KHNES 4525 Study Guide
Lecture 1 - Intro to KNHES 4525
Health behavior: 2 definitions
- the actions of individuals, groups and organizations as well as those actions’ determinants, correlates and consequences
- Personal attributes such as beliefs, expectations, motives, values, perceptions and other cognitive elements; personality and overt behavior patterns
Physical Activity: any bodily movement produced by skeletal muscles that require energy expenditure
Exercise: a subset of physical activity that is planned, structured and repetitive and has as a final or intermediate objective improvement or maintenance of physical fitness
- Behavior Change has barriers and facilitators
Socio-Ecological Model of influence on behavior change - genetic to homeostatic to behavioral to environmental
CBT (cognitive triangle): thoughts behaviors and feelings all collectively play a role in behavior change
The top down approach:
- From the expert given to the new person
- Traditional medicine/clinics
- Giving orders and not equals
Compliance: implies behavior characterized by the extent to which people obey, follow instructions or use prescriptions
Adherence: implies that people freely choose to undertake behavioral plans and have collaborative involvement in developing and adjusting their plan
Passive participation: there by force, haphazard, not truly engaged
Active participation: wants to be involved and change - people are this
Lecture 2: Foundations of Changing physical activity behavior
Actual causes of death in the US → leading causes of death are diseases like heart disease and cancer but those things are actually caused by smoking, poor diet, inactivity or alcohol consumption
- Behavioral factors most prominent contributors to mortality
- Life-span increases but people are living with chronic disease and have low health-span
- Shift in focus to prevention care with money and public health goals and initiatives
Health Determinants: the range of personal, social, economic, and environmental factors that influence society
Beginnings of PA research:
- Studied correlates, antecedents and consequences
- Early studies were observational only and demonstrated high rates of heart disease in sedentary individuals
- London bus company
- Havard alumni study
- San Francisco Longshoremen study
- Observational studies can’t say the determinants of the disease → ice cream sales and shark bites)
WHO guidelines
- Limit sedentary time
- Replace sedentary time with PA of any intensity for health benefits
- Adults should aim to do more than the recommended levels of moderate to vigorous exercise
- Effects of high amounts of sedentary behavior
- All-cause mortality
- Cardiovascular disease
- Cancer mortality
- Cardiovascular disease
- Cancer
- Type 2 diabetes
- Key aspects
- Adults should do ≥ 150-300 min of moderate-intensity aerobic PA; or ≥ 75–150 minutes of vigorous-intensity aerobic PA; or an equivalent combination of moderate & vigorous-intensity activity throughout the week, for substantial health benefits”
- “Adults should also do muscle strengthening activities at moderate or greater intensity that involve all major muscle groups on ≥ 2 days/week, as these provide additional health benefits
- “Adults may increase moderate-intensity aerobic PA to ≥ 300 min; or do ≥ 150 minutes of vigorous-intensity aerobic PA; or an equivalent combination of moderate- and vigorous- intensity activity throughout the week for additional health benefits”
- Need to stay within the range to maintain benefits of PA without getting hurt
- Overall doing some PA is better than doing none and has significant benefits
- Look AHEAD Walden paper
Attitudes towards Physical Activity
- Ambivalence: you want to change and not change simultaneously
- Unable to maintain exercise long-term
- Going forward - examine mediators, moderators, casual pathways
- Convergence of exercise science and cognitive behavioral psychology
- Factors involved in the pathway from adoption to maintenance of behavior
- Health-related consequences of behavioral participation
Lecture #3:
Mediators: the process through which 2 variables are related
Moderators: affects the strength and direction of the mediators
Determinants show how someone goes from being sedentary to adopting physical activity
- 50% drop-out within 6 months
- 80% drop-out within 1 year
- How to get people to maintain exercise big question Why not??
Utility of Studying Correlates:
- Define what factors are related to adoption and maintenance
- Develop profiles and patterns of “active” and “inactive” individuals
- Identify potentially modifiable factors for experimentation
- Develop and tailor programs/interventions to correlates
- Refine theories and models used to predict behavior
Cross-sectional studies most popular - associations are considered
- Correlates not Causes
- Determinants are only in longitudinal studies
If exposure temporally precedes outcome assessment then they a provide strong basis for drawing casual inferences
Correlates = Generic Term; Determinant = specific to longitudinal
Observational vs Experimental
- Know that change in physical activity impacts health but not how
- Experimental shows the how people adopt the change and how to replicate and refine that change moving forward
Categories of Determinants:
- Demographic: age, gender, status, education
- Program Factors: intensity, duration v frequency, home v gym
- Environmental: built environment, access to facilities
- Knowledge, Attitudes and Beliefs: Confidence, self-efficacy, motivation, knowledge and expectations of PA
- Psychological/Behavioral Skills: self-regulatory skills or EX skills, personality, mental health
Lecture #4:
Intervention: systematic approaches targeting modifiable determinants of PA/EX adoption and adherence
- Not directly changing target behavior but instead modifying determinants to yield behavior change
Behavior patterns: antecedent → behavior → consequences
2 needs for effective intervention:
- Manage antecedents by providing elements to motivate one to adopt PA/EX
- Manage consequences by providing appropriate reinforcement of activity
Informational Intervention:
- Provide information about PA/EX behavior
- Increases awareness of opportunities for PA/EX
- Increases awareness of negative attitudes and barriers to PA/EX
Social Intervention:
- Develop PA/EX groups of people who want to make change
- Dyadic approaches
- Finding and assigning groups of individuals to work together to make behavior changes
- Increases confidence, motivation and accountability
Policy and Environmental Intervention
- Creating activity-friendly environments
- Modifying school-based physical activity curriculum
- Access to activity facilities and resources
Behavioral Intervention
- Teach behavioral skills that aid adaptation and adherence
- Provide opportunities for practice and mastery of these newly acquired behavioral skills
- Develop plans to get active and stay active
- Learn to recognize and manage situations that threaten exercising plans
Behavioral Skills
- Self-monitoring: Process of recording thoughts, feelings and behaviors related to making progress towards desired goals
- Informs behavioral goals
- Where you are so you can see how to get to where you want to be
- Can be done using Ratings of Perceived Exertion (RPE)
- Daily diet and activity using logs and apps
- Goal-Setting: process of creating valued goals for activity, fitness, performance, etc. to help develop and sustain motivation to exercise
- Cyclical and done on a trial-and-error basis - takes time to develop
- Barrier Problem-Solving: overcoming barriers to PA/EX adoption/maintenance is a key self-regulatory behavioral skill that supplements the process of goal setting and planning
- 3 most frequent barriers
- Time
- Accessibility
- Boredom with PA/EX
Most effective interventions are behavioral
- Most effective integrate multiple different types of behavioral strategies
Concept of multi-level intervention
- Downstream: these approaches are needed to treat individual lifestyle-related health conditions and foster self-management of lifestyle behaviors
- Midstream: intervention at social/organizational levels to establish conditions that support lifestyle behavior
- Upstream: Change in regulatory policy and environmental conditions necessary to support,enable and reinforce lifestyle changes
Lecture #5:
Self-regulation skills are the missing link between intention and action towards goal realization
Intentions explains 22-35% of variance in PA behavior
Self-regulation skills can make that difference in impact
Self-monitoring: a cognitive behavioral self-regulation strategy that requires individuals to keep track of their own behavior
- Not one way to do it
- Many tools exist
- The goal is to manage barriers to self-monitoring and encourage consistency of use over-time
Goal-setting
Process (behavior) goal: set and/or agree on a goal defined in terms of behavior to be achieved
- Daily walking goal
- 2 full-body resistance training sessions per week
Outcome Goal: Set or agree on a goal defined in terms of a positive outcome of desired behavior
- Weight loss goals as outcome of lifestyle changes
- 5% increase in 1-RM as outcome of training
SMART Goal Setting: Specific, Measurable, Achievable/Appealing, Recordable/Realistic, Timeline - a way to set goals
Barrier Problem-Solving: analyze or prompt the person to analyze factors influencing the behavior and generate or select strategies that include overcoming behaviors and/or increasing facilitators
- Self-monitoring and goal setting form foundation for this to be effective
IDEA Barrier Problem-Solving:
- Identify - stop and reflect on thoughts feelings and behavior; identify barrier
- Develop - develop list of possible solutions
- Evaluate - choose possible solution to try, develop action plan to carry out
- Analyze - analyze results, reevaluate plan and recycle process
Toolbox for Success:
- Empower individuals to take and maintain action towards goals
- Visualize building a ‘toolbox’ of self-regulation skills
- Apply the tools to barriers in order to maintain success
GMCB: group-mediated cognitive behavioral lifestyle - supportive model for integrating all tools into toolbox with the help of group-mediated support and individual planning
Lecture #6:
The righting reflex: telling people what we think they should do
- Installing change
- top-down approach of I am the expert
- When met with ambivalence sets the stage for argument and resistance
- Feelings of: anger, defensiveness, misunderstanding, ashamed, helplessness, trapped
- Behaviors: disengagement, procrastination, relapse
Examples
- might think patients don’t see so we try to give them insight
- Might think patients don’t know so we try to give them knowledge
- Might think patients don’t know how so we try to give them skills
Motivational Interviewing:
- The spirit: People make changes only when ready, Collaborative, Evocative - bring forward and elicit change processes, Support autonomy through caring and compassion
- Change of roles: you can’t give all the answers and support, teach to roll with the punches, patient works harder than caregiver
- Principles of MI:
- Accurate Empathy: desire to see the world from another person’s perspective
- Autonomy: they make all the decisions about what to do, people are free to change
- Evocation: you have what you need and we will work together to find it, reflections and reflective listening
- OARS
- O = Open Questions - facilitates change talk
- A = Affirmations - statements about efforts, achievements and insights
- R = Reflections - listen to what is said rather than asking focusing on next comment
- S = Summaries - simple: repeat or rephrase, complex: paraphrase and add more details
- Change Talk: I want to lose weight
- Activated change talk: I’m thinking about going to a gym so that I can get some activity; That might help me lose weight
- Sustain Talk: I want to keep eating so I’m not even going to try and lose weight
Preparatory Language:
- D = Desire (want, would like, wish)
- A = Ability (could, can, might be able to)
- R = Reason (would probably feel better if)
- N = Need (ought to, have to, really should)
Commitment Language:
- C = Commitment (going to, will, intend to)
- A = Action
- T = Take steps (I actually went out and did…)
Managing difficult clients:
- Chatty participant: specific questions, time limit, use body language, interrupt in polite ways and summarize
- Emotional participant: be aware of own emotional response, empathize and name emotion, small groups to take focus off the individual
- Silent participant: large groups into small groups, popcorn call and response, inquire privately with person about why
- Resistant Participants: invite person to share experiences, don’t single the person out, remain calm with good eye contact and reassure that reaction is normal
- “Factual” participant: remain calm and know its ok to not know the answers, trust the process, say thank you for sharing and move on
Lecture #7:
Theory: set of interlaced concepts, definitions, and propositions that preset a systematic view of events or situations by specifying relations among variables in order to explain and predict the events or situations
- Relationship between dependent and independent variables
- Identifies potential mediating variables of behavior change
Model: draws on number of theories to help understand specific problem in particular setting or context
Constructs: concepts developed for a particular theory
Variable: how a construct will be measured (Latent, Manifest, IV, DV, MV)
Surveillance Research: research that tracks population-wide trends in behavior/outcomes
Basic/Fundamental Research: research into determinants
Intervention Research: research aimed towards change in mediators and outcomes
Application/Program Delivery: research aiming to systematically improve intervention delivery, acceptability, scalability, and effectiveness
Uses of Theory
- Planning - Why are people not following recommendations?
- Implementation - how can we modify intervention strategies to make an impact on the target population?
- Evaluation: What should be monitored, measured, compared?
Types of theories:
- Explanatory Theory: describes and identifies why a problem exists
- Example: HBM
- Change Theories: guide development of interventions, forms the basis for evaluation
- Example: SCT
- Implementation Theories: Change theories that link theory to specific problem, audience and context
- Example: Intervention Mapping Model
Theories must include:
- Major explanatory factors
- Hypothesized relationships
- Specified conditions
- Applications
- Must be TESTABLE
Interventions based in theory are favored over those not based in theory
Theory-Informed Research: 69.1% of studies (just acknowledging theory)
Theory-based Research: 17.9% of studies (apply theories)
Testing theory/Creating or Revising theories: 9.4% of studies
Lecture #8
Most thoroughly tested theories of behavior change are: HBM, SCT, Theory of Planned Behavior and Transtheoretical Model
- 82 formal theories of behavior change
HBM was one of the 1st theories of health behavior
- Developed to understand why people did or did not adopt preventive services offered by public health departments
Primary principles of motivated action according to HBM:
- Individuals will take action to ward off or control illness if:
- Perceived to be susceptible
- Consequences perceived to be serious
- Action will be beneficial
- Benefits outweigh barriers
- Feel confident to overcome barriers
- Cue to action prompts behavior
Focuses on how attitudes and beliefs explain and predict health behaviors
Posits that desire to prevent illness and belief that a specific action can achieve that goal will motivate behavior change
Challenges to HBM as explanatory theory include:
- People not susceptible to disease less likely to want to change behavior
- Does not weigh economic, environmental, or social factors to change
Motivation: degree of determination, drive, or desire with which an individual approaches or avoids a behavior
- Direction and intensity of one’s effort
- Origin of motivation
- Intrinsic: from within
- Extrinsic: motivation from a force outside an individual
- Closely related to intention constructs in many theories of health behavior change
Original HBM 1.0 5 core constructs:
- Perceived Susceptibility: assessment of chances to get disease
- Perceived Severity: judgment of seriousness of effect of getting disease
- Perceived Benefits: individual’s evaluation of positive things that will happen as a result of enacting health behavior
- Perceived Barriers: opinion regarding costs of enacting health behavior
- Cues to Action: consists of prompts to cue health behavior
HBM 2.0 adds:
- Self-efficacy: one’s belief about their capabilities to produce designated levels of performance that influence events affecting their lives; determine how you think, feel, motivate and behave
- Identifies modifiable targets for change
Cues to action are needed when perceived threat is great
Lecture #9
TRA → TPB → IBM development trajectory
TRA = Theory of Reasoned Action
- Assumes people are rational actors
- People process information and are motivated to act
- Basic Idea: people make rational decisions about behavior based on information and beliefs about the behavior and its consequences, what they expect and the value they place on its outcome
Attitudes and Subjective Norms are the antecedent to Intention which is the antecedent to
Behavior
Intention most important determinant to behavior however the gap exists
Intention: a person’s estimate of the likelihood they will perform a specific behavior
Attitude: behavioral beliefs, evaluation of behavioral outcomes
Subjective norm: the belief of whether most people approve or disapprove of behavior, normative belief, motivation to comply
TPB = Theory of Planned Behavior
- To predict behaviors with incomplete volitional control
- Some control of outcome but not total
- Perceived behavioral control (PBC) added to TRA to account for factors outside an individual's direct control
- Another antecedent to intention
- Control beliefs: likelihood of behavioral support or constraint
- Perceived Power: likelihood one’s control will facilitate or inhibit behavior
- Another antecedent to intention
- More effort will be expended when perception of control is high!
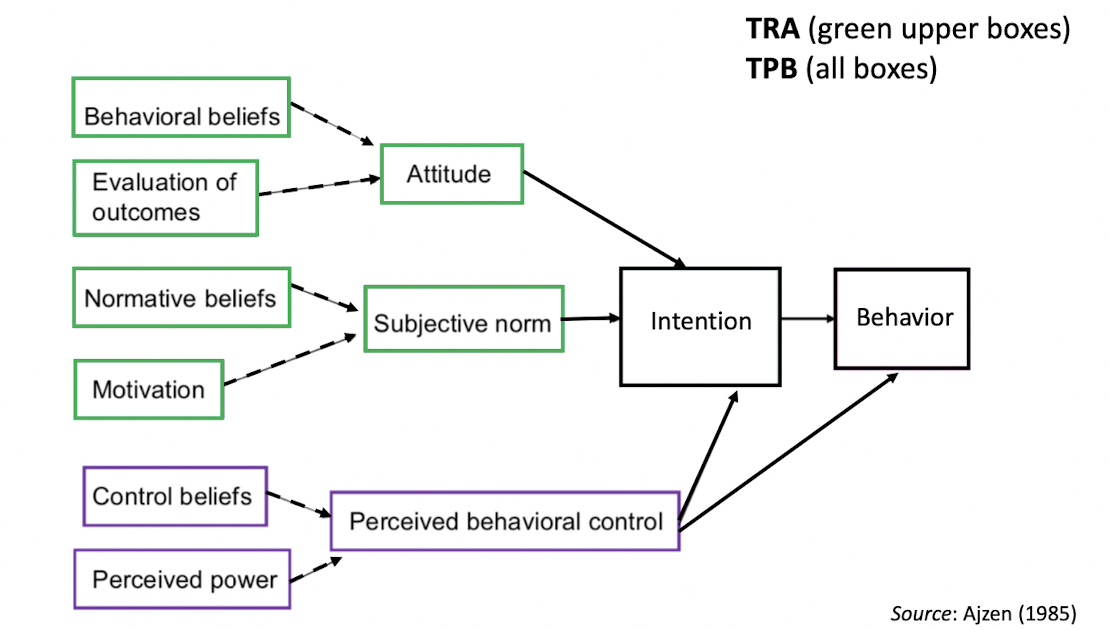
TPB and Targets of Intervention:
- Aimed at enhanced perceived behavioral control
- Promote sense of personal control over one’s PA/EX behavior
- Strategies
- Allow exercisers some input when designing their program
- Teach exercisers methods to control perceived barriers to PA/EX
TPB results
- Intention strong predictor of PA/EX
- PBC is a moderate indicator of PA/EX
- Attitude and PBC are strong predictors of intention
- Subjective norm is a weaker predictor of intention compared to attitude or PBC
Lecture #10
Integrated Behavioral Model = IBM
Constructs from:
- TRA
- TBP
- HBM
- SCT
Intention remains the most important determinant of behavioral engagement
- Without motivation a person is unlikely to carry out a behavior
NEW: even if intention is strong, other factors are STILL needed
IBM 3 categories of constructs:
- Attitude
- Experimental attitude: an individual’s emotional response to an idea of performing a recommended behavior (TRA)
- Instrumental attitude: beliefs about outcomes of behavior (TRA)
- Perceived Norm
- Injunctive Norm: perceptions about what others think one should do (TRA)
- Descriptive Norm: perceptions about what others are doing
- Personal Agency
- Self-efficacy: degree of confidence in performing the behavior (HBM and SCT)
- Perceived Control: perception of degree of whether certain factors under one’s own control make it easy or difficult to carry out the behavior (TPB)
In addition to intention IBM posits 4 additional constructs which affect behavior
- Knowledge and skill in performing behavior
- Salience of Behavior
- Environmental constructs
- Habit
Important to ask questions which will elicit a response about each category (open-ended)
TRA - cognitive factors that determine motivation
TPB extends TRA with Perceived Behavioral Control
IBM was created by consensus
Lecture #11
Transtheoretical Model: health behavior change model integrating key elements from 300+ theories of health behavior, behavior change and psychology, designed to apply to and unite dominant theories/model at the time
- Successfully applied to the study of smoking cessation and then extended to other risk behaviors
6 main assumptions:
- Theories of health behavior change differ from theories of health behavior
- Theories of behavior - more concerned with the best predictors of future behaviors, favor variables that account for most variance in behavior
- Theories of behavior change - more concerned with the best predictors of future behavior change, favors variables that yield the most behavior change
- No single theory can account for all complexities of behavior change
- Behavior change is a process that unfolds over time through a sequence of stages
- Stages are stable and open to change just as health behavior risks are stable and open to change
- Most at-risk populations are not prepared for action and will not be served effectively by traditional action-oriented behavior change programs
- Specific processes and principles of change should be emphasized at specific stages
6 Stages of Change Descriptions:
- Descriptive
- Categorical
- Behavior specific
- Cyclical and bidirectional
- Early stages: cognitive
- Later stages: behavioral
6 Stages:
- Precontemplation: no intention to take action in the near future
- Contemplation: intends to take action in near future; considering pros and cons of modifying behavior
- Preparation: intends to take action soon and has taken some behavioral steps in this direction
- Action: has demonstrated recent specific overt modifications to change behavior
- Maintenance: has demonstrated specific sustained modifications in behavior
- Termination: no temptation to relapse and 100% confidence
Lecture #12
Transtheoretical Model: Process of Change
In early stages people rely on:
- cognitive
- Affective
- Evaluative
In action-oriented stages, people rely on:
- commitments
- Conditioning
- Contingencies
- Environmental controls
- Helping relationships for progressing towards maintenance
Cognitions, behaviors and emotions are proposed ‘targets’ of intervention
“Covert” and “Overt” activities aimed at modifying these targets to facilitate movement through the stages of change
10 major processes have been identified to date:
- 5 Experimental processes: aim to increase awareness of benefits of changing thoughts and feelings about one’s self and PA/EX behavior
- Consciousness Raising: seeking new information to better understand EX
- Self-Reevaluation: assessing how one thinks and feels about oneself as an inactive person
- Environmental reevaluation: considering how inactivity affects the physical and social environment
- Dramatic relief: experiencing and expressing feelings about becoming more active or remaining inactive
- Social Liberation: increasing awareness of the social and environmental factors that support physical activity
- 5 Behavioral processes: aime to change actions or aspects of environment that can affect PA/EX participation
- Self-liberation: activities that strengthen one’s commitment to change and belief that one can change
- Counterconditioning: substituting physical activities for sedentary activities
- Stimulus Control: controlling situations and cues that trigger inactivity and skipped workouts
- Reinforcement management rewarding oneself for being active
- Helping relationships: using support from others during attempts to change
- Which stage each change process mediates:
- Precontemplation: consciousness raising, dramatic relief, environmental reevaluation
- Contemplation: self-reevaluation
- Action: Self-liberation
- Maintenance: counterconditioning, helping relationships, reinforcement management, stimulus control
3 principles of change:
- Decisional Balance: weighing the pros/cons of changing
- Pros = benefits of changing
- Cons = costs of changing
- Must consider inherent value of the pros and cons when planning
- Pros must be increased by x2 as much as cons are decreased for average peron to move from one stage to another
- Self-Efficacy: level of confidence one can perform the behavior across increasingly challenging situations without relapse
- SE in situation and behavior specific
- Critical to motivation for increasing PA/EX participation
- Assumed that barrier/coping SE increases across stages
- Temptation: intensity of urges to engage in unhealthy behaviors across challenging situations
- Common triggers: negative affect, social cues, cravings/biological signals
- Essentially converse of self-efficacy
TTM and other models provide…
- Additional descriptive layer to integrate with other theories/models
- Suggested pathways of progression with targets and activities for planning intervention/modification
Critiques of Stage Models
- Stages and processes have not been useful for predicting PA change
- False classification of meeting guidelines
- Probabilities of predicting 6mo PA by stage were worse than chance
- TTM assumes that stage-matched interventions would be more effective than those that were not
- Data does not confirm this
Lecture #13
Social Cognitive Theory targets both:
- Intrapersonal: within individual
- Interpersonal: within social
- Fundamental assumption: social connections influence health
- Also influence learning/decision making, emotional response, perceptions of capabilities, coping strategies, sense of belonging
- Posits that cognitions, affect and behaviors of individuals are shaped by the people with whom they interact with through 2 key social processes:
- Perceived/Actual Social Support
- Social Influence
Why use groups:
- Theoretical Rationale:
- Groups are agents of change - source of influence over members
- Social influence present in all activities
- Groups are targets for change - entire group is considered for change
- Groups are agents of change - source of influence over members
- Clinical Rationale
- Processes: patient monitoring and therapist feedback; patient provide feedback to other members; patients learn in safe group and can communicate about experiences in ways that otherwise could not; social modeling of desirable self-regulatory behaviors of others in group
- Outcome: facilitate commitments and accountability; produce group cohesins -support for adherence; increase peer to peer collaboration; acceptance of common process + goal
5 basic capabilities of humans that facilitate behavior:
- Symbolic capability
- Forethought capability
- Vicarious capability
- Self-regulatory capability
- Self-reflective capability
People want control of life events which influences motivation for volitional behavior
One’s behavioral motivation is directly influenced by self-efficacy judgements - Will I succeed?
Triadic Reciprocal Determinism: influenced by bidirectional interactions
- Cognitive constructs:
- Self-efficacy: the belief that one can produce desired outcome
- Collective efficacy: situations where individuals do not have control over social conditions that affect their lives
- Outcome expectations: expectations about the consequences of taking action
- Knowledge: understanding the health risk and benefits of different practices
- Social Environmental Constructs
- Observational Learning: social modeling
- Normative Beliefs: norms + beliefs about social acceptability and perceived prevalence of behavior
- Social Support: perception of encouragement and support a person receives from social network
- Opportunities and Barriers: attributes of environment that makes behaviors harder or easier to perform
- Behavioral Constructs
- Behavioral and self-regulation skills
- Intentions: serve as an indicator of readiness to perform behavior
- Reinforcement and punishment
Self-efficacy is a situation and behavior-specific judgment of one’s ability to produce desired outcome and determines:
- The challenges people undertake
- How much effort people expend in the face of obstacles
- How long people persevere
- Whether failures are motivating or demoralizing
Low SE:
- Avoid challenges
- Give up quickly when faced with obstacles
- Weak commitment to chosen goals
- Undermine their own efforts
- More prone to stress and depression
High SE:
- Approach difficult tasks as challenges to be mastered
- Set challenging goals
- Stronger commitment to goals
- Failure = insufficient effort
- Quickly recover from setbacks
Improving SE:
- Mastery experiences: success with a task
- Vicarious Experiences: modeling
- Verbal persuasions: meaningful feedback from valued individual
- Physiological and affective states: manage somatic appraisals and decrease negative affective states
SCT map
SE → outcomes, Goals, Socio Structural Factors (and behavior) → Behavior
Self-regulation also key to adoption and maintenance of behavior change
- Monitoring behaviors, setting/updating goals, managing barriers, preventing relapse…
Lecture #14
Humans can be:
- Motivated or ambivalent
SCT tells us these are critical for behavior change:
- Intention
- Self-efficacy
- Self-regulation
- Outcome expectations
- Social dynamics
Setting an intention is a strong predictor of behavior but not always the independent result of action towards changing behavior
SDT:
- Posits motivation is at the core of PA/EX behavior change
- Motivation → action towards PA/EX change → desired health outcomes
- Social factors facilitate and inhibit motivated action
- Important for providers to match interventions to individual motives
- Argues that motivation is often treated as singular construct
- Inclination towards activity but vulnerable to passivity
- People have different types of motivation
- Initial focus: what motivations are being exhibited?
- Identifies continuum to move forward
- Affects learning, performance, personal experience, well-being
- Allows for investigation of how each type is being developed
- Explains processes for making change: what conditions elicit self-motivated and self-regulated action?
3 types of motivation on a continuum varying in the extent to which their regulation is autonomous:
- Amotivation: lacking any motivation to engage in activity
- Results from:
- Not valuing an activity
- Not feeling competent in doing it
- Not expecting to yield desired outcome
- Results from:
- Extrinsic Motivation: doing activity because it leads to outcome
- 4 stages in between
- External regulation: performed to satisfy an external demand or reward contingency
- Introjected regulation: taking in a regulation but not fully accepting it as one’s own, performed to avoid guilt and anxiety
- Identified regulation: reflects conscious valuing of behavioral goal such that the action is accepted or owned as personal importance
- Integrated Regulation: occurs when identified regulations are fully assimilated to the self which means they have been evaluated and brought into congruence withone’s other values and needs similar to intrinsic but still done to achieve outcome rather than enjoyment
- 4 stages in between
- Intrinsic motivation: doing activity for inherent satisfaction of doing activity itself
- To know more
- To accomplish accomplishments
- To experience stimulation
Developing intrinsic motivation:
- Internalization: people’s acceptance of a value or regulation style
- Integration: further transformation of that regulation into their own
- Internalizing regulation leads to greater autonomy
- Satisfying basic needs:
- Autonomy: need to have control over one’s life
- Competence: need to be effective in one’s activity
- Relatedness: need to feel belongingness and connectedness with others
- These determine direction and persistence in engaging with goal-directed behavior
- Tangible rewards, threats, deadlines, directives, pressured evaluations and imposed goals diminish intrinsic motivation
Lecture #15
HAPA suggests social cognitive continuum models of health behavior change should promote change through addressing processes within 2 distinct phases:
- Motivational Phase: pre-intentional
- First an intention to change is developed
- Primarily based on self-beliefs
- Requires thinking mindset
- Confidence to initiate PA/EX
- Develop motivation to act
- Anticipate outcomes
- Outcome expectancies and Risk Perception part of this phase
- First an intention to change is developed
- Volitional Phase: post-intentional
- Second the change must be planned initiated and maintained
- Requires a doing mindset
- Self-regulation is critical
- Confidence to maintain PA/EX
- Newly adopted behavior may be difficult to maintain than first thought
- Need belief that one can manage barriers as they arise
- Action and Coping planning as well as resources part of this phase
- Second the change must be planned initiated and maintained
3 mindsets along this path to change:
- Nonintenders: improve SE, discuss outcomes
- Intenders: benefit from planning to translate intentions to actions and other self regulation strategies
- Actors: benefit from relapse prevention strategies, avoiding all or nothing, group accountability
4 key beliefs for priming action:
- Self-efficacy
- Outcome expectancies
- Intentions
- Risk Perceptions
5 key steps to go from intention to action to maintenance
- Make detailed plans
- Take action
- Persist
- Possibly fail
- Recover
HAPA is a 2-layer model:
- Continuum layer is conceptually useful
- Phasic layer is pragmatically useful