W10: Non-Accidental Injuries (NAI) - Imaging Through the Lifespan
Non-Accidental Injuries (NAI)
Indications of Possible Abuse
Inconsistent Explanation: The carer's explanation of the injury does not match the injury itself or the child's developmental stage.
Unexplained Injuries: There is no explanation for the injuries or the explanation changes upon repetition. If the child is old enough, their explanation might contradict the carer's.
Delayed Medical Help: The carer delays seeking medical assistance.
Self-Absorption: The carer is more focused on their own needs than the child's.
Frozen Watchfulness: The child exhibits a state of being unresponsive to their surroundings but is clearly aware of them, often expressionless and difficult to engage, despite normal intelligence. This is a marker of child abuse.
Frozen Watchfulness
Definition: A state where a child is unresponsive to their surroundings but remains aware. They are typically expressionless and hard to engage, despite having normal intelligence.
Significance: It is a marker of child abuse.
Injury Patterns
Bruising: Present in approximately 90% of NAI cases.
Bruise Patterns: Suggest the type of abuse.
Normal areas: Bruising over the shin and forehead can be normal.
Suspicious areas: Bruising on the abdomen, face, ears, hands, buttocks, and trunk are not common in normal physical activity.
Multiple Bruises: Clusters of bruises are highly suggestive of NAI.
Bruising in Young Children: Bruising on children under 2 years old should be viewed with suspicion.
Aging of Bruises
Stages:
Red, tender, swollen: 1-2 days
Blue-purple: 1-5 days
Green-yellow: 5-7 days
Yellow-brown: 7-10 days
Cleared: 1-4 weeks
Reliability: The accuracy of bruise aging by color has been challenged and deemed unreliable in court. Systematic reviews support this finding.
Reference: "Can you age bruises accurately in children? A systematic Review." S Maguire, M K Mann, J Sibert, A Kemp. Arch Dis Child 2005; 90:187–189. doi: 10.1136/adc.2003.044073
Skeletal Fractures Linked to NAI
Types of Fractures:
Metaphyseal fractures
Sternum and rib fractures
Vertebral fractures
Fractures of the shoulder (especially scapula, clavicle, and, rarely, acromion)
Digit fractures
Spiral fractures of upper and lower limbs
Skull fractures
Bilateral fractures
Fractures of varying ages
Fracture Patterns
Metaphyseal Fractures:
Description: Corner or bucket handle fractures.
Detection: Can be occult.
Location: Often appear on lower limbs.
Diaphyseal Fractures:
Prevalence: Most common fracture type.
Suspicion: Highly suspicious in non-ambulatory children.
Periosteal Reaction:
Cause: Disturbance of bone histology.
Etiology: Bone growth, fracture, or subperiosteal hemorrhage.
Presentation: Occurs about 1 week post-injury.
Differential Diagnosis: Consider metabolic diseases such as Caffey’s disease, which presents with profuse periosteal reaction.
Caffey’s Disease
Description: A metabolic disease that can cause excessive periosteal reactions.

Other Fracture Patterns
Clavicle Fractures:
Uncommon in NAI.
Cause: Typically result from shaking or a direct blow.
Rib Fractures:
Cause: Compression from squeezing while shaking.
Vertebral Fractures:
Unusual but likely to occur at the thoracolumbar (T/L) junction.
Cause: Shaking.
Reasons for Common Injury Sites
Common Injuries:
Subdural Hematoma (SDH)
Rib Fractures: Posterior and lateral to anterior
Corner Fractures and Bucket-Handle Fractures
Role of Imaging
Objectives:
Demonstrate and date clinically suspected fractures.
Demonstrate and date clinically occult fractures.
NAI Radiographic Skeletal Survey
Basic Series (based on common injury regions):
AP chest x-ray
AP supine abdomen
AP upper limbs (including shoulders)
AP lower limbs (including hips)
Lateral thoracolumbar (T/L) spine
Lateral skull
Additional Projections:
Coned projections of identified fractures, especially at joints
Dorso-palmar (DP) hands and feet if bruising is present
NAI Radiographic Skeletal Survey (Royal Children’s Hospital - Melbourne)
Standard Views:
AP chest x-ray
AP supine abdomen (including pelvis)
AP upper limbs (forearms to humerus)
AP lower limbs (tibia/fibula to femurs)
Lateral cervical/thoracic/lumbar (C/T/L) spine
Lateral skull
Lateral sternum
PA hands
AP feet
Additional Projections (Royal Children’s Hospital - Melbourne)
Specific Views:
Coned PA wrists
Coned AP ankles
Coned AP knees
Oblique ribs
Image Evaluation (Royal Children’s Hospital - Melbourne)
AP Chest:
Visualization: Entire bony thorax.
Bone Detail: Optimum.
Rotation: No rotation of the child.
Density: Sufficient to visualize intervertebral disc spaces.
AP Abdomen and Pelvis:
Coverage: Diaphragm to lesser trochanters.
Limbs:
Alignment: Each long bone must be true AP, including the joint above and below.
Collimation: Adequate collimation is essential.
Number of Projections: Initially, only one projection per region.
Equipment: To be performed on DR equipment.
Markers: All images MUST have markers applied at the time of imaging; electronic markers are not accepted.
Limbs: When imaging entire upper and lower limbs with one exposure, the elbow, wrist, knee, and ankle MUST be in true AP position. Babygrams are generally discouraged.
Reporting: Reports available within 24 hours.
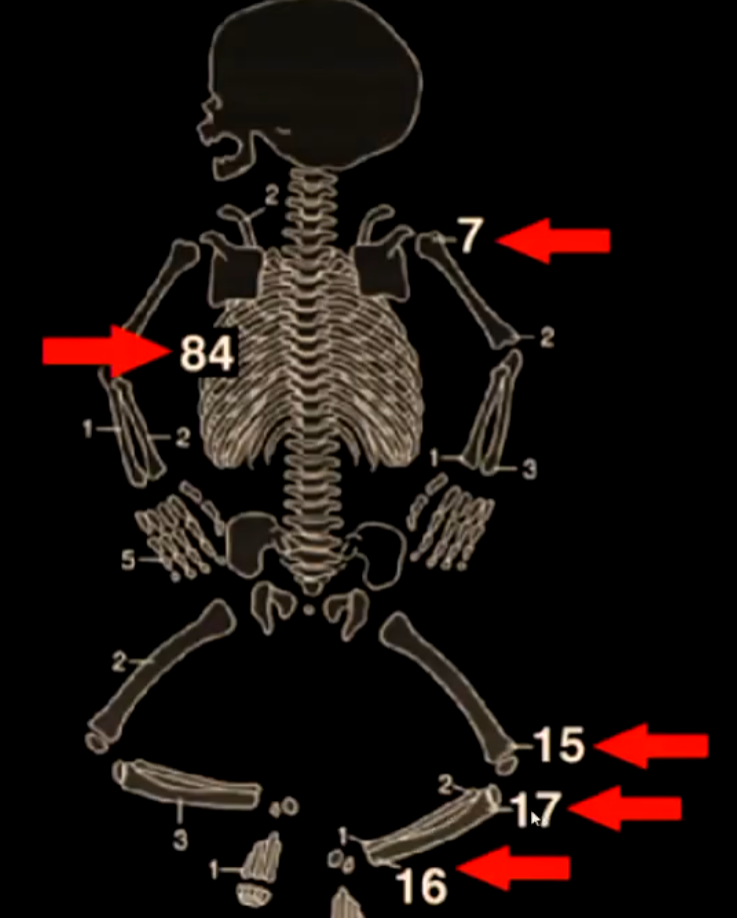
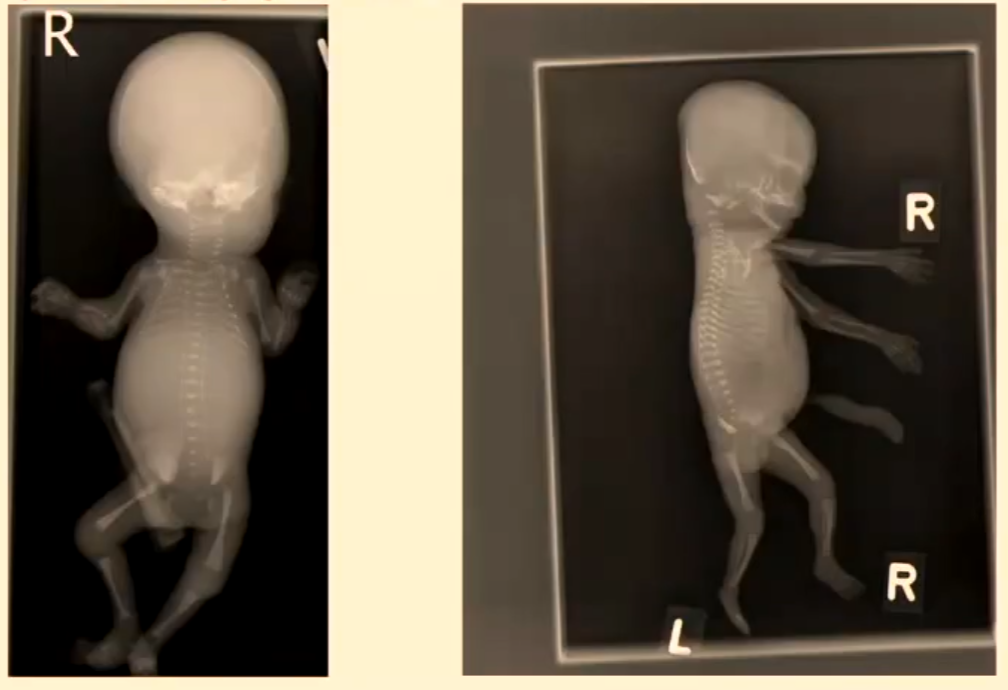
Babygram
Purpose: Performed on certain aborted fetuses to determine skeletal abnormalities.
Note: Babygrams lack the fine detail required for imaging an NAI case; they are not used for NAI diagnosis.
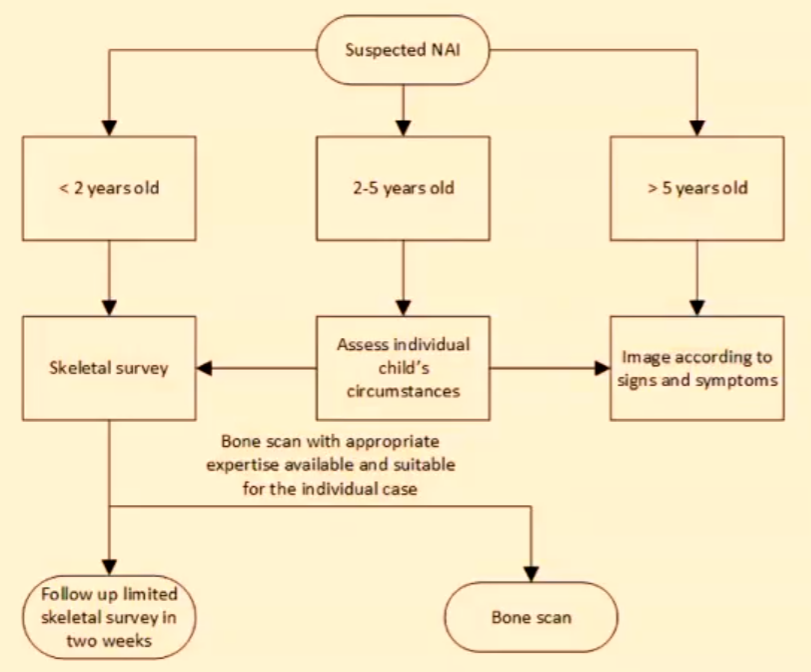
Suspected NAI Imaging Protocols (RANZCR 2022)
Age-Based Protocols:
< 2 years old: Skeletal survey.
2-5 years old: Follow-up limited skeletal survey in two weeks. Assess individual child's circumstances. Image according to signs and symptoms.
> 5 years old: Bone scan with appropriate expertise available and suitable for the individual case. Bone scan.
RANZCR 2022 Protocol - Detailed Views
Head, Chest, Spine, and Pelvis:
AP and lateral skull (if a volume acquired multiplanar CT head with 3D reconstructions has not been performed)
CAP (Cranio-caudal, AP) and lateral chest (to include shoulders and sternum), both obliques (to include all ribs, left and right, 1-12)
CAP abdomen and pelvis
Lateral views of the whole spine.
(For children under one year, this may be possible with one view; for larger children and those over one year, separate views will probably be required.)
Upper Limbs:
Where possible:
CAP of the whole arm (centered at the elbow if possible)
Coned lateral elbow
Coned lateral wrist
Posterior-anterior (PA) hand and wrist
In larger children where a single whole arm view is not possible:
CAP humerus (including the shoulder and elbow)
AP forearm (including the elbow and wrist)
Coned lateral elbow
Lower Limbs:
Where possible:
Whole AP lower limb, hip to ankle
Coned lateral knee
Coned lateral ankle
Coned AP ankle (mortise view)
Coned AP knees
DP foot
For larger children
AP femur
CAP tibia and fibula
Coned AP knee
Coned AP ankle (mortise view)
Coned lateral knee
Coned lateral ankle
DP foot
Supplementary views:
Additional views should be obtained in the following circumstances:
Lateral views of any suspected shaft fracture.
Coned lateral view of sternum when poorly demonstrated on lateral chest X-ray
RANZCR 2022 Protocol - Follow-up Imaging
Timing: 14 days, and no later than 28 days after the initial skeletal survey.
Views: Follow-up radiographs should be performed of any abnormal or suspicious areas on the initial skeletal survey plus the following views:
Chest:
Chest AP and lateral and both obliques (to include the shoulders and all ribs, left and right, 1-12)
Upper limbs:
Infants and small children:
AP whole upper limb (centred at the elbow if possible)
AP hand and wrist
In larger children where whole upper limb views are not possible:
AP humerus (including the shoulder and elbow)
AP forearm (including the elbow and wrist)
PA hand and wrist
Lower limbs:
Infants and small children:
Whole AP lower limb, hip to ankle
Coned AP knee
Coned AP ankle (mortise view)
DP foot
In larger children where whole lower limb views are not possible:
AP femur
AP tibia and fibula
Coned AP knee
Coned AP ankle (mortise view)
DP foot
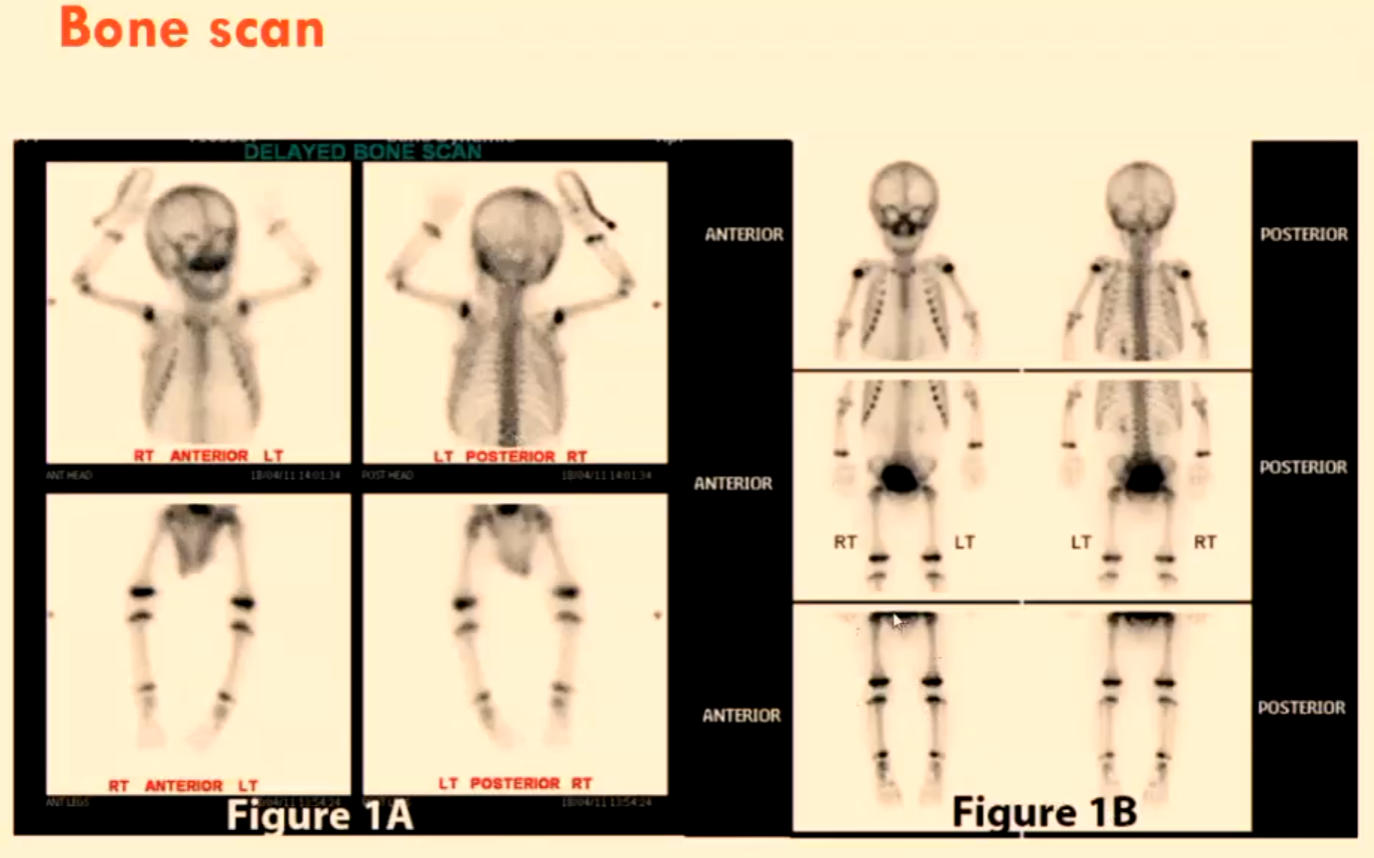
Bone Scan
Delayed bone scan images (anterior, posterior, RT anterior LT, LT posterior RT, ANT HEAD, POST HEAD, ANT LEGS).
Imaging Examples
Fractured ribs on CXR (6-week-old).
NAI lower legs (6-weeks-old) showing metaphyseal bucket handle fractures.
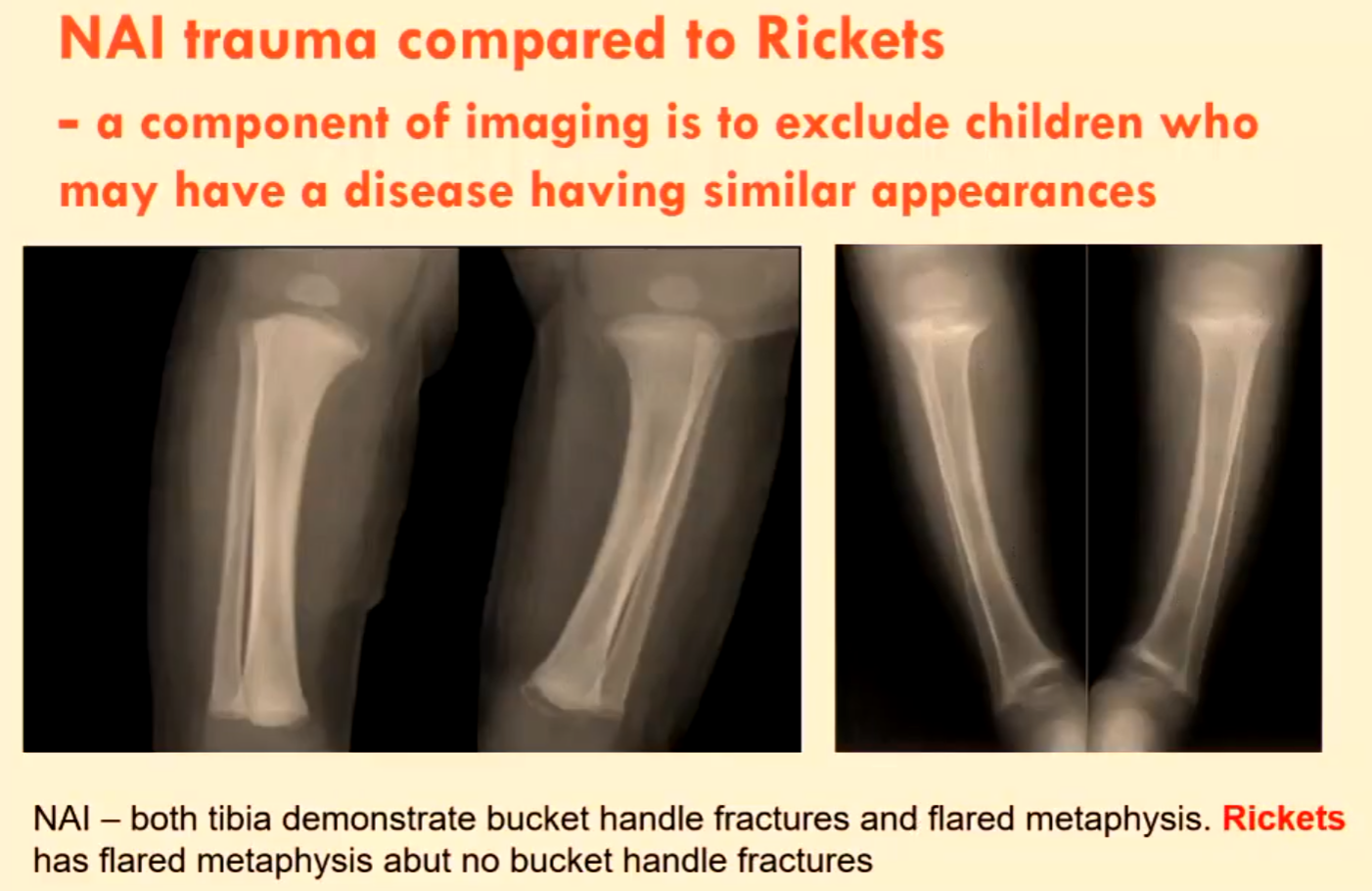
NAI Trauma vs. Rickets
Differentiation: Imaging helps exclude diseases with similar appearances.
NAI Findings: Both tibias demonstrate bucket handle fractures and flared metaphysis.
Rickets Findings: Flared metaphysis but no bucket handle fractures, associated with Vitamin D deficiency.
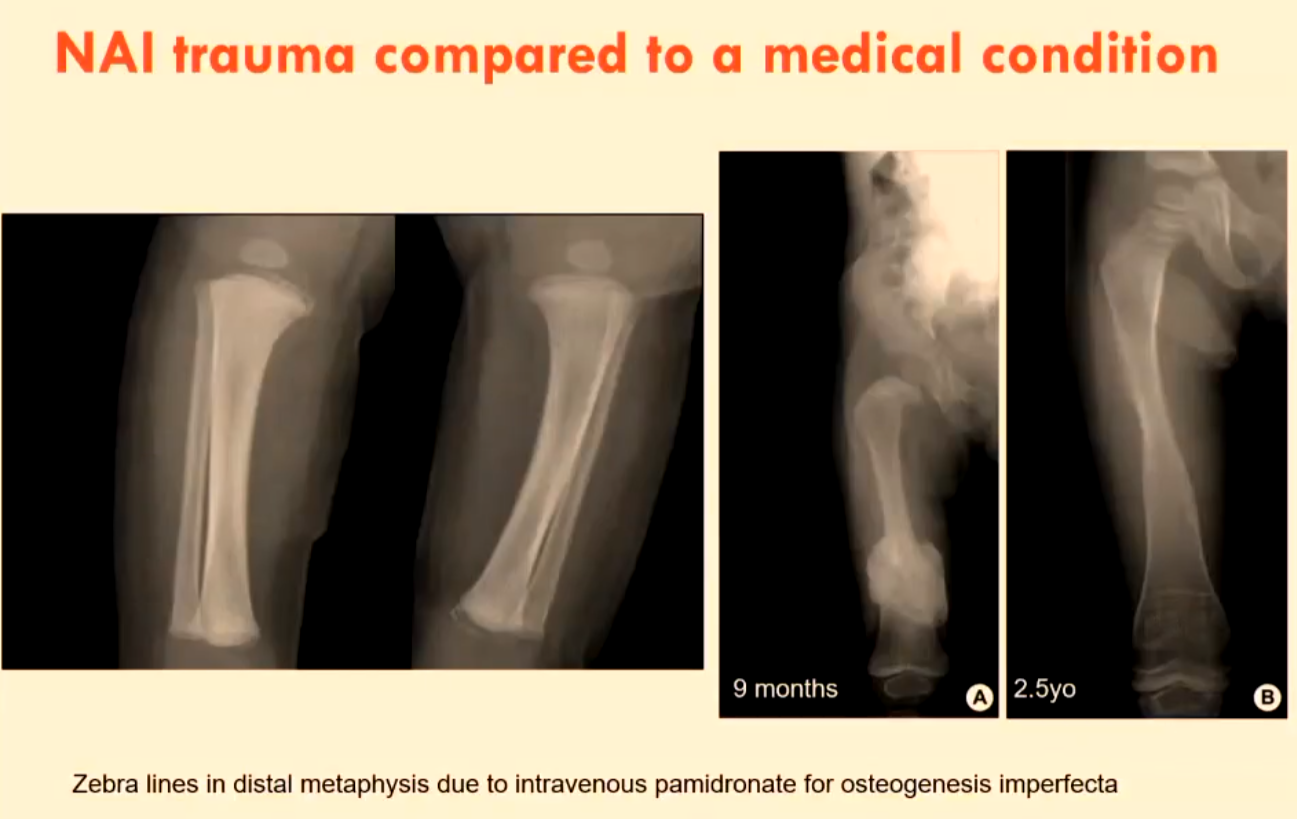
NAI Trauma vs. Medical Conditions
Example: Zebra lines in distal metaphysis due to intravenous pamidronate for osteogenesis imperfecta.
Ages: Example shown for a 9-month-old and a 2.5-year-old.
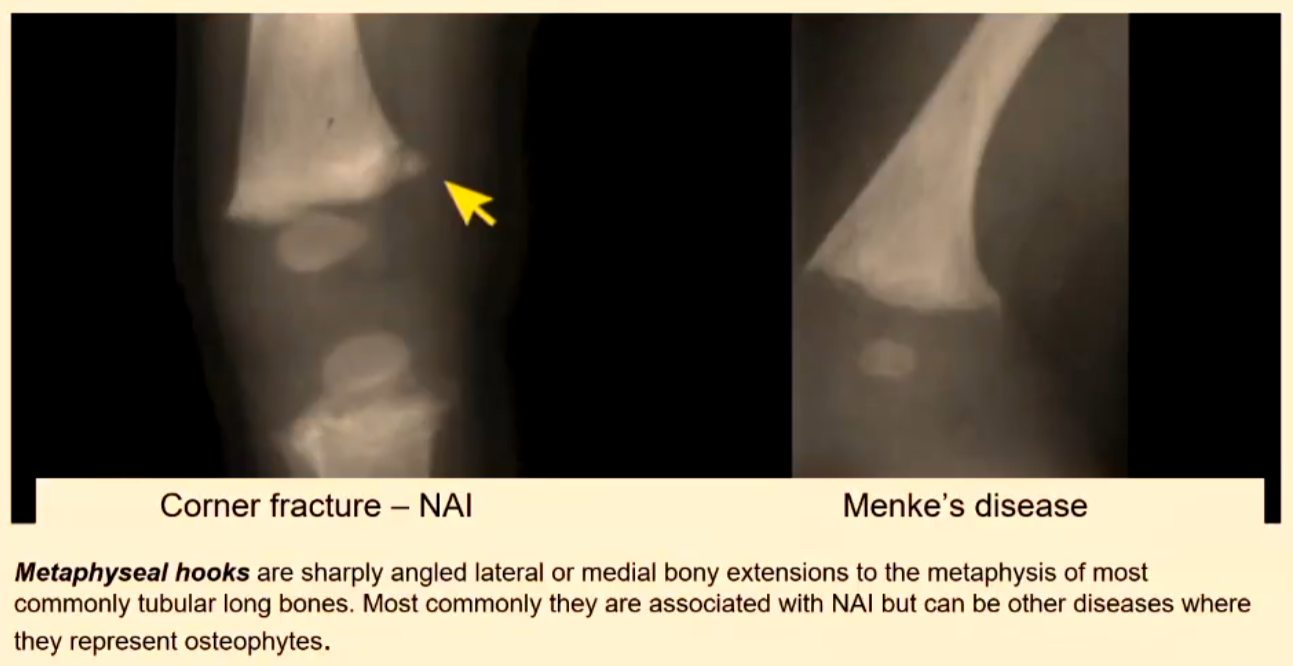
Other Diseases Mimicking NAI
Metaphyseal Hooks:
Description: Sharply angled lateral or medial bony extensions to the metaphysis of tubular long bones.
Association: Most commonly associated with NAI but can occur in other diseases.
Differential: Menke’s disease.
Metaphyseal Dysplasia vs. NAI
Both have metaphyseal hooks.
Metaphyseal dysplasia can resemble an old corner fracture.

Non-NAI Patients with Excessive Periosteal Reactions
Conditions:
Caffey’s disease
Osteogenesis imperfecta

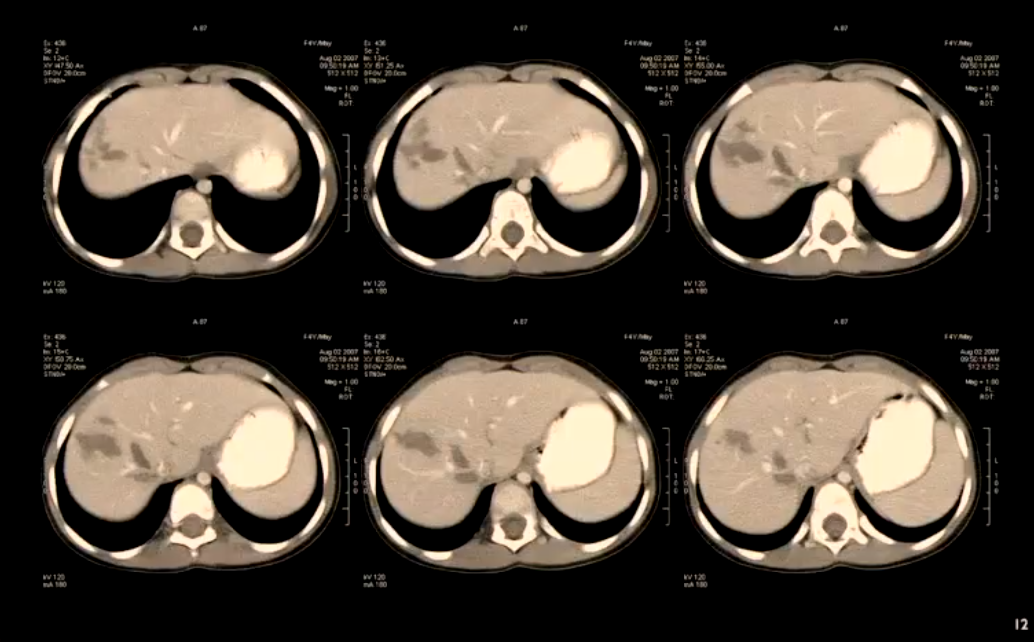
Case Study: 4-Year-Old with Sore Tummy
History: 4-year-old tripped and now has a sore tummy.
Findings:
Multiple irregular linear hypodense lesions in the right lobe of the liver, compatible with lacerations from blunt trauma (compression or shearing injury).
Mechanism Inconsistency: The stated mechanism of injury (a simple fall) is unlikely to produce such severe liver injuries.
Behavior: The child exhibited an