The Urinary System
Beginning of PP#1
Functions of the Urinary System
- The most important function of the urinary system is to maintain homeostasis, which is the maintenance of a constant environment. The urinary system does this by:
- Filtering the blood to remove waste products, such as urea, which is the major byproduct of protein metabolism, creatinine which is the major byproduct of muscle metabolism, uric acid, and other waste materials.
- Maintaining the electrolyte/water balance in the body.
- Stabilizing blood pH by controlling the loss of hydrogen (H+ ) and bicarbonate (HCO3 - ) ions in the urine.
- Regulating blood volume and blood pressure by adjusting the water lost in the urine, releasing erythropoietin to stimulate the production of red blood cells, and releasing renin, which is an enzyme that causes an increased blood pressure.
- Converting the waste products and excess fluids in the body to urine, which takes place in the kidneys, and then excreting those substances from the body through the urinary bladder.
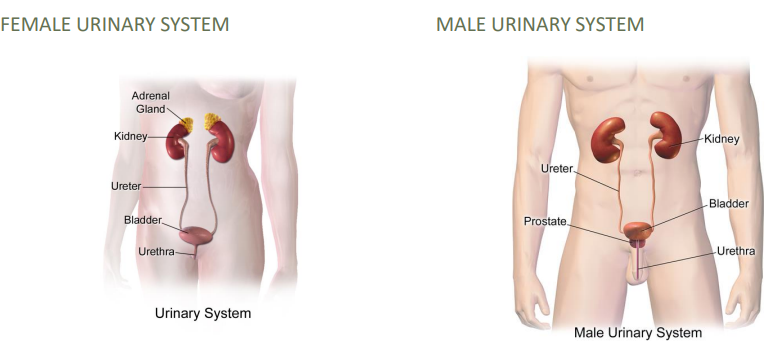
Urinary System Structure
The urinary system has six major structures: ◦ 2 kidneys ◦ 2 ureters ◦ 1 urinary bladder ◦ 1 urethra
Males also have a prostate which is actually part of the reproductive system, but surrounds the urethra, so it does play a role in the urinary system as well.
The Kidneys
- The kidneys are the major functional organ of the urinary system.
- They constantly filter the blood, removing waste products and excess water, and converting these substances to urine, which is excreted. This maintains fluid homeostasis.
- Urine consists of 95% excess water, and 5% urea and other waste.
- The kidneys filter about 50 gallons of blood each day, which produces about 2 quarts (or half a gallon) of urine.
- The kidneys also play a role in blood pressure maintenance, red blood cell production, and the activation of vitamin D through the release of hormones important in these processes.
The Kidneys: Overview
- The term renal is used to refer to the kidneys.
Ren/o means kidney
-al means pertaining to
- The kidneys are bean-shaped structures, with one located on each side of the vertebral column near the lower edge of the rib cage, and beneath the diaphragm. This area is also called the retroperitoneal space
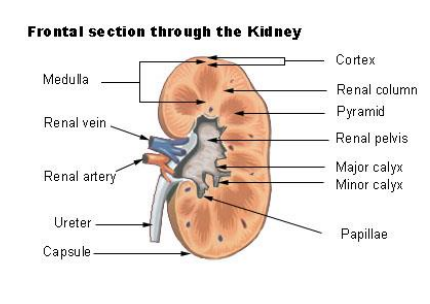
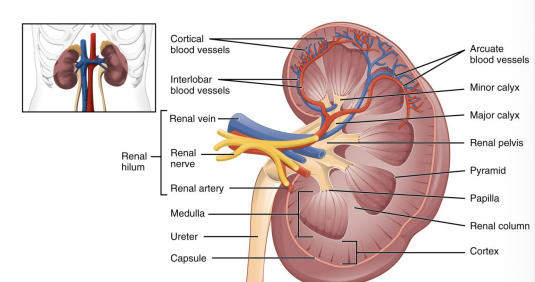
- There are two major regions of the kidney:
- The renal cortex is the outer layer of the kidney, which contains the millions of microscopic functional units of the kidney, which are called nephrons.
- The medulla is the inner region of the kidney, and contains the tubules, which are the urine-collecting structures of the kidney.
The Kidneys: Nephrons
- Nephrons are the microscopic functional units of the kidneys that produce urine through filtration, reabsorption, and secretion.
- Reabsorption is the process by which some of the substances filtered by the kidneys are returned to the blood.
- Blood enters the nephron at the renal artery, which takes oxygenated blood to the renal corpuscle, and the filtered, deoxygenated blood exits the kidney and returns to the bloodstream through the renal vein.
- Each nephron has some of its own specific structures:
- The nephron begins at the renal corpuscle which is also called Bowman’s capsule. This is a cupshaped chamber that contains the glomerulus, and is the site of filtrate production.
- The glomerulus is a capillary network, in which blood pressure pushes the fluid and dissolved substances out of the capillaries and into the space surrounding them, called the capsular space.
- The processes that occur in the renal corpuscle are called filtration, and result in a protein-free solution known as filtrate.
- The filtrate leaves the renal corpuscle and enters the renal tubule, which is composed of three distinct sections, which are the proximal convoluted tubule, the loop of Henle, and the distal convoluted tubule. Proximal refers to the area closest to the glomerulus, and distal refers to the area of the tubule furthest from the glomerulus.
- The renal tubule is where water, sugars, and salts are reabsorbed and returned to the bloodstream.
- The remaining filtrate moves through the renal tubule, where substances are reabsorbed into the bloodstream or secreted into the filtrate by the blood, depending on the body’s needs at that time.
- About 90% of the water that was originally in the filtrate is reabsorbed in the renal tubule. The concentrated urine then moves to the renal pelvis.
The Renal Pelvis
The renal pelvis, labeled on this image, is the area of the kidney that collects the urine from the nephrons.
It is a funnel-shaped area, which is surrounded by the renal cortex as well as the medulla.
The renal pelvis is continuous with the ureter, and the urine flows to the ureter when the renal pelvis fills.
Ureters
- Once the urine leaves the renal pelvis, it moves into the ureters which are two narrow tubes that connect the kidneys and the urinary bladder.
- The ureters are about 10-12 inches long.
- Through the action of peristalsis, which is a series of wave-like muscle contractions, and gravity, the urine moves down the ureter to the bladder.
- Ureteral orifices are present at the point where the ureter meets the urinary bladder, which are openings in the urinary bladder through which the urine enters the bladder.
The Urinary Bladder
- The urinary bladder is a hollow, muscular, oval-shaped organ that serves as the storage and collection area for urine before it is excreted from the body.
- The bladder is lined with rugaewhich are folds that allow it to expand when filled with urine, and to contract when it empties.
- It is located in the front part of the pelvic cavity, and can generally store more than one pint of urine.
The Urethra
- The urethra ) is the tube that spans from the bladder to the exterior of the body. *Note: The spellings of ureter and urethra are very similar! Remember that ureter comes first, both physically and alphabetically!
- The urethra contains two urinary sphincters, which are rings of muscle that contract and relax to control the flow of urine to and from the body.
- The internal urethral sphincter is the muscle that controls the flow of urine from the bladder.
- The external urethral sphincter is the muscle that controls the flow of urine from the body.
- The urethral meatus is the external opening of the urethra to the outside of the body.
Meatus means the external opening of a canal.
- The female urethra is about 1.5 inches long, and transports urine to the outside of the body. Due to its proximity to the vagina and external surfaces of the body, women are more susceptible to urinary tract infections.
- The male urethra is about 8 inches long, and transports both urine and semen. The prostate gland surrounds the urethra, and disorders of the prostate gland can affect the ability of a male to effectively urinate.
Urine Excretion
- The act of excreting urine is known as urination, voiding, or micturition.
- Urination occurs when the bladder fills with urine. This places pressure on the urethra, resulting in the urge to urinate, or micturate.
- Urination occurs because of the coordinated contraction of the bladder’s muscles as well as the rings of muscle of the sphincters.
Beginning of PP#2
The Urinary System Pathology
Kidney Pathology: Renal Failure
- Nepropathy is the general temr meaning any disease of the kidney
Nephr/o means kidney
-pathy menas disease
- Renal Failure is the inability of one or both kidneys to adequately perform their functions. This failure is the result of nephron destruction; the body cannot create new nephrons, so as they are lost, kidney function declines.
- Azotemia is the increase of blood urea nitrogen (BUN) caused by lack of blood flow to the kidney. Because blood cannot be filtered adequately, waste products in the form of urea nitrogen buildup in the blood.
Azot- means containing nitrogen
–emia means blood condition
- Uremia is the condition of blood toxicity resulting from kidney failure. As with azotemia, the urea and other waste products normally filtered by the kidneys are retained in the blood until they become toxic.
Ur/o means urine
- Acute Renal Failure e is renal failure with a sudden onset. This causes uremia, and can be due to the kidneys not receiving enough blood to filter adequately, or due to a sudden drop in blood pressure that prevents the kidneys from receiving enough blood to remove waste products.
- Chronic kidney disease is long-term renal failure that is characterized by the progressive loss of kidney function. This can occur over months or years, and can be life-threatening. This can happen because of untreated diabetes mellitus, hypertension, and other factors.
- *Note: The buildup of toxic substances in the blood as a result of chronic kidney disease is a contributing factor in heart disease and strokes.
- End-stage renal disease is fatal, and is the final stage of chronic kidney disease. Individuals with this must undergo dialysis or a kidney transplant to stay alive.
Kidney Pathology: Nephrotic Syndrome
- Nephrotic syndrome is actually a group of conditions that are characterized by excessive protein loss in the urine. These conditions cause decreased blood protein levels, and are caused by glomerular damage.
Nephr/o means kidney
–tic means pertaining to
- Nephrotic syndrome can be caused by a variety of issues, including diabetes mellitus, infection, and kidney disorders.
- In young children, minimal change disease is responsible for most cases of nephrotic syndrome.
- Edema is a symptom of nephrotic syndromes, and is the buildup of fluid in the tissues. This swelling can be anywhere in the body, but is most common around the eyes, legs and feet, and the abdomen.
- Hyperproteinuria is the condition of excessive amounts of protein in the urine.
Protein/o means protein
-uria means urine
- Hypoproteinemia is the condition of abnormally low levels of protein in the blood. Hyperproteinuria can cause hypoproteinemia
Hypo- means deficient
Miscellaneous Kidney Conditions
- Nephritis Is the inflammation of the kidneys which is most commonly caused by infection, toxins, or autoimmune disease
- Glomerulonephritis is the inflammation of the glomeruli that causes red blood cells and protein to leak into the urine. This causes pink or red-tinged urine, as well as high protein values in the urine.
Glomerul/o means “glomerulus
- Hydronephrosis is the swelling of one or both kidneys, which can be caused by the backup of urine due to an obstruction (such as a kidney stone) or narrowing of the ureter.
Hydr/o means water
-osis means disease
- Nephropyosis is also called pyonephrosis, and is the formation or discharge of pus by the kidney.
Py/o means pus
-osis means condition
- Renal Colic is acute pain in the kidney that is caused by a blockage created by a kidney stone.
- Colic is a term that means spasms of pain in the abdomen
- Renal colic pain can come in waves due to the wave-like actions of peristalsis.
- Polycystic kidney disease or PKD is a genetic disorder that causes the growth of numerous fluid-filled cysts in the kidney, which replace the mass of the kidney and destroy nephrons. This destruction leads to renal insufficiency, and eventual renal failure.
- A Wilms tumor is a rare, malignant tumor of the kidney that affects young children. Thankfully, it has a high success rate for treatment, if applied early.
- Nephroptosis is the prolapse of a kidney into the pelvis when the patient stands. Prolapse means “the slipping forward or down of a body part.” This condition is also known as floating kidney
Kidney Stones
- A stone, which is also called a calculus, is a mineral deposit that has formed in abnormally within the body. These are named for the body part in which they grow. Some may pass unnoticed and be as tiny as a grain of sand, while others may be as large as a marble, causing extreme pain.
- In the urinary system, waste products can crystallize to create calculi. Dehydration makes a person extremely prone to this, as dehydration upsets the balance of enzymes and chemicals that prevent crystallization.
- Nephrolithiasis is the presence of stones in the kidney. They can travel with the flow of urine, becoming lodged and causing pain.
-lithiasis means the presence of a stone
- A nephrolith is a stone in the kidney. They are also called kidney stones or renal calculi
-lith means stone
- An ureterolith is a stone located in the ureter.
Ureter/o means ureter
- A cystolith is a stone located in the bladder.
Cyst/o means urinary bladder
Pathology of the Ureters
- Hydroureter is the swelling of the ureter with urine that is unable to flow into the bladder because the ureter is blocked.
-ureter means ureter
- Ureterectasis is the swelling of a ureter due to hydroureter or congenital abnormalities.
-ectasis means enlargement
- Ureterorrhagia is the flow of blood from the ureter.
-rrhagia means bleeding
Urinary Bladder Pathology
- Vesicoureteral reflux is the backflow of urine into the ureters from the bladder. This is most common in infants and children, and is often the route of entry for bacteria into the kidney
Vesic/o means bladder
–al means pertaining to
- Cystalgia and cystodynia mean pain in the bladder
Cyst/o means bladder
–algia means pain
–dynia also means pain
- Interstitial cystitis is chronic inflammation of the walls of the bladder. Interstitial means “the spaces within a tissue or organ.
- A cystocele ) is also called a prolapsed bladder, and is the herniation of the bladder through the vaginal wall, which can sometimes occur due to pregnancy or childbirth
-cele means hernia
- A vesicovaginal fistula is an abnormal opening between the bladder and vagina that allows urine to flow from the bladder to the vagina. This can be caused by difficult delivery during childbirth, or even a surgery such as a hysterectomy.
- A fistula is an abnormal passage between two internal organs.
Vesic/o means bladder
vagin/o means vagina
Urinary Bladder Pathology: Neurogenic Bladder
Neurogenic bladder is a disorder caused by the interruption of the normal nerve pathways that control the bladder.
Neur/o means nerve
–genic means created by.
- Normal urinary function relies on the nervous system to sense when the bladder is full, and to control the muscles that retain urine and allow the bladder to empty.
- Neurogenic bladder disorders can cause the bladder to empty spontaneously, or prevent the bladder from emptying completely or at all.
- Neurogenic bladder can be caused by trauma, a tumor in the central nervous system, damage or disease of the nerves, or an inflammatory disease such as multiple sclerosis.
Prostate Gland Pathology
- Benign prostatic hyperplasia abbreviated BPH, is the enlargement of the prostate gland that occurs in men over the age of 50, which causes difficulty urinating due to the pressure placed on the urethra. This is also called benign prostatic hypertrophy and enlarged prostate.
Prostat/o means prostate
–ic means pertaining to
- Hyperplasia means “an increase in cell number,” and it is usually associated with tumor growth. In this case, no neoplasm or infection is the cause. Hyper- means “excessive,” and –plasia means “growth.”
- Prostatism describes the difficulty urinating due to compression or obstruction on the urethra due to BPH.
- Prostatitis is the inflammation of the prostate.
Prostat/o means prostate gland
- Chronic benign prostatitis is inflammation of the prostate with no known cause.
- Bacterial prostatitis is inflammation of the prostate due to bacterial infection transported by the urine.
- Prostate cancer is one of the most common cancers that afflicts men, and can be asymptomatic (no symptoms) and grow slowly, or be aggressive and life-threatening, spreading throughout the body.
Pathology of the Urethra
- Urethrostenosis is the narrowing of the urethra that is usually caused by scarring from infection or injury. This condition occurs almost exclusively in males, and is also known as urethral stricture. Stricture means narrowing
Urethr/o means urethra
-stenosis means narrowing or tightening
- Urethrorrhagia is bleeding from the urethra
- Urethrorrhea is an abormal discharge from the urethra , which is often associated with sexually transmitted diseases.
-rrhea means discharge
There are two terms that refer to abnormal urethral openings:
- Epispadias is a congenital abnormality of the urethral opening. In males, the urethral opening is located on the upper surface of the penis, and in females, the urethral opening is located in the region of the clitoris, rather than between the clitoris and the vagina.
Epi means above
-spadias means something torn
- Hypospadias is the congenital abnormality of the urethral opening. In males, the urethral opening is on the underside of the penis, and in females, the urethral opening is located in the vagina.
Hypo- means below
Urinary Tract Infections
- Urinary Tract Infections or UTI are bacterial infections that can affect any and all parts of the urinary system. Most UTIs are caused by Escherichia coli, or E. coli, and are the result of fecal contamination of the urethral opening. They usually begin in the bladder, and are more common in females due to how short the urethra is.
- Urethritis is the inflammation of the urethra due to a bacterial infection.
- Cystitis is the inflammation of the bladder due to a UTI.
- Pyelonephritis is the inflammation of the renal pelvis and kidneys due to a bacterial infection that has migrated up the ureter to the kidney.
Pyel/o means renal pelvis
Pathology of Urination
- The following terms are related to excessive urination:
- Diuresis is the increased output of urine
Di- means through
-uresis measn urination
- Polyuria is excessive urination and is common in individuals with diabetes
Poly- means many
-uria means urination
- Nocturia is excessive and frequent urination during the night
Noct/o means night
- The following terms are related to insufficient urination
- Anuria is the absence of urine formation by the kidneys which is often the result of kidney failure or a urinary obstruction.
An- means without
- Oliguria is decreased urinary output, which can be caused by dehydration, renal failure, or a urinary tract obstruction.
Olig/o means scanty
Urinary Difficulty
The following terms are related to urinary difficulty:
- Urinary hesitancy is difficulty beginning urination, which can be common in men with enlarged prostates, or in younger people with “shy bladder,” meaning they cannot urinate when another person is present.
- Urinary retention or ischuria , is the inability to completely empty the bladder when urinating. This is often also due to an enlarged prostate.
Isch means hold back
- Enuresis is the involuntary discharge of urine
En- means into
- Nocturnal enuresis or bedwetting is urinary incontinence during sleep.
- Dysuria is difficult or painful urination, which is common during UTIs.
Dys- means bad or painful
Urinary Incontinence
- Urinary incontinence is the inability to control the excretion urine. The term incontinence can also be applied to feces.
- Overflow incontinence is the continuous leakage of urine due to the bladder being too full or from incomplete voiding of the bladder. This condition usually affects men with enlarged prostates.
- Stress incontinence is the inability to control the voiding of urine during physical activity, such as running, sneezing, coughing, squatting, or laughing. This occurs more often in women than men, and can be the result of weak pelvic floor muscles due to pregnancy and childbirth.
- Overactive bladder is also called urge incontinence and is the involuntary contraction of the bladder muscles, even when it is not full enough to urinate. The urinary sphincters may react, causing increased urinary frequency or urinary leakage.
- This condition is common in older adults, and is exacerbated by the use of caffeine, alcohol, UTIs, neurological problems, or bladder or prostate problems.
Beginning of PP#3
Diagnostic and Treatment Procedures for the Urinary System
Medical Professionals
- Nephrologists are e physicians who specialize in diagnosing and treating disorders of the kidneys.
- Urologists are physicians who specialize in diagnosing and treating disease and disorders of the urinary system of both males and females.
- Urologists also specialize in the genital and reproductive system of males.
Ur/o means urine
-ologists means specialist
Diagnostic Techniques
- Bladder Ultrasound is the use of ultrasound, which are high-frequency sound waves, to produce an image of the bladder and prostate.
Ultra means beyond
- With this type of ultrasound, the physician can look for stones, enlargement of the prostate, and measure the amount of urine left in the bladder after voiding. This is used to diagnose a distended, or enlarged, bladder.
- Cystoscopy is the use of a cystoscope, which is a specialized endoscope, to visually examine the bladder. The cystoscope can also be used for the removal of tumors or the reduction of an enlarged prostate gland.
scopy means visual examination
- A voiding cystourethrography is the use of a fluoroscope to examine the flow of urine from the bladder through the urethra.
-graphy means the process of producing a picture or record
- Computed Tomography or CT , is the use of an X-ray beam to make an image of structures in the body. For the urinary system, it can provide a complete view of the abdomen, which could give clues to other issues that may be causing urinary tract symptoms.
- Nephrotomography is the use of CT to examine the kidneys
Diagnostic Technique: Radiographic Imaging
- Cystography is the use of x-rays to examine the bladder. This is done with the use of a constrant medium which is a susbtance used to aid in imaging. In the case of a cystography, it is introduced to the system via urethral catheter.
- Intravenous pyelography is the use of a contrast dye administered intravenously (through an IV line) to radiographically study the kidneys and ureters. This dye defines these structures, which allows for the diagnosis of nephrolitis, infections, an enlarged prostate, tumors, and internal injuries.
Intra- means within
ven/o means veins
-ous means pertaining to
pyel/o means renal pelvis
- A KUB (kidney, ureters, bladder) is a raradiographic survey of the kidney and bladder, without the use of a contrast medium. This is done to detect bowel obstruction and nephrolitis. Although “ureter” is in the name, this technique does not include the ureters.
- Retrograde urography is the radiographic examination of the urinary system after the application of a contrast medium through a catheter. The contrast medium moves through the urinary tract in the opposite direction that fluids usually flow, hence the name retrograde, which means backward.
Diagnostic Techniques: Laboratory Testing
Laboratory specimens for the urinary system are collected by a clean catch urination, in which urine is sterilely collected for examination, or by a urinary catheterization, which is the insertion of a tube into the bladder to remove sterile urine specimen
- Urinary catheterization is also used to void the bladder for patients that cannot do so, or to place medications into the bladder directly
Urinalysis is the clinical examination of urine, chemically and physically, to determine the presence of abnormal elements. Urinalysis can diagnose abnormal protein levels, blood in the urine, the presence of bacteria, the presence of drugs, or to determine pregnancy.
- A urinary culture and sensitivity is a test ordered after urinalysis is performed, especially if white blood cells and/or bacteria is seen in the urine. Urine is placed on a growth plate, and whatever bacteria grows is tested against antibiotics to see which would work best for that infection.
- The glomerular filtration rate (GFR) is a blood test done to determine how well the kidneys are filtering wastes from the blood
- Blood urea nitrogen (BUN) is another blood test that detemines how well the kidneys are filtering wastes from the blood by giving a quantitative level of urea nitrogen in the
Diagnostic Techniques: Prostate Gland
- A digital rectal examination is a physical test performed by a physician in which a gloved finger is placed in the rectum to check for the presence of an enlarged prostate or the presence of prostate or rectal tumors.
In this context, digital refers to the finger.
- The prostate-specific antigen (PSA) is analyzed using a blood test. The PSA is a protein produced by the prostate gland to help liquefy semen, but the higher the levels of PSA, the more likely the chance of prostate cancer. This test provides a quantitative measurement of how much PSA is present in the patient’s blood.
Treatment Procedures: Medications
- Diuretics are the most commonly prescribed medications that affect the urinary system. They increase urine secretion, helping rid the body of excess water and salt.
- These medications are given after open heart surgeries to keep water from building up in the body after surgery.
- Some foods and drinks have diuretic properties, such as coffee, tea, and alcoholic drinks.
- Nutritional and dietary considerations are important for people with kidney disease.
- Nutritional interventions for kidney disease are aimed primarily at controlling the amounts of certain substances that enter the body, including sodium, potassium, phosphorous, and protein.
Treatment Precedures: Dialysis
- Dialysis is the procedure used to compensate for kidneys that can no longer function. During dialysis, waste products such as urea, creatinine, and excess water are removed from the blood.
Dia means complete
-lysis means separation
- There are two types of dialysis
- Hemodialysis is the process of filtering wastes directly from the patient’s blood with the use of an external hemodialysis unit, also called an artificial kidney. This is the most common type of dialysis.
During hemodialysis, a shunt is placed in the patient’s arm that connects to the dialysis unit, and arterial blood flows through the machine. The machine contains a solution of water and electrolytes called dialysate, which cleans the blood by removing the waste products. The filtered blood is then returned to the body through a vein.
- In peritoneal dialysis, a catheter is placed in the peritoneal cavity, and dialysate is left for a period of time in that cavity, during which the waste products are absorbed and drained through the tube. This is done multiple times per day, and is considered less effective than hemodialysis.
Continuous ambulatory peritoneal dialysis is a type of peritoneal dialysis in which the dialysis continues as the patient goes about their daily life, and the dialysate container is carried under the patient’s clothing. Continuous cycling peritoneal dialysis is peritoneal dialysis that continues during the night while the patient sleeps.
Treatment Procedures: The Kidneys
- Nephrostomy is a treatment procedure for a kidney affected by hydronephrosis, or to gain access to the kidneys for diagnostic procedures. In this procedure, a catheter is placed through an opening in the pelvis into one or both kidneys to the exterior of the body
- Pyelotomy is the surgical incision into the renal pelvis, which can be performed to correct obstructions.
-otomy means surgical incision o surgical removal
- Nephrolysis is a surgical procedure to free the kidney of adhesions, or bands of fibers that hold structures abnormally.
-lysis can mean destruction or setting free
so nephrolysis can also mean “destruction of kidney cells
- Renal Transplatation is the end stage e treatment for renal disorders, and is the grafting of a donor kidney into the body of a recipient to replace failed kidneys. The kidney donor can be living or deceased, and do not need to be related to the recipient. A single kidney can adequately perform all of the kidney functions for the body.
Kidney Transplant
- After a kidney transplat the blod flow is diverted to the transplanted and healthy kidney
Treatment Procedures: Kidney Stones
- Often, kidney stones (nephroliths) pass through the urinary tract without intervention, albeit painfully.
- There are two main interventions for kidney stones that are too large to pass naturally:
- Extracorporeal shockwave lithotripsy ) is the most common treatment, and is the use of high-energy ultrasonic waves that travel through a water or gel placed on the outside of the body to break the stone into fragments small enough to pass naturally in the urine
Extra means outside
-coporeal measn pertaining to the body
- Percutaneous nephrolithotomy is a surgical procedure in which the kidney stone is removed through a small incision into the back. This procedure is used if extracorporeal shockwave lithotripsy is not successful. An incision is made into the back and kidney, and a tube is inserted, through which urine is removed. The kidney stone is then crushed and the pieces are removed.
Percutaneous means through the skin
lith/o means stone
Treatment Porecedures: Ureters
- Ureteroscopy is the use of a ureteroscope, which is a specialized endoscope, to remove a kidney stone lodged in the ureter. If the stone cannot be removed in one piece, it is broken apart with a laser and the pieces are then removed.
- Ureterorrhaphy is the surgical incision of a ureter
rrhaphy means surgical suturing
- A ureterectomy is the surgical removal of a ureter
ectomy means surgical removal
Treatment Procedures: Urinary Bladder
- A lithotomy is the surgical incision into the bladder to remove a nephrolith, or kidney stone. This term is also used to describe the position of the body for certain examination procedures involving the lower abdomen and pelvis, since it is the position used for the removal of a nephrolith.
- Cystorrhaphy is the surgical suturing of a wound or anatomical defect in the bladder
- Cystectomy is the surgical removal of the urinary bladder, either partially or completely, usually as the treatment of bladder cancer.
- A cystopexy is the surgical fixation of the bladder to the abdominal wall.
pexy means surgical fixation
- An ileal conduit is the use of a piece of small intestine to transport urine to the ureters and an abdominal stoma.
Ile/o means small intestine
al means pertaining to
Treatment Procedures: Urinary Catheterization
- Urinary Catheterization is the insertion of a tube to withdraw urine from the bladder for diagnostic purposes, to allow urine to drain from the bladder freely in cases when patients cannot urinate, or to introduce medications or substances into the bladder. There are various types of catheters:
- An indwelling catheter is one that remains inside the body for a prolonged period of time.
- An intermittent catheter is one that is inserted several times per day to drain urine from the bladder.
- An intermittent catheter is one that is inserted several times per day to drain urine from the bladder.
- Urethral catheterization is a catheter inserted through the urethra and into the bladder.
- Suprapubic catheterization is the placement of a catheter through a small incision into the abdominal wall, just above the pubic bone.
supra means above
pubic means pubic bone
Treatment Procedures: Urinary Incontinence
- Kegel exercises are pelvic muscle exercises that are designed to strengthen the muscles of the pelvic floor.
- They can be used to help with urinary incontinence in both men and women.
- In men, they can be used to help treat prostate swelling and pain.
- In women, they can be used to condition the muscles of the pelvis during childbirth to help with recovery.
- Bladder Retaining is a behavioral therapy in which the patient urinates on a schedule, gradually increasing the length of time between which they urinate. This helps, with time, to break the cycle of urinary frequency and urgency related to urge incontinence.
Treatment Procedures: The Urethra
- Urethroplasty is the surgical repair of the urethra, due to damage or a defect.
plasty measn surgical repair
- A urethrotomy is a surgical incision into the urethra to correct an abnormal narrowing of the urethra, known as a stricture.
- A meatotomy is the surgical incision into the urethral meatus to enlarge the opening to the outside of the body
Meat/o means meatus
Treatment Procedures: The Prostate
- A prostatectomy is the partial or complete surgical removal of the prostate gland. This is done in case of prostate cancer, or to help relieve symptoms due to an enlarged prostate.
- A prostatectomy can lead to erectile and urinary dysfunction, so its use is reserved for severe cases.
- A transurethral prostatectomy (TURP) is one that is performed with the use of a resectoscope which is an endoscopic instrument that is inserted into the penis to remove excess tissue from an enlarged prostate. The most common complication from TURP is retrograde ejaculation, in which the semen flows backwards into the bladder instead of out of the body through the penis.
Trans measn through
- An ablation is a procedure used to treat some types of prostate cancer, which is the removal of a body part or the destruction of its functions through various means. These processes can include the use of surgery, drugs, hormones, heat, chemicals, and electrocautery. Electrocautery is the use of electrical current to destroy tissue.