Catheterization
Urinary Catheterization
The procedure involves inserting a sterile catheter into the bladder via the urethral opening to drain urine

Classification
Intermittent catheterization (single-lumen catheter) is used for:
Immediate relief of urinary retention
Long-term management of incompetent bladder
Obtaining a sterile urine specimen
Assessing residual urine in the bladder after voiding (if a bladder scanner is not available)
Indwelling catheterization (double- or triple-lumen catheter) is used for:
Promoting urinary elimination
Measuring accurate urine output
Preventing skin breakdown
Facilitating wound management
Allowing surgical repair of urethra, bladder, or surrounding structures
Instilling irrigation fluids or medications
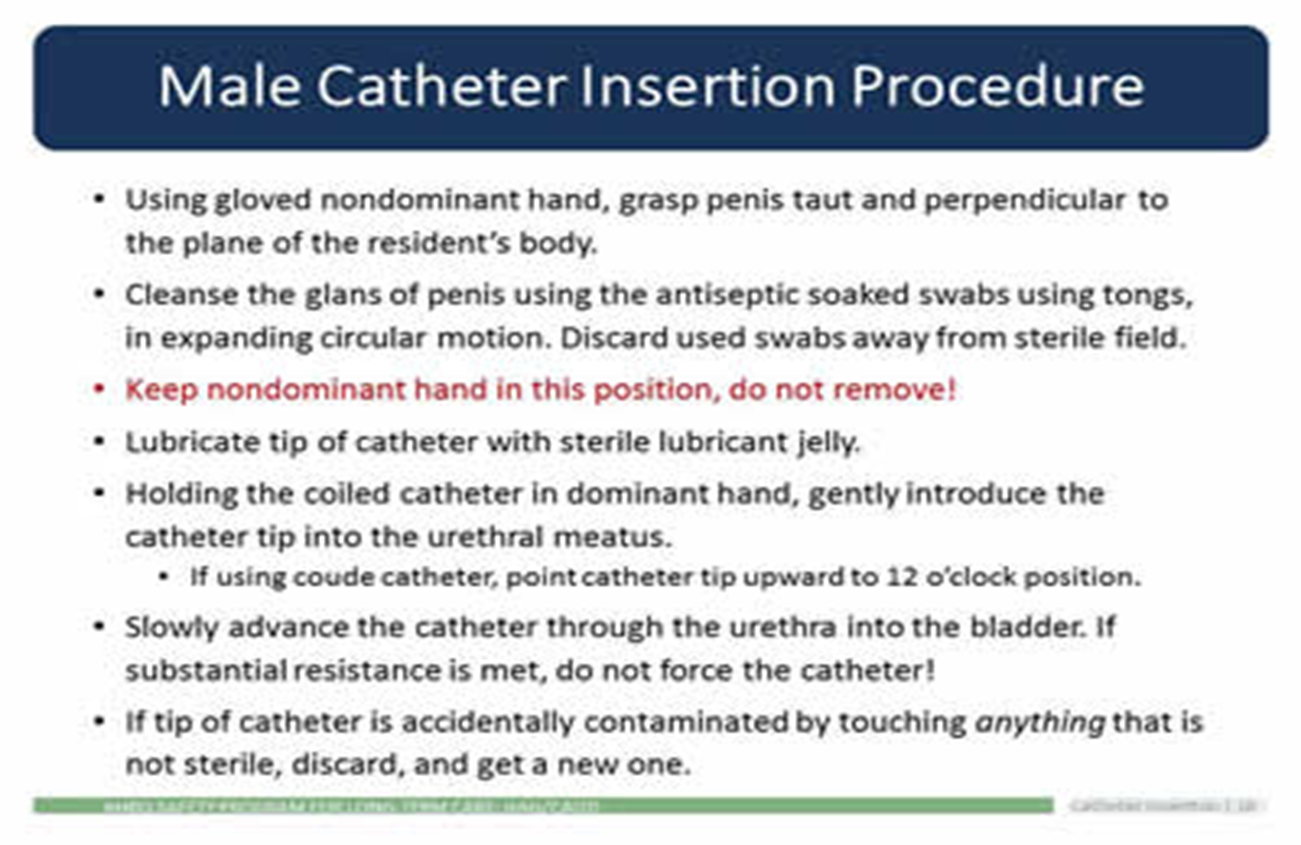
Assessing abdominal/pelvic pain
Investigating conditions of the genitourinary system
Urethral catheter types:
Straight tip
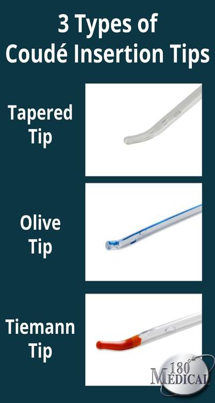
Coude (curved) tip
3-way catheter irrigation
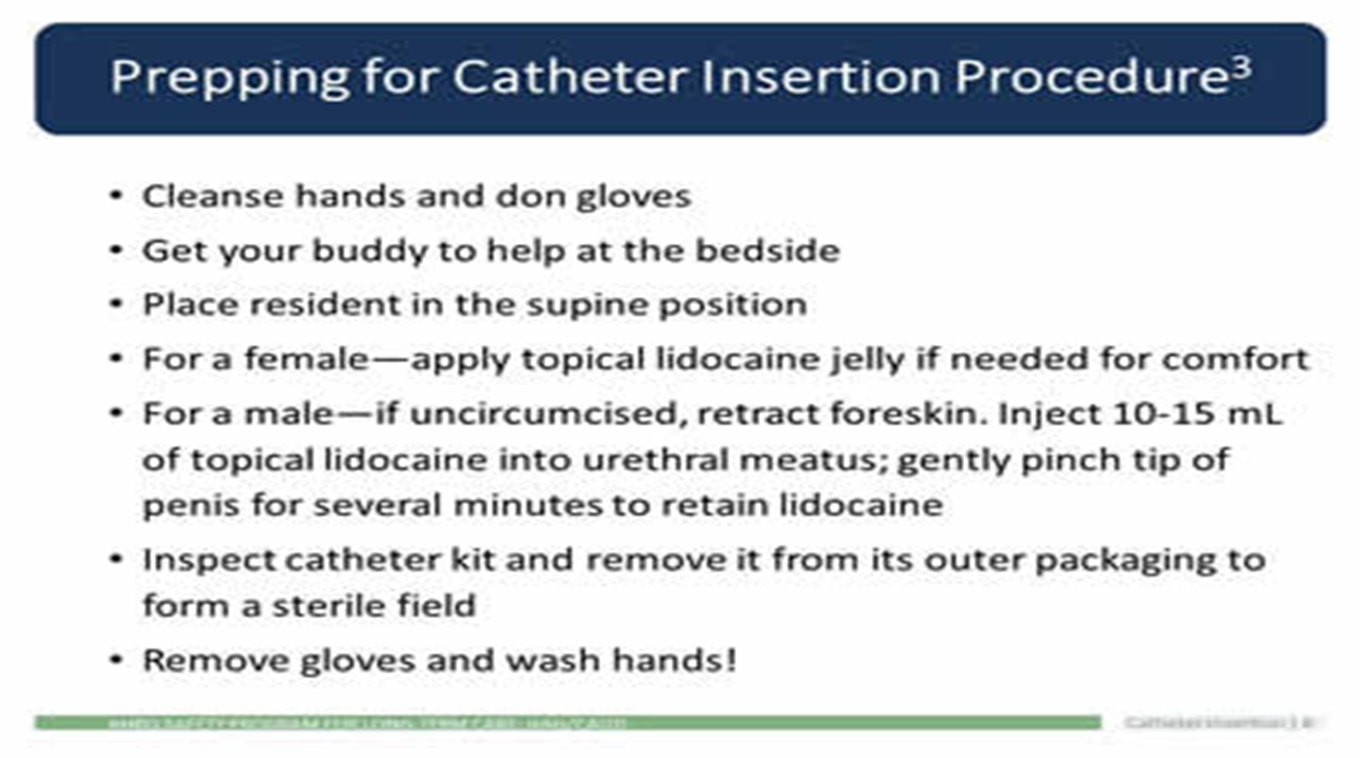
Guidelines for insertion
The meatus should be cleaned before the catheter is inserted, in accordance with local guidelines or policy (for example, with sterile normal saline)
An appropriate lubricant from a single-use container should be used during catheter insertion to minimize urethral trauma and infection.
Indication & Contraindications
Indication for inserting a urinary catheter:
To relieve acute urinary retention or bladder outlet obstruction
Sudden and complete inability to void.
Need for immediate and rapid bladder decompression.
Monitoring of intake and output
Contraindications for inserting a urinary catheter:
Blood at the meatus - Insertion of the catheter can worsen an underlying injury
Gross hematuria
Evidence of urethral infection
Urethral pain or discomfort
Low bladder volume/compliance
Patient refusal
Inability to define bladder location clinically via ultrasound
An empty bladder
Suspected pelvic or lower abdominal adhesions (e.g., after pelvic or lower abdominal surgery or radiation therapy
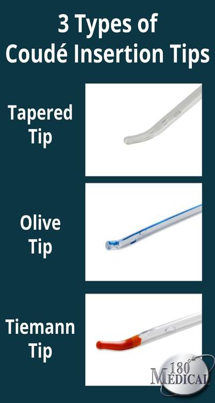
Coude (Curved) Catheter
Why Do I Need to Use Coudé Tips (curved tip)?
Standard straight tip catheters don’t work for everyone’s anatomy. Most of the time, this issue happens to men who need to use catheters
Possible causes:
Benign Prostatic Hyperplasia (BPH)
Prior prostate surgery
Urethral strictures
False passages in the urethra or a stoma
Radiation in the pelvic area to treat cancer
Females with an atrophic vagina
Those with urinary stricture disease or urethral trauma
Things to remember
Perform hand hygiene immediately before and after handling the catheter or drainage system, and use clean gloves while handling the catheter or drainage system
Perform peri-care using only soap and water or a similarly gentle cleaning agent
Keep the catheter and tubing from kinking and becoming obstructed
Signs that the catheter is blocked
There is urine leaking around the catheter
Check for and remove any kinks in the catheter or the drainage bag tubing. This could also indicate that your catheter is blocked.
Immediately request for replacement as the catheter may need to be changed
What is an urgent reason for catheterizing a patient?
A urinary catheter tube drains urine from your bladder.
You may need a catheter because of:
urinary incontinence (urine leakage)
urinary retention (not being able to urinate)
prostate problems, or
surgery that made it necessary
How often should you flush the tubing ?
Catheter flushes and bladder washouts can be carried out as required, or routinely (for example once or twice a day) to prevent a build-up of mucus within the bladder
Complications of urinary catheterization
Allergy or sensitivity to latex
Bladder stones
Blood infections (septicemia)
Blood in the urine (hematuria)
Kidney damage (usually only with long-term, indwelling catheter use)
Urethral injury
Urinary tract or kidney infections

Insertion of foley catheter
What is the female position for Foley catheter insertion?
Position female patient in a dorsal recumbent position (on back with knees flexed)
Ask them to relax thighs to accommodate hip rotation.
Drape female patient with a bath blanket
Position light to illuminate genitals or have assistant available to hold light source to visualize urinary meatus
Procedures and Rationale
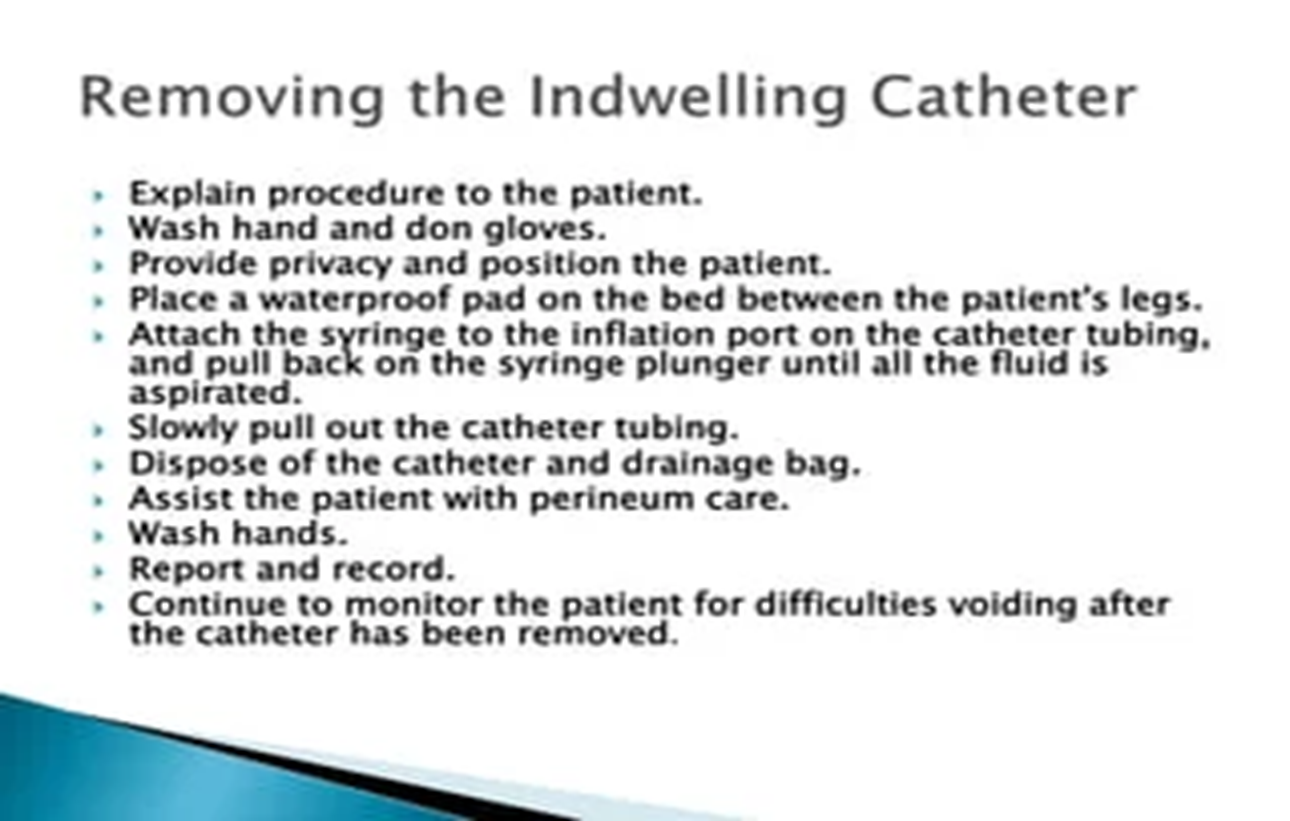
1. Verify physician order for catheter insertion. Assess for bladder fullness and pain by palpation or by using a bladder scanner
Palpation of a full bladder will cause an urge to void and/or pain.
2. Position patient prone to semi-upright with knees raised; apply gloves; and inspect perineal region for erythema, drainage, and odor. Also assess perineal anatomy.
Assessment of perineal area allows for determination of perineal condition and position of anatomical landmarks to assist with insertion.
3. Remove gloves and perform hand hygiene.
This prevents transmission of microorganism
4. Gather supplies:
Sterile gloves
Catheterization kit
Cleaning solution
Lubricant (if not in kit)
Prefilled syringe for balloon inflation as per catheter size
Urinary bag
Foley catheter
Preparation ahead of time enhances patient comfort and safety.
Prep sterile field
5. Check for size and type of catheter, and use smallest size of catheter possible
Larger catheter size increases the risk of urethral trauma
6. Place waterproof pad under patient.
This step prevents soiling of bed linen
Place waterproof pad under patient
7. Positioning of patient depends on gender.
Female patient: On back with knees flexed and thighs relaxed so that hips rotate to expose perineal area. Alternatively, if patient cannot abduct leg at the hip, patient can be side-lying with upper leg flexed at knee and hip, supported by pillows.
Male patient: Supine with legs extended and slightly apart.
Patient should be comfortable, with perineum or penis exposed, for ease and safety in completing procedure.
8. Place a blanket or sheet to cover patient and expose only required anatomical areas.
This step helps protect patient dignity.
9. Apply clean gloves and wash perineal area with warm water and soap or perineal cleanser according to agency policy.
Cleaning removes any secretions, urine, and feces, and reduces risk of CAUTION
10. Ensure adequate lighting.
Adequate lighting helps with accuracy and speed of catheter insertion.
11. Perform hand hygiene.
This reduces the transmission of microorganisms.
12. Add supplies and cleaning solution to catheterization kit, and according to agency policy.
This step ensures preparation and organization for procedure.
13. If using indwelling catheter and closed drainage system, attach urinary bag to the bed and ensure that the clamp is closed.
Urinary bag should be closed to prevent urine drainage leaving bag.
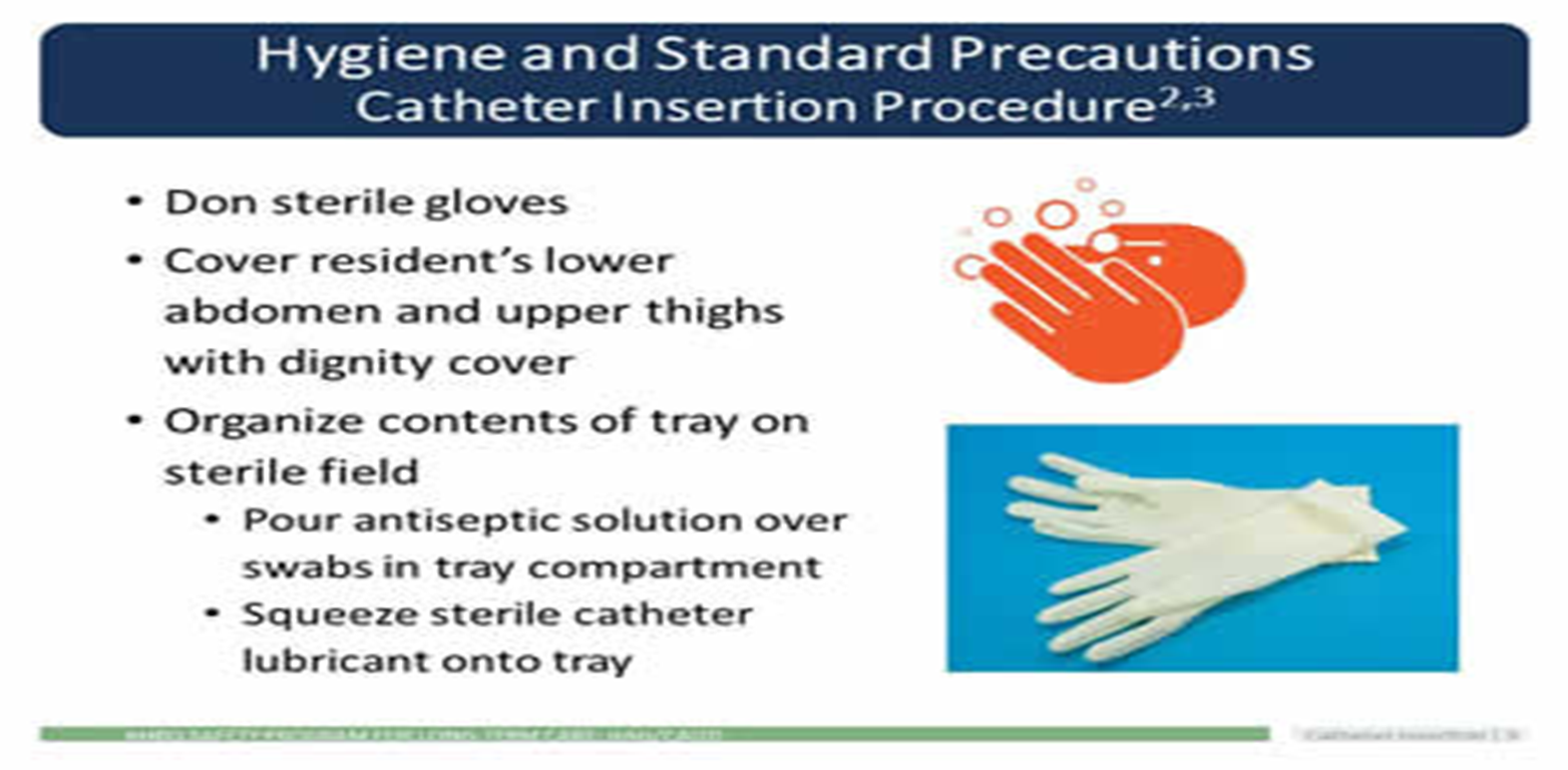
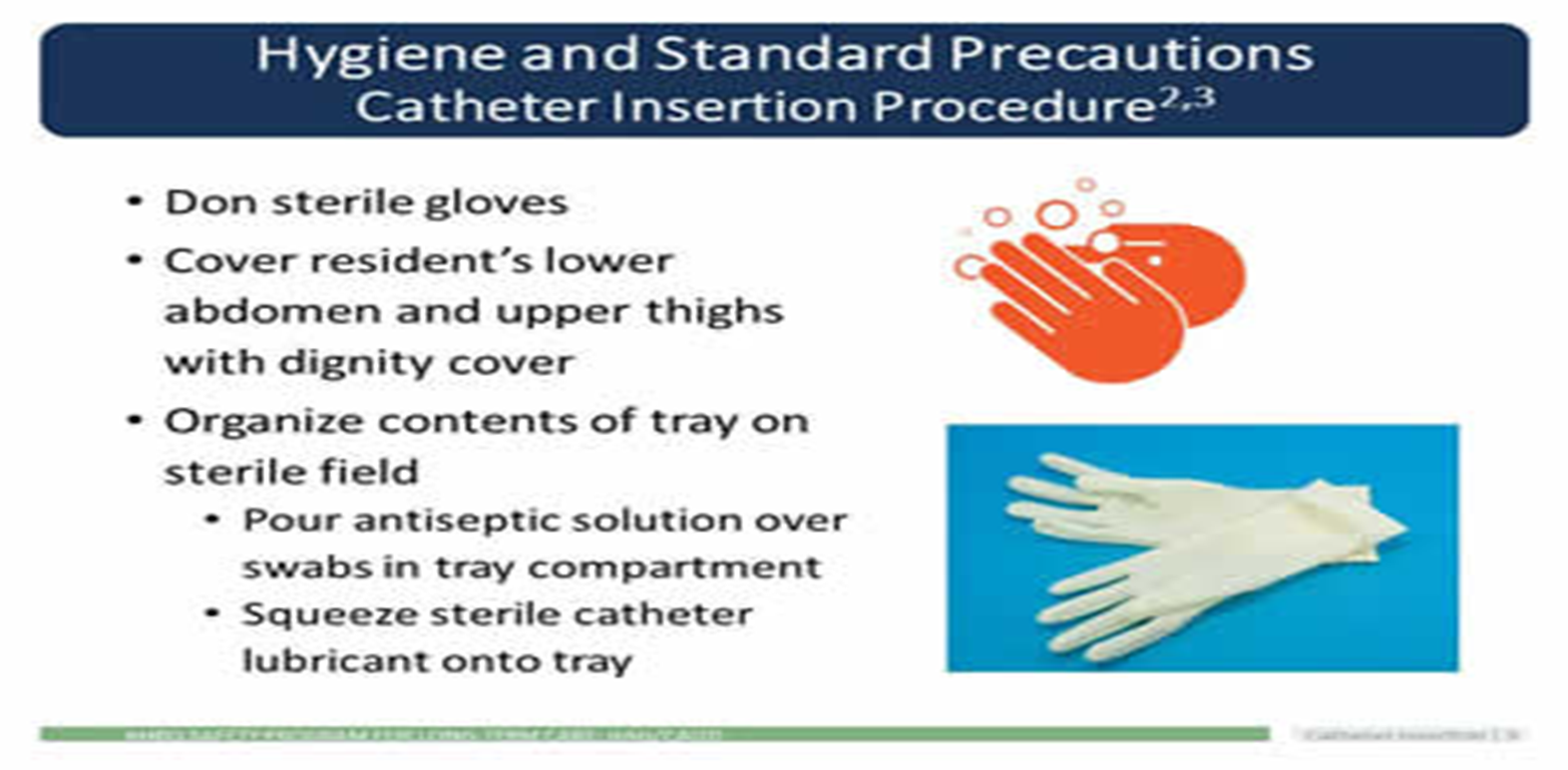
14. Apply sterile gloves using sterile technique.
This reduces the transmission of microorganisms.
15. Drape patient with drape found in catheterization kit, either using sterile gloves or using ungloved hands and only touching the outer edges of the drape.
Ensure that any sterile supplies touch only the middle of the sterile drape (not the edges), and that sterile gloves do not touch non-sterile surfaces. Drape patient to expose perineum or penis.
The outer 2.5 cm is considered non-sterile on a sterile drape.
Cover pt w sterile drape
16. Lubricate tip of catheter using sterile lubricant included in tray, or add lubricant using sterile technique.
Lubrication minimizes urethral trauma and discomfort during procedure.
17. Check balloon inflation using a sterile syringe.
This maintains sterility of catheter.
18. Place sterile tray with catheter between patient’s legs.
Sterile tray will collect urine once catheter tip is inserted into bladder.
19. Clean perineal area as follows.
Female patient: Separate labia w/ fingers of non-dominant hand (now contaminated and no longer sterile). Using sterile technique and dominant hand, clean labia and urethral meatus from clitoris to anus, and from outside labia to inner labial folds and urethral meatus. Use sterile forceps and a new cotton swab with each cleansing stroke.
This reduces the transmission of microorganisms.
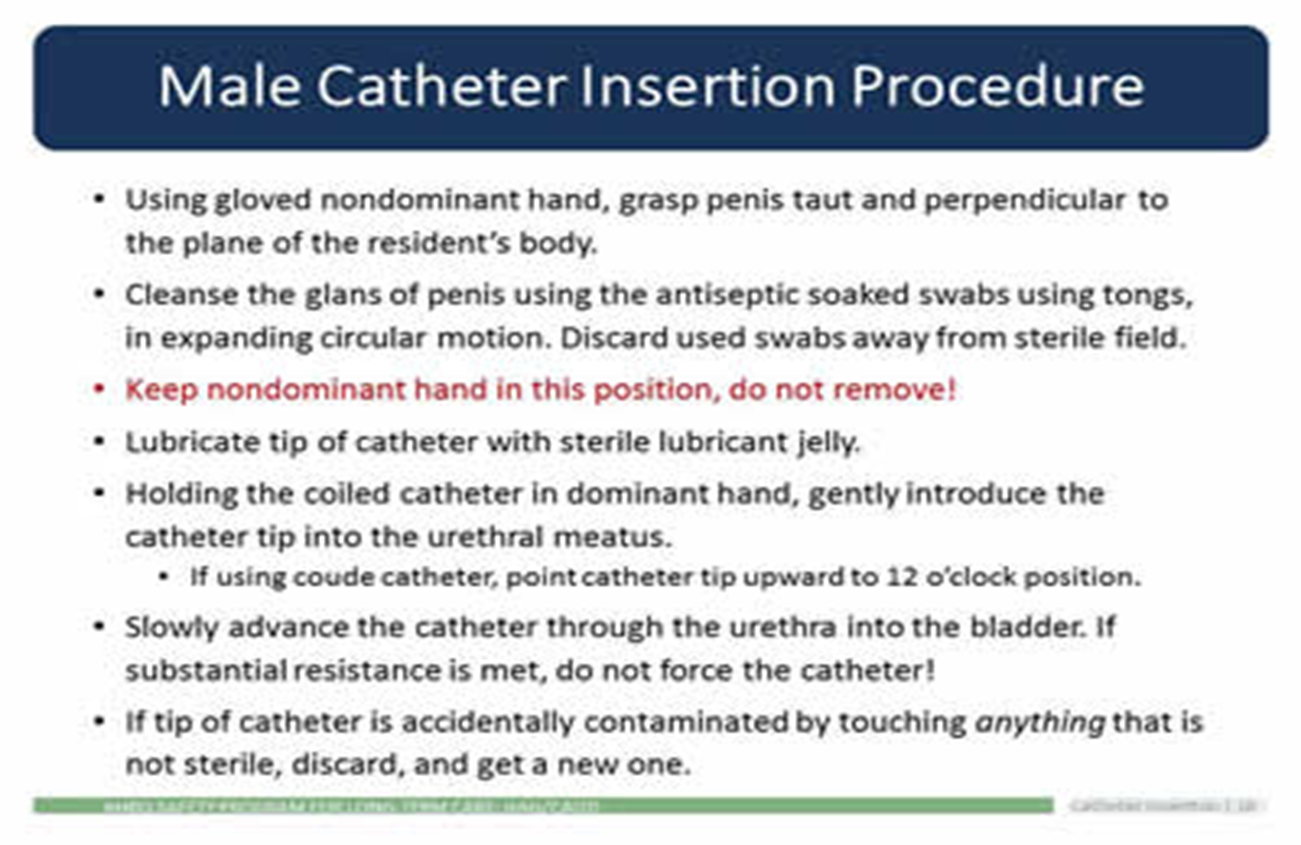
Male patient: Gently grasp penis at shaft and hold it at right angle to the body throughout procedure with non-dominant hand (now contaminated and no longer sterile). Using sterile technique and dominant hand, clean urethral meatus in a circular motion working outward from meatus. Use sterile forceps and a new cotton swab with each cleansing stroke.
20. Pick up catheter with sterile dominant hand 7.5 to 10 cm below the tip of the catheter.
21. Insert catheter as follows.
Female patient:
Ask patient to bear down gently (as if to void) to help expose urethral meatus.
Advance catheter 5 to 7.5 cm until urine flows from catheter, then advance an additional 5 cm.
Male patient:
Hold penis perpendicular to body & pull up slightly on shaft
Ask patient to bear down gently (as if to void) and slowly insert catheter through urethral meatus.
Advance catheter 17 to 22.5 cm or until urine flows from catheter
Holding catheter closer to the tip will help to control and manipulate catheter during insertion.
Maintenance care of foley catheter
Use standard precautions before contact with catheter, tubing, or bag.
When performing peri-care use only soap and water
Periurethral area should NOT be cleaned vigorously or with antiseptic solutions.
Keep the catheter and all tubing from kinking/obstruction.
Indwelling urinary catheter and suprapubic catheter systems must be kept CLOSED
If any disconnection of tubing or bag leakage, replace it.
Make sure you don't contaminate catheter outlet valve when emptying the collection bag.
Nurses are daily hands on the "front line" between residents and families, and potential infection-causing microbes
Remember:
Wash hands BEFORE and AFTER contact with catheter, tubing, or bag.
Keep bag below bladder at all times without kinking.
When emptying bag, do not let outlet port touch ANYTHING
Drain into a container used only for ONE resident.
Sampling port must be DISINFECTED before any use
Only STERILE needle/syringe can be used to aspirate urine
Only trained staff should empty the urine bag and rinse/store containers.
Empty drainage bags regularly (at least once per shift).
Stabilize the catheter and drainage bag.
Keep drainage bag below level of bladder at all times OFF floor.
Stabilize urine drainage bag properly
Wheelchair
Walker (clamp or hook)
Bed
Dining/activity area when the patient needs to eat or move as allowed
Catheterization
Urinary Catheterization
The procedure involves inserting a sterile catheter into the bladder via the urethral opening to drain urine

Classification
Intermittent catheterization (single-lumen catheter) is used for:
Immediate relief of urinary retention
Long-term management of incompetent bladder
Obtaining a sterile urine specimen
Assessing residual urine in the bladder after voiding (if a bladder scanner is not available)
Indwelling catheterization (double- or triple-lumen catheter) is used for:
Promoting urinary elimination
Measuring accurate urine output
Preventing skin breakdown
Facilitating wound management
Allowing surgical repair of urethra, bladder, or surrounding structures
Instilling irrigation fluids or medications
Assessing abdominal/pelvic pain
Investigating conditions of the genitourinary system
Urethral catheter types:
Straight tip
Coude (curved) tip
3-way catheter irrigation
Guidelines for insertion
The meatus should be cleaned before the catheter is inserted, in accordance with local guidelines or policy (for example, with sterile normal saline)
An appropriate lubricant from a single-use container should be used during catheter insertion to minimize urethral trauma and infection.
Indication & Contraindications
Indication for inserting a urinary catheter:
To relieve acute urinary retention or bladder outlet obstruction
Sudden and complete inability to void.
Need for immediate and rapid bladder decompression.
Monitoring of intake and output
Contraindications for inserting a urinary catheter:
Blood at the meatus - Insertion of the catheter can worsen an underlying injury
Gross hematuria
Evidence of urethral infection
Urethral pain or discomfort
Low bladder volume/compliance
Patient refusal
Inability to define bladder location clinically via ultrasound
An empty bladder
Suspected pelvic or lower abdominal adhesions (e.g., after pelvic or lower abdominal surgery or radiation therapy
Coude (Curved) Catheter
Why Do I Need to Use Coudé Tips (curved tip)?
Standard straight tip catheters don’t work for everyone’s anatomy. Most of the time, this issue happens to men who need to use catheters
Possible causes:
Benign Prostatic Hyperplasia (BPH)
Prior prostate surgery
Urethral strictures
False passages in the urethra or a stoma
Radiation in the pelvic area to treat cancer
Females with an atrophic vagina
Those with urinary stricture disease or urethral trauma
Things to remember
Perform hand hygiene immediately before and after handling the catheter or drainage system, and use clean gloves while handling the catheter or drainage system
Perform peri-care using only soap and water or a similarly gentle cleaning agent
Keep the catheter and tubing from kinking and becoming obstructed
Signs that the catheter is blocked
There is urine leaking around the catheter
Check for and remove any kinks in the catheter or the drainage bag tubing. This could also indicate that your catheter is blocked.
Immediately request for replacement as the catheter may need to be changed
What is an urgent reason for catheterizing a patient?
A urinary catheter tube drains urine from your bladder.
You may need a catheter because of:
urinary incontinence (urine leakage)
urinary retention (not being able to urinate)
prostate problems, or
surgery that made it necessary
How often should you flush the tubing ?
Catheter flushes and bladder washouts can be carried out as required, or routinely (for example once or twice a day) to prevent a build-up of mucus within the bladder
Complications of urinary catheterization
Allergy or sensitivity to latex
Bladder stones
Blood infections (septicemia)
Blood in the urine (hematuria)
Kidney damage (usually only with long-term, indwelling catheter use)
Urethral injury
Urinary tract or kidney infections

Insertion of foley catheter
What is the female position for Foley catheter insertion?
Position female patient in a dorsal recumbent position (on back with knees flexed)
Ask them to relax thighs to accommodate hip rotation.
Drape female patient with a bath blanket
Position light to illuminate genitals or have assistant available to hold light source to visualize urinary meatus
Procedures and Rationale
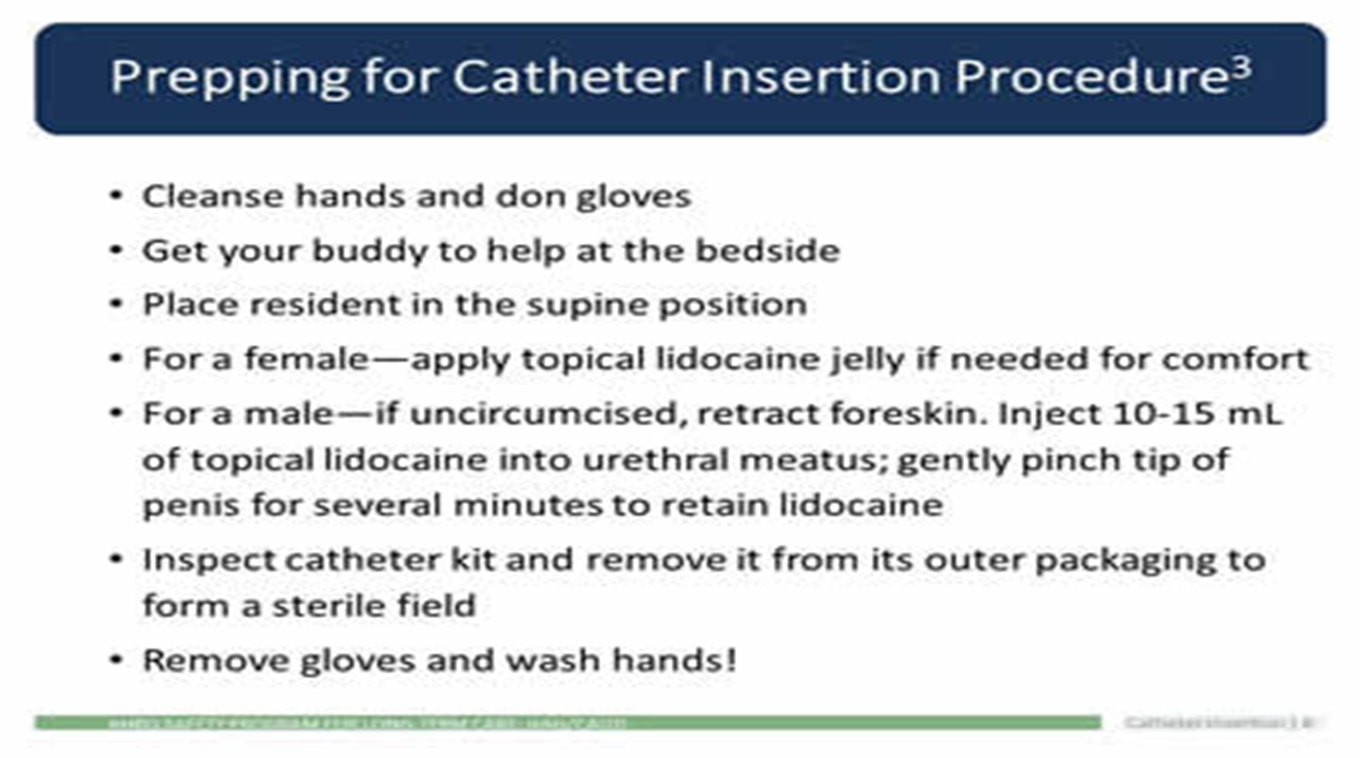
1. Verify physician order for catheter insertion. Assess for bladder fullness and pain by palpation or by using a bladder scanner
Palpation of a full bladder will cause an urge to void and/or pain.
2. Position patient prone to semi-upright with knees raised; apply gloves; and inspect perineal region for erythema, drainage, and odor. Also assess perineal anatomy.
Assessment of perineal area allows for determination of perineal condition and position of anatomical landmarks to assist with insertion.
3. Remove gloves and perform hand hygiene.
This prevents transmission of microorganism
4. Gather supplies:
Sterile gloves
Catheterization kit
Cleaning solution
Lubricant (if not in kit)
Prefilled syringe for balloon inflation as per catheter size
Urinary bag
Foley catheter
Preparation ahead of time enhances patient comfort and safety.
Prep sterile field
5. Check for size and type of catheter, and use smallest size of catheter possible
Larger catheter size increases the risk of urethral trauma
6. Place waterproof pad under patient.
This step prevents soiling of bed linen
Place waterproof pad under patient
7. Positioning of patient depends on gender.
Female patient: On back with knees flexed and thighs relaxed so that hips rotate to expose perineal area. Alternatively, if patient cannot abduct leg at the hip, patient can be side-lying with upper leg flexed at knee and hip, supported by pillows.
Male patient: Supine with legs extended and slightly apart.
Patient should be comfortable, with perineum or penis exposed, for ease and safety in completing procedure.
8. Place a blanket or sheet to cover patient and expose only required anatomical areas.
This step helps protect patient dignity.
9. Apply clean gloves and wash perineal area with warm water and soap or perineal cleanser according to agency policy.
Cleaning removes any secretions, urine, and feces, and reduces risk of CAUTION
10. Ensure adequate lighting.
Adequate lighting helps with accuracy and speed of catheter insertion.
11. Perform hand hygiene.
This reduces the transmission of microorganisms.
12. Add supplies and cleaning solution to catheterization kit, and according to agency policy.
This step ensures preparation and organization for procedure.
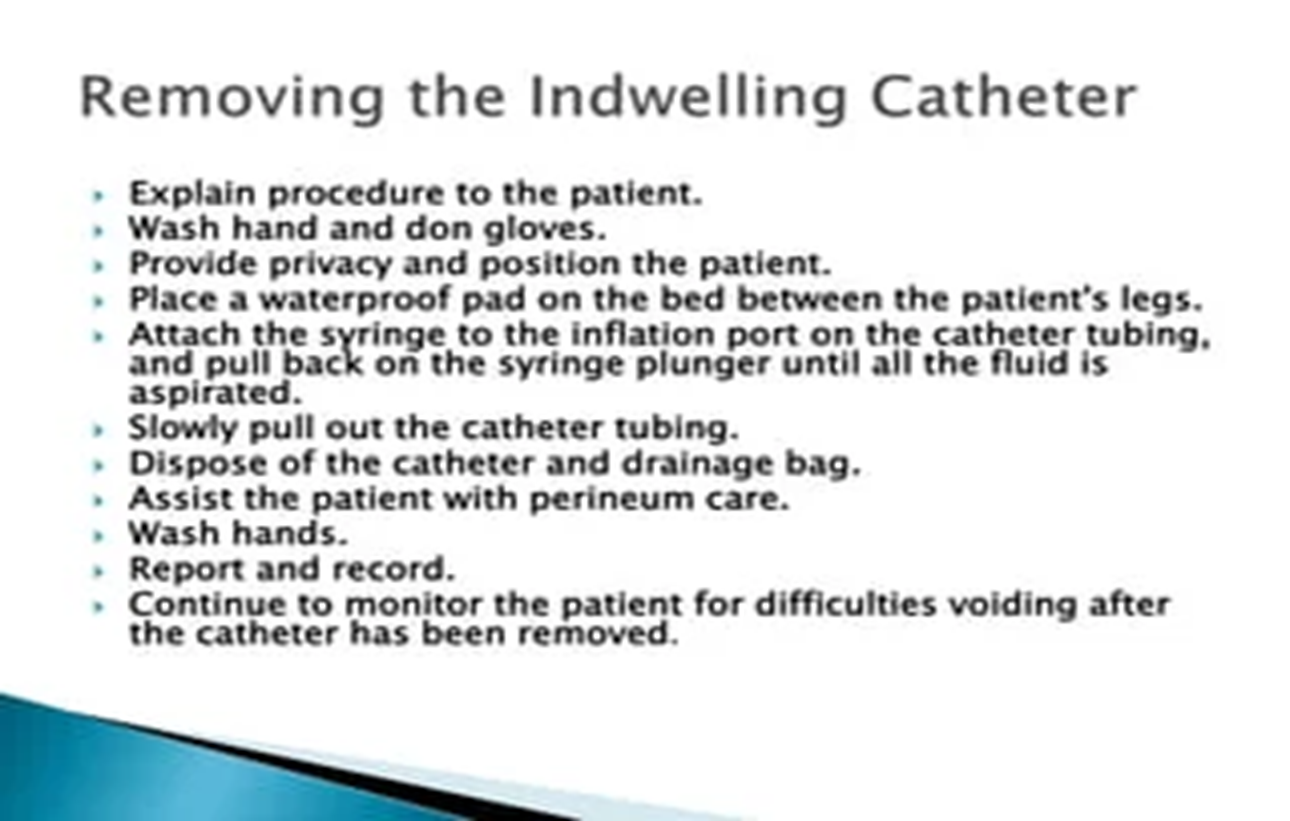
13. If using indwelling catheter and closed drainage system, attach urinary bag to the bed and ensure that the clamp is closed.
Urinary bag should be closed to prevent urine drainage leaving bag.
14. Apply sterile gloves using sterile technique.
This reduces the transmission of microorganisms.
15. Drape patient with drape found in catheterization kit, either using sterile gloves or using ungloved hands and only touching the outer edges of the drape.
Ensure that any sterile supplies touch only the middle of the sterile drape (not the edges), and that sterile gloves do not touch non-sterile surfaces. Drape patient to expose perineum or penis.
The outer 2.5 cm is considered non-sterile on a sterile drape.
Cover pt w sterile drape
16. Lubricate tip of catheter using sterile lubricant included in tray, or add lubricant using sterile technique.
Lubrication minimizes urethral trauma and discomfort during procedure.
17. Check balloon inflation using a sterile syringe.
This maintains sterility of catheter.
18. Place sterile tray with catheter between patient’s legs.
Sterile tray will collect urine once catheter tip is inserted into bladder.
19. Clean perineal area as follows.
Female patient: Separate labia w/ fingers of non-dominant hand (now contaminated and no longer sterile). Using sterile technique and dominant hand, clean labia and urethral meatus from clitoris to anus, and from outside labia to inner labial folds and urethral meatus. Use sterile forceps and a new cotton swab with each cleansing stroke.
This reduces the transmission of microorganisms.
Male patient: Gently grasp penis at shaft and hold it at right angle to the body throughout procedure with non-dominant hand (now contaminated and no longer sterile). Using sterile technique and dominant hand, clean urethral meatus in a circular motion working outward from meatus. Use sterile forceps and a new cotton swab with each cleansing stroke.
20. Pick up catheter with sterile dominant hand 7.5 to 10 cm below the tip of the catheter.
21. Insert catheter as follows.
Female patient:
Ask patient to bear down gently (as if to void) to help expose urethral meatus.
Advance catheter 5 to 7.5 cm until urine flows from catheter, then advance an additional 5 cm.
Male patient:
Hold penis perpendicular to body & pull up slightly on shaft
Ask patient to bear down gently (as if to void) and slowly insert catheter through urethral meatus.
Advance catheter 17 to 22.5 cm or until urine flows from catheter
Holding catheter closer to the tip will help to control and manipulate catheter during insertion.
Maintenance care of foley catheter
Use standard precautions before contact with catheter, tubing, or bag.
When performing peri-care use only soap and water
Periurethral area should NOT be cleaned vigorously or with antiseptic solutions.
Keep the catheter and all tubing from kinking/obstruction.
Indwelling urinary catheter and suprapubic catheter systems must be kept CLOSED
If any disconnection of tubing or bag leakage, replace it.
Make sure you don't contaminate catheter outlet valve when emptying the collection bag.
Nurses are daily hands on the "front line" between residents and families, and potential infection-causing microbes
Remember:
Wash hands BEFORE and AFTER contact with catheter, tubing, or bag.
Keep bag below bladder at all times without kinking.
When emptying bag, do not let outlet port touch ANYTHING
Drain into a container used only for ONE resident.
Sampling port must be DISINFECTED before any use
Only STERILE needle/syringe can be used to aspirate urine
Only trained staff should empty the urine bag and rinse/store containers.
Empty drainage bags regularly (at least once per shift).
Stabilize the catheter and drainage bag.
Keep drainage bag below level of bladder at all times OFF floor.
Stabilize urine drainage bag properly
Wheelchair
Walker (clamp or hook)
Bed
Dining/activity area when the patient needs to eat or move as allowed