Week 3 Pharm - Recreational Drugs
Week 3: Pharm: Recreational Drugs
Alcohol and Its Misuse
The most commonly used and abused psychoactive agent in the United States
Some therapeutic use
Primarily used for non-medical purposes
Moderate consumption: Prolongs life and reduces risk of dementia and cardiovascular disorders
Excessive consumption: Diminishes quality and quantity of life
There is a lot of controversy around benefits of alcohol (red wine is good for you)
Basic Pharmacology of Alcohol
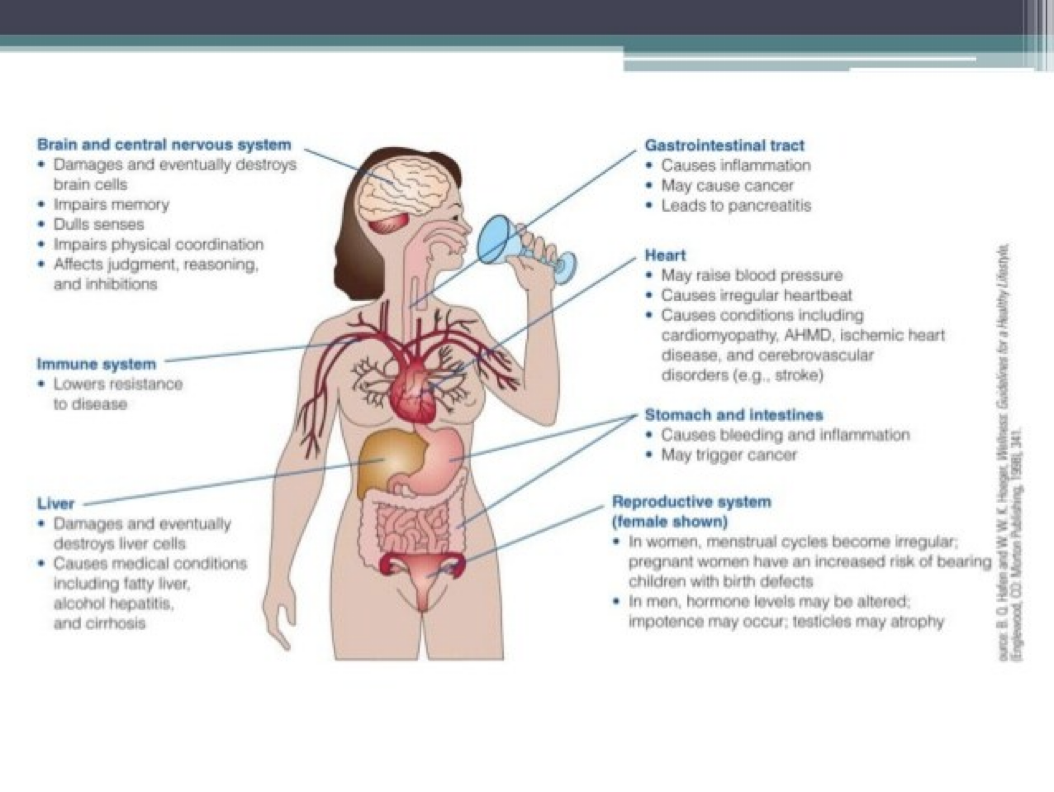
Central Nervous System (CNS) Effects
Acute effects
General depression of CNS function
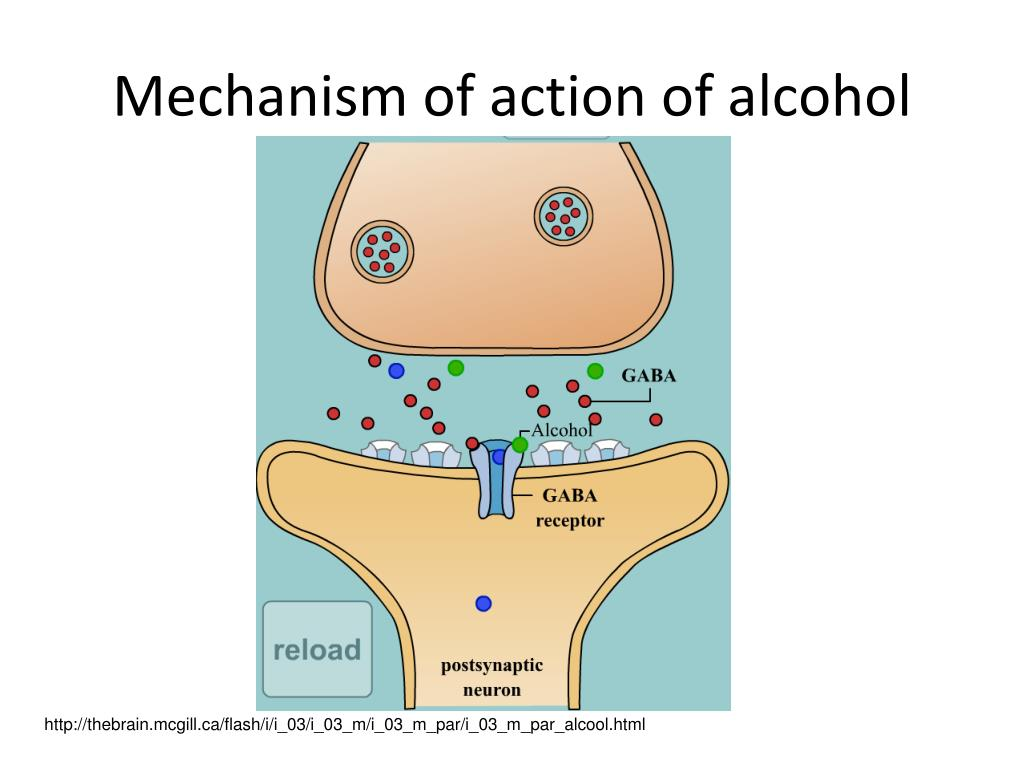
Enhances GABA-mediated inhibition
Dose-dependent
Activation of the reward circuit
Binds with 5-HT3 receptors
Chronic Effects
Two neuropsychiatric syndromes
Wernicke’s encephalopathy: Confusion, nystagmus, and abnormal ocular movements; readily reversible with thiamin
Korsakoff’s psychosis: Polyneuropathy, inability to convert short-term memory into long-term memory, and confabulation (unconscious filling of gaps in memory with fabricated facts and experiences) are not reversible
Impact on cognitive function
Effects on sleep
Other Pharmacologic Effects
Cardiovascular system: Abuse of alcohol results in direct damage to the myocardium, increasing the risk of heart failure and elevation of blood pressure
Glucose metabolism
Bone health
Patho
Respiration: Alcohol depresses respirations
Liver: Nonviral hepatitis
Stomach: Erosive gastritis
Kidney: Alcohol is a diuretic
Pancreas: Pancreatitis
Cancer: Breast and colorectal cancer
Pregnancy and lactation: Fetal alcohol spectrum disorder and fetal alcohol syndrome
Impact on longevity
Basic Pharmacology of Alcohol
Pharmacokinetics
Absorption
Distribution
Metabolism
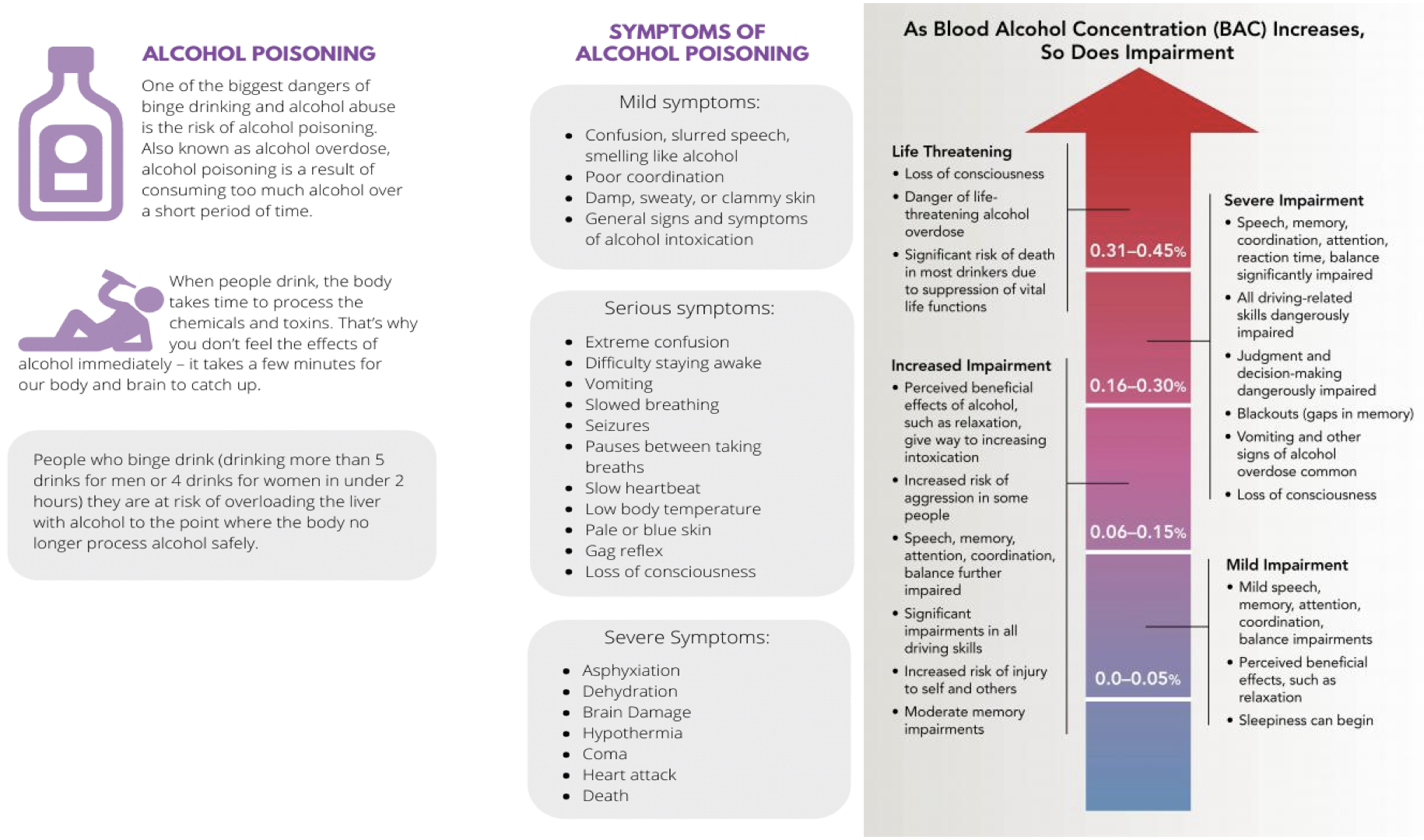
Blood levels
In the United States, 0.08% defines intoxication
Earliest effects at 0.05%
When blood alcohol level exceeds 0.4%, there is a substantial risk of respiratory depression, peripheral collapse, and death
Tolerance
Physical dependence
Drug interactions
CNS depressants
Nonsteroidal anti-inflammatory drugs
Acetaminophen
Disulfiram
Antihypertensive drugs
Quitting ❌alcohol 🍺cold 🥶 turkey 🦃 can 👍lto seizureses 😬, coma 💤, and 🫰 death 💀!
Overdose
Acute overdose
Vomiting, coma, and pronounced hypotension and respiratory depression
Aspiration
Alcohol-induced hypotension: Direct effect on peripheral blood vessels
Hypotension cannot be corrected with vasoconstrictors (eg, epinephrine)
Hypotension can lead to renal failure and cardiovascular shock
Alcohol poisoning is treated like poisoning with all other general CNS depressants
Precautions and Contraindications
Peptic ulcer disease
Liver disease
Pregnancy
Epilepsy
Dose-related increase in the risk of breast cancer
Increases the risk of cancer of the liver, rectum, and aerodigestive tract
Serious adverse effects if combined with CNS depressants, nonsteroidal anti-inflammatory drugs, acetaminophen, vasodilators, and disulfiram
Alcohol use disorder:
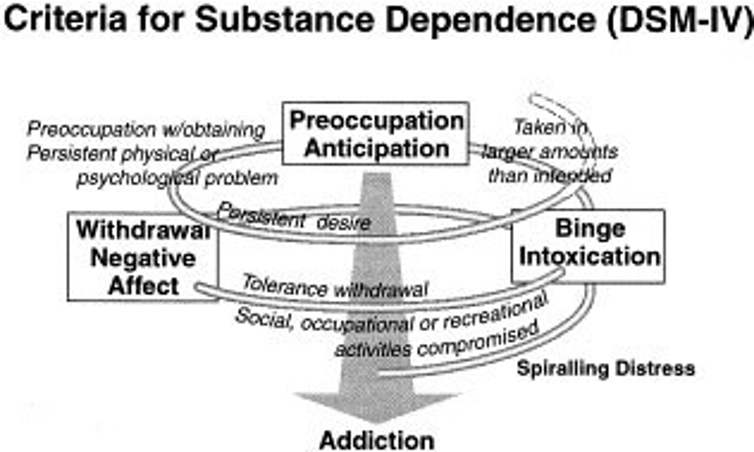
Relapsing disorder
Impaired control over drinking
Preoccupation with alcohol consumption
Use of alcohol despite awareness of adverse consequences
Distortions in thinking
Influenced by genetics as well as psychosocial and environmental factors
Alcoholism is a cycle 🌀
Drugs for alcohol use disorder:
Drugs used to facilitate withdrawal
Benzodiazepines
Chlordiazepoxide [Librium, others]
Clorazepate [Tranxene]
Oxazepam [Serax]
Lorazepam [Ativan]
Adjuncts to benzodiazepines
Carbamazepine (antiepileptic drug)
Clonidine (alpha-adrenergic blocker)
Atenolol and propranolol (beta-adrenergic blockers)
Drugs used to maintain abstinence
Disulfiram
Naltrexone
Acamprosate
Other drugs used for the treatment of alcohol abuse
B vitamins
Thiamin
Folic acid
Cyanocobalamin
Vitamin supplements
Fluid replacement therapy
Antibiotics
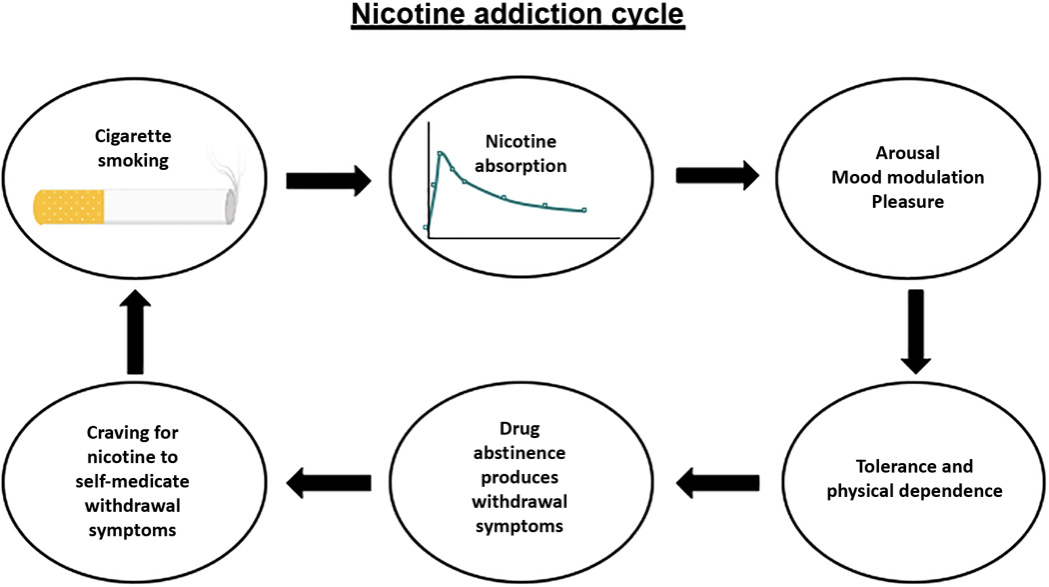
Nicotine and smoking:
Cigarette smoking remains the greatest single cause of preventable illness and premature death
In Canada, smoking kills more than 230,000 adults each year; this is just under 1 of every 5 deaths
Mechanism of action of nicotine:
Effects of nicotine result from actions at nicotinic receptors:
Can activate nicotinic receptors found in the autonomic ganglia, the adrenal medulla, the carotid body, the aortic arch, and the central nervous system
Actions in the central nervous system mimic those of cocaine and other highly addictive substances
Pharmacokinetics
Pharmalogic effects
Cardiovascular
It constricts blood vessels, accelerates the heart, and increases the force of ventricular contraction
The net result is elevation of blood pressure and increased cardiac work
Gastrointestinal
Increases secretion of gastric acid
Augments tone and motility of gastrointestinal smooth muscle
Can promote vomiting
Central nervous system
Stimulates respiration and produces an arousal pattern on an electroencephalograph
Moderate doses can cause tremors; high doses can cause convulsions
Psychological effect
Pregnancy and lactation
Exposure during gestation can harm fetus
Nicotine in breast milk can harm nursing infant
Pharmaceutical nicotine is safer than tobacco smoke
It is reasonable to consider using nicotine therapy during pregnancy to help a patient quit smoking
Nicotine and Smoking
Tolerance
Dependence
Acute poisoning
Treatment: Reducing nicotine absorption and supporting respiration
Activated charcoal
Ventilatory assistance
Chronic toxicity from smoking
“5 A’S” Model for treating tobacco use and dependence
Ask (screen all patients for tobacco use)
Advise tobacco users to quit
Assess willingness to make a quit attempt
Assist with quitting (offer medication and provide or refer to counselling)
Arrange follow-up contacts, beginning within the first week after the quit date
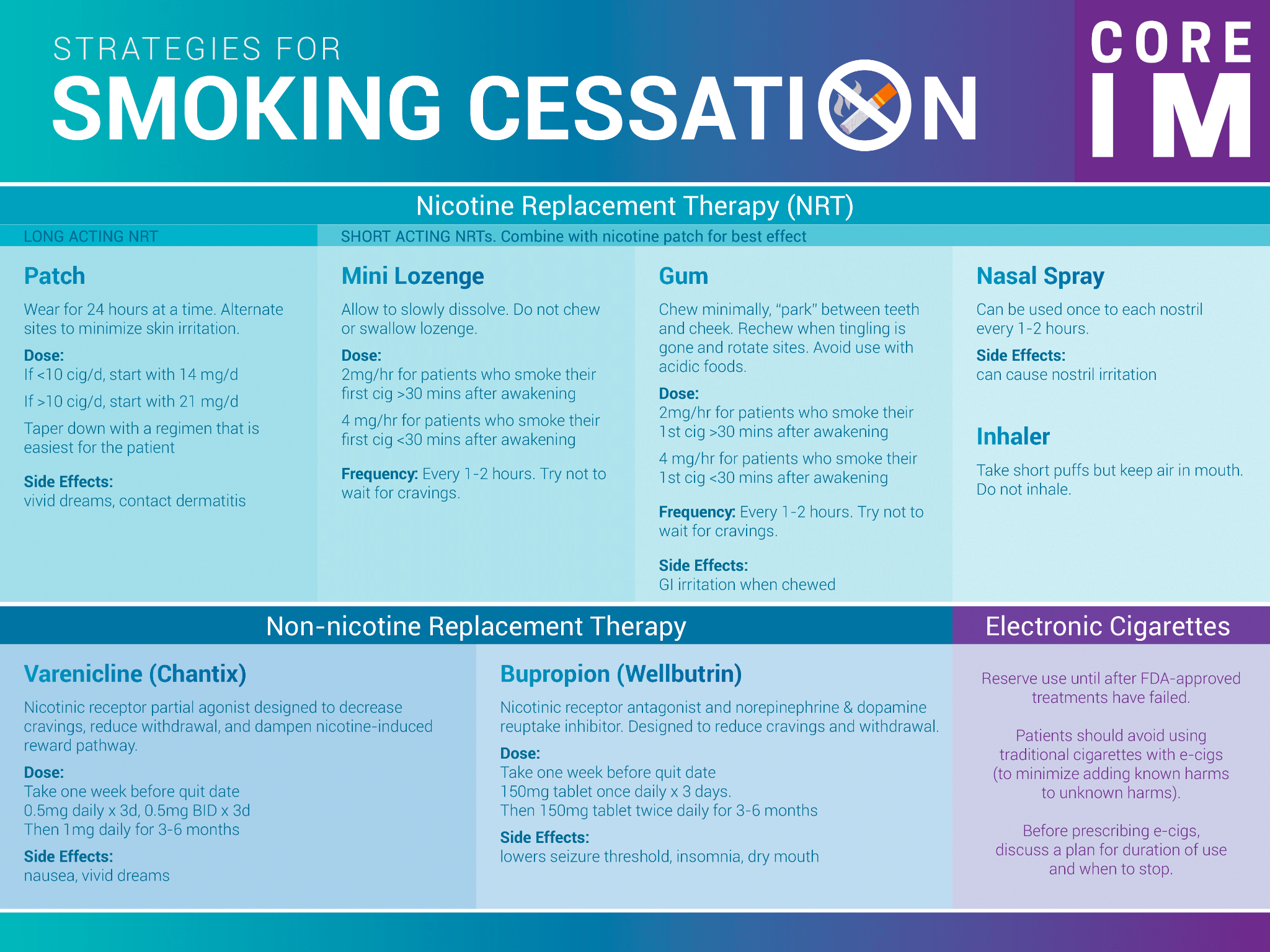
Nicotine chewing gum
Double the cessation success rate
Adverse effects: Mouth and throat soreness, jaw muscle ache, eructation (belching) and hiccups
Chew the gum slowly and intermittently for about 30 minutes
Avoid eating or drinking while chewing, and wait 15 minutes before chewing.
Nicotine lozenges
Double the cessation success rate
Adverse effects: mouth irritation, dyspepsia, nausea, and hiccups
Allow lozenge to dissolve in mouth over 20to 30 minutes
No eating or drinking for 15 minutes before dosing and while the lozenge is in the mouth
Do not chew or swallow the lozenge.
Nicoderm CQ and Nicotrol
Doubling the cessation success rate
Adverse effects: short-lived erythema, itching, and burning occur under the patch
Applied once a day to clean, dry, non-hairy skin of the upper body or upper arm
Application sites should be changed daily and not reused for at least one week.
Nicotine Inhaler
Doubles the cessation success rate
Adverse effects: Dyspepsia, coughing, throat irritation, oral burning, and rhinitis
Frequent puffing over 20 minutes
It should not be used by patients with asthma
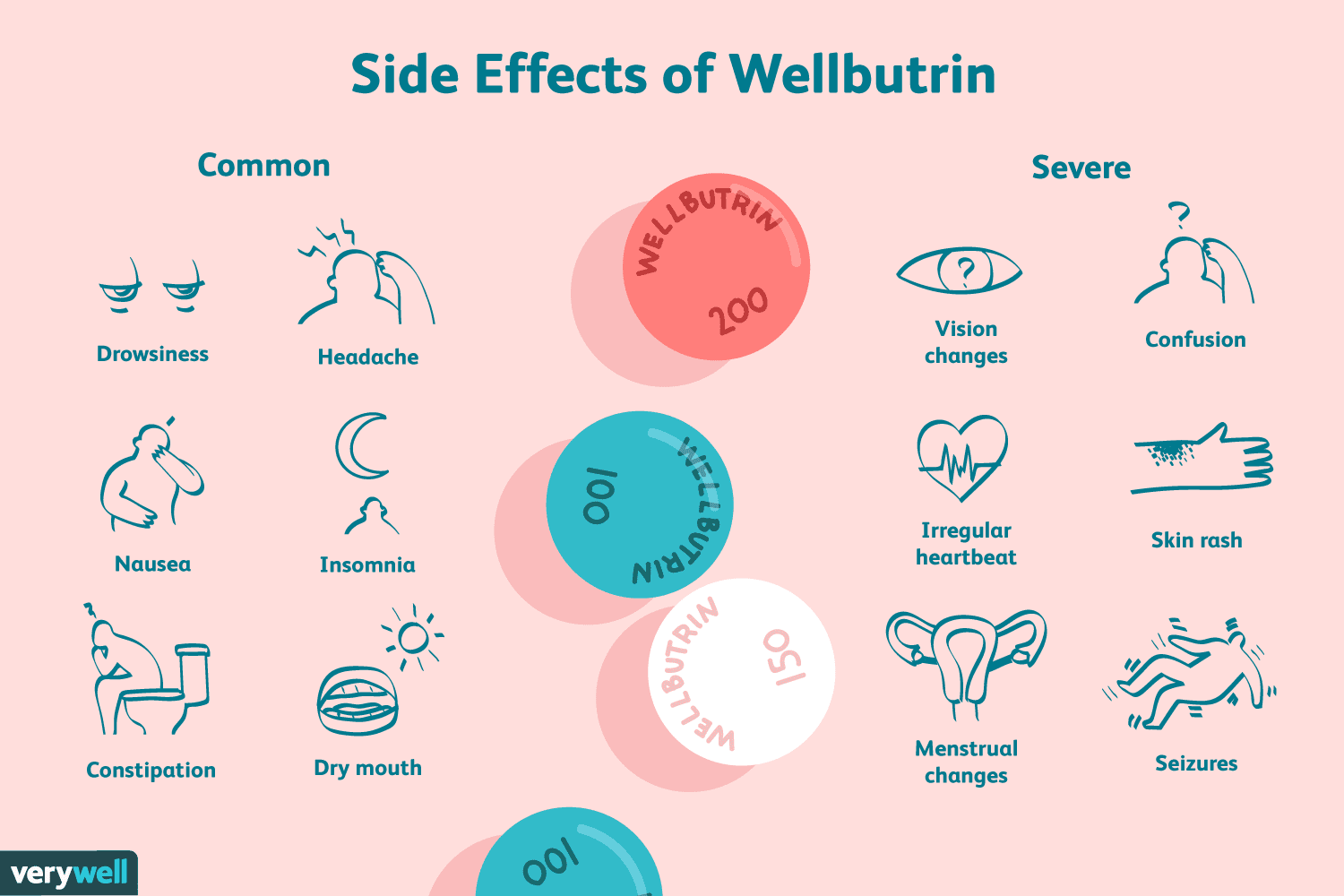
Bupropion SR [Zyban, Buproban]
Atypical antidepressant
Reduces the urge to smoke and reduces some symptoms of nicotine withdrawal, such as irritability and anxiety
Adverse effects: Dry mouth and insomnia
Varenicline [Chantix, Champix]
Partial agonist at nicotinic receptors
The most effective aid for smoking cessation
Atypical antidepressant
Adverse effects: Nausea, sleep disturbances, headaches, abnormal dreams, constipation, dry mouth, flatulence, vomiting, and altered sense of taste
Serious neuropsychiatric effects
Cardiovascular events
U.S. authorities have banned the use of varenicline by truck drivers, bus drivers, airplane pilots, and air traffic controllers
Case study
You are working at a family clinic. Your patient is a 17-year-old young man who came in today for a sports physical examination. Upon completing a substance abuse history, he shares that he has been smoking for the past year. He read on the Internet that nicotine is a natural substance from the nightshade family and that there are not as many harmful effects as the media lets on. He would like you to answer the following questions:
Can I become addicted to cigarettes?
Yeah
How can cigarettes be so harmful if they are made from natural substances?
Anything in your lungs that is not air is bad for you
Processed
Over 2000 substances
Chemically complex that cause issues
Are there treatments available for quitting smoking?
Yeah there is gum, patches, lozenges, medications, counselling, spray, and inhalation
Major drugs of abuse
Opioids
Psychostimulants
Depressants
Psychedelics
Dissociative drugs
Anabolic steroids
Miscellaneous drugs of abuse
Marijuana
d-Lysergic acid diethylamide (LSD)
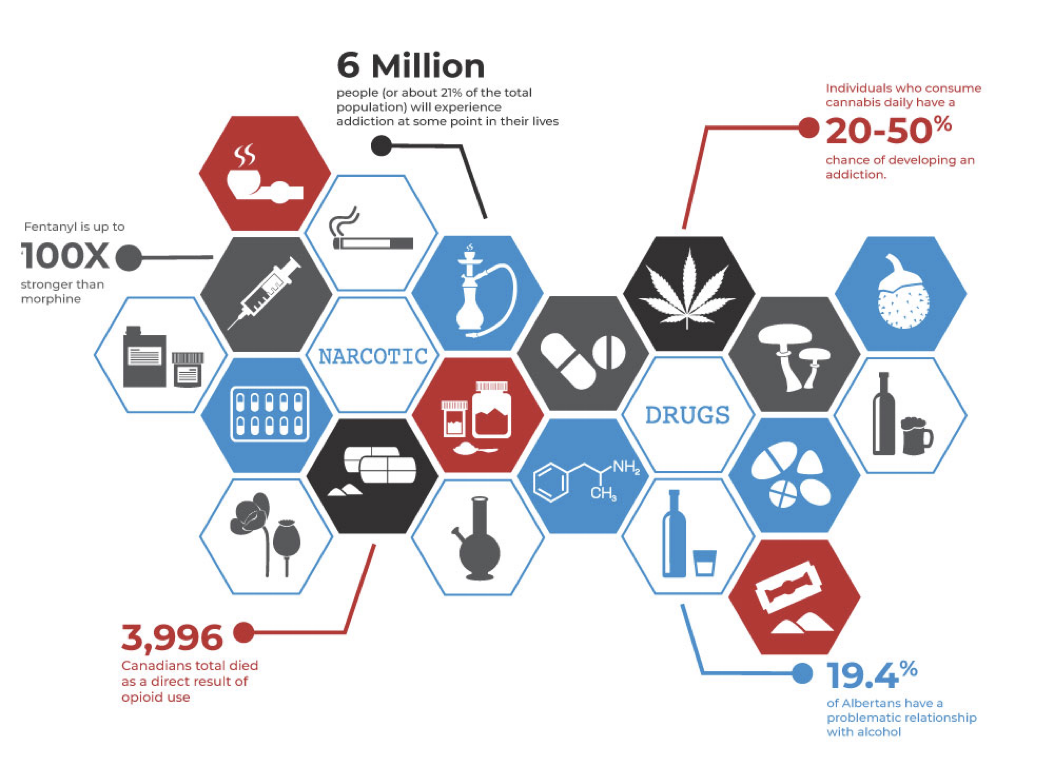
Heroin, Oxycodone, and other opioids
Major drugs of abuse: Heroin, oxycodone, and meperidine
Most opioids are Schedule II
Patterns of abuse
Subjective and behavioural effects
Preferred drugs and routes of administration
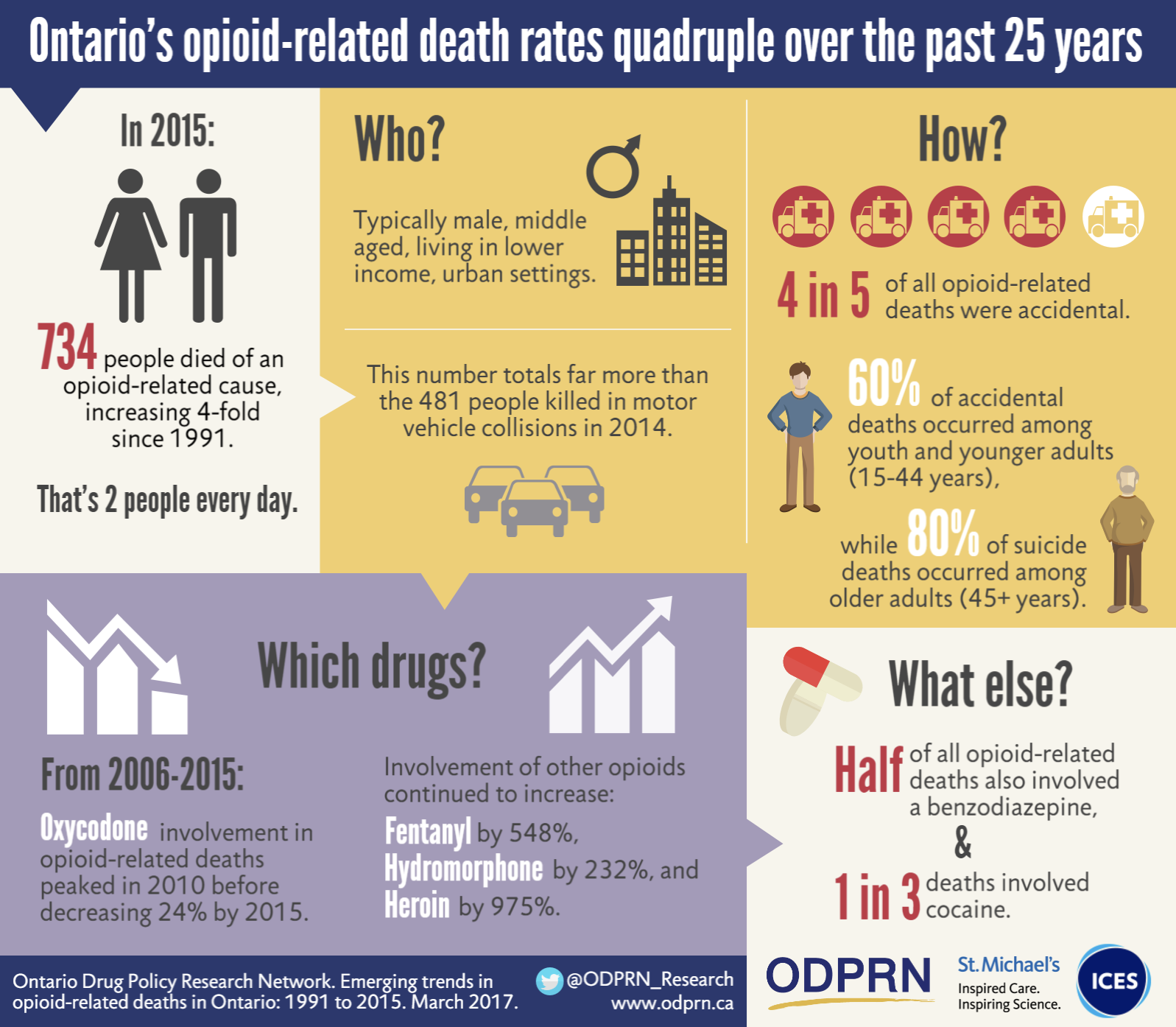
Heroin
Patterns of use
Greatest use among 18- to 25-year-olds
All segments of society
The first exposure is usually social or for pain management
Subjective and behavioural effects
Moments after IV injection: Sensations of pleasure, relaxation, warmth, and thirst
Followed by euphoria
Initial use causes nausea and vomiting
Initially, it may also cause an overall sense of dysphoria
Preferred drugs and routes of administration
Opioid of choice for street use
High lipid solubility
IV route preferred, but also smoking and nasal inhalation
Oxycodone
Opioid is similar to morphine
Intended as controlled-release drug [OxyContin]
Abusers crush tablet
Snort powder or dissolve in water for IV
The entire dose absorbed immediately, with high risk of death
R-r-r-roll💿up⬆to2⃣the🤩party🥳with🧶my🧚crazy🤪pink💝wig💇🏼
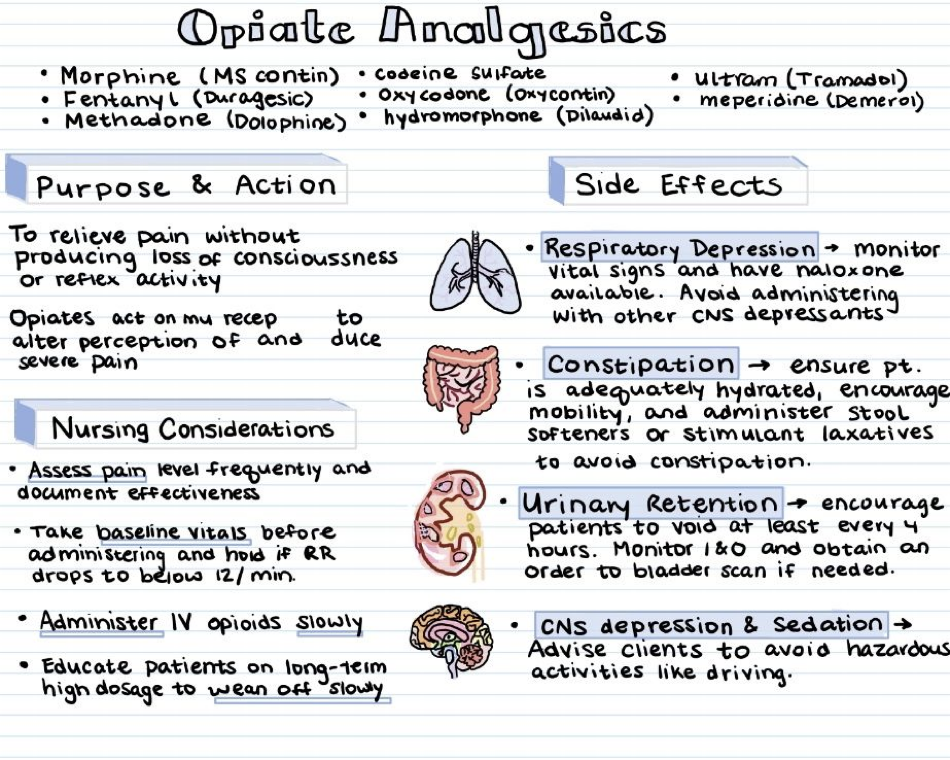
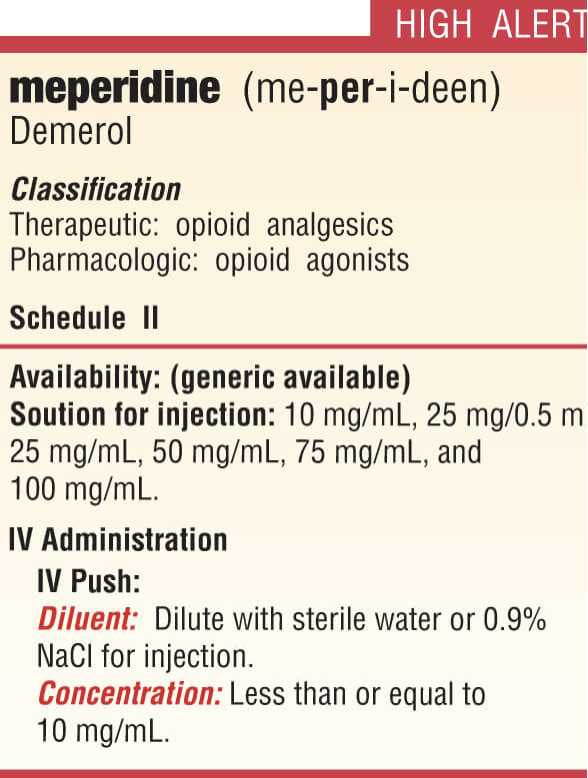
Meperidine
Nurses and healthcare providers who abuse opioids often select meperidine
Highly effective in oral route (unlike injections, leaves no sign)
Minimal effect on smooth muscle: Fewer problems with constipation and urinary retention
Tolerance and physical dependence
Tolerance
Prolonged use
Effects for which tolerance develops
Effects for which tolerance does not develop
Cross-tolerance
Physical dependence
Long-term use
Abstinence syndrome
Acute phase and second phase
Alcholics have a low dependence on depressants and anxiety medications like Benzodiazapines
Treatment of acute toxicity
Triad of symptoms and treatment
Respiratory depression
Coma
Pinpoint pupils
Naloxone [Narcan]: Careful titration
Opioid detoxification
Detoxification
Clonidine-assisted withdrawal
Centrally acting alpha2-adrenergic agonist
Most effective against symptoms related to autonomic hyperactivity (nausea, vomiting, diarrhea)
Provides modest relief from muscle aches, restlessness, anxiety, and insomnia
Does not diminish opioid craving
Rapid withdrawal
Ultrarapid withdrawal
Administration of naloxone or naltrexone: Immediate withdrawal
The withdrawal process accelerated
Ultrarapid procedure: General anesthesia or heavy sedation with IV midazolam [Versed]
In both procedures, clonidine may be added to ease symptoms
No more effective than standard withdrawal techniques
Considerably more expensive
Methadone substitution (much better option) Tapering (3 weeks or 1 month)
Long-acting oral opioids
The most commonly used agent
Approximately 10 days
Buprenorphine
Substituted for opioids, the addict is physically dependent on
Prevents symptoms of withdrawal
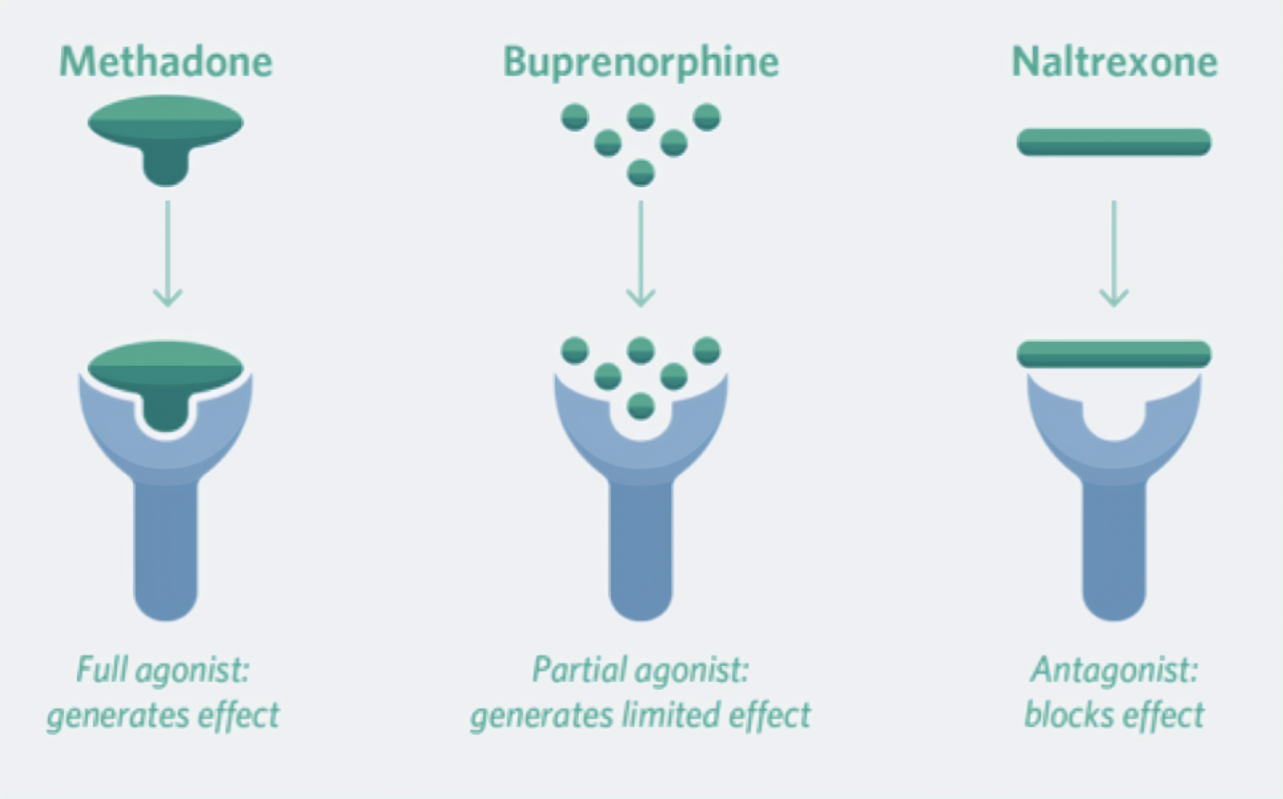
Drugs for long-term opioid addiction management
Three groups of medications
Opioid agonists, opioid agonist-antagonists, and opioid antagonists
Methadone
Maintenance and suppressive therapy
Buprenorphine
Maintenance therapy and detox facilitation
Naltrexone
Discourages renewed opioid abuse
Sequelae of compulsive opioid use
Few direct detrimental effects
Individuals on methadone maintenance can be successful socially and at work
Indirect hazards: Septicemia, cellulitis, abscesses, endocarditis, tuberculosis, hepatitis C, HIV, and foreign body emboli
Accidental overdose
General CNS depressants
Barbiturates, benzodiazepines, alcohol, and other agents
Benzodiazepines have unique properties
Barbiturates
Depressant effects are dose-dependent
Mild sedation to sleep to coma and death
Subjective effects similar to those of alcohol
Agents with a short to intermediate duration of action have highest abuse incidence and are Schedule II
Amobarbital, pentobarbital, and secobarbital
Tolerance

Physical dependence
Withdrawal
Acute toxicity
Maintain respiration and remove drug
Naloxone reverses opioid poisoning, but it is not effective against barbiturate poisoning.
Benzodiazepines
Benzodiazepines (Schedule IV)
Much safer than barbiturates
Overdose is rare when taken alone and orally
Risk increased with IV or with other depressants
Tolerance
Physical dependence and withdrawal techniques
Acute toxicity
Flumazenil [Romazicon]
Psychostimulants
CNS stimulants (Schedule II) with a high potential for abuse
Methamphetamines
Cocaine
Can stimulate the heart, blood vessels, and other structures under sympathetic control
The nods. They start nodding and pass out; they dont wake up
Cocaine
CNS effect similar to that of amphetamines
Two forms are used by abusers:
Cocaine
“Crack”
Can produce local anesthesia, vasoconstriction, and cardiac stimulation
Acute toxicity
Mild overdose: agitation, dizziness, tremor, blurred vision.
Severe overdose: hyperpyrexia, convulsions, ventricular dysrhythmias, hemorrhagic stroke, angina pectoris, myocardial infarction.
Treatment: intravenous diazepam or lorazepam, nitroprusside, hypertonic sodium bicarbonate, and aspirin.
Chronic toxicity
Intranasally: atrophy of the nasal mucosa and loss of sense of smell
Extreme cases: necrosis and perforation of the nasal septum
Injury to the lungs can occur from smoking cocaine.
Use during pregnancy
Treatment of cocaine addiction
Anticocaine vaccine
Disulfiram (antabuse)
Cocaine
Cocaine hydrochloride
White powder
Diluted for sale
Taken intranasally
Cocaine base: commonly called “crack:
Heated for use
Taken by IV injection
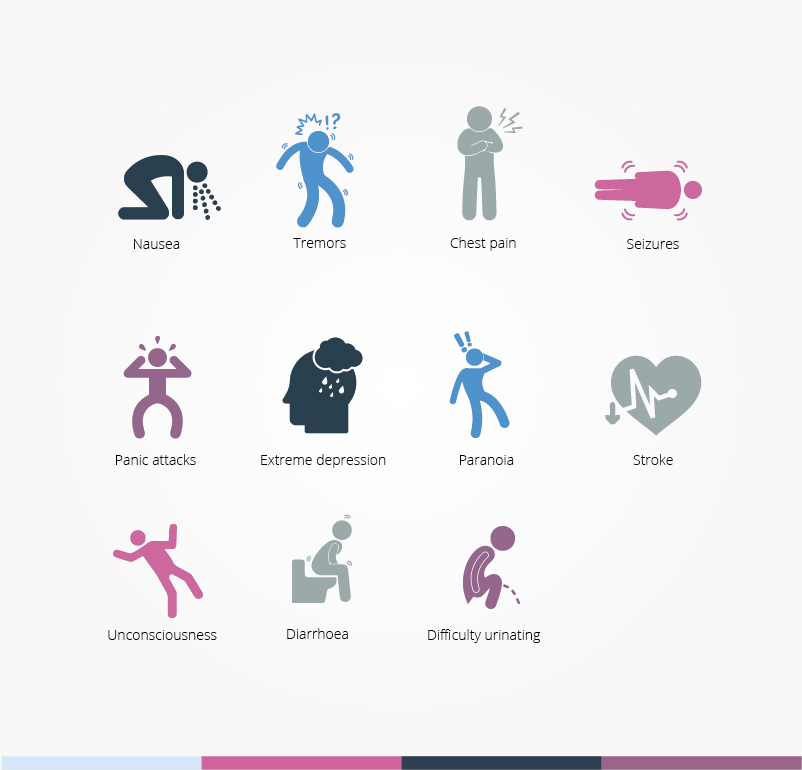
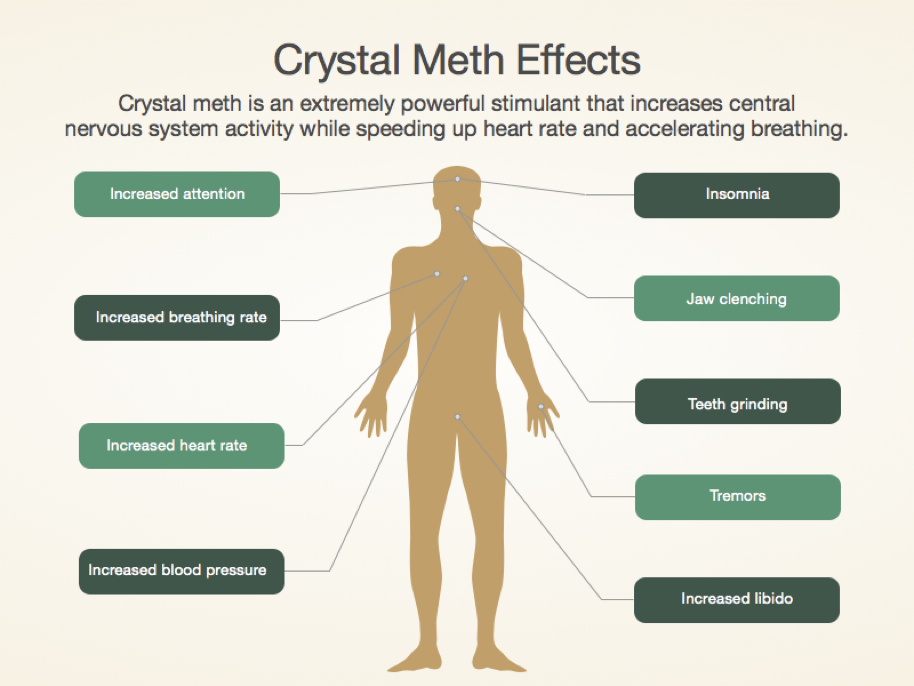
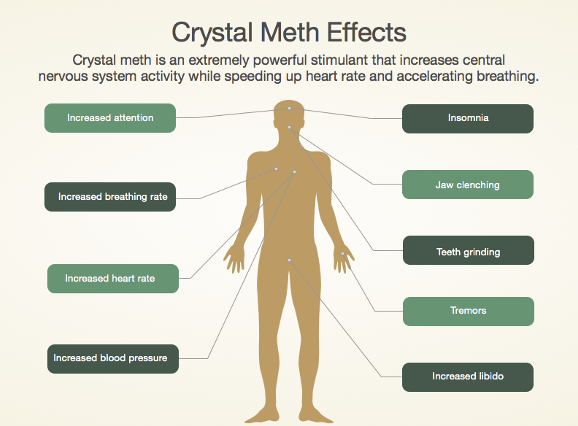
Methamphetamines
In abuse, usually taken orally, snorted, smoked, or IV
Also called “ice” or “crystal meth,”
Form of dextroamphetamine
Smoked, snorted, or inserted into rectum
Effects
Arousal, euphoria, and a sense of increased physical strength and mental capacity
Hallucinations, psychotic states, and sympathomimetic actions
Adverse cardiovascular effects
Hypertension
Angina pectoris
Dysrhythmias
Cerebral and systemic vasculitis, renal failure, stroke
Vasoconstriction can be relieved with an alpha-adrenergic blocker, e.g., phentolamine.
Cardiac stimulation can be reduced with a mixed alpha and beta blocker (eg, labetalol)
Other adverse effects
Significant weight loss
Fetal effects
“Meth mouth” (severe tooth decay, disinegrated gums)
Tolerance, dependency, and withdrawal
Treatment: cognitive behavioural therapy, matrix model, bupropion [Wellbutrin, Zyban], modafinil [Provigil, Alertec], and lbudilast.
Marijuana
Cannabis sativa (hemp)
Marijuana and hashish are derivatives
Common names: “grass,” “weed,” "pot.”
Most commonly used illicit drugs in the United States, although it is now legal in some states
Psychoactive substance
Delta-9-tetrahydrocannabinol (THC)
Routes
Smoking
60% of THC content is absorbed; effects begin in minutes and peak within 20 to 30 minutes
Oral
Most of THC is inactivated by first-pass effect
Increased production of prostaglandin E2
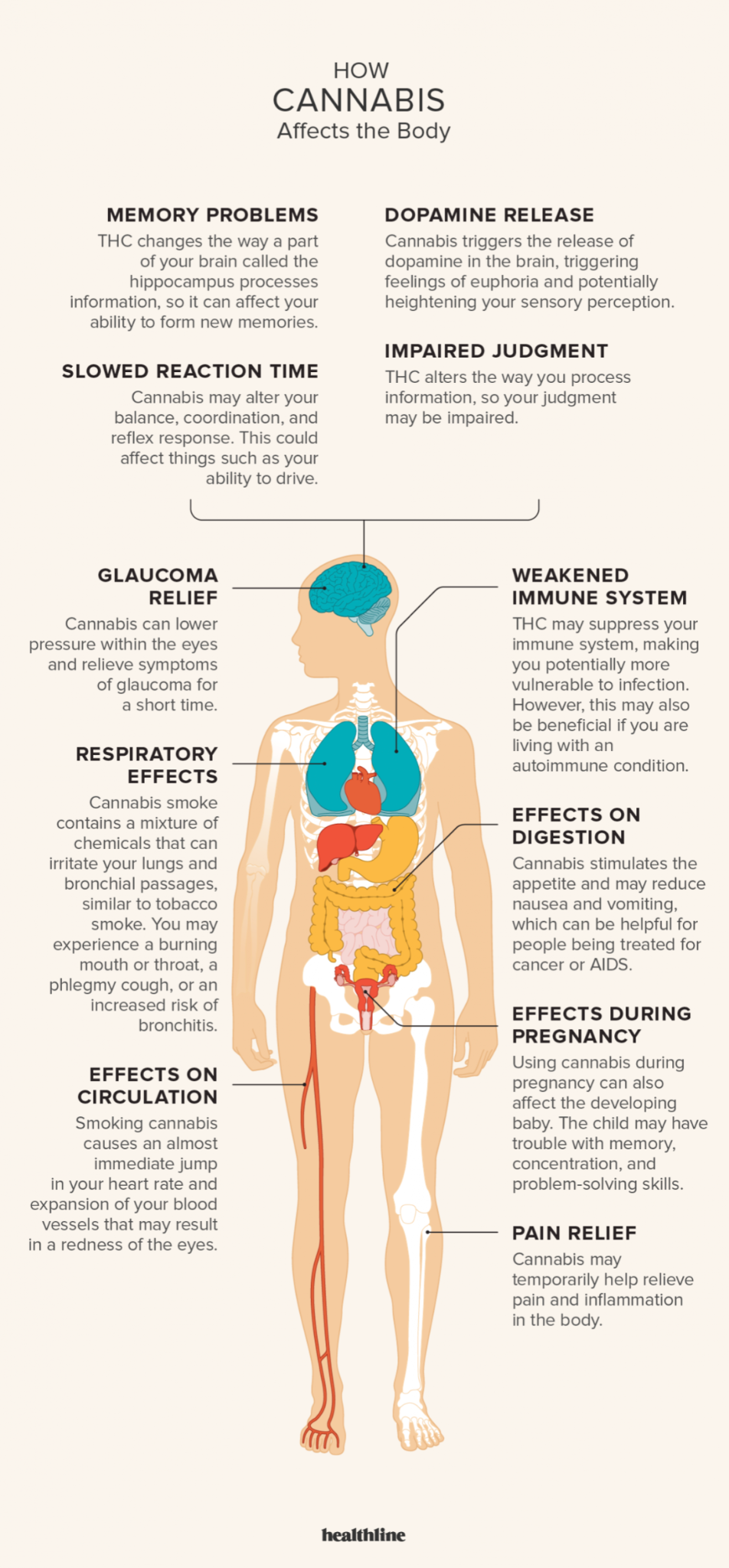
Behaviors
Euphoria
Sedation
Hallucinations
Therapeutic uses
Antiemetic
Appetite stimulant
Neuropathic pain
Effects
Low to moderate dose
High dose
Long-term use
Schizophrenia
Cardiovascular
Dose-related increase in heart rate
Respiratory
Acute: Bronchodilation
Chronic: Airway constriction
Reproduction
Males and females affected
Altered brain structure
Hippocampal volume, left hemisphere
Tolerance and dependence
Therapeutic use of Marijuana
Approved uses for cannabinoids
Unapproved uses for cannabinoids
Medical research on marijeuna
The legal status of medical marijuana
Synthetic Marijuana
Comparison of marijuana with alcohol
Aggressive behaviour is rare with marijuana use
Less loss of judgment with marijuana
Increased appetite with marijuana: Fewer problems with nutritional deficiencies
Marijuana produces increased toxic psychosis, dissociative phenomena, and paranoia, more so than alcohol does.
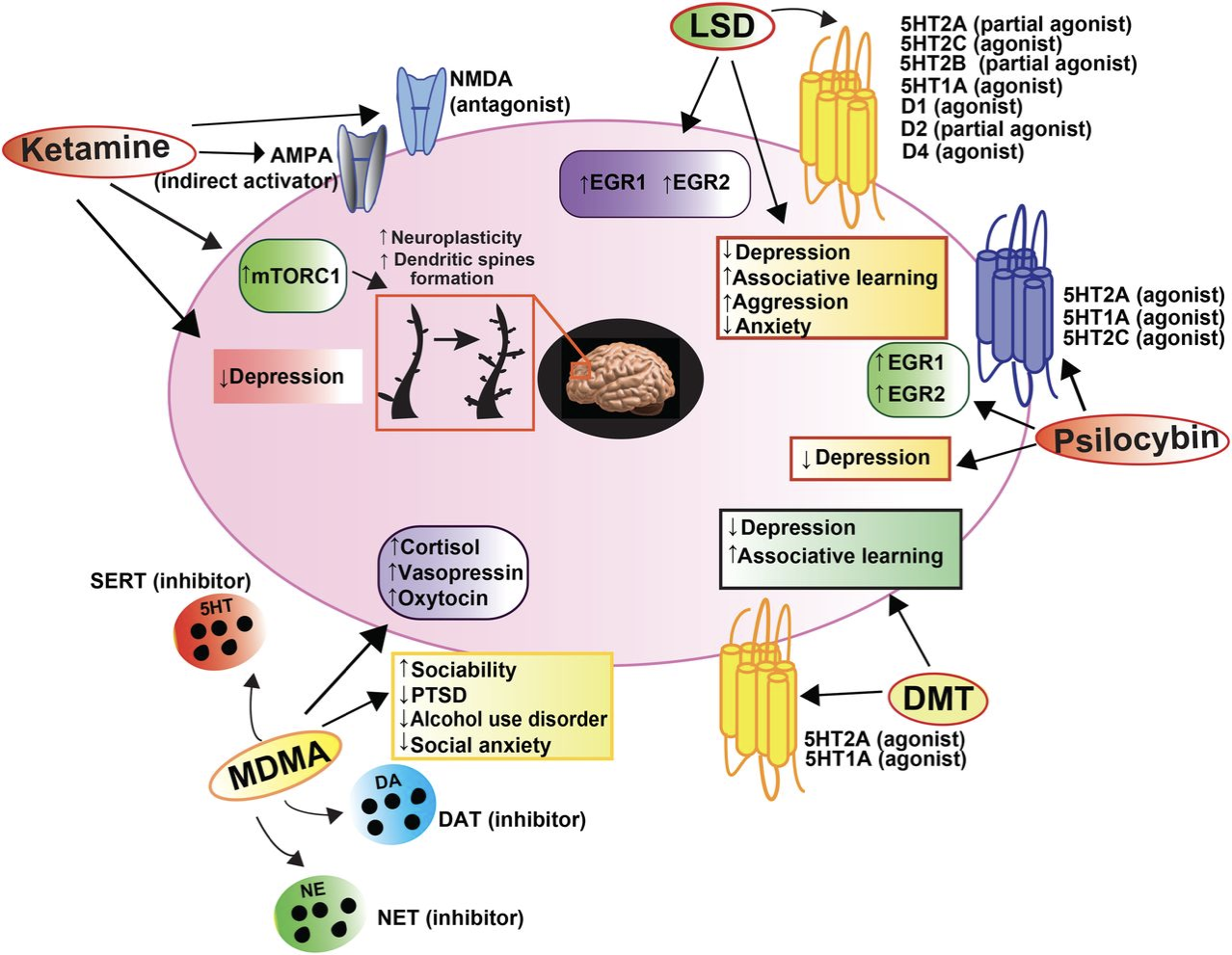
Psychedelics
d-Lysergic acid diethylamide (LSD)
Acts on the brain’s serotonin receptors
Routes: Oral, IV, smoked
Alters the following (as otherwise occurs only in dreams):
Thinking
Feelings
Perception
Relationship to environment
Saliva: causes dream-like state of unreality
Mescaline
From peyote cactus
Psilocybin
Psilocin
Dimethyltryptamine
Dissociative drugs
Phencyclidine (PCP) and ketamine
Original use: Surgical anaesthetics
Recreational use: Distort sight and sound and produce dissociation
Act in the cerebral cortex and limbic system
PCP easily synthesized and manufactured by amateurs
Routes: Oral, intranasal, IV, smoking
Phencyclidine (PCP)
Effects
Low to moderate doses, high doses
Toxicity
Ketamine
Similar to PCP in structure, mechanism, and effects
Shorter duration of effects
Dextromethorphan
Over-the-counter (OTC) cough suppressant
Low dose for antitussive: No psychologic effects
Doses 5 to 10 times higher: produce euphoria, disorientation, paranoia, altered sense of time, and hallucinations
Also used in combination cold products
Highly abused by adolescents and teenagers because of accessibility and low cost
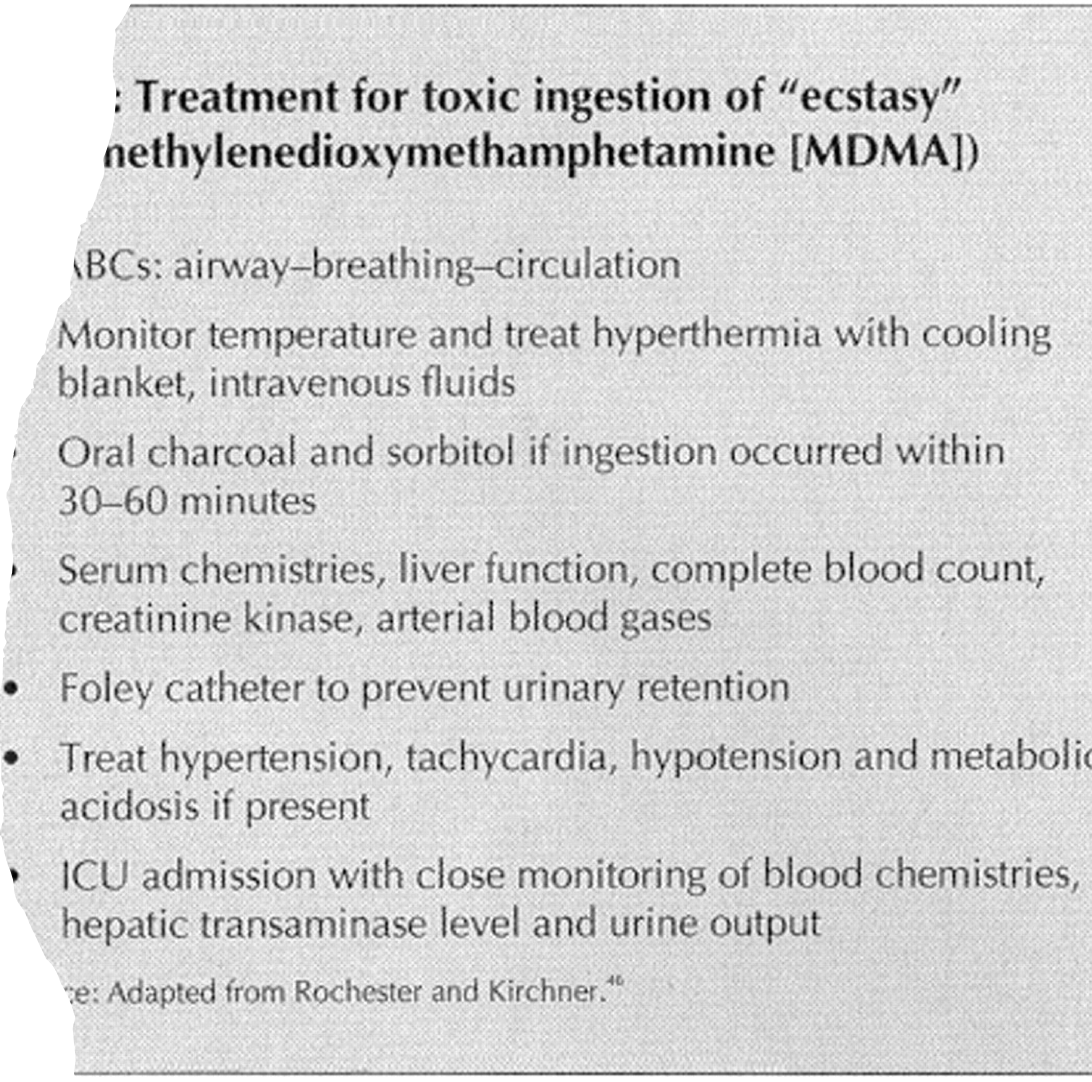
3, 4: Methylenedioxymethamphetamine
Common names: MDMA, ecstasy
A complex drug with stimulant and psychedelic properties
Structurally related to methamphetamine (stimulant) and mescaline ( hallucinogen),
Low doses: Mild LSD-like psychologic effects
Higher doses: Amphetamine-like effects
Promotes release of neurotransmitters
Usually taken orally; also snorted, injected, or taken by rectal suppository
Adverse effects
Can injure serotonergic neurons, stimulate the heart, and dangerously raise body temperature
Neurologic effects
Seizures, spasmodic jerking, jaw clenching, teeth grinding
Confusion, anxiety, paranoia, panic
Inhalants
The term can refer to many drugs; common characteristic is administration by inhalation
Anesthetics
Volatile nitrites
Organic solvents
Anabolic Steroids
Androgens
Taken to enhance athletic performance
Increase muscle mass and strength
Massive doses often used have high risk for adverse effects
Most are classified as Schedule III drugs
Question 1
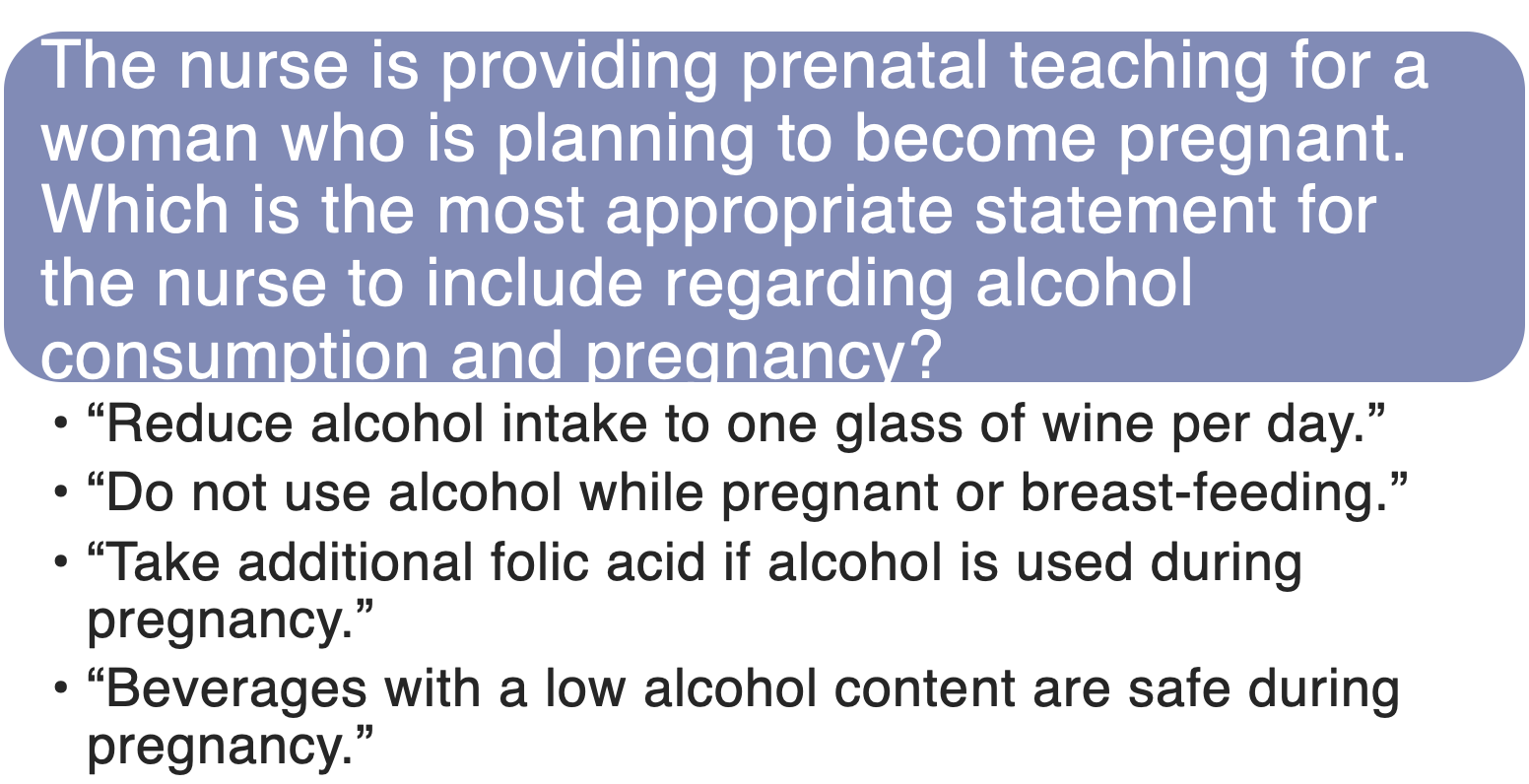
Answer B
Rationale: pregnant and lactating women should be advised to avoid alcohol entirely.
Question 2
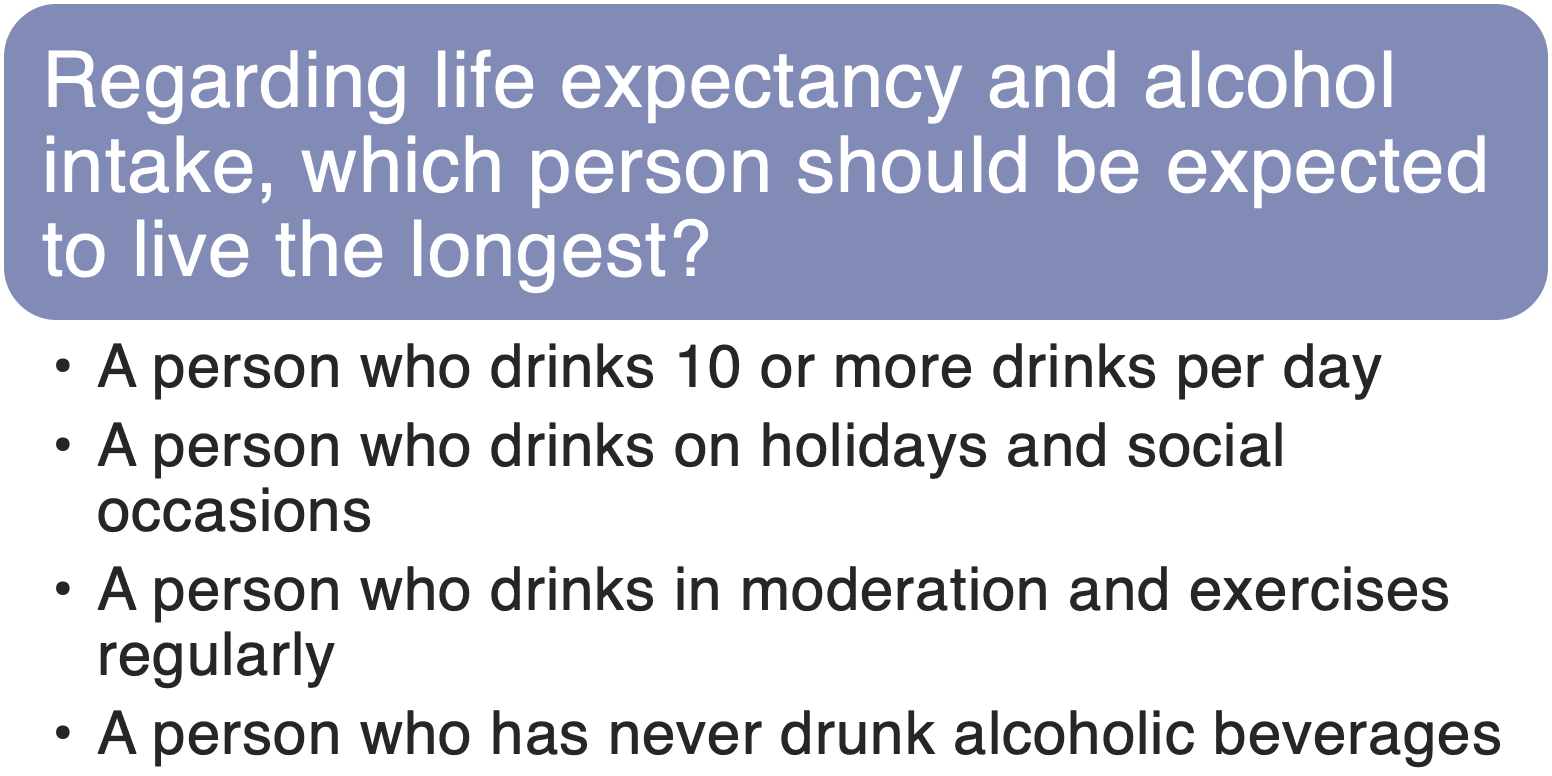
Answer C
Rationale: people who consume moderate amounts of alcohol live longer than those who abstain. The life span is even greater if the person drinks moderately and performs regular exercise.
Question 3
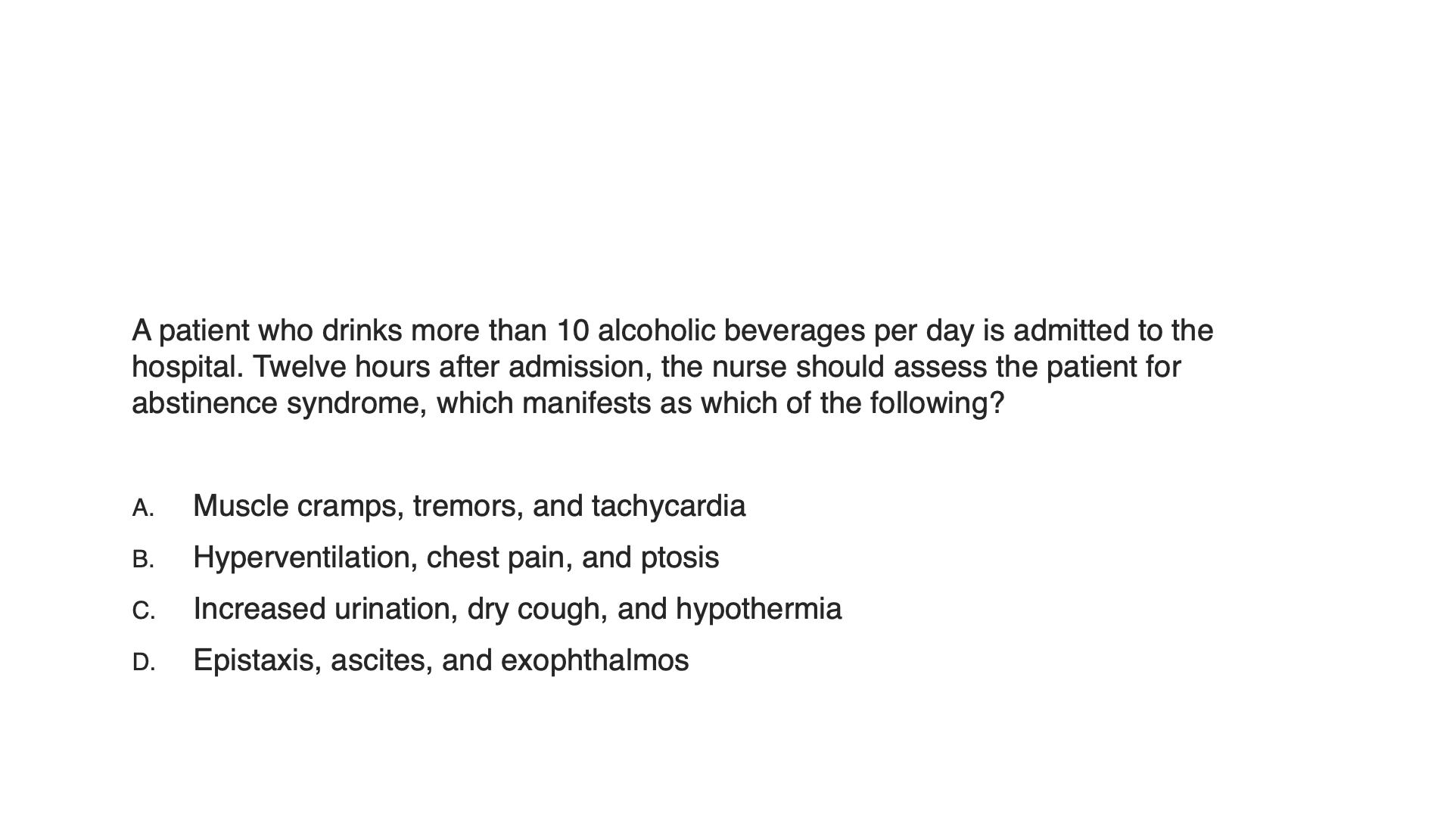
Answer A
Rationale: The long-term use of alcohol produces physical dependence, and abrupt withdrawal produces an abstinence syndrome. When the degree of physical dependence is low, withdrawal symptoms (e.g., disturbed sleep, weakness, nausea, anxiety, and mild tremors) are mild and last less than a day. By contrast, when the degree of dependence is high, withdrawal symptoms can be severe. Initial symptoms appear 12 to 72 hours after the last drink and continue for 5 to 7 days. Early manifestations include cramps, vomiting, hallucinations, and intense tremors; heart rate, blood pressure, and temperature may rise, and tonic-clonic seizures may develop. As the syndrome progresses, disorientation and loss of insight occur. A few alcoholic patients (<1%) experience delirium tremens (severe persecutory hallucinations). In extreme cases, alcohol withdrawal can result in cardiovascular collapse and death.
Question 4
The nurse is providing teaching about smoking cessation to a patient with heart disease who smokes 1 to 1½ packs of cigarettes per day. Which statement should the nurse include?
The reduction of nicotine use will decrease blood pressure.
Weight loss occurs with the decreased use of nicotine.
Smoking decreases the heart rate and increases the respiratory rate.
Smoking causes a decreased workload for the heart.
Answer: A
Rationale: Nicotine in low doses (such as smoking 1 to 1½ packs per day) causes the following pharmacologic effects: elevation of blood pressure, weight loss, and increased heart rate and cardiac workload. Smoking cessation will reduce blood pressure, heart rate, and cardiac workload; it will also stimulate the appetite and result in possible weight gain.
Question 5
The nurse completed smoking cessation teaching for a patient with peptic ulcer disease. Which statement by the patient indicates that more teaching is indicated?
“Nicotine can increase problems with vomiting.”
“Smoking could have caused the ulcers in my stomach.”
“If I switch to nicotine patches, my stomach will start to heal.”
“Smoking causes an increase in the amount of stomach acid.”
Answer: C
Rationale: Nicotine influences gastrointestinal function primarily by activating nicotinic receptors in the parasympathetic ganglia, thereby increasing the secretion of gastric acid and augmenting the tone and motility of gastrointestinal smooth muscle. In addition, nicotine can promote vomiting. Nicotine-induced vomiting results from a complex process that involves nicotinic receptors in the aortic arch, the carotid sinus, and the central nervous system. Nicotine can cross membranes easily, and it is widely distributed throughout the body.
Question 6
After being admitted to the hospital, a patient indicates a willingness to make an attempt to quit smoking. It is most appropriate for the nurse to do what?
Advise the patient that insurance will not cover medications.
Assist the patient with strategies to stop smoking.
Ask the patient to find a support group after discharge.
Encourage the patient to use electronic cigarettes.
Answer: B
Rationale: The overall intervention strategy is summarized in the “5 A’s” model for treating tobacco use and dependence: Ask (screen all patients for tobacco use); Advise tobacco users to quit; Assess willingness to make a quit attempt; Assist with quitting (offer medication and provide or refer to counselling); and Arrange follow-up contacts, beginning within the first week after the quit date.
Question 7
The nurse instructs the patient about how to use nicotine chewing gum [Nicorette]. The nurse determines that teaching is successful if the patient makes which statement?
“I will not eat or drink for 1 hour before chewing the gum.”
“The gum is safe during the first 3 months of pregnancy.”
“Chewing the gum rapidly reduces belching and hiccups.”
“I should chew the gum slowly for about 30 minutes.”
Answer: D
Rationale: Nicotine chewing gum must be chewed to release the nicotine. The most common adverse effects are mouth and throat soreness, jaw muscle ache, eructation (belching), and hiccups. Using optimal chewing techniques minimizes these problems. Patients should be advised to chew the gum slowly and intermittently for about 30 minutes. Rapid chewing can release too much nicotine at one time, which results in effects similar to those of excessive smoking, such as nausea, throat irritation, and hiccups. Because foods and beverages can reduce nicotine absorption, patients should not eat or drink while chewing or for 15 minutes before chewing. It is not known whether using nicotine gum during pregnancy is safe.
Question 8
A patient is admitted to the healthcare facility for the treatment of cocaine addition. It is most appropriate for the nurse to do what?
Administer delta-9-tetrahydrocannabinol (THC) to reduce withdrawal symptoms.
Give regular doses of naloxone [Narcan] to precipitate immediate withdrawal.
Provide individual and group psychosocial therapy with a focus on drug counseling.
Initiate maintenance therapy with tapering doses of methadone [Methadose].
Answer: C
Rationale: The cornerstone of cocaine addiction treatment is psychosocial therapies (both individual and group counseling). THC is delta-9-tetrahydrocannabinol, or marijuana. Naloxone and methadone are used for opioid addictions.
Question 9
The nurse cares for a patient who has used marijuana daily for the past 7 years. The nurse should assess the patient for which manifestations of excessive use of marijuana?
Hallucinations, delusions, and paranoid behavior
Disheveled appearance, lack of interest, and flat affect
Increased appetite, improved sense of humor, and euphoria
Impaired memory, slow reaction time, and altered judgment
Answer: B
Rationale: Long-term, excessive use of marijuana is associated with a behavioral phenomenon known as amotivational syndrome, characterized by apathy, dullness, poor grooming, reduced interest in achievement, and disinterest in the pursuit of conventional goals. High doses of marijuana result in hallucinations, delusions, and paranoia. Low to moderate doses of marijuana can cause euphoria and relaxation; gaiety and a heightened sense of the humorous; increased sensitivity to visual and auditory stimuli; enhanced sense of touch, taste, and smell; increased appetite and ability to appreciate the flavor of food; and distortion of time perception. Moderate doses of marijuana can produce undesirable responses (for example, impairment of short-term memory; decreased capacity to perform multistep tasks; slowed reaction time and impairment of motor coordination; altered judgment and decision making; temporal disintegration; depersonalization; decreased ability to perceive the emotions of others; and reduced interpersonal interaction
Question 10
A patient is admitted to the emergency department with psychotic behavior related to an overdose of phencyclidine (PCP). Which action by the nurse is most appropriate?
Administer ammonium chloride to raise the urine pH.
Instruct the patient to take slow, deep breaths.
Administer an IV fluid bolus to prevent hypotension.
Place the patient in a quiet room with dim lighting.
Answer: D
Rationale: Psychotic reactions that occur with phencyclidine overdose are best managed by isolation from external stimuli. “Talking down” (eg, controlled breathing) is not effective. Severe hypertension (not hypotension) may occur and can be managed with diazoxide, a vasodilator. Elimination of phencyclidine can be accelerated by acidification (lowering the pH) of the urine with ammonium chloride. Acidification of the urine promotes phencyclidine excretion by reducing tubular reabsorption of this weak base.
Question 11
Which of the following is the most commonly abused opioid by healthcare providers?
Meperidine [Demerol]
Oxycodone [OxyContin]
Hydromorphone [Dilaudid]
Morphine sulfate
Answer: A
Rationale: Among healthcare providers who abuse opioids, meperidine is a drug of choice; meperidine is orally active, causes minimal pupillary constriction, and causes less constipation and urinary retention than other opioids.