Psychopathology
Abnormality
There are four definitions for abnormality:
Statistical Infrequency
Deviation from Social Norms
Failure to Function Adequately
Deviation from Ideal Mental Health
Statistical Infrequency
Statistical Infrequency uses a normal distribution curve to define whether a person is abnormal through what is found at the extreme ends of the curve. Subsequently, normality is what statistically is most common. These stats need to be localised and up-to-date.
For example, IQ uses a normal distribution curve to define a range of normal IQ. The majority of people fall within 85-115 points with 100 set as the normal. A score below 70 is statistically infrequent with approximately 2% of individuals, therefore those who have less than 70 may receive a diagnosis of ‘intellectual disability disorder.’ The curve is symmetrical meaning it is statistically infrequent to have an IQ greater than 130.
Deviation from Social Norms
Social Norms are standards and expectations of behaviour set by social groups and society which define what is desirable and undesirable. Deviation from what is desirable is seen as abnormal because it may upset or offend those social group.
For example, homosexuality was classed as abnormal and seen as a mental disorder by societal standards before approximately 1980s. However, as societal norms change so did the definition of abnormality. Another example is antisocial personality disorder (psychopathy) as some people get offended by unsocial behaviour.
Failure to Function Adequately
Abnormality is judged as an inability to deal with the demands of everyday living. It considers mental state, motivation levels and obedience social norms. Behaviour is maladaptive, irrational or dangerous as it can cause personal distress and/or distress to others. The DSM-5 includes an assessment affability to function known as WHODAS to quantify functionality including understanding and communicating, self-care and life activities.
Some suggested features include:
Personal distress
Maladaptive behaviour
Unpredictability
Irrationality
Overt Discomfort
Violation of moral standards
Unconventionality
Deviation from Ideal Mental Health
Jahoda (1958) focused on defining normality, using a more positive approach compared to others, as opposed to abnormality. Her definition is “abnormality is the absence of criteria for good mental health.” This is similar to how physical health is defined.
Some suggested features include:
Self attitudes
Personal growth and self-actualisation
Integration
Autonomy
Accurate perception of reality
Environmental mastery
The more features a person fails to meet, the more abnormal they are.
Phobias
Top 5 phobias in the UK
Social Phobia: fear of interacting with other people
Agoraphobia: fear of open public spaces
Emetophobia: fear of vomiting
Erythrophobia: fear of blushing
Amaxophobia: fear of driving
A phobia is a persistent anxiety disorder, which interferes with daily living, and is irrational and/or disproportionate fear (emotional characteristic). Phobias are extreme fears triggered by an object, situation or an activity. The DSM recognises the following categories of phobia and related anxiety disorder:
Specific phobia: phobia of an object such as an animal or a situation such as flying.
Social anxiety (social phobia): phobia of a social situation such as public speaking.
Agoraphobia: phobia of being outside or in a public place.
Cognitive
Often a characteristic is selective attention to the phobic stimulus. For example, an inability to stop looking at dogs. This is a cognitive characteristic. The sufferer won’t be able to think rationally about the stimulus increasing the pressure on their reaction. The sufferer will not see reality, genuinely perceive something as bad in some way because of their phobia.
Behavioural
A sufferer may engage in endurance which is when they will remain in the presence of the phobic stimulus but will continue to experience a high level of anxiety. Others will avoid the stimulus disrupting their life in order to achieve this. Other behavioural characteristics include panic, crying, screaming, running away or freezing.
Emotional
Some emotional characteristics include anxiety, the sufferer may not experience positive emotion and may have a high state of unpleasant arousal. Fear occurs when the more unpleasant, direct and immediate form of anxiety, it is intense and short-lived.
Behavioural Approach: Phobias Explanation
Phobias are acquired through classical conditioning - they are learnt through association.
An unconditioned stimulus (UCS) elicits an unconditioned response (UCR).
A neutral stimulus (NS) is paired with an UCS resulting in a new stimulus-response link.
The neutral stimulus is now a conditioned stimulus (CS) producing a conditioned response (CR)
This conditioning may now be generalised to similar objects.
Example: Little Albert
Before Conditioning
UCS of a loud noise elicited a natural fear response (UCR). The NS was the rat which Albert loved and played with.
During Conditioning
The loud noise (UCS) was paired with the white rat (NS) resulting in the fear response (UCR).
After Conditioning (after learning)
The white rat became the CS and now elicits a CR of fear.
Extinction occurs when the conditioned stimulus is no longer paired with an unconditioned stimulus. This gradually weakens the conditioned response that results in the behaviour (phobia) decreasing or disappearing.
Stimulus generalisation is a tendency for the conditioned stimulus to evoke similar responses after the response has been conditioned. For example, Little Albert could generalise his phobia to white mice or other rats.
The two-process model
Mowrer (1947) proposed the two-process model to explain how phobias are learnt and maintained.
Acquisition by Classical Conditioning
Maintenance by Operant Conditioning (Negative Reinforcement)
Something Horrible (aversive)
Something Lovely (rewarding)
Adding/giving ‘Positive’
Positive Punishment
(Behaviour is weakened)
Positive Reinforcement
(Behaviour is strengthened)
Removing/taking ‘Negative’
Negative Reinforcement
(Behaviour is strengthened)
Negative Punishment
(Behaviour is weakened)
Evaluation
Research Evidence
Research evidence that individuals with phobias recall a specific incident, supporting classical conditioning
De Jongh et al (2006) - 73% of people with dental phobias had a traumatic (dental) experience.
Watson and Rayner (1920) - Little Albert showed classical conditioning
Öst (1987) - people may not remember the incident but there was a specific incident
Bregman (1934) - failed to condition a fear response pairing loud bell and wooden blocks
Incomplete Theory
Simple conditioning may be an inadequate explanation as the neutral stimulus can be paired with a fear response but elicit no phobia.
The diathesis-stress model suggests that one may inherit a genetic vulnerability to acquire a phobia which will be triggered by a life event.
Two-process model may be inadequate. Seligman (1971) suggested biological preparedness which suggests that there is an adaptive quality.
Avoidance may not be motivated by anxiety but positive feelings of safety.
Phobias may develop due to irrational thinking.
Bouton (2007) - pointed out evolututionary factors.
DiNardo (1990) - suggested that sufferers cannot remember having a related bad experience.
Real World Application
Certain phobias respond better to cognitive behaviour therapy (CBT) compared to behaviourist treatments.
Exposure therapy helps people with phobias
Behavioural Approach: Phobias Treatment
The aim is to replace a faulty association between conditioned stimulus and conditioned response in order to remove the phobic response. This is primarily done in one of two ways.
Gradual use of systematic desensitisation
Sudden use of flooding.
Systematic Desensitisation
Counterconditioning was developed by Wolpe (1958) in order to replace the fear with a harmful response, systematically and gradually desensitising the stimulus.
Anxiety Hierarchy: build a hierarchy of the stimuli including the degree of fear experience from 5 to 100.
Relaxation: Train the client in deep muscle relaxation techniques, such as meditation.
Reciprocal Inhibition: Client uses relaxation techniques to work through the hierarchy.
Exposure: Client confronts the real fear, and reaches the end of the hierarchy.
Flooding
Inescapable exposure to the feared stimuli until fear or anxiety disappears based on the suggestion that fear responses cannot be sustained. The suggestions states that the fear response will eventually fall (extinction), sometimes leading to a relaxed state.
Although this is not unethical per se, there are ethical concerns. Therefore it must be clearly explained and planned as it is an extremely unpleasant therapy technique.
Aversion Therapy
Another exposure therapy is aversion therapy which aims to associate undesirable behaviour with an unpleasant stimulus. More often used now as a therapy for addictive states. It classically conditions the state with a horrible feeling, for example smoking is laced with an emetic drug to induce nausea. However, aversion therapy stems from a controversial history - it was used in the 1950s to ‘cure’ homosexuality by electrically shocking men when looking at pictures of naked men. Other uses include alcoholism, drugs, and paedophilia.
Evaluation
Research evidence shows that SD is effective.
McGrath et al (1990): Found 75% of people with phobias were treated by Systematic Desensitisation especially in vivo (live) rather than in vitro (imagining).
Choy et al (2007): Found that people’s imaginations weren’t strong enough to use solely in SD. In vivo was more effective.
Real-World Application
Virtual reality treatment could work when exposure would be too dangerous (eg heights).
Research Evidence shows that flooding is effective.
Wolpe (1973): Flooding successfully helped a girl who was afraid of cars.
Öst (1989): Found flooding was 90% successful after one session and was maintained for 4 years.
It is more cost-effective than SD as the phobia could “cured” after one session.
Ethics
Although the technique is not unethical per se, Schumacher et al (2015) found that both therapists and clients felt flooding was significantly more stressful than other therapies.
Wolpe (1969): Found it was so traumatic it could lead to hospitalisation.
Furthermore, attrition (drop-out) rates were higher than SD.
Nomothetic vs Idiographic
Both treatments apply a nomothetic approach when there are many individual differences to consider, a idiographic approach may be better.
Depression
Depression is a mood disorder affecting emotional state. Depression is characterised by low mood and low energy levels.
All forms of depression and depressive disorders are characterised by changes to mood. The DSM recognises the following categories:
Major depressive disorder: severe but often short-term depression
Persistent depressive disorder: long-term or recurring depression including sustained major depression and what used to be called dysthymia
Disruptive mood dysregulation disorder: childhood temper tantrums
Premenstrual dysphoric disorder: disruption to mood prior to and/or during menstruation.
For a diagnosis, sufferers are required to display at least 5 symptoms every day for at least 2 weeks - including either sadness or loss of interest and pleasure in normal activities.
Depressed mood
Lack of interest or pleasure in all activity
Significant weight loss or gain
Insomnia
Psychomotor agitation (restlessness)
Loss of energy
Feelings of worthlessness
Diminished ability to think or concentrate
Recurrent thoughts of death
Behavioural
Activity levels are reduced. Social withdrawal, anhedonia (loss of enjoyment), apathy (avolition), lacking personal hygiene or more literally reduced movement/speech. Disruption of sleeping and eating. Insomnia, hypersomnia, eating too much or too little. Aggression or even self-harm which can be physical or verbal including irritability and rash decision.
Cognitive
Poor concentration leading to finding it hard to stick to a task, and decision-making is particularly difficult. This can interfere with work, school and general life. Attending to or even dwelling on the negative leading to a bias towards unhappiness. Absolutist thinking can occur. Believing everything is “black-and-white” “all-or-nothing,” and catastrophising is strongly linked with depression.
Emotional
Lowered mood is more pronounced than a typical low mood, including worthlessness feelings. Anger towards others or internally. This links to the behavioural aggression and irritability. Lowered self-esteem can even extend to self-loathing.
Cognitive Approach: Depression Explanation
A number of cognitive explanations of depression believe that the disorder is the result of disturbance in ‘thinking.’ These explanations focus on an individual’s negative thoughts, irrational beliefs and misinterpretation of events as being the cause of depression: negative or maladaptive biases in thinking leads to depression. There are two main “schools of thought” as to how faulty cognitions cause depression: one by Aaron Beck and the other by Ellis.
Aaron Beck (1967)
Beck proposed that some people are more vulnerable to depression due to their faulty cognitions creating an underlying vulnerability. He based his theory around three components:
Faulty information processing
Depressed people make fundamental errors in logic and tend to selectively attend to (pay attention to) the negative aspects of a situation ignoring the positive aspects. This then leads to black-or-white thinking. This includes dichotomous thinking (all-or-nothing), arbitrary inferences (drawing conclusions with no evidence), overgeneralisation (incorrect conclusions from little evidence), catasrophising (normal events are perceived as disasters), selective abstraction (ignoring features and paying attention to different features), excessive responsibility (taking blame for things).
Negative self-schemas
People who have become depressed often develop negative self-schemas interpreting all the information about themselves in a negative way. Sometimes these are acquired in childhood and if they do not go away as the person matures and nears adulthood, it can be a sign of depression. Events such as the loss of a parent, rejection by peers, criticism by parents and or teachers, physical or emotional abuse, may lead to negative schemas.
The Negative Triad
Beck built on the idea of maladaptive response and suggested that people with depression become trapped in a cycle of negative thoughts. The triad of impairments is the tendency to view themselves, the world, and the future in pessimistic ways.
Albert Ellis (1955)
Ellis proposed that good mental health is the result of rational thinking therefore bad mental health is the result of irrational thinking. Ellis argued that there are common irrational beliefs that underlie much depression, and sufferers have based their lives on these beliefs. Ellis suggested the ABC model:
A. an activating event causes
Example: A break up causes
B. an individual’s beliefs which result in
Example: thoughts of loneliness, worthlessness which may lead to
C. a consequence
Example: depression due to constant irrational beliefs.
Ellis coined the term “musturbatory thoughts/thinking” which implies the potentially addictive habit of absolutionist thinking, or unchecked use of verbs like ‘must’ or ‘should.’ These verbs make a person feel like they have a pressure to do something, applying more pressure of a societal duty or expectation. He also coined the term “utopianism” - the believing that life should be fair. This pressure of how life should be pressurises a person to challenge anything that is unfair leading to catasrophising of events.
Evaluation
Research Evidence
Grazioli and Terry (2000) assessed pregnant women for cognitive vulnerability and depressive illness before and following birth their child. It was found that women were more likely to suffer from post-natal depression if they had scored highly in cognitive vulnerability before birth.
Boury et al (2001) found depressives were more likely to negatively misinterpret information and feel hopeless.
Bates et al (1999) gave depressives with negative statements to read and found that their symptoms worsened. This supports the negative information processing/faulty information processing.
Counter Evidence
Alloy and Abrahmson (1979) suggested that individuals with depression may actually be “realists” and that normal individuals see the world through rose-tinted glasses - the ‘sadder but wiser effect.’
Zhang et al (2005) found that there is a gene for low serotonin that is ten times more likely to be found in those suffering from depression.
Biological Approach
Suggests that depression is a result of genetics and neurotransmitters levels which may underpin the disorder.
For example, certain genes are more common in people with depression and low levels of serotonin may be implicated in the disorder.
Zhang et al (2005)
Incomplete theory
It has been criticised for being overly simplistic in explaining a complex disorder. Often, individuals with depression experience extreme emotion such as anger and delusions and hallucinations.
This approach assumes that faulty thoughts underpin depressive illness. However, emotions may not always be influenced by thoughts. Faulty thinking may be a product of low mood.
It cannot explain reactive depression which is when the disorder follows an activating event such as bereavement. In these cases it is not due to faulty thinking.
RWA
Beck’s explanation forms the basis of CBT. Negative thinking can be challenged and corrected in CBT, providing support for negative self-schemas and the negative triad.
Ellis’s ABC model had led to effective therapy in the form of ABCDEF which is based of off REBT (Rational Emotive Behaviour Therapy). DEF challenges irrational beliefs and replaces them with more rational ways of thinking.
Free will vs Determinism
The cognitive approach suggests that the client has the power to change their depressive behaviour since they can change their irrational thought processes. It blames the client rather than situational factors which could aid recovery.
This is a free will outlook. The individual has free will to have those faulty thoughts therefore has the power to change them. Depression is their own fault but they also have the power to change it.
Determinism states that depression was meant to happen, depression was always destined to occur. On the other hand, this means that it was not their fault unlike free will.
This is a sensitive topic.
Cognitive Approach: Depression Treatment
There are two main ways for treating depression: Cognitive Behavioural Therapy (based on Beck’s explanation) and Rational Emotive Behavioural Therapy (based on Ellis’s explanation).
CBT
Based on both cognitive (how people think) and behavioural (what people do) techniques to change these processes to be more rational.
Recognising the thoughts and feelings are affected by what you do.
Challenging the negative triad through reality testing.
Focussing on the present instead of the negative view of the past and the negative thoughts of the future.
Behavioural Activation in which one challenges to do the activities they once avoided.
The sessions typically involve meeting with a therapist for between 5 and 20, weekly or fortnightly sessions lasting between 30 and 60 minutes. It starts with an assessment in which goals are identified to help treatment. These are monitored with the client having homework to complete for behavioural activation or reality testing. This is repeated until the treatment is completed.
REBT
This extends Ellis’s ABC model into the ABCDEF model.
A. Activating event causes
B. Beliefs
C. Consequence
D. Dispute
E. Effect
F. Feelings
The central technique of REBT is to identify and dispute the patient’s irrational thoughts. This is done by empirically, logically or pragmatically challenging the beliefs. Empirical arguments includes self-debating the beliefs that may not be consistent with reality. Logical arguments includes self-debating the beliefs that do not follow logically from the information available. Pragmatic arguments include emphasising the lack of usefulness of self-debating beliefs.
Ellis (1994) recognised the importance of giving the client respect and self-worth so adopted the traditional therapeutic idea of unconditional positive regard/unconditional love.
Evaluation
Research evidence vs Relapse
Ellis (1957) found that 90% of clients successfully treated depression after an average of 27 session.
Lewis and Lewis (2016) found that CBT was as effective as antidepressants paired with behavioural therapies for cases of bad depression.
Ali et al (2017) found that after over a year, half of the clients who used CBT relapsed.
CBT vs Drug therapy
March et al (2007) followed a group of 327 adolescents whom had a main diagnosis of depression. After 36 weeks the improvement rates showed that CBT was as effective. as antidepressants. The improvement rates for CBT and antidepressants were 81%.
In his third experimental group, the improvement rates were marginally higher when CBT was paired with drugs (86%)
Cuijpers et al (2013) found that CBT worked best when paired with antidepressants.
This highlights the importance of the biological approach in treating depression even though the cognitive approach is strong by itself.
Suitability
Taylor et al (2008) argued against Strumey saying CBT was effective for people with learning difficulties.
Strumey (2005) argued that talking therapies were not suitable for people with learning difficulties.
This suggests that CBT is not suitable for all cases of depression - reflected in March et el’s study - as those with serve depression may lack motivation to go to regular sessions.
Elkin et al (1985) found CBT to not be suitable for those with rigid beliefs that were not susceptible to change.
Simons et al (1995) CBT is also not suitable when external stressors affect the individual too much.
OCD
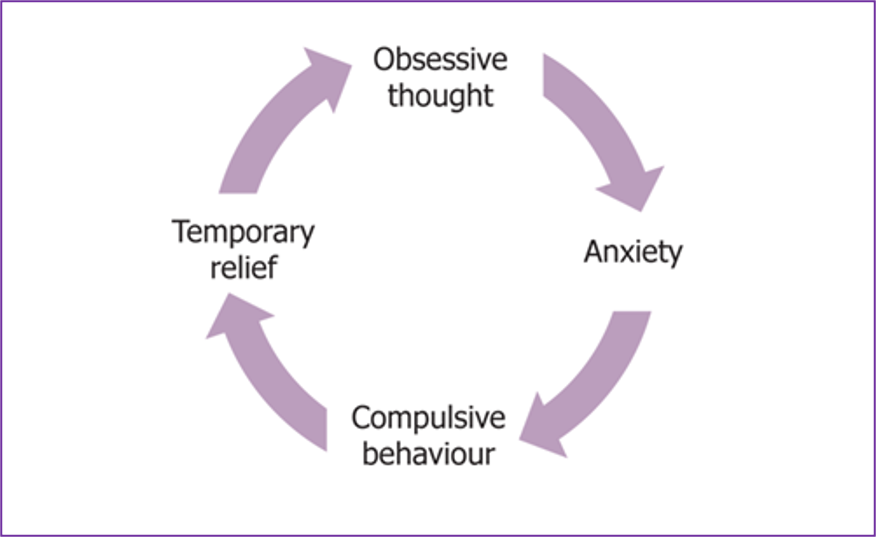
Obsessive Compulsive Disorder is characterised by obsessions and compulsions. It is associated with repetitive intrusive thoughts, and anxiety reducing behaviours. Only 2% of the population have OCD. Obsessions are persistent thoughts, ideas, impulses or images that are experienced repeatedly, they feel intrusive and cause anxiety. Compulsions are a repetitive and rigid behaviour or mental act that a person feels driven to perform in order to prevent or reduce anxiety.
DSM-5 Categories
Trichotillomania - compulsive hair-pulling
Hoarding Disorder - the compulsive gathering of possessions and the inability to part with anything, regardless of its value.
Excoriation Disorder - Compulsive skin-picking
Behavioural
Repetitive compulsions including tidying, ordering and washing, which make sufferers feel compelled to complete these in order to alleviate anxiety. 10% of sufferers only show compulsions; usually a direct response to the anxiety-inducing stimulus. Sufferers avoid the anxiety inducing stimulus, then they won’t have the need for the compulsions.
Cognitive
90% of sufferers have obsessive, recurrent thoughts, irrational beliefs or obsessions. To deal with this, sufferers often find coping strategies like praying or meditating. Sufferers have excessive anxiety insight - they are generally aware but still are hypervigilant/attentional bias.
Emotional
Anxiety and distress is caused because of the unpleasant, frightening thoughts with cause negative cognition. Depression often accompanies OCD. High comorbidity with depression which is eased by compulsions but return soon. Irrational personal guilt and disgust at self or at something is often experienced.
Biological Approach: OCD Explanation
Lewis (1936) made an observation that of his OCD patients, 37% had parents with OCD and 21% had siblings with OCD. This suggests there is a genetic explanation to OCD as the general population have a 2% prevalence of OCD.
Genetic Explanation
Neutrotransmitters are chemical messengers that transmit nerve impulses from one cell across the synapse to another cell. Serotonin, nicknamed the happy hormone, is a neurotransmitter which helps regulate mood. Lower levels of it are found in people with OCD. Dopamine is implicated in being frantically happy (link to gambling addiction). Higher levels of it are found in people with OCD.
SERT - Gene 5HT1-D beta/5HTT, better known as SERT, determines how serotonin is transported across the synapse. When it is faulty, less serotonin is transported causing mood (particularly relaxation) to become less regulated associated with OCD.
COMT - COMT (Catechol-O-methyltransferase) is a gene which helps regulate dopamine down. When it is faulty, dopamine is not under control meaning it becomes harder to regulate franticness to calmness, associated with OCD.
There are other genes which are implicated with OCD, OCD is likely to be attributed to serval genes (polygenic). This may explain the several types of the disorder making it aetiologically heterogenous - a number of different combinations of genes can lead to the same disorder. It is also suggested that each individual gene is likely to create a vulnerability which is then triggered by environmental stressors. The Diathesis-Stress Model.
Neural Explanations
Low levels of serotonin mean that normal neurotransmitters which relay information from one neuron to another about mood do not occur.
Abnormal obito-frontal cortex (OFC) - the OFC is linked with logical thinking and decision-making, it is nicknames ‘the worry circuit’ as it is particularly linked with the logical thinking of unpleasant emotions. When it is abnormal or faulty, these processes become impaired and may cause OCD.
Abnormal Basal Ganglia - the left parahippocampal gyrus, processes unpleasant emotions and regulates our ability to worry. When it is abnormal or faulty, this becomes impaired and may cause OCD, there is an inability to filter small worries such as bacteria leading to an overactive worry circuit.
Evaluation
Genetic Explanation
Research Evidence
Lewis (1936) showed OCD is correlated with genetics.
Samuels et al (2007) used gene mapping to compare OCD sufferers who exhibited compulsive hoarding with those who didn’t. It was found that there was a link to a specific chromosome
COUNTER
Nestadt et al (2010) showed 68% of monozygotic twins (identical) would share OCD and only 31% of dizygotic (fraternal). This suggests there are other factors to consider, otherwise if it was purely genetic MZ twins would both have OCD.
CRomer et al (2007) found that environmental factors have a massive impact on OCD - there is a correlation between past trauma and OCD. The more trauma the stronger the correlation.
Neural Explanation
Research Evidence
Saxena and Rauch (2000) reviewed studies of OCD that used PET, fMRI, and MRI neuro-imaging techniques to find consistent evidence of an association between the OFC and OCD symptoms.
Menzies et al (2007) found that OCD patients had less grey matter in MRI scans in areas of the brain OCD was linked to.
Comer et al (1998) found that these areas malfunction with low serotonin levels
Rauch et al (1994) found through PET scans over activation of the basal ganglia to be linked with OCD
COUNTER
Suket (2007) found that high dopamine levels lead to overactivity in the basal ganglia suggesting that the neural and genetic explanation are linked.
This is a correlational relationship - it is not definitive that the abnormalities caused OCD
Both
Incomplete theory - Albucher et al (1998) showed behavioural treatment for OCD was very effective (60 - 80% improvement)
Both explanations are reductionist and deterministic arguments - it takes a ‘nature’ viewpoint ignoring influence of ‘nurture’ and ignores the free will of the individual
Research shows correlation not causation
Biological Approach: OCD Treatment
Low levels of serotonin are associated with OCD therefore Selective Serotonin Re-uptake Inhibitors (SSRIs) are used to increase the levels of serotonin by blocking the re-uptake in pre-synaptic neuron. For example, prozac or fluoxetine. Drug therapy is often not used in isolation but combined with CBT to treat the condition. If a patient does not respond to SSRIs, tricyclics may be used, or SNRIs may be used.
Serotonin is released in the brain by presynaptic neurons
The serotonin diffuses across the synapse and binds to receptor sites on the post-synaptic neuron.
A new electrical impulse is started in the post-synaptic neuron.
Serotonin in the synapse is then reabsorbed into the pre-synaptic neuron to break down and recycle.
SSRIs block the reabsorption enabling more serotonin to be present in the synaptic cleft.
The levels of serotonin are increased in the synapse and the postsynaptic neuron continues to be stimulated.
This raises neural activity and compensates for the faulty serotonin system in a patient with OCD.
Antidepressants
The tricyclic (named after the molecular structure looking like three fused rings) Anafranil was the first antidepressant to be used followed by the Clomipramine. They work like SSRIs but have more side effects since they are not selective to serotonin. Selective noradrenaline re-uptake inhibitors work to block noradrenaline reuptake.
Anti-anxiety Drugs
Benzodiazapines (BZs) are commonly used to reduce anxiety by slowing down the central nervous system (CNS) using gamma-aminobutyric acid (GABA). This has a general quieting effect as when it locks onto receptors, it opens channels to increase the flow of chloride ions. Chloride ions make it harder for the neuron to be stimulated by other neurotransmitters.
Evaluation
Effectiveness
In studies comparing placebos and the drug, the drug is effective: Soomro et al (2008) reviewed 17 studies of the use of SSRIs with OCD patients and found them to be more effective than the placebos.
Koran et al (2007) suggested that CBT is more effective long term as it treats the cause and not the effects although drug therapies are effective in the short term
Drug therapy is not a lasting cure and it has been found that relapse is common. Maina et al (2001) found that patients often relapse fairly quickly after stopping drug treatments.
Preference
Health services prefer drugs as they are cheaper, they can be mass-produced and require little time from a doctor.
Little effort is required in taking drugs, it requires little monitoring and there is much less effort involved compared to other therapy techniques such as CBT
However, Koran et al in their review recommend that psychological treatments such as CBT should be tried first as this helps identify and treats the cause of OCD. Sufferers also benefit from talking to the GP about the symptoms and treatment
This is supported by Skapinakis et al (2016) who found that both cognitive and behavioural therapies such as exposure were better than SSRIs for OCD treatment.
Side-effects
Soomro et al (2008) stated that common side-effects of SSRIs include headaches, nausea and insomnia.
On the other hand, tricyclics tend to have more frequent side-effects including hallucinations and irregular heartbeat. Therefore these are only used when SSRIs are not effective.
Furthermore, side-effects of BZs can be aggression and long-term impairment of the memory. There are also problems with addiction so they should only be used for a limited time. Ashton (1997) recommended using BZs for 4 weeks maximum due to the side-effects.
Bias in results
Much research into drug therapies are funded by drug companies - supported by Goldacre (2013). Turner et al (2008) found there to be biases in antidepressant trials publications towards studies showing positive outcomes.
Selective publication like this can lead to doctors to make inappropriate treatment decisions.
16 Markers
Discuss FFA and DIMH as definitions of abnormality