Week 6
Types of Psychotic Disorders
Schizophrenia:
Lasts at least six months, with at least one month of two or more of the following: delusions, hallucinations, disorganised speech, grossly disorganised or catatonic behaviour and/or negative symptoms.
Schizotypal (Personality) Disorder:
A pattern of pervasive social and interpersonal deficits and cognitive or perceptual distortions and eccentricities of behaviour beginning before early adulthood.
Schizophreniform Disorder:
Equivalent to schizophrenia except the disturbance is of lesser duration (one to six months).
Schizoaffective Disorder:
The co-occurrence of the symptoms of schizophrenia and a major mood episode, in addition to at least a two-week period of delusions or hallucinations without mood disturbance.
Mood symptoms are present for the majority of the total duration of the disorder.
Delusional Disorder:
At least one month of delusions.
Brief Psychotic Disorder:
A psychotic disturbance lasting more than one day but less than a month with eventual return to premorbid levels of functioning.
Psychotic Disorder due to another medical condition:
Prominent hallucinations or delusions that are the direct physiological consequence of another medical condition.
Substance/Medical-Induced Psychotic Disorder:
Delusions and/or hallucinations that develop during or soon after substance intoxication or withdrawal, or after exposure to medication.
Other specified schizophrenia spectrum and other psychotic disorder:
Symptoms of psychosis that cause clinically significant distress or impaired functioning, but do not meet the full criteria for any other psychotic disorders.
Specific reasons for why the criteria for another disorder is not met must be specified by the clinician (e.g., persistent auditory hallucinations in the absence of other psychotic features).
Unspecified schizophrenia spectrum and other psychotic disorder:
Symptoms of psychosis that cause clinically significant distress or impaired functioning, but do not meet the full criteria for any other psychotic disorders.
The clinician is not required to specify the reasons why the criteria for this diagnosis are not met.
The History of Schizophrenia
Emil Kraepelin:
Dementia praecox.
Incorporated hebephrenia, catatonia, and paranoia.
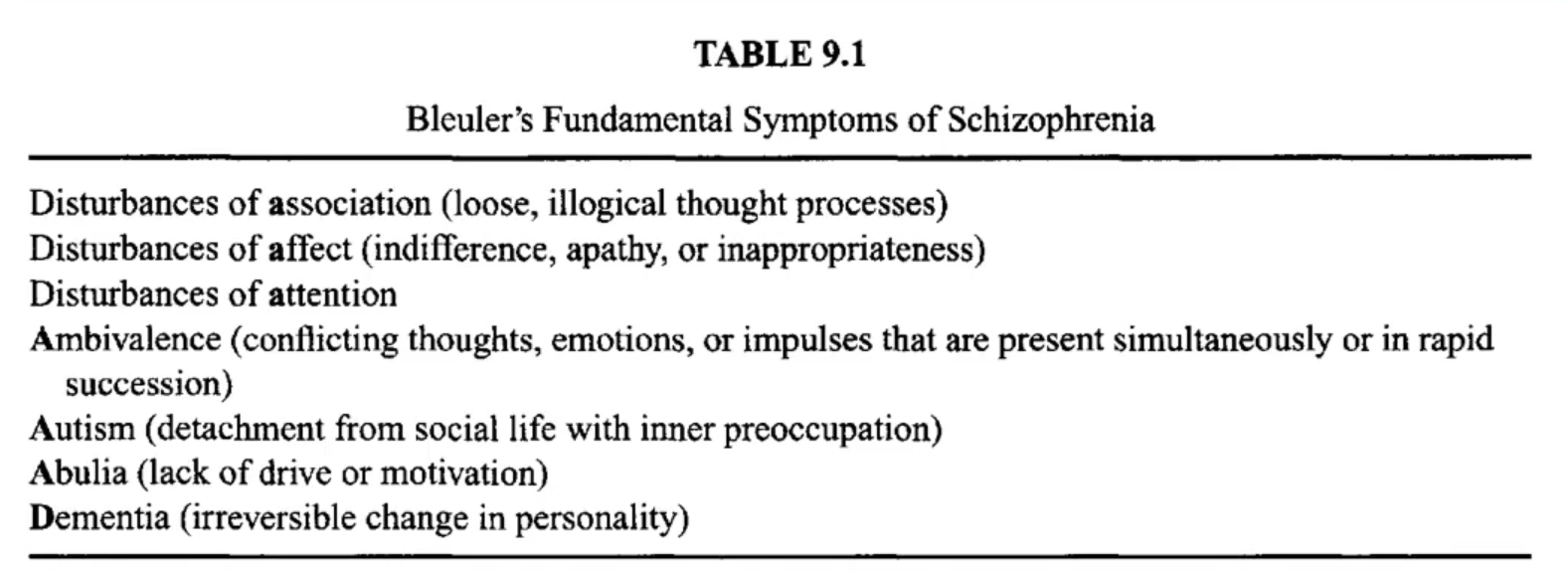
Eugen Bleuler:
First use of the term “schizophrenia.“
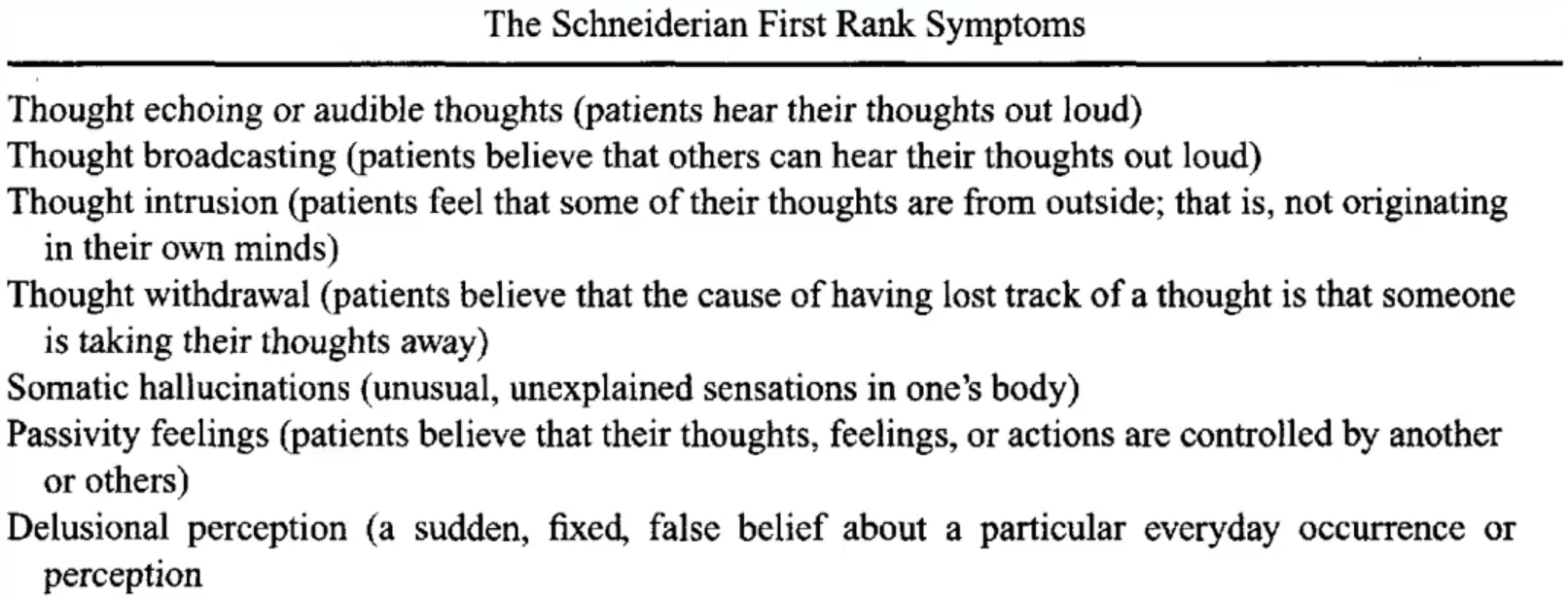
Kurt Schneider:
Listed “first rank” symptoms of schizophrenia.
First rank symptoms are the prototypical or most important symptoms of schizophrenia.
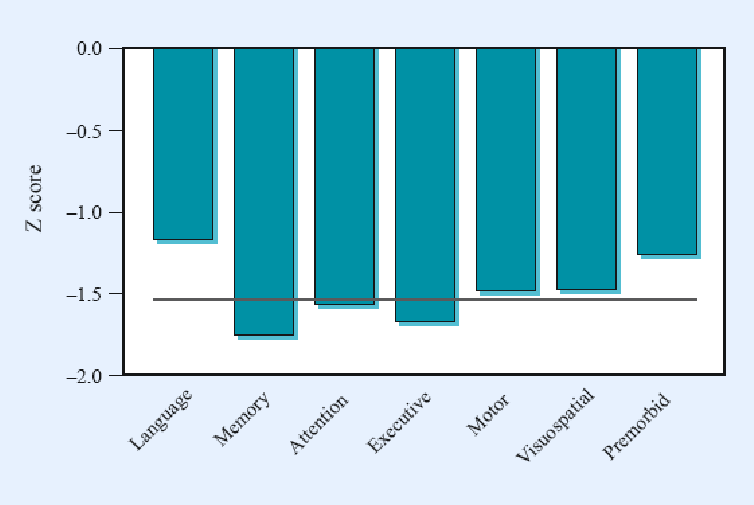
Symptoms of Schizophrenia
Positive Symptoms:
Delusions: beliefs that are rigidly held, despite contradictory evidence or bizarreness.
Hallucinations: perception of sensory stimulus in the absence of that stimulus.
Passivity Phenomena: individuals believe that their behaviour, thoughts, and urges are being controlled by an external agent.
Negative Symptoms:
Affective flattening.
Restricted emotional range.
Amotivation/abulia/avolition.
Apathy.
Social withdrawal.
Poverty of thought.
Poverty of speech.
Poor attention.
Disorganisation Symptoms:
Formal thought disorder.
Loosening of associations.
Clang associations/pun associations.
Word salad.
Circumstantiality.
Tangentiality.
Neologisms.
Derailment/Knight’s move thinking.
Catatonic Symptoms:
Ambitendence: alternation between opposite movements.
Echopraxia: automatic imitation of another person’s movements even when asked not to.
Stereotypies: repeated regular fixed parts of movement (or speech) that are not goal directed (e.g., moving the arm backwards and not outwards repeatedly while saying ‘but not for me’).
Negativism: motiveless resistance to instructions and attempts to be moved, or doing the opposite of what is asked.
Posturing: adoption of inappropriate or bizarre bodily posture continuously for a substantial period of time.
Waxy flexibility: the patient’s limbs can be ‘molded’ into a position and remain fixed for long periods of time.
Types of Hallucinations
Auditory Hallucinations:
Perception of a sound without external stimulus.
Content of hallucinations may include voices, music, or sounds.
Voices can be heard in second person (“you are…”) or third person (“she is…”) and often comment on the individual, argue about the individual, or repeat the individual’s thoughts.
Most common form of hallucination reported in schizophrenia, occurring in 60-70% of cases.
Visual:
Seeing things which are not present.
Do not reconcile with the physical reality.
Content of hallucinations may include shapes, colours, flashes of light, and other people.
Much less common in schizophrenia, occurring in only 10% of cases.
Generally thought to suggest the presence of an organic disorder, or intoxication.
Olfactory:
Smelling odours that are not present.
Most common olfactory hallucinations are usually unpleasant smells including rotting flesh, vomit, urine, faeces, and smoke.
Tactile:
The illusion of tactile sensory input, stimulating the skin or other organs.
Formication: formica = ant, the sensation of bugs crawling along the skin.
Often associated with drug and/or alcohol withdrawal.
Gustatory:
Perception of taste without a stimulus.
Fairly prevalent in individuals with epilepsy.
Often associated with psychoactive substances.
Usually, the taste is unpleasant including metallic, bitter, rusty, and salty.
Hypnagogic and Hypnopompic
Hypnagogic: brief hallucinations that take place as you're falling asleep.
Hypnopompic: occur as you're waking up from sleep.
Types of Delusions
Paranoid Delusion:
A false belief that one is being persecuted, harmed, or conspired against by others.
Individuals experiencing paranoid delusions may interpret benign actions as threatening and may feel an intense sense of mistrust towards others.
Persecutory Delusion:
Persecutory delusions occur when paranoia becomes extreme.
A person’s paranoid feelings become fixed beliefs, even when they’re presented with opposing evidence.
Delusion of Reference:
An individual believes that common elements of the environment, such as conversations, events, or media, are directly related to them or have special significance.
Grandiose Delusion:
A false belief characterised by an individual's conviction that they possess exceptional abilities, wealth, or fame.
This condition is marked by inflated self-esteem and a sense of self-importance, often leading individuals to believe they have special powers or talents.
Delusion of Influence:
A belief that one's thoughts, feelings, or actions are being controlled or influenced by external forces.
Feeling manipulated by others or external entities
They include delusions of control, i.e., the (false) belief of external influence on thoughts, feelings, impulses, or behaviours, as also manipulations of thoughts, such as thought insertion, withdrawal, and broadcasting.
Nihilistic Delusion:
An individual believes that they, others, or the world do not exist or have no meaning or value.
This delusion can manifest as feelings of emptiness, despair, or the belief that life is pointless.
Bizarre Delusions:
False beliefs that are implausible and not grounded in reality.
They often involve scenarios that are highly unlikely or impossible, such as believing that one has been abducted by aliens or that one's thoughts are being controlled by external forces.
Capgras’ Syndrome:
A psychological condition where a person believes that someone they know has been replaced by an identical impostor.
This delusion often affects close relatives or friends.
The syndrome is named after Joseph Capgras, a French psychiatrist who first described it in 1923.
Delusions of Infidelity:
Also known as the "Othello syndrome," involve a false belief that a partner is being unfaithful.
Individuals experiencing this delusion may interpret benign behaviours as evidence of infidelity, leading to jealousy and mistrust.
Delusions of Thought Possession
Thought Insertion:
An individual believes that thoughts that are not their own are being placed into their mind by an external force.
Thought Withdrawal:
The belief that one's thoughts are being taken away or removed by an external force, leading to a sense of loss of control over one's own mind.
Though Broadcasting:
The belief that one's thoughts are being transmitted to others and can be heard or perceived by them.
Thought Blocking:
A phenomenon where an individual suddenly stops speaking or loses their train of thought.
Relationship of Positive Symptoms
Delusions are often congruent with the hallucinations the patient is experiencing.
The paranoid delusion that others are trying to poison them, along with an olfactory hallucination of poisonous gas.
The religious/grandiose delusion that one has been appointed by God, accompanied by auditory command hallucinations.
Diagnosis of Schizophrenia
A. Characteristic symptoms: Two (or more) of the following, each present for a significant portion of time during a 1-month period 9or less if successfully treated):
Delusions.
Hallucinations.
Disorganised speech (e.g., frequent derailment or incoherence).
Grossly disorganised or catatonic behaviour.
Negative symptoms (i.e., affective flattening, alogia, or avolition).
Note: only one Criterion A symptom is required if delusions are bizarre or hallucinations consist of a voice keeping a running commentary on the other person’s behaviour or thoughts, or two or more voices conversing with each other.
B. Social/occupational dysfunction: for a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care are markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, failure to achieve expected level of interpersonal, academic, or occupational achievement).
C. Duration: continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences).
Subtypes of Schizophrenia
Paranoid:
Preoccupation with delusions and hallucinations.
Later onset, and better prognosis.
Disorganised:
Disorganised speech, behaviour and inappropriate or flat affect.
Catatonic:
Motor and volition disturbance.
Undifferentiated:
The individual exhibits the characteristic symptoms of schizophrenia but the overall picture is not one of catatonic type, paranoid type, or disorganised type schizophrenia.
Residual:
An individual has suffered an episode of schizophrenia but there are no longer any delusions, hallucinations, disorganised speech or behaviour.
Prevalence of Schizophrenia
Point-prevalence of 0.5% to 1.5%.
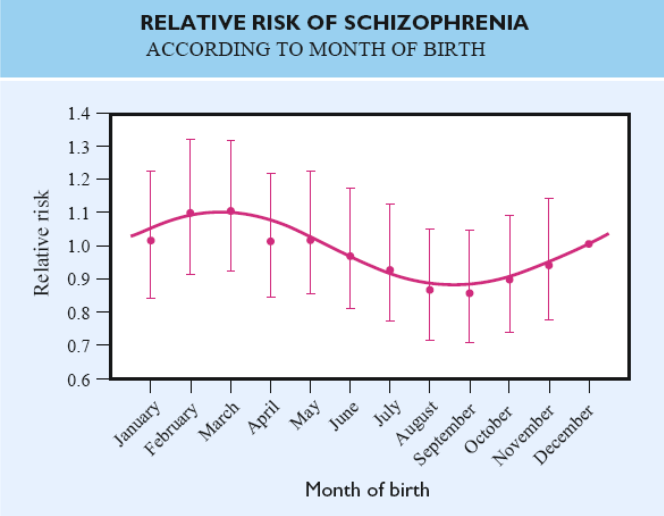
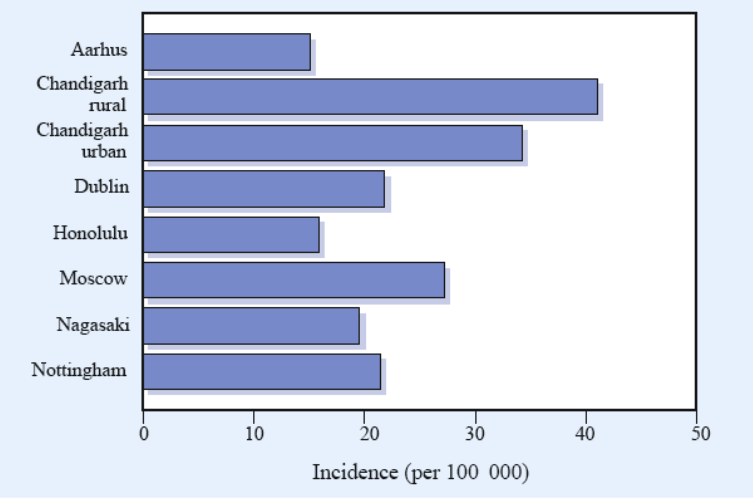
Prevalence varies by birth month, gender, distance from the equator, and socioeconomic status.
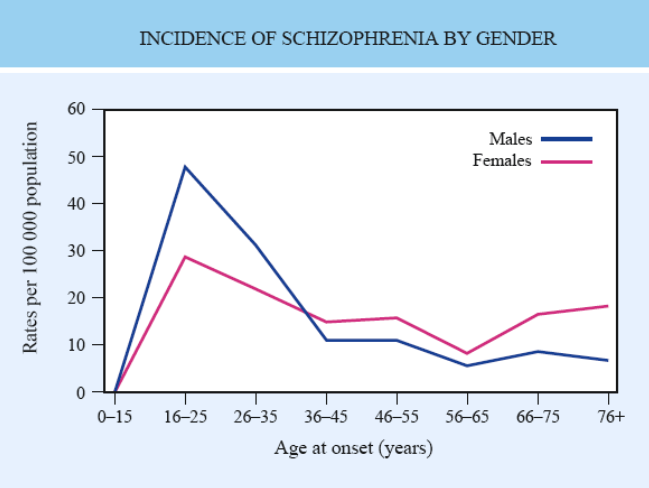
Age of Onset
Risk: Birth Month
Risk: Geographic Differences
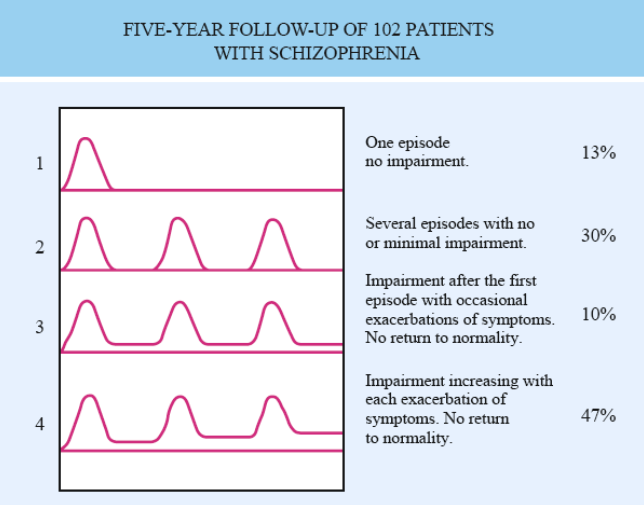
Course of Schizophrenia
Median onset is approximately the mid-20s for males and late-20s for females.
Onset may be abrupt or insidious.
Prodromal symptoms are common including social withdrawal, apathy, unusual beliefs, and oddness.
Later onset is associated with better prognosis.
Etiology of Schizophrenia
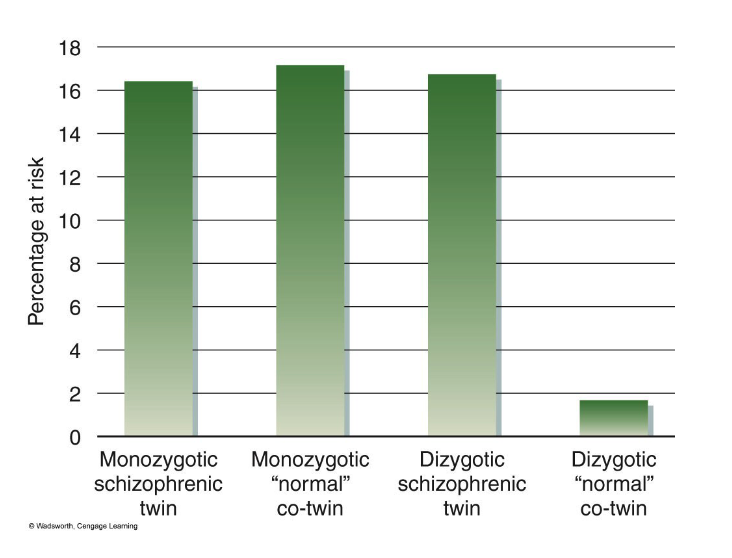
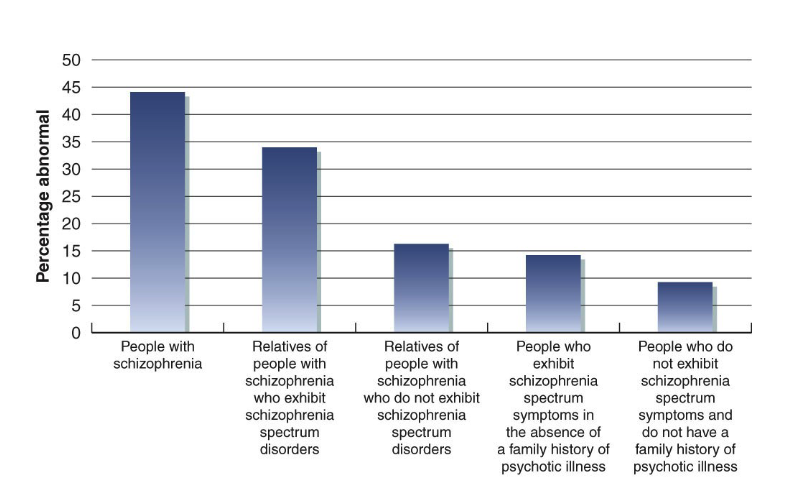
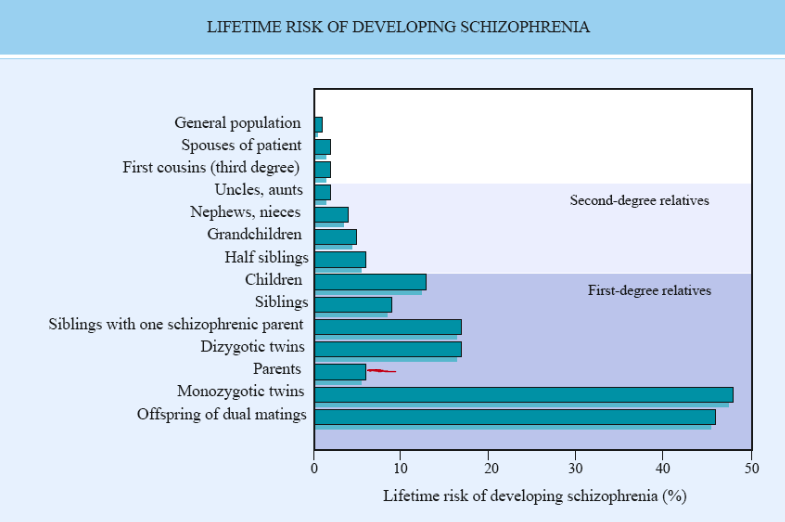
Genetics and Schizophrenia:
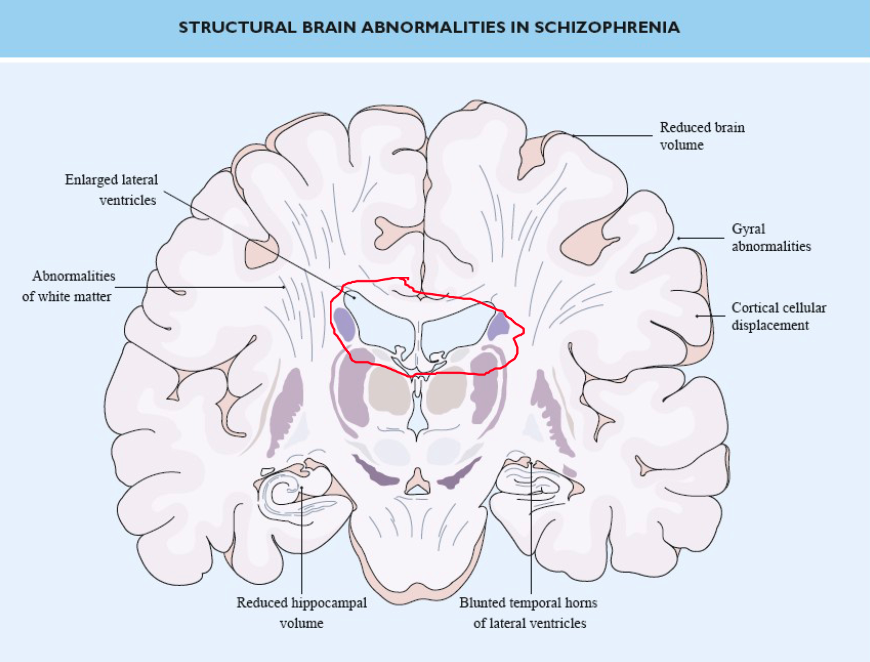
Dopamine Pathways:
Mesolimbic dopamine pathway from the midbrain ventral tegmental area to the nucleus accumbens (limbic system).
Includes experiences of pleasure, euphoria, delusions, and hallucinations.
Mesocortical dopamine pathways from the midbrain ventral tegmental area to the limbic cortex.
includes experiences of negative and cognitive symptoms of schizophrenia.
Through the pre-frontal cortex includes motivation and emotional response.