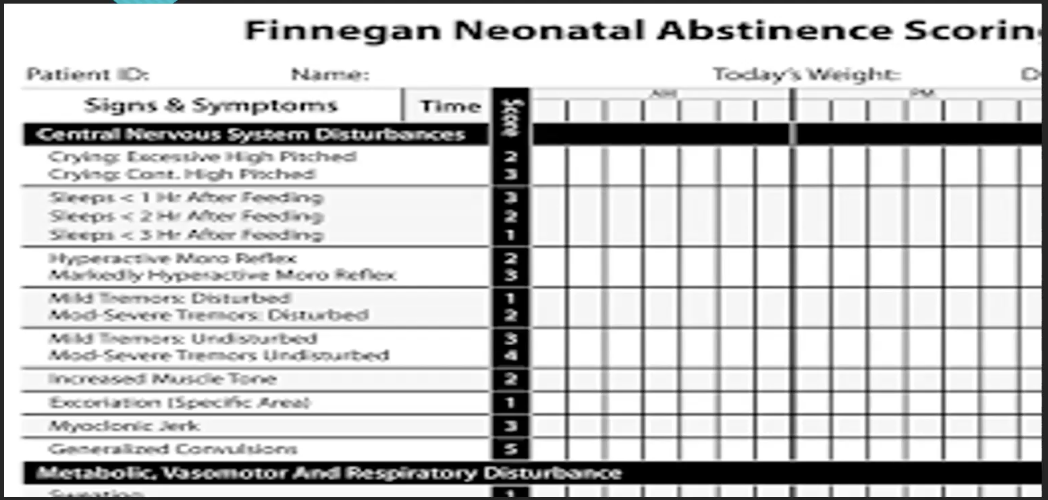
Constant monitoring for signs of distress, including seizures, weight loss, and feeding difficulties.
Detailed scoring will guide medication administration and weaning strategies.
Assessment of Withdraw
W: Wakefulness
I: Irritability
T: Temperature variations with tachycardia, tremors (3 Ts)
H: Hyperactivity with high-pitched cry, hyperreflexia, hypertonia
D: Diarrhea, diaphoresis, disorganized sucking reflex
R: Respiratory distress
A: Apneic events, autonomic dysfunction
W: Weight loss/failure to gain weight
A: Alkalosis
L: Lacrimation (flow of tears)

Treatment of NAS
Inital treatment is supportive care.
Symptomatic treatment in a controlled environment:
Quiet, low-stimulus settings, pacifiers, swaddling.
Medication options include methadone or morphine+phenobarbital, with careful tapering.
Give low lactose formula due to sensitivity.
Provide respiratory care as needed.
Supporting gradual withdrawal while ensuring proper nutrition and hydration.
Complications of Neonatal Withdrawal
Risks associated with maternal drug use include:
Low birth weight
Increased rates of sudden infant death syndrome (SIDS)
Neurobehavioral issues
Marijuana use may cause fetal growth retardation, high-pitched cry, low birth weight, and more.
Findings that Indicate Drug Testing Should be Performed
Maternal:
Lack of prenatal care
Previous unexplained fetal demise
Precipitous labor
Altered nutrition
Abruptio placenta
HTN episodes
Severe mood swings
Recurrent spontaneous abortions
Fetal:
Preterm labor
Cardiac defects
Unexplained IUGR
Neurobehavioral abnormalities
Urogential anomalies
Hypoglycemia in Neonates
Definition: Blood glucose < 30 mg/dL (normal is 30-60 mg/dL) within the first three days for term newborns.
Possible causes include a lack of adequate glucose production following umbilical cord clamping, increased physiological stressors.
Assessment/Symptoms: Jitteriness, weak cry, irritability, lethargy, and respiratory irregularities.
Management includes:
Regular heel-stick glucose checks
Oral feeding for asymptomatic newborns, IV dextrose for symptomatic ones.
Oral/gavage/parenteral feeding to increase glucose.
Maintain skin-to-skin for thermoregulation.
Respiratory Distress Syndrome (RDS)
Risk factors:
Primarily seen in preterm infants due to immature lung development.
Carries long-term respiratory and neurologic complications.
Characterized by inadequate surfactant production.
Surfactant: A substance composed of lipids and proteins that reduces surface tension in the alveoli, helping to prevent their collapse during exhalation and allowing for easier breathing.
Maternal diabetes and stress during delivery that produce acidosis in the neonate.
Expected findings and clinical manifestations:**
Expiratory grunting, retractions, labored breathing, and cyanosis.
RDS can lead to atelectasis, increased work of breathing, respiratory acidosis, and hypoxemia.
At risk of developing asthma, pneumothorax, and intraventricular hemorrhage.
Treatment for RDS
Supportive care includes maintaining body temperature, oxygen supplementation, and potentially mechanical ventilation.
Some are on BiPAP or CPAP.
Parenteral feedings (gavage/oral feedings are not recommended due to high oxygenation needs).
Administration of surfactant should occur via an endotracheal tube, with careful monitoring thereafter.
Assess endotracheal tube placement.
Meconium Aspiration Syndrome
It occurs when meconium is inhaled during delivery, leading to airway obstruction.
Typically occurs in utero or during the neonate’s first breath.
It damages the Type II cells in the airway and inhibits surfactant production- making breathing difficult.
Symptoms include cyanosis, rapid/labored breathing, and low Apgar scores.
Hyperinflation, hypoxemia, and acidemia can result.
Risk Factors: maternal diabetes, maternal HTN, difficult delivery, fetal distress, intrauterine hypoxia, advanced gestational age (>40 weeks), and poor intrauterine growth.
Testing: Breath sounds will be coarse and crackly. ABG to assess status and chest x-ray for presence.
Management strategies include suctioning the trachea if necessary and supportive respiratory care.
Suction the mouth and nose as soon as the baby is delivered.
Additional treatments include chest physiotherapy, antibiotics, use of a radiant warmer, supplemental oxygen, and mechanical ventilation.
Complications: aspiration pneumonia, bronchopulmonary dysplasia, cerebral palsy, mental retardation, pneumothorax/air leak, seizures, or persistent pulmonary HTN in the neonate (PPHN).
Legal and Ethical Considerations
Ethical implications of care for high-risk infants and their families.
The importance of knowledge about congenital anomalies and management strategies in promoting optimal outcomes across healthcare settings.
Ongoing education and support for families, informed consent in medical decision-making.
Hyperbilirubinemia Analysis
Types of jaundice: Physiologic vs. Pathologic
Physiologic resolves in 7-10 days; pathologic requires further investigation if present within the first 24 hours or persists longer than two weeks (clinical jaundice that occurs past 14 days; vice versa for physiologic).
Jaundice normally appears on the head (sclera/mucus membranes), then progresses down to the thorax, abdomen, and extremities.
Testing: done by direct or indirect bilirubin levels.
Levels that are excessively elevated or vary daily suggest a pathologic process.
Causes: requires patient and family history of blood disorders for incompatibilities.
Treatment options include phototherapy (use eye protection and cover genitalia) and exchange transfusions (albumin assists with binding; IV globin is done for isoimmune hemolytic disease) for severe cases to prevent kernicterus.
Complications:
Acute bilirubin encephalopathy (bilirubin deposited in the brain)
Kernicterus (levels >25 mg/dL, toxicity)
Nursing Management and Follow-Up Care
Continuous education around feeding and eye protection during phototherapy.
Importance of follow-up labs to monitor bilirubin levels post-discharge.
Observe effects of phototherapy.
Bronze discoloration: not a serious complication
Maculopapular skin rash: not a serious complication
Dehydration: poor skin turgor, dry mucous membranes, decreased urinary output.
A newborn may have loose, green stool (containing bile).
Conclusion and Resources
Reinforcement of summary points; additional resources for study such as related videos and recommended readings in the RIPE book and specific chapters.
Encouragement for students to ask questions and engage actively with their instructors before exams.