Fecalysis lecture
Introduction to Fecal Analysis
Fecalysis is a vital diagnostic tool used in medical practice to provide critical insights for the differential diagnosis of gastrointestinal (GI) disorders. It is particularly effective in detecting various conditions affecting the GI tract including malabsorption syndromes, infections, and neoplasms. One of its primary applications is in identifying GI tract bleeding through the use of the Fecal Occult Blood Test (FOBT).
Liver and Biliary Duct Disorders
Fecalysis plays a significant role in identifying liver and biliary duct disorders through the examination of stool components. The liver produces bile essential for fat digestion. A biliary obstruction can result in acholic stool, which is characterized by an absence of color due to the loss of stercobilin (the brown pigment in stool) and urobilin. This alteration in stool color is a key indicator of potential liver dysfunction or a blockage in the biliary ducts.
Maldigestion and Malabsorption
Fecalysis can effectively detect:
Maldigestion: This refers to issues primarily due to pancreatic insufficiency, where food is not adequately broken down. It is often associated with conditions such as chronic pancreatitis or cystic fibrosis.
Malabsorption: This refers to problems in nutrient absorption, which can be linked to a variety of conditions including Celiac disease or tropical sprue. The presence of steatorrhea (increased fat in the stool) is indicative of malabsorption issues or pancreatic problems. Fecalysis can also identify infections caused by various pathogens including bacteria, viruses, or parasites.
Composition of Stool
The normal components of stool include:
Bacteria: Microbiota that play a role in digestion.
Cellulose: Undigested plant material.
Undigested food: Reflects the efficiency of the digestive process.
Digestive juices: Enzymes and fluids that assist in digestion.
Bile pigments: Responsible for stool coloration.
Electrolytes: Essential for maintaining fluid balance.
Water: Constitutes a significant portion of stool.
Digestion Process Overview
Mouth:
Food combines with saliva, forming a cohesive mass known as bolus, which initiates the digestive process.
Esophagus to Stomach:
The bolus moves through the esophagus to the stomach. Here, hydrochloric acid creates chyme through the action of gastric acid on food.
Small Intestine:
Duodenum: The initial section where most chemical digestion occurs.
Jejunum and Ileum: Responsible for nutrient absorption; the total length of the small intestine can reach up to 20 feet.
Large Intestine:
Comprising the ascending, transverse, descending, and sigmoid colon, it absorbs additional water (up to 3000 mL) before the waste reaches the rectum.
Diarrhea Classification
Diarrhea manifesting as:
Characteristics: Occurs when the stool frequency exceeds three times a day with a consistency that is watery, typically weighing over 200 grams/day (normal: 100-200 grams).
Types:
Acute Diarrhea: Duration of less than 4 weeks.
Chronic Diarrhea: Lasting more than 4 weeks.
Mechanisms of Diarrhea
Secretory Diarrhea:
Characterized by an increased secretion of water, occurring even without oral intake. Often caused by infections with pathogens like Vibrio cholerae and enterotoxigenic E. coli. This type may show the presence of white blood cells (WBC), red blood cells (RBC), and mucus due to microorganisms.
Osmotic Diarrhea:
Results from poorly absorbed solutes in the bowel leading to a failure in water absorption. An example is lactose intolerance, where undigested lactose draws water into the intestine. Unlike secretory diarrhea, osmotic diarrhea is alleviated with fasting and does not present WBC, RBC, or mucus in the stool.
Malabsorption:
Involves impaired nutrient absorption, leading to the presence of creatorrhea (muscle fibers in stool) and steatorrhea. Causes include celiac disease and tropical sprue. Differentiating from maldigestion can be done through assessment of pancreatic enzyme levels.
D-Xylose Test
The D-Xylose Test is instrumental in differentiating between pancreatic insufficiency and intestinal malabsorption. The patient ingests 25 grams of D-Xylose, and subsequent blood and urine samples are collected and analyzed to determine absorption efficiency.
Intestinal Hypermotility
This condition is characterized by rapid transit time through the GI tract, often caused by factors such as secretory or osmotic diarrhea, the use of laxatives, or physiological stress.
Osmotic Gap Calculation
The osmotic gap can be assessed using the formula: 290 - (2 x fecal sodium + fecal potassium).
An osmotic gap greater than 50 mOsm/kg indicates osmotic diarrhea, while a gap less than 50 mOsm/kg suggests secretory diarrhea.
Specimen Collection
To perform fecalysis, a pea-sized stool sample should be collected in a non-contaminated container. Qualitative tests can be done from random samples, whereas quantitative evaluations are based on a three-day collection for fecal fat analysis. The FOBT necessitates acquiring two samples from different parts of three separate stools over the span of three days.
Stool Appearance and Color
Normal stool typically appears brown due to the presence of urobilin and stercobilin. Specific stool characteristics indicate various pathological conditions:
Acholic stool: Suggests hepatic obstruction.
Melena: Black stool, suggesting upper GI bleeding.
Hematochezia: Red stool, indicative of lower GI bleeding. The consistency of stools can range from watery to well-formed; types of stool consistency are categorized by the Bristol stool chart, with types 3 & 4 considered normal ranges.
Introduction (ME)
Microscopic Examination
Fecal WBCs: diarrhea with fecal leukocytes may suggest an inflammatory process, such as infection or ulcerative colitis (destruction of intestinal mucosa)
Invasive organism (+) for fecal WBC
Toxin producing organism (-) for fecal WBC
WBCs Present may signify:
➢ Ulcerative colitis
➢ Bacillary dysentery
➢ Ulcerative diverticulitis
➢ Intestinal tuberculosis
➢ Abscesses or fistula
WBCs Absent indicates:
➢ Viral gastroenteritis
Characterized by the presence of watery diarrhea, vomiting, and abdominal cramps, often caused by infections.
WBCs in stool:
Positive:
Salmonella.
Shigella
Campylobacter
Yersinia
Enteroinvasive E. coli
Negative: Toxin-Producing microorganism
S. aureus
Vibrio spp.
Viruses
Parasites
To examine WBC in the stool
Wet preparation with Methylene blue
Wright stain or gram stain
3 WBC / HPF is significant
More than 3 WBC / HPF must be reported.
Lactoferrin latex agglutination (Immunological test):
This test uses antigens specific to lactoferrin, which is a protein found in neutrophils, to detect the presence of white blood cells in the stool sample.
Detects fecal WBC even frozen specimen
Muscle fibers: Show undigested food, indicating issues with digestion or absorption
Significance:
pancreatic insufficiency
- bulky frothy stool with lots of fecal fats
Biliary obstruction-
Gastrocolic fistulas- abnormal connections between the stomach and colon, leading to diarrhea and malabsorption due to the rapid transit of food.
Muscle Fiber
Patient should include red meat in the diet
Procedure
Stool with 10% eosin
Examine slide for 5 minutes
Count the red-stained undigested muscle fibers
digested meat fiber has no striations
partially digested fiber has 1 striation
Undigested fiber has 2 striations
>10 /slide is significant
In fecalysis, the presence of striations can help determine the degree of digestion of meat fibers, where:
Digested meat fiber shows no striations.
Partially digested fiber exhibits 1 striation.
Undigested fiber displays 2 striations.A count of more than 10 striations per slide is considered significant and may indicate underlying digestive issues.
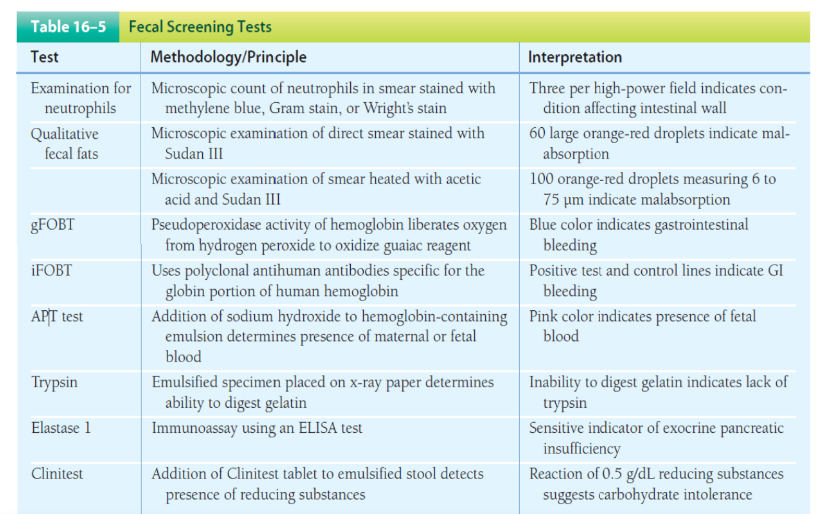
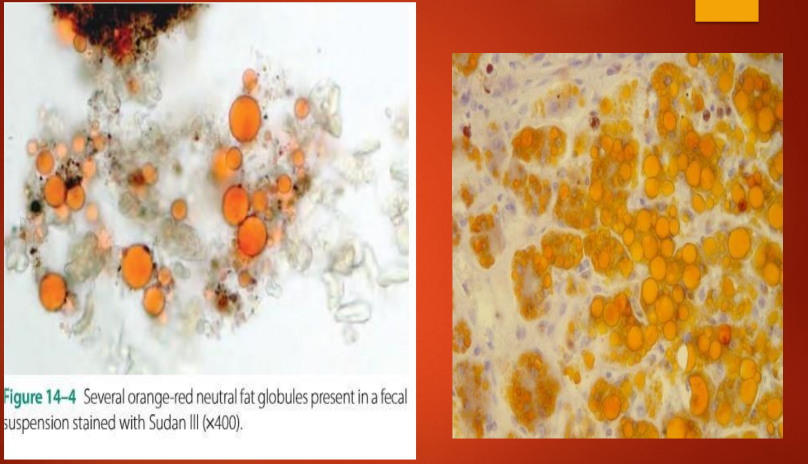
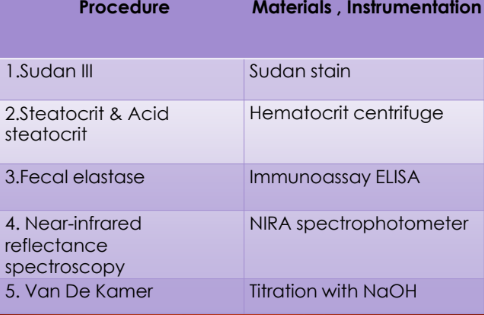
Qualitative Fecal Fat
Done in cases of steatorrhea and malabsorption syndromes
Types of Fats:
Neutral Fat (TAG)
Fatty acid salts or soaps
Fatty acid
Cholesterol
Stains used are Sudan III, IV OR ORO (Oil Red O)
Routinely used: Sudan III
Fecal Fat Testing
Neutral Fat Stain ( can only seen TAG in this method) is performed in the 1st slide.
1. Mix stool with 95% ethyl alcohol and sudan III
2. Count the large orange-red droplets
Significant: > 60 droplets / HPF
Split Fat Stain is performed in the 2nd slide.
Total fecal fat includes all types of fat found in feces free fatty acids ◦ fatty acids produced by hydrolysis of the soaps and the neutral fats
Mix stool with 36% acetic acid.
acetic acid in fecal fat testing is to aid in the hydrolysis of fats, specifically to break down neutral fats into free fatty acids and glycerol.
Stain with Sudan III.
Heat the mixture.
Count and take note of the size of fat droplets:
Normal: Less than 100 small droplets that are less than 4 micrometers (µm) in size suggests a typical amount of fat in the stool, indicating normal fat absorption and digestion.
Increased: More than 100 droplets ranging from 6 to 75 micrometers (µm) suggest excessive fat in the stool.
Note: The Neutral Fat Stain does not require heat because it relies on the solubility of neutral fats in the mixture of ethyl alcohol and Sudan III to visualize fat droplets.
- The Split Fat Stain utilizes heat to facilitate the hydrolysis of fats into free fatty acids, enhancing their visibility during staining with Sudan III.
The heating step is essential for breaking down neutral fats to allow for accurate measurement of the resulting fat droplets' size and number.
INTERPRETATION OF SLIDES:
Maldigestion:
Increased neutral fats on the 1st slide indicates that there is an issue with the initial digestion of fats, leading to undigested fats remaining present. This suggests a potential problem with pancreatic enzyme production or function, which is necessary for breaking down dietary fats.
Malabsorption:
Normal fat content on the 1st slide suggests that the fats are being digested properly, indicating no issues with fat digestion itself. However,
Increased total fats on the 2nd slide indicates that there is an issue with their absorption in the intestines.
Cholesterol Fecal Fat Testing:
Evaluates the presence of cholesterol in stool samples.
Procedure:
Stool is mixed with Sudan III then heated, allow to cool and then look for cholesterol crystals (notched-end rhombic plates)
Fecal Occult Blood Test (FOBT) Overview
Definition: The FOBT detects hidden (occult) blood in the stool that is not visible during microscopic examination.
Normal Findings: Typically, only small amounts of blood are present, with a reference of up to 2.5 ml of blood per 150 grams of stool considered normal.
Purpose: This test serves as a screening tool for colorectal cancer, helping to identify potential tumors or polyps that may cause bleeding.
Significant Findings: A finding of more than 2.5 ml of blood per 150 grams of stool is considered significant and may warrant further diagnostic evaluation.
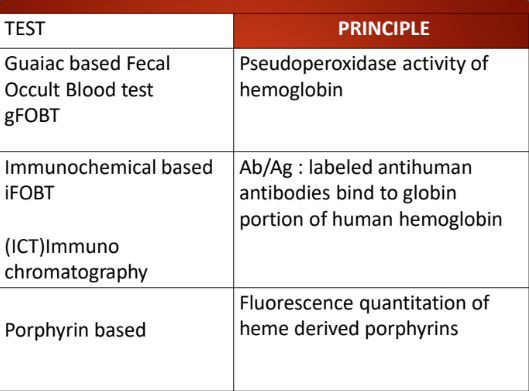
Guaiac-Based Fecal Occult Blood Test (gFOBT)
Overview: The gFOBT is one of the most frequently used screening tests for detecting hidden blood in the stool, which can indicate colorectal cancer.
Sample Collection:
Requires two samples taken from the center of the stool.
Stool specimens are collected over three consecutive days to improve test accuracy and sensitivity.
Testing Procedure:
The sample is placed on the front side of a slide that contains the Guaiac reagent using an applicator stick.
After the sample is applied, hydrogen peroxide is added to the back of the filter paper slide.
Interpretation: The reaction between the blood in the stool and the Guaiac reagent, in the presence of hydrogen peroxide, will produce a color change, indicating the presence of occult blood in the stool.
NOTE: Color blue indicates a positive result, while the negative result is indicated by no color change.
Principle:
Pseudoperoxidase activity of hemoglobin molecule react with the chromogen.
Gum guaiac is a commonly used reagent in fecal occult blood testing, known for not being sensitive.
However, it is not highly sensitive compared to other chromogens.
The sensitivity of chromogens varies:
benzidine- being the most sensitive,
O-tolidine, then
gum guaiac.
REMEMBER: BOGus
- A positive test result is indicated by a color change to blue, suggesting the presence of occult blood in the stool.
Causes of False Positive Results in Fecal Occult Blood Testing
Red Meat: Consumption of red meat can lead to false positive results. It's advised to avoid red meat for 3 days before testing to prevent interference with the test's accuracy.
Certain Vegetables: Foods such as horseradish, broccoli, cauliflower, radish, turnips, and melons may also cause false positive results if consumed within 3 days prior to the test. These foods contain compounds that can mistakenly indicate the presence of blood in the stool.
horseradish and broccoli are known to have peroxidase activity.
Aspirin and NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin can irritate the gastrointestinal (GI) tract and may lead to bleeding. Patients are advised to avoid these medications for 7 days before undergoing the test to reduce the risk of false positives.
Contamination: Menstrual blood or contamination from hemorrhoids can also lead to false positive results, as they introduce blood into the stool sample that is not from an internal source, affecting the test outcome.
Causes of False Negative Results in Fecal Occult Blood Testing
Vitamin C: High doses of vitamin C can interfere with the chemical reactions used in the fecal occult blood test. It can reduce the likelihood of detecting blood, leading to a false negative result. Therefore, it is advised to avoid vitamin C supplements for at least 3 days before the test.
Iron Supplements Containing Vitamin C: iron supplements that also contain vitamin C can negatively affect the test outcome by masking the presence of blood in the stool. These should also be avoided for 3 days prior to the test to ensure accurate results.
Immunochemical Fecal Occult Blood Test (iFOBT)
Specificity: The iFOBT is specifically designed to detect the globin portion of human hemoglobin, providing a more targeted approach.
Detection Method: It utilizes polyclonal anti-human hemoglobin antibodies, which enhance the test's specificity for human blood.
Dietary and Drug Restrictions: Unlike guaiac-based tests, the iFOBT does not require any dietary or drug restrictions before testing, making it more convenient for patients.
Sensitivity: This test is more sensitive to bleeding occurring in the lower gastrointestinal (GI) tract, allowing for better detection of potential issues such as colon cancer.
Clinical Relevance: It serves as an important indicator of colon cancer or other GI diseases, aiding in early diagnosis and intervention.
Upper vs. Lower GI Bleeding: Hemoglobin from upper GI bleeding is often degraded by bacterial and digestive enzymes before reaching the large intestine, leading to reduced detection rates. In contrast, there is little degradation of hemoglobin in lower GI bleeding, enhancing the iFOBT's ability to detect blood originating from this area.
Porphyrin-Based Fecal Occult Blood Test
HemoQuant: A specific type of test that uses a fluorometric test to detect hemoglobin in fecal samples.
Testing Method: This test measures hemoglobin based on the conversion of heme to fluorescent porphyrins, allowing for the detection of both intact hemoglobin and hemoglobin that has been transformed into porphyrins.
Labor Intensity: The test is labor-intensive and time-consuming, requiring careful handling and processing of samples.
False Positives: Consumption of red meat can lead to false positive results, as the heme present in red meat may interfere with the test outcomes.
Dietary Restrictions: There are no restrictions on the intake of fruits or vegetables prior to testing.
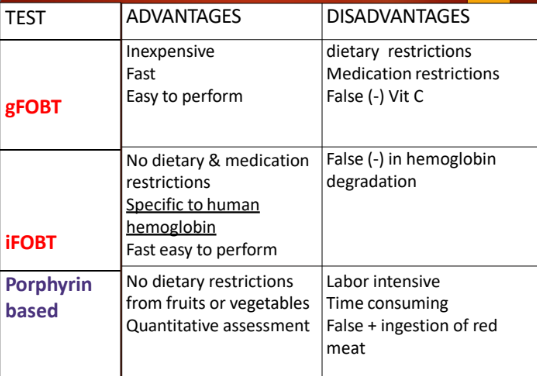
Summary:
Quantitative Fecal Fat Analysis
Purpose: This is a confirmatory test for steatorrhea, which is characterized by excess fat in the stool.
Results Reporting: The results are reported as grams of fat excreted per day, providing an essential measure of fat malabsorption.
Sample Collection: A 3-day specimen collection is necessary (72 hours) to obtain accurate results.
Diet Regulation: During the testing period, the patient is typically required to maintain a regulated intake of fat, usually around 100 grams per day, to standardize the test results.
Method: Van de Kamer Titration
Routine Use: The Van de Kamer titration method is routinely used in clinical settings to analyze fecal fat.
Conversion Process: In this method, fecal lipids are converted to fatty acids.
Titration: The fatty acids are then titrated to a neutral endpoint using sodium hydroxide, allowing for precise measurement of fat content.
Measurement Efficiency: This method measures approximately 80% of the total fecal lipid content, giving a reliable assessment of fat excretion.
Gravimetric Method:
Time-consuming method for analyzing fecal fat.
Utilizes corrosive and flammable solvents to extract lipids from the stool.
Extracts and quantifies all fecal lipids present, providing a comprehensive analysis of fat content.
Hydrogen Nuclear Magnetic Resonance Spectroscopy:
A rapid analysis method taking only about 5 minutes.
Considered safe as it does not involve hazardous materials or solvents.
Acid Steatocrit:
A rapid test designed to estimate the amount of fat excretion.
Requires only 0.5 grams of stool for testing.
Particularly useful in pediatric patients for assessing fat malabsorption.
Apt Test (Apt-Downey)
Purpose: The Apt test is designed to determine whether an infant's stool or vomitus originates from fetal blood or maternal blood (Or kay mother).
Procedure:
Emulsification: The specimen is emulsified in water to prepare it for testing.
Centrifugation: The sample is then centrifuged to separate its components.
Alkali Addition: 1% sodium hydroxide (NaOH) is added to the centrifuged sample.
Interpretation of Results:
Fetal Blood: Resists alkali denaturation; the sample remains pink in color, indicating the presence of fetal blood.
Maternal Blood: Sensitive to alkali denaturation; the color changes to yellow-brown, indicating the presence of maternal blood.
Fecal Enzymes
Trypsin
Function: A digestive enzyme responsible for the digestion of proteins. This enzyme is from the pancreas.
Clinical Significance: Abnormal levels can indicate conditions such as cystic fibrosis.
Test Methods: Uses Gelatin Hydrolysis
X-ray Film Test:
Positive Result: Clear x-ray film indicates the presence of trypsin.
Negative Result: X-ray film remains opaque, suggesting a lack of trypsin.
Chymotrypsin
Characteristics:
More resistant to intestinal degradation than trypsin.
Suitable for detecting less severe cases of pancreatic insufficiency.
Stable for up to 10 days at room temperature.
Testing Methods:
Gelatin Hydrolysis: A method used to assess activity.
Spectrophotometric Method: Commonly utilized for measuring enzyme levels.
Elastase I
Source: Produced by the pancreas.
Testing Method:
Immunoassay using the ELISA kit.
Very sensitive indicator of exocrine pancreatic insufficiency.
A single stool sample is used.
Mechanism:
Utilizes monoclonal antibodies against human pancreatic elastase-1.
Specific in differentiating pancreatic causes from non-pancreatic causes in patients with steatorrhea.
Carbohydrates Analysis
Absorption Issues:
Inability to absorb carbohydrates can be linked to conditions such as Celiac Disease.
Lack of Digestive Enzymes:
For instance, lactase deficiency leads to lactose intolerance.
Testing Method:
Copper Reduction Test (Clinitest Tablet):
Stool pH < 5.5 indicates malabsorption (normal pH is 7-8).
Presence of lactose in the stool suggests lactose intolerance.
Summary ng buong mundo