Module 4.3: Connective Tissue
Learning Outcomes
Compare and Contrast the roles of individual cell and fiber types within connective tissues
Identify the different types of connective tissue, and describe where in the body they are found
Describe the functions of each type of connective tissue, and correlate function with structure in each tissue type
Connective Tissue functions
Connecting and Binding:
Connects tissues to structures, like anchoring organs in place
Support:
Bone and cartilage support the weight of the body
Protection:
Bones provide protection for organs, fat and cartilage provide shock absorption, and many parts of the immune system are found within the connective tissues
Transport:
Blood is a fluid connective tissue that transports nutrients
Made up of loosely packed cells, surrounded by protein fibers, all within ground substance
Although diverse in function, all of their ECM plays an extensive role
Two classifications: Connective tissue proper, and specialized connective tissue
They differ in the types of cells and the components of the ECM
Connective Tissue Proper
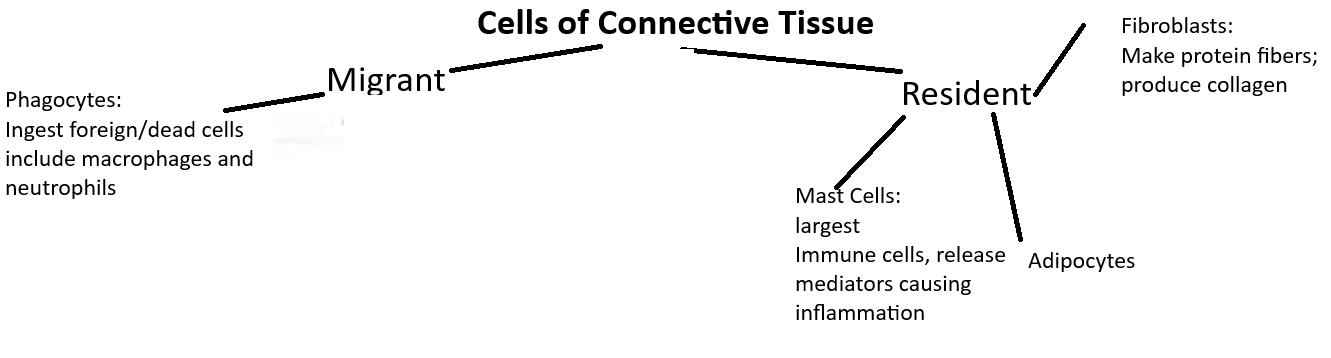
Resident cells inhabit a tissue permanently, while migrant cells go where ever their function is needed
Cells of Connective Tissues
Fibroblasts (-blast = immature)
Most common resident cell in connective tissue
Is a mature cell with properties of an immature cell
produce ground substance, protein fibers, and other elements of ECM
Are close to collagen fibers, as they produce collagen proteins
Adipocytes
The cytoplasm is most commonly dominated by a single large inclusion containing lipids
The nuclei and other organelles are pushed to the perimeter and hard to see
Mast Cells
Largest resident cell in connective tissue
Cells of the immune system that have cytosolic inclusions (or granules), containing inflammatory mediators (like histamine)
When stimulated, they release their granules and cause inflammation, signaling to activate the immune system and get more immune cells
Phagocytes
ingest foreign substances, microorganisms, and dead/damaged cells, by phagocytosis
2 types
macrophages: either resident or migrant cells in connective tissue
neutrophils: migrant immune cells
Other Immune Cells
Other cells migrate in and out of connective tissue based on their needs
Types of Connective Tissue Proper
Four basic types:
Loose Connective Tissue
Also known are areolar connective tissue
Mace mostly of ground substance
all protein fibers, fibroblasts, and adipocytes are suspended in it, thus allowing the ECM to be loose
Found to the epithelium of the skin, in the membranes lining body cavities, and layers the walls of hollow organs
Supports blood vessels allowing nutrients and oxygen to diffuse up
Houses many immune cells to protect, in case the epithelium is breached
Dense Connective Tissue
Composed primarily of protein fibers, hence why it is also called fibrous connective tissue, and ECM is coarse and tough
Grouped in 3 classes
Dense Irregular Connective tissue
Predominant fiber is collagen
Their disorganization makes them strong resistant to tension in all 3 planes
Found in organs subjected to high tension: Dermis, around organs and joints
Dense Regular Collagenous Connective Tissue
Thick collagen fiber bundles, arranged in one plane
They are very strong in that single plane but weak in others
found in tendons (unites bone to muscle), and ligaments (unites two bones)
Dense Regular Elastic Connective tissue
Often shorted to elastic tissue
Run parallel, much like the regular connective tissue
and orientated kind of wavy-ish
Elastic is thinner than collagen
Found in certain organs to stretch and lining of large blood vessels, like the aorta and certain ligaments like the spine
Reticular Tissue
Named because of the presence of many reticular fibers produced by surrounding fibroblasts
interweave to form “meshes” that support blood vessels and lymphatic vessels
Found in lymph nodes and spleen to trap foreign and old cells, and house white blood cells
forms a part of the basement membrane that supports the epithelia and structure of the liver and bone marrow
Adipose Tissue
Consists of adipocytes, fibroblasts an ECM
Though, initially, the collagen fibers may be predominant, the adipocytes can increase in size and outcompete the space used
They insulate, shock absorption, protection, and energy reserve
White adipose tissue consists of adipocytes with a single large lipid inclusion in their cytosol
They are found in the hypodermis (deep to the skin), on top of the dense superficial facia, this fat is also called subcutaneous fat
Found mainly in the abdomen, breast, hips, buttocks, and thighs, also surrounding the heart and abdominal organs (visceral fat)
Brown adipose tissue have multiple adipocytes and appear brown due to extensive mitochondria and blood supply. Oxidizes fatty acids 20 times faster
Specialized Connective Tissue
Three types: Cartilage, Bone or Osseous, and Blood
Cartilage
Found between joints, in ears, nose, and certain respiratory pathways
Its solid gel-like ECM, containing many glycosaminoglycans, proteoglycans, collagen fibers, and elastic fibers, allow to be tough and flexible
Contains two major cell types:
Chondroblasts
actively divide by mitosis and make most of the ECM of cartilage
As they are surrounded by their own ECM they eventually become inactive and mature chondrocytes
Chondrocytes
Eventually inhabit small cavities of the ECM called lacunae (lacuna = cavity)
Is essentially avascular, as almost no blood vessels are in it, thus oxygen and nutrients must diffuse through the outer sheath of dense irregular connective tissue called the perichondrium
Thus, this slow diffusion process limits thickness to only a few millimeters
Divided into 3 classes, based on composition of the ECM
Hyaline Cartilage (Hyaline = glass-like):
Most abundant
ECM has large amount of ground substance with a fine type of collagen fibers, thus giving them a bluish-gray glassy appearance
covers the end of bones where they form joints (articulations, so hyaline is also called articulate cartilage)
smooth, allowing for little friction between bones and distributes mechanical tension more equally
Is used where strong yet flexible cartilage is needed, like the connection of the sternum to the ribs, framing of the respiratory tract, and nose.
Fibrocartilage:
The ECM is dominated by collagen fibers, little room for ground substance
The collagen fibers are there because, in addition to the chondrocytes and chondroblasts, there are fibroblasts
have little elastic fibers
This composition gives great tensile strength, and some flexibility
Found in fibrous joints and intervertebral discs; also articular discs (allows two bones to fit better)
differs from the other two types of cartilage because, it lacks a perichondrium (outer sheath of dense irregular connective tissue that surrounds cartilage)
Elastic cartilage:
Limited to the external ear, and parts of the framework of the larynx
filled with elastic fibers, allowing it to vibrate to assist in the detection of sound and production of sound
Bone
35% of its mass consists of organic substances (collagen fibers, and a type of ground substance called osteoid)
65% is inorganic (calcium phosphate crystals)
Mature bone tissue contains 3 cell types:
Osteoblasts:
carry out bone deposition (synthesize the organic parts of the ECM, which is secreted by exocytosis, and produces chemicals for calcium salts to deposit within the ECM)
found on outer surface of the bone
near a dense irregular connective tissue covering (periosteum)
Osteocytes:
once osteoblasts are surrounded in the ECM they secrete, they reside in lacunae and become osteocytes (mature bone cells)
produce substances for bone maintenance
Osteoclasts (-clasia = broken):
large and multinucleated
carry out bone resorption
secrete hydrogen ions and enzymes to break down the parts of the ECM
Blood
ECM of blood is called plasma
consists largely of water, dissolved solutes, and proteins
does not have protein fibers, but smaller proteins to transport and aid in clotting
Contains cellular fragments called platelets to aid in clotting
two main types of blood cells:
Erythrocytes (erythro- = red)
Bind and transport oxygen
Leukocytes (leuko- = white)
Function in immunity