CHAPTER 37
SPINAL CORD INJURY
SCI is a catastrophic event causing loss of mobility or sensation.
Can result from direct spinal cord injury or indirect damage to bones, tissues, or blood vessels.
Mechanisms of injury:
Hyperextension
Hyperflexion
Rotation
Vertical compression (axial loading)
Penetrating injuries
Compression
12,000 new SCIs each year in US
300,000 Americans living with SCI.
Decrease life expectancy and increase mortality
30% rehospitalization rate
Risk factors:
High-risk physical activities (speeding, alcohol, drug use).
Lack of protective gear in sports.
Falls in the elderly.
Age 16-18
Male
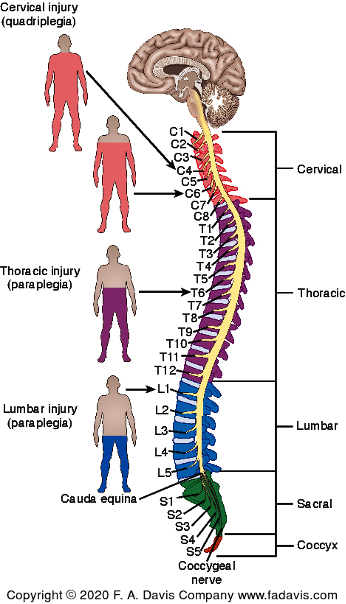
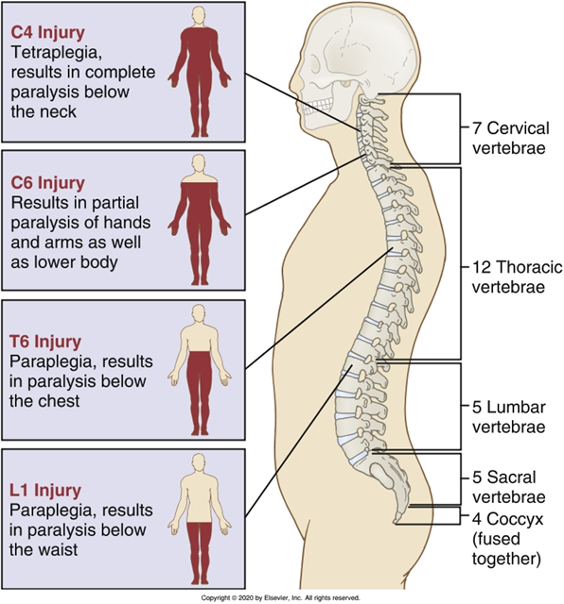
Most common injury levels: C4, C5, C6, T12.
Types of SCI:
Incomplete tetraplegia (47%)
Paraplegia (~20%)
Quadriplegia (~20%)
Leading causes:
Motor vehicle accidents (38%)
Falls (31%)
Violence/gunshot wounds (15%)
Sports injuries (8%)
Pathophysiology
SCI results from:
Concussion
Contusion
Compression
Tearing/laceration
Transection
Ischemia
Spinal cord anatomy:
Upper motor neurons: Carry messages between brain and spinal cord.
Lower motor neurons: Transmit signals to the body (sensory + motor).
Primary Injury: Direct trauma to neurons, glia, and blood vessels, or a penetrating trauma
Mechanical injury such as shering and compression forces, Vasculature disruption, Cell death
Disruption: Respiratory difficullties, neurogenic shock, inflammation, membrane compromise, alteration in ions and neurotransmitter levels
Secondary Injury: Biochemical cascade causing further damage.
Ongoing progressive damage that occurs after primary injury
Ischemia: activation of the ischemic cascade, Excessive Ca and ROS production, Apoptosis
Inflammation: Astrogliosis, lymphocyte infiltration of lesion, activated phagocytic monocytes
Excitotoxicity: Excessice Ca2+ leading to ROS production and oxidative stress, Excessive glumate, Apoptosis.
Effects of SCI:
Axonal injury: Some neurons may recover, others lead to paralysis.
Swelling: Can cause anoxia (oxygen deprivation).
Blood pressure drop: Interferes with neuron function.
Inflammatory response:
WBCs invade damaged area.
Neutrophils, T cells, macrophages, monocytes contribute to scar formation.
Excitotoxicity: Excessive glutamate release damages neurons.
Free radicals: Contribute to cell damage and degeneration.
Apoptosis: Leads to myelin loss and worsens function.
SCI Classification
Complete SCI
Total loss of motor & sensory function below injury level.
Incomplete SCI (some function preserved)
Central Cord Syndrome:
Result: cervical spinal injuries, greaater motor impairement in the upper body compared to lower body. variable sensory loss below the level of injury
Most common incomplete cervical injury.
Etiology
Hyperextension injury leading to central cord swelling.
Common in elderly individuals with cervical spine degeneration.
Clinical Manifestations (Symptoms):
Motor loss:
Greater weakness in arms than in legs.
Bladder dysfunction (may include urinary retention or incontinence).
Variable sensory loss (extent depends on severity of injury).
Anterior Cord Syndrome:
Result: below injury level, motor paralysis and loss of pain and temperature sensation. Preprioception (position sense) touch and vibratory sensation preserved
Etiology
Acute anterior compression of the spinal cord.
Common causes:
Bony fragments from vertebral fractures.
Acute disk herniation.
Clinical Manifestations (Symptoms):
Loss of:
Motor function (paresis or paralysis) below the injury level.
Pain sensation.
Temperature sensation.
Crude touch and pressure.
Preserved (intact) functions:
Proprioception (position sense).
Fine touch and pressure.
Vibration sensation.
Additional symptoms:
Urinary incontinence.
Posterior Cord Syndrome:
Result: Below injury level, motor fuction preserved, loss of sensory function, pressure, strech and preprioception.
Etiology
Acute compression of the posterior spinal cord.
Clinical Manifestations
Loss of:
Proprioception (body position awareness).
Fine touch and pressure.
Vibration sensation.
Intact (preserved) functions:
Pain sensation.
Temperature sensation.
Crude touch and pressure
Brown-Séquard Syndrome:
Result: below injury level, motor weakness and paralysis on one side of the body(heiparaplegia), loss of sensation on the opposite side (hemianesthesia)
Cause: Hemisection of spinal cord (gunshot, stabbing, ischemia, infection, hemorrhage).
Etiology
Hemisection (one-sided damage) of the spinal cord.
Common causes:
Penetrating injuries (gunshot, knife wounds).
Other causes: Primary ischemia, infection, hemorrhage.
Clinical manisfestation
Ipsilateral (same side as injury):
Loss of motor function (paralysis/paresis).
Loss of proprioception (body position awareness).
Loss of vibration sensation.
Contralateral (opposite side of injury):
Loss of pain sensation.
Loss of temperature sensation.
Clinical Manifestations
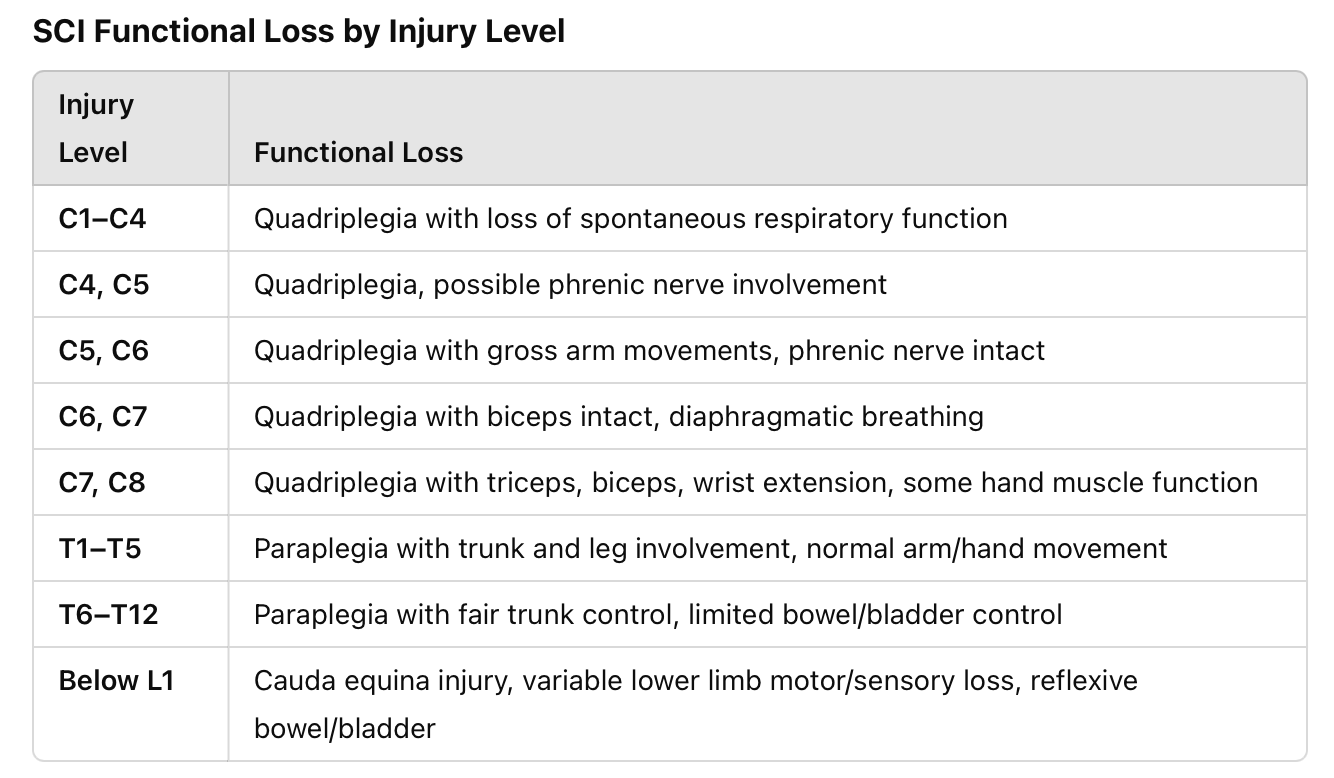
Level of injury predicts affected body functions:
Incomplete SCI, cause mixed manisfestation
Cervical (C1–C4): Can lead to quadriplegia, loss of respiratory function (C4 and above affect the phrenic nerve).
Above C3 total loss of respiratory function
C3- C5- respiratory insufficiency
Thoracic (T1–T12): Paraplegia, poor trunk control, variable bowel/bladder function.
injury above T6 leads to dysfuction of the SNS leads to neurogenic shock
Lumbar/Sacral (Below L1): Affects leg movement, bowel/bladder control, sexual function.
Other effects of SCI:
Chronic pain- Noiceptive or neuropathic pain
Low blood pressure.
Inability to sweat below injury level.
Decreased temperature regulation
GI: neurogenic bowel and bladder
Integumentary: Risk for skin breakdown
Thermoregulation- Poikilothermia
level of Injury
Diagnostic
SCI is a medical emergency
Initial steps:
If the patient is admitted with a suspected SCI (associated with trauma to the head or neck), the spine is immobilized (cervical collar, spine backboard)
Transfer to a specialized spine center for expert care.
Thorough neurological exam
•CT scan
Preferred study for location and degree of injury and degree of spinal canal compromise
it determines the location, severity, and extent of injury (e.g., hematomas, cord compression)
•MRI
Soft tissue injury
Guide decisions about surgery
X-rays
Hard to see C7 and T1
Identifies vertebral fractures or misalignments.
Medical management
SCI is irreversible once damage occurs.
Treatment focuses on airway, breathing, circulation, and preventing further injury.
Spinal shock monitoring is critical.
High cervical injuries (C3-C5) require immediate ventilatory support due to phrenic nerve involvement.
Maintain airway Patency
Maintain blood pressure
Spinal immobilization
Acute care
The loss of autoregulation and reduced sympathetic stimulation result in:
•Cardiac dysrhythmias
•Hypotension
•Decreased blood vessel tone
•Reduced cardiac output
Manage ABCs and vital signs
•Secure airway
•Keep SpO2 >92%
•MAP > 65mmHg
•SBP > 90mmHg
Drug therapy
•SCI disrupts autonomic regulation, leading to:
Bradycardia, hypotension, arrhythmias (esp. in T6 and above injuries).
Loss of vasomotor tone → blood pooling → hypotension.
Medications Used
IV Fluids: Crystalloids, colloids, blood products.
Vasopressors & Inotropes: Used if hypotension persists after fluids.
Dopamine, norepinephrine, epinephrine, vasopressin, dobutamine, phenylephrine.
Oral Midodrine & Desmopressin: Reduce IV vasopressor use.
Corticosteroids NOT routinely recommended due to risks (hyperglycemia, immunosuppression).
Nursing Considerations for Vasopressors
Continuous BP monitoring (arterial line recommended).
Large IV access (18G or central line) for administration.
Monitor for ischemia (cold/mottled extremities, low pulses).
Monitor fluid balance (risk of pulmonary edema).
Immobilization & Stabilization
Early spinal reduction & immobilization prevents complications.
Methods include:
•Maintain neck in neutral position
•Maintain traction at all times
Sternal-occipital-mandibular immobilizer brace
Halo vest
•Stable thoracic or lumbar spine injuries
Thoracolumbar sacral orthosis (TLSO)
Jewett brace
•Pin site care
•Effects of immobility
Halo traction device (cervical immobilization with external fixation).
Gardner-Wells tongs (skull traction for spinal alignment).
Surgery (decompression, fusion, laminectomy) if needed.
Surgical Management
Indications for surgery:
Spinal cord compression.
Progressive neurological deficits.
Penetrating injuries, fractures, or bony fragments.
Surgical options:
Decompression laminectomy (relieves pressure from edema).
Anterior/posterior fusion (stabilizes the spine with bone grafts or rods).
Decompression laminectomy
Spinal fusion
Management Focus
Early intervention, respiratory support, hemodynamic stabilization.
Prevent secondary injury & optimize recovery.
Complication
1. Spinal Shock
Occurs immediately after injury and can last days to week due to temporary loss of all spinal reflexes, loss of sensation, motor, and autonomic function below the injury, flaccid paralysis below level of injury.
Clinical Signs:
Flaccid paralysis
Loss of deep tendon reflexes
Urinary & fecal retention
Absence of sweating (anhidrosis)
Paralytic ileus
Duration: Can last from hours to weeks/months depending on reflex recovery.
2. Neurogenic Shock
A form of distributive shock seen in brain, cervical, and upper thoracic injuries.
Cause: Loss of sympathetic nervous system signals leads to vasodilation, bradycardia, and hypotension.
Occurs in cervical or high thoracic (at or above T6) injury; can last 1 to 3 weeks
Loss of SNS innervation causing unopposed parasympathetic response
Pheriperal vasodilation
venous pooling
decreased CO
Clinical Signs:
Severe hypotension less than 90mmHg
Bradycardia
Temperaturedysregulation
Treatment:
IV fluids, vasopressors (norepinephrine, dopamine)
Atropine for bradycardia
3. Autonomic Dysreflexia (AD)
Occurs in 48%-70% of SCI patients with injuries at or above T6.
Triggered by noxious stimuli (e.g., bladder distension or UTI, full bowel, infection, tight clothing, pressure injuries).
Mechanism:
Sympathetic surge → severe vasoconstriction → hypertension.
Brain attempts to lower BP but is blocked by spinal injury.
Parasympathetic system slows heart rate (bradycardia), but hypertension persists.
Clinical Signs:
Severe headache
Hypertension (20-40 mmHg above baseline)
Bradycardia or tachycardia
Flushing & sweating above injury, pallor below
Nasal congestion, blurred vision, chest pain
Potential Complications:
Seizures, MI, pulmonary edema, cerebral hemorrhage, death
Treatment:
Elevate head of bed (first intervention)
Identify & remove trigger (e.g., empty bladder, check for pressure injuries)
Administer antihypertensives if needed
4. Halo Brace/Traction Complications
Pin site infections (20% of cases)
Skin breakdown from prolonged pressure
Pin loosening or migration
Swallowing difficulty
Dural tears (potential CSF leaks)
Nursing Care:
Monitor pin sites for infection (redness, drainage, pain).
Clean pin sites with normal saline (no hydrogen peroxide).
Ensure proper alignment to prevent pressure ulcers.
Respiratory Dysfunction
Respiratory complications are the leading cause of acute and chronic morbidity and mortality in SCI
During first 48 hours after SCI, edema may increase the level of dysfunction and cause respiratory distress
Regular assessment
Maintain ventilation
Atelectasis, pneumonia, ARDS
•Vagal response unopposed
Cardiovascular Instability
Hypotension
Bradycardia
Decreased cardiac output
Impaired tissue perfusion
Orthostatic hypotension
VTE prophylaxis
Gastrointestinal
First 38 to 72 hours, GI tract may not function (paralytic ileus); requires NG tube
Nutrition should be started within 72 hours; patient in hypermetabolic state
Bowel management
Neurogenic bowel initially
Start bowel program to prevent constipation; allow 30 to 60 minutes
Daily rectal stimulant
suppository or small-volume enema
Adequate fluid and fiber intake
Increased activity and exercise
Bladder management
Immediately following SCI, urinary retention occurs from loss of autonomic and reflex control of bladder and sphincter; neurogenic bladder
Overdistention
Indwelling urinary catheter
CAUTI – prevention
Skin care
Pressure injury is the most common long-term complication
Prevention
Risk assessment
Daily comprehensive visual and tactile examination
Vulnerable areas:
sacrum, ischia, trochanters, and heels
check surgical incisions and skin under collars and braces
Assess nutritional status
Care positioning and repositioning every 2 hours
Specialty mattresses
 Knowt
Knowt