Animal Physiology Exam 1
Lecture 1/2: Homeostasis
Homeostasis: taking action to keep body processes functioning to
maintain a “set point.”
Maintains Homeostasis through: Feedback Loop (Negative and Positive) and Law of Mass Balance
Law of Mass Balance: Law states that if the amount of a substance in the body is to remain constant, any gain must be offset by an equal loss.
Homeostatic Control Systems:
Local Control: a response restricted to the area
where the change happened. This is a response
at the cellular or tissue level
Reflexive Control: A long-distance response that
uses Neurological or Endocrine signaling (or both)
Input Signal→ Integrating Center→ Output Signal
Biological Rhythms: Patterns of physiological changes that follow a regular cycle, often influenced by environmental cues such as light or temperature.
Equilibrium ≠ Homeostasis
External environment → Extracellular Fluid (ECF) →|Cell Membrane| Intracellular (ICF)
Homeostasis and equilibrium are not the same- Equilibrium implies that the two compartments are of identical composition; the ICF and ECF exist in a state of disequilibrium called Dynamic Steady State
Starling Forces
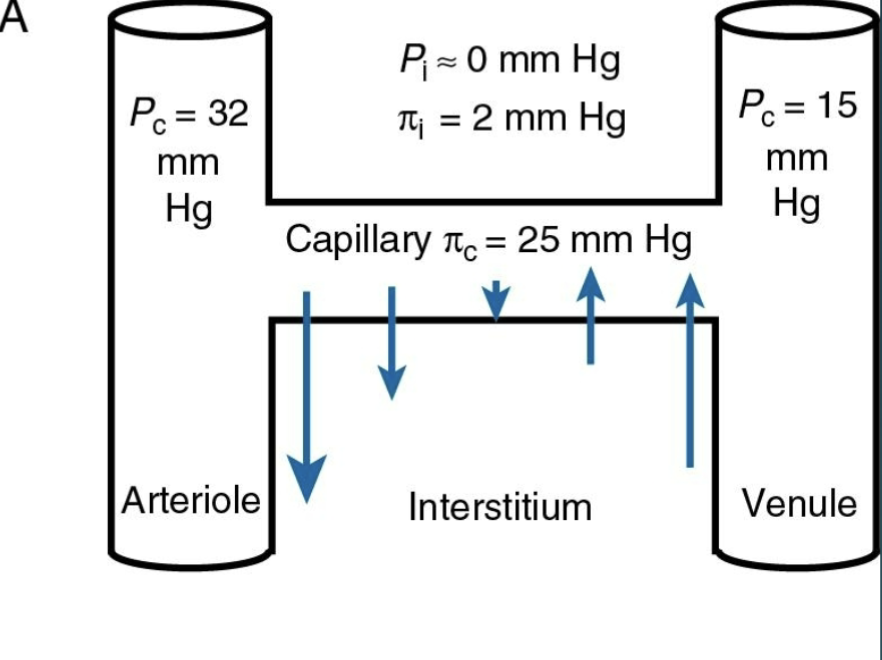
Forces that influence the movement of fluid.
Pi= Oncotic Pressure (pulling)
P= Hydrostatic Pressure (Pushing)
Body Fluid Compartments:
TOTAL BODY MASS (BM)- The 60-40-20 Rule
Total Body Water (TBW)= 60% of total body weight
2/3 is ICF (40% BM)
1/3 is ECF (20% BM) — 75% is interstitial (ISF) (15% of total BM)
25% is plasma (PV) (~5% of total BM)
Calculating TBW, ICF, ECF, ISF, and PV:
Determine the TBW, ICF, ECF, ISF and PV in a 40kg person and an 85kg person.
40kg Person:
TBW: 40kg x 0.6 = 24L
ICF: 24L x 2/3= 16L
ECF: 24L x 1/3= 8L
ISF: 8L x 3/4= 6L
PV: 8L x 1/4= 2L
85kg Person:
TBW: 85 × 0.6= 51L
ICF: 51L x 2/3= 34L
ECF: 51L x 1/3= 17L
ISF: 17L x 3/4= 12.75
PV: 17L x 1/4= 4.25
Practice Problem for you to try on your own- Calculate the Body fluid measurments for a 65kg person (Click Triangle at start of heading to reveal answers):
TBW: 65kg x 0.60= 39L
ICF: 39L x 2/3= 26L
ECF: 39L x 1/3= 13L
ISF: 13L x 3/4= 9.75L
PV: 13L x 1/4= 3.25 L
Lecture 7: Intro to Action Potentials
Resting Membrane Ions:
Na+ → outside
K+ → inside
Ca2+ → outside
Cl- → outside
Protein → inside
Think of “Salty Banana in Milk” for remembering where the ions are in regard to the cell membrane
Resting Membrane Potential (RMP) Maintained by Potassium Leak Channels
Cell Membrane Receptors
The most rapid signal pathways change ion flow through channels:
Ligand Gated
Mechanically Gated
Voltage Gated
Always open
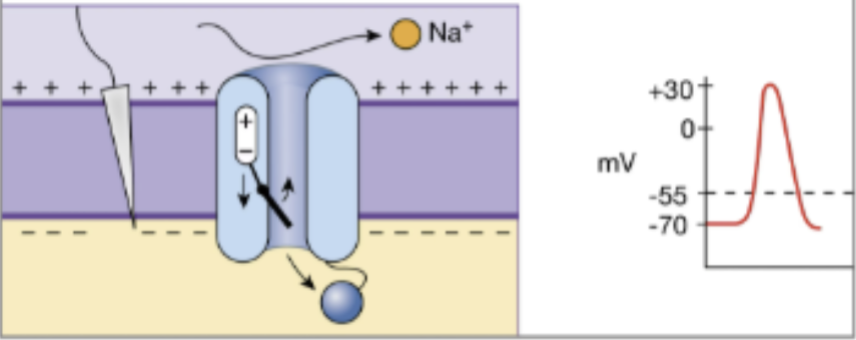
Voltage-Gated Sodium Channel
a) At the resting membrane potential, the Activation Gate is Closed; the Inactivation Gate is open
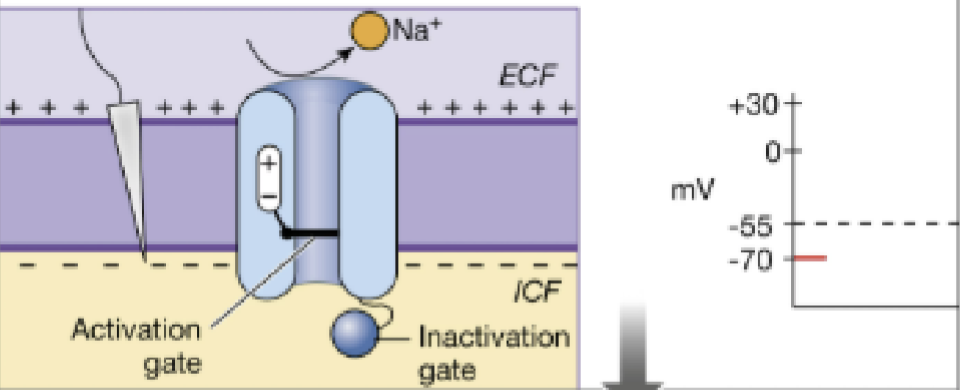
b) A depolarizing stimulus arrives at the channel, causing the Activation Gate to Open; Inactivation Gate is still open
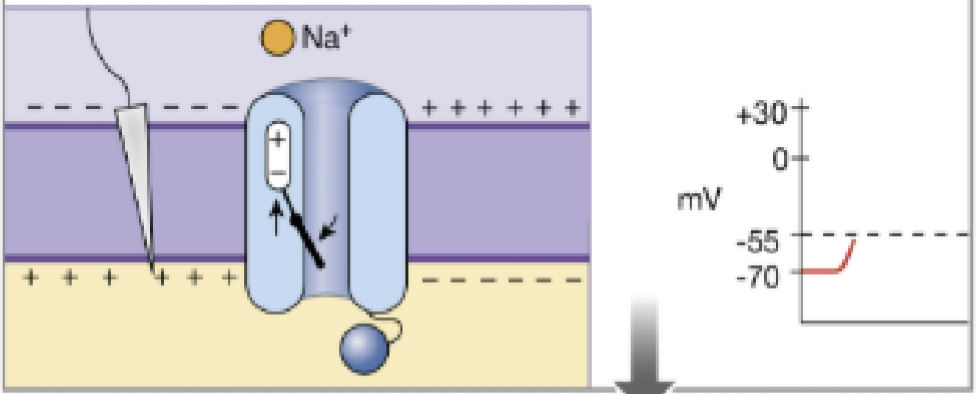
c) With both the Activation Gate and the Inactivation Gate open, Na+ enters the cell.
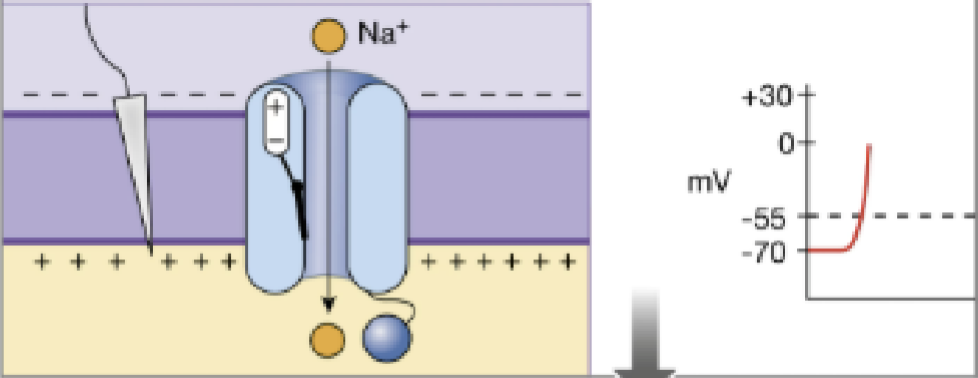
d) Inactivation Gate closes and the Na+ entry stops- refractory period.
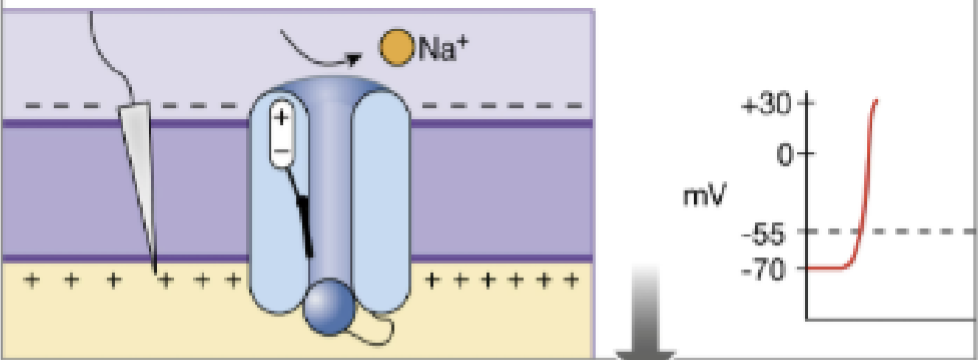
e) During repolarization caused by K+ leaving the cell, the two gates reset to their original positions.
Efferent v Afferent
Efferent: Side outgoing→ signal of the presynaptic neuron
Afferent: Side incoming→ signal of the postsynaptic neuron
Synapse: The region where an axon terminal communicates with its postsynaptic target cell; made up of the presynaptic axon terminal, the synaptic cleft, and the postsynaptic dendrite
Membrane Potentials: Resting, Graded, and Action
When cells are able to change their membrane potential in response to a stimulus they are called excitable
Gated Potential: subthreshold changes in membrane potential due to chemically gates channels opening and closing
Action Potential: starts when membrane potential voltage crosses threshold
Threshold: The critical voltage that a cell’s membrane must reach to trigger an “all or none” action potential→ typically -55mv.
Subthreshold Graded Potential: A graded potential starts above threshold (T) at its initiation point but decreases in strength as it travels through the cell body. At the trigger zone, it is below threshold and therefore does not initiate an action potential.
Suprathreshold Graded Potential: A stronger stimulus at the same point on the cell body creates a graded potential that is still above threshold by the time it reaches the trigger zone, so an action potential results
EPSP- Excitatory Post-Synaptic Potential
IPSP- Inhibitory Post-Synaptic Potential
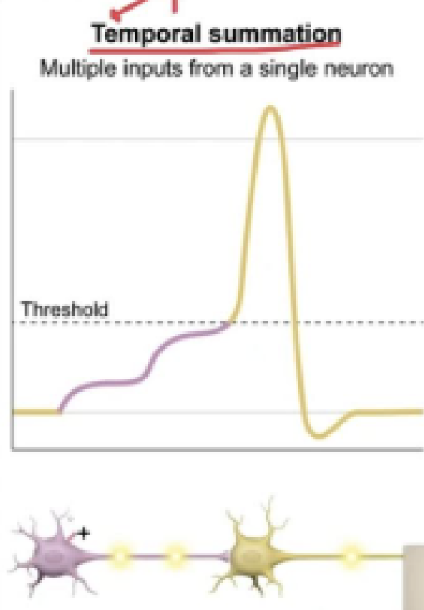
Temporal Summation: Occurs when two graded potentials from one presynaptic neuron occur close together in time. If close enough together in time, it can summate and reach threshold at the trigger zone and initiate an action potential. ESPS’s added up essentially.
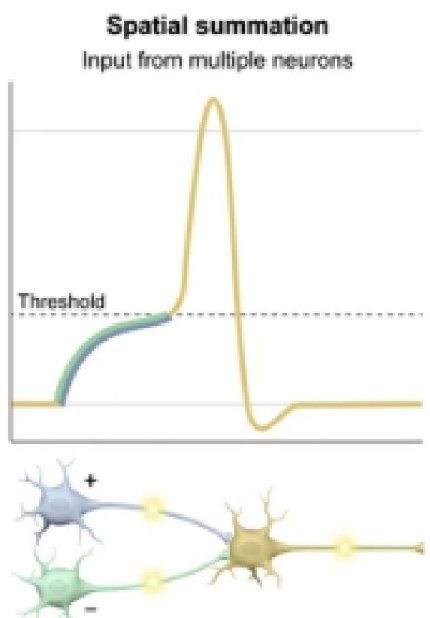
Spatial Summation: Summation of several subthreshold signals results in an action potential.
Anatomy of an Action Potential
The Action Potential begins at the Axon hillock and travels along the axon all the way to the synapse at the post-synaptic neuron
Action potentials are not generated at the Dendrites or the Cell Body of the Neuron
Action Potentials start when the voltage crosses the Threshold Potential due to Voltage-gated channels opening and closing
Presynaptic Neuron:
Voltage-regulated calcium channels are triggered by an action potential, causing them to open. Ca2+ flows into the axon terminal. (Remember our salty b
Ca2+ then triggers changes in the proteins of the presynaptic membrane and synaptic vesicles. Ca2+ causes the synaptic vesicles to fuse with the membrane of the presynapitc axon terminal. The inside of the synaptic vesicle is now in communication with the synaptic cleft.
Neurotransmitter is released into the synaptic cleft by diffusion.
Postsynaptic Neuron:
The neurotransmitter is now moving across the synaptic cleft to bind to the chemically regulated receptors of the postsynaptic dendrite’s membrane or target cell.
Chemically regulated Na+ channels open and sodium enters, following the concentration gradient.
Na+ diffuses across the cell body and starts depolarizing- if it reaches the axon hillock with enough Na+ to reach threshold, the action potential is carried down the axon to trigger voltage-regulated Na+ channels at the axon terminal (Shit starts over).
The axon that has carried the initial action potential down the axon then enters a refractory period and will not be activated again until resting-membrane potential is restored.
Continuous Conduction v. Saltatory Conduction
Continuous occurs in non-myelinated axon
Saltatory occurs in myelinated axon
Lecture 6: Cell Communication
Local Communication:
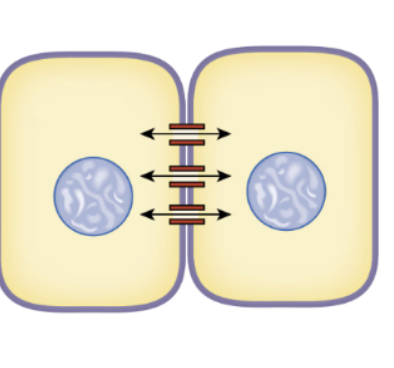
Gap Junctions- Connexins
form direct cytoplasmic connections/ bridges between adjacent cells
the most direct and rapid form of communication
Contact Dependent Signals- Surface molecules (Cell Adhesion Molecules/ CAMs) from one cell bind to CAMs from another cell.
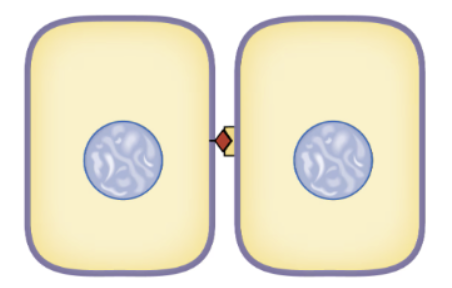
Chemical Diffusion- chemicals sent to cells close by- either Paracrine or Autocrine Signals.
Autocrine signals act on the same cell that secreted them
Paracrine signals are secreted by one cell and diffuses to adjacent cells
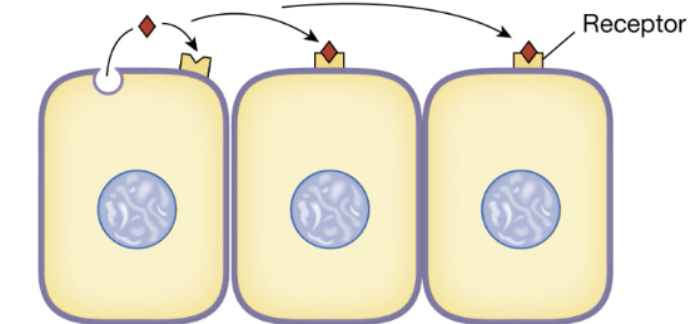
Long-Distance Communication
Can be either electrical, chemical, or both electro-chemical. The Major type of Cell Communication. However, only a cell with the appropriate receptor protein can bind to the chemical signal.
Ligand- The signal molecule that binds to the receptor and initiates a response.
Agonist- a molecule that also activates the receptor and triggers a response
Antagonist- a molecule that binds to and block the activity of a receptor
Cell Membrane Receptors- Gated Ion Receptors
Gated Ion Channels
The most rapid signal pathways change ion flow through channels:
Ligand-Gated- These are also known as Chemically gated Channels (Ligand = Chemical). The binding of the ligand to the receptor causes the channel to open, changing the permeability of the cell and the ion composition of the ICF/ECF
Voltage Gated- the voltage-gated sodium channel exists in one of three states, only one of which is open:
the closed (resting) state: activation gate closed, inactivation gate open (channel closed)
the open (activated) state: activation gate open, inactivation gate open (channel open)
the inactivated (refractory) state: activation gate closed, inactivation gate closed (channel closed)
Mechanically Gated
Always open
G-Protein Coupled Receptors
G Proteins linked to amplifier enzymes make up the bulk of all known signal transduction mechanisms
Includes a 7 Transmembrane Receptor and a trimeric G-Protein with three subunits: Alpha, Beta, + Gamma.
Alpha subunit activates adenylyl cyclase.
The two common amplifier enzymes for GPCR’s are Adenylyl Cyclase and Phospholipase C
The Main GPCR Pathways are:
cAMP Pathway (G alpha s)
PLC Pathway (G alpha q)
cAMP = Cyclic Adenosine Monophosphate-
Major Functions:
1) Second Messenger that amplifies the original signal
2) Activation of Proteins- Most importantly, Protein Kinase A, which Phosphorylates enzymes, ion channels, and transcription factors
3) Regulation of MANY Cell Processes
Activated G Alpha s subunit activates the enzyme Adenylate Cyclase (AC) - AC converts ATP – cAMP (Increasing cAMP), cAMP then acts as a second messenger and Activates Protein Kinase A (PKA)
Phosphodiesterases (PDEs) - primary function is to degrade cAMP and cGMP – which regulates the cellular response→ cAMP Pathway Inactivation
Phospholipase C Pathway
Alpha Q activates an enzyme in the membrane named Phospholipase C (PLC) which converts membrane phospholipids into:
Inositol Triphosphate (IP3) and diacylglycerol (DAG) (2 Lipid-Derived second messengers)→ these are the second messengers.
DAG- Directly activates Protein Kinase C
IP3- Causes release of Ca from the Smooth Endoplasmic Reticulum
Ca2+ acts as a 3rd messenger
Catalytic Receptors
2 Subfamilies:
Receptor Enzymes
Integrin Receptors
Up-Regulation: The target cell inserts more receptors into its CM
Down-Regulation: A decrease in receptor number
Calcium
Ca enters the cell through channels that are either:
Voltage-Gated
Chemically-Gated
Mechanically-Gated
Ca2+ is released from storage sites inside the cell. Most Ca is stored in the Endoplasmic (Sarcoplasmic) Reticulum
Gases as Signaling Molecules
Nitric Oxide (NO), Carbon Monoxide, + Hydrogen Sulfide
In Tissues, NO is synthesized by Nitric Oxide Synthase, then NO diffuses into Tissue cells and binds to intracellular proteins converting GTP to cGMP; NO also acts in the brain as a neurotransmitter (NT) and neuromodulator
So NO can be a Second Messenger, a Paracrine Signal, a Hormone or a NT
She explicitly stated we needed to know this:
NO→ Guanyl Cyclase→ GTP→ cGMP→ Relaxation→ Vasodilation→ Blood Pressure decreases
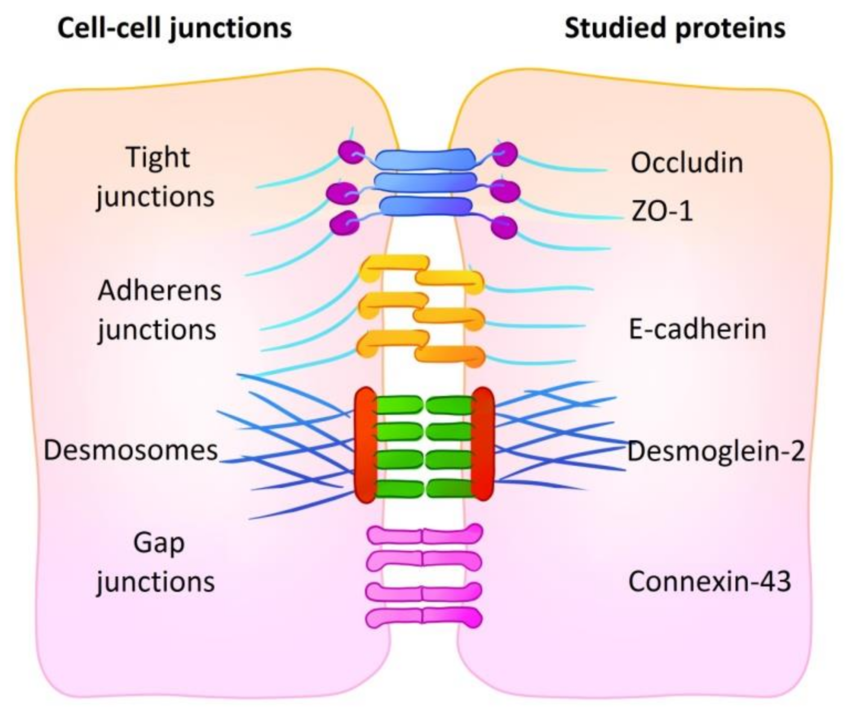
Gap Junction: Cells connected by connexins that make pores so the cytoplasm of one connects to the cytoplasm of another (Cytoplasmic bridge)
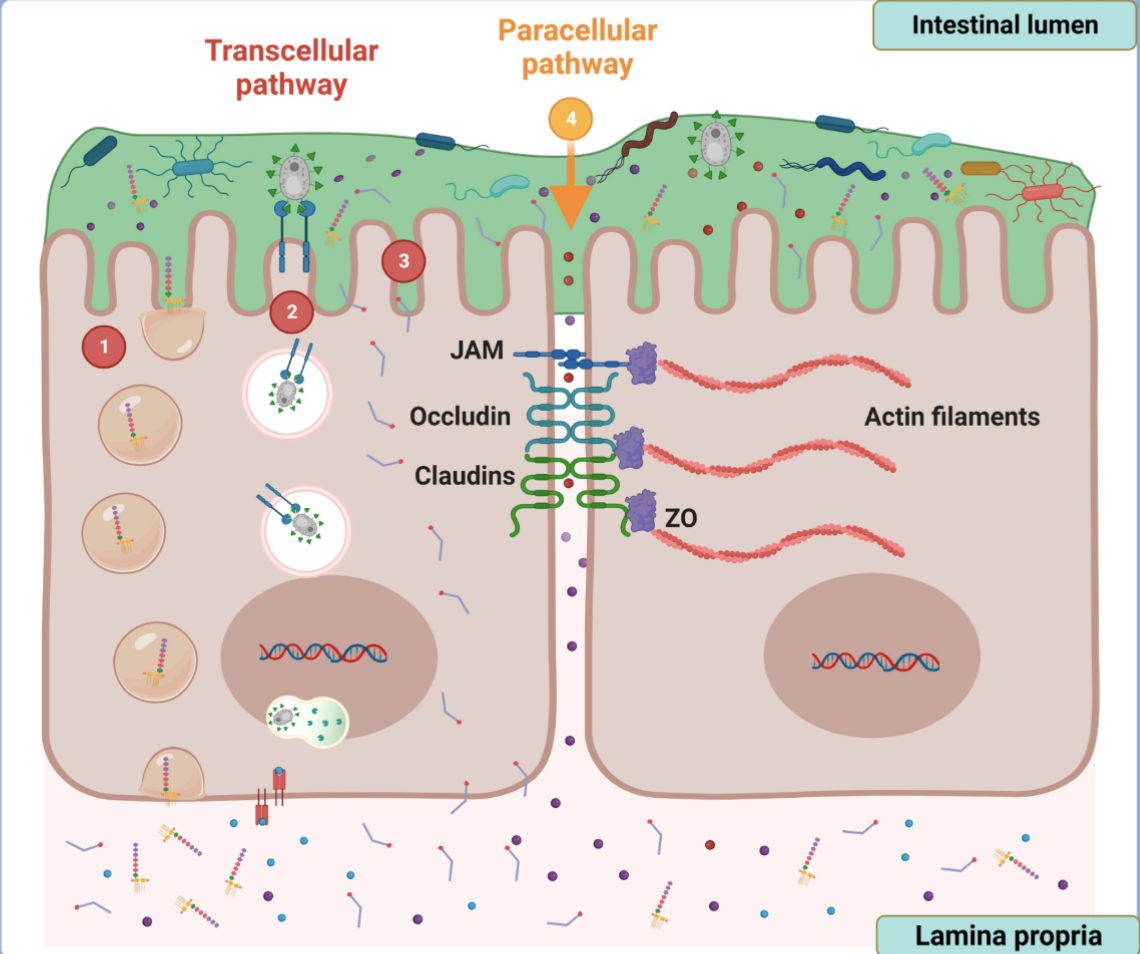
Occuluding Junctions (Tight Junction) - made up of claudins or occuldins; involve the cytoskeleton and the actin holding them together, blocks the movement of large molecules between the cells. Mainly ions and water getting through but nothing big. Can tend to be more selective depending on where they are located.
Anchoring Junction: 3 types:
Desmosome- cadherins, involved intermediate filaments actin
Adherin Junctions- proteins are also cadherins
Hemidesmosomes- basement membrane specifically, proteins are integrins
Lecture 5: Cell Membrane
Epithelial cells are polarized when they are organized into tissues, with different parts of the cell responsible for performing distinct functions.
Epithelial cells are divided into distinct apical and basolateral domains that differ in function and protein composition.
Epithelial Transport Mechanisms
Paracellular Transport- Movement of substances between adjacent epithelial cells, through the intercellular space.
Transcellular Transport- Movement of substances inside the cell, from the Apical membrane to the Basal membrane or vice versa.
Animal Cell Membrane (CM)
Cells are able to maintain Homeostasis in their interior because the CM is selectively permeable to small molecules
The CM is selectively permeable because of its Phospholipid Bilayer and its unique structure and polarity
Some molecules pass freely (diffuse) through the membrane-
Gases: Oxygen, Carbon Dioxide
Small Polar Uncharged Molecules: Water and Ethanol
Charged molecules of any size, and larger, uncharged polar molecules (glucose) are unable to cross the CM by passive diffusion. These require specific transport proteins
The Lipid Bilayer
The 3 Main types of Lipids that make up the Bilayer:
Phospholipids (most abundant)
Cholesterol
Glycolipids
These lipids are “self-sealing” because they are Amphipathic (They have a polar and non-polar end)
Cholesterol
Mammalian CM contain large amounts of Cholesterol
Position themselves with their OH (hydroxyl) group (weakly polar) forming a bond with the polar head groups.
Because of their Rigid Ring structure, Cholesterols will interact with and partially immobilize those regions of the hydrocarbon chains closest to them- it has distinct effects on Membrane Fluidity
Too much Cholesterol stiffens the CM and causes pathology → (hardens arteries- only thing holding us back from absolutely housing a pound of bacon.)
Glycolipids
Ubiquitous across all living organisms
A lipid molecule containing carbohydrate moieties
They are Cell Identity markers and are antigenic
They form part of the glycocalyx (sugar coat) - which gives cells their identity
Gycocalyx
A Carbohydrate coat that surrounds the Cell Membrane formed by the Oligosaccharides of glycolipids and transmembrane glycoproteins
Also composed of Glycosaminoglycans (GAGs)- and these bind to membrane-spanning proteins to anchor it to the cell membrane
The Function of the Glycocalyx
1) Provides a molecular signature to the cell
2) Helps cells adhere to one another
3) Provides protection from digestion by enzymes
The Glycocalyx can do the following-
1) Provides a molecular signature to the cell
2) Helps cells adhere to one another
3) Provides protection from digestion by enzyme
Membrane Proteins Classified by Structure
Integral Plasma Membrane Proteins- Found all the way through the Bilayer
Peripheral Membrane Proteins- found only on the outer surface
“All transmembrane proteins are integrated, but not all integrated proteins are transmembrane.” - Sun Tzu probably
Membrane Proteins by Function
Channels/Pores
Passive Channels (alway open)
Gated Channels- open or closed by specific stimuli
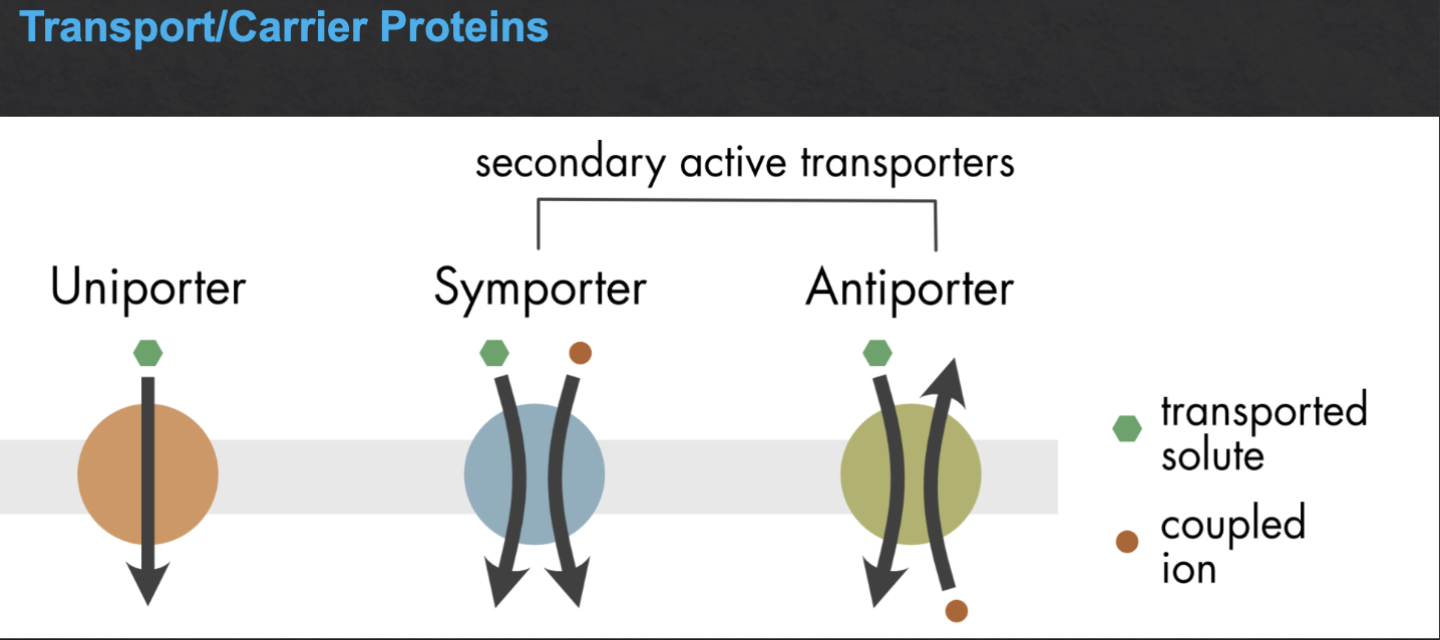
Transporter/Carrier Proteins
Receptors (can also be enzymes)
Enzymes- some carbonic Anhydrase
Cell Adhesion Molecules- cadherins, connexins, claudins, occludins
Cell Identity Markers- the glycoproteins, glycolipids of the glycocalyx
Molecular Movement Across the CM
Passive Transport- No energy (ATP splitting) required + Goes with the Concentration Gradient
Diffusion- solutes
Osmosis- water
Facilitated Diffusion
Bulk Flow- pressure
Active Transport- Energy (ATP splitting) required + Goes against the Concentration Gradient
Primary Active Transport
Na/K ATPase Pump→ 3 Na+ go out, 2 K+ come in (creates the negative membrane potential)
Secondary Active Transport
set up by primary active transport stored energy
Mechanism of the Na+ Glucose Secondary Active Transporter (SGLT)
Bulk/ Vesicular Transport
Endocytosis
Phagocytosis- actin mediated; engulfing macromolecule
Pinocytosis- capture small particles from the ECF through miniature vesicles
Receptor-Mediated Endocytosis- Clathrin-coated vesicles
Exocytosis
Membrane Potential
Membrane potential is defined as the voltage difference between the inner and outer surfaces of the cell membrane
Ions are not distributed evenly between the ECF and ICF.—> This system is in chemical disequilibrium, with concentration gradients for all four ions
The CM acts as an insulator to prevent free movement of ions between the ICF and ECF
K is always leaking out
Na is always leaking in (though to a lesser extent)
~K IONS ARE THE KEY PLAYERS IN MEMBRANE POTENTIAL~
Since there is always a little exchange, there is always a need to reestablish- So we have the Na/K ATPase Pump (which maintains the Resting Membrane Potential)
For each ATP split: 3 Na out and 2 K in
Lecture 4: Metabolism- unfinished (probably not gonna finish)
A network of highly coordinated chemical reactions in which the activities taking place in a cell at any given moment are matched to the needs of the cell.→ All of these reactions are mediated by enzymes
Enzymes: Proteins that speed up the rate of chemical reactions (act as catalysts)
Cellular Metabolism
Cells regulate their metabolism
Lecture 3: Tissues- In work
Capillary Fluid Exchange
Hydrostatic forces again
The Hydrostatic and Osmotic Pressures that produce fluid movement across the capillary wall
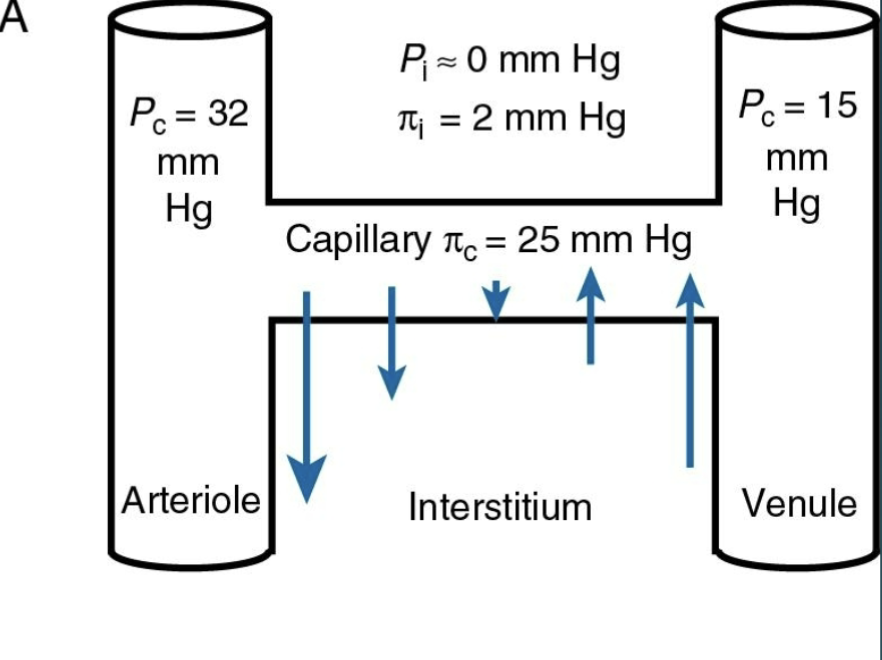
Net movement of water OUT is Filtration
Net movement of water IN is Absorption
Forces that influence the movement of fluid:
Pi = Oncotic Pressure (pulling)- stays the same
P = Hydrostatic Pressure (Pushing)- decreases as we move towards venule
The force of fluid against a wall- PUSHES fluid out into the Interstitium
Is opposed by interstitial fluid hydrostatic pressure
Colloid Osmostic Pressure
Pulling Pressure- The pressure exerted by large plasma proteins in the blood that pulls water into the capillaries→ crucial for maintaining blood volume and pressure.
Does not vary from arterial to venous side
Interstitial fluid has very little osmotic pressure
4 Major Types of Tissues
Nervous
Found in excitable cells (cells that can change their membrane potential)
Epithelial
Groups of cells that cover the exterior surfaces of the body line internal cavities and passages and form certain glands
Muscle
3 different types: Smooth, skeletal, cardiac
Excitable cells
Contract to provide movement
Connective
Binds the cells and organs together
Bones, Cartilage, blood -
Specialized Connective Tissues
Supporting CT
Cartilage
Bone
Fluid CT
Distinct collections of cells in a fluid matrix
Does not connect structures or provide mechanical support (because… y’know… fucking fluid :| )
Blood- classified as CT because of its embryonic origins (Mesenchyme); Plasma considered the ECM
Lymph
Adipose (fat)
found in the subcutaneous tissues, breast, bone marrow
Connective Tissue- Extracellular Matrix
ECM is very important Connective Tissue Structure
The ECM is the extracellular material that is synthesized and secreted by the cells of a tissue→ matrix components are primarily secreted by Fibroblasts
Composition of the ECM and the mechanical properties depend on the tissue type
ECM always has two basic components:
Proteoglycans
Insoluble Protein Fibers (Collagen, Fibronectin, Laminin→ the textural nightmares when you’re eating chicken :’( )
Epithelial Tissue
Definition: Groups of cells that cover the exterior surfaces of the body, line internal cavities and passages, and form certain glands.
Function: Protect the internal environment of the body and regulate the exchange of materials between the internal and external environments
8 Types of Epithelial Tissues:
Simple Squamous - Alveoli
Simple Cuboidal - Kidney
Simple Columnar - Stomach
Transitional - Bladder
Stratified Squamous - Esophagus
Stratified Cuboidal - Sweat gland
Stratified Columnar - Salivary Duct
Pseudostratified Columnar - Trachea
Squamous | Cuboidal | Columnar |
Simple + Stratified | Simple + Stratified | Simple + Stratified + Pseudostratified |
Appearance:
| Appearance:
| Appearance:
|
Function and Location:
| Function and Location:
| Function and Location:
|
Epithelial Cells’ Main Features
Polarity
Intercellular Junction
Basement Membrane (ECM)
Supported by Connective Tissue
Five Functional Groups of Epithelium
Polarity:
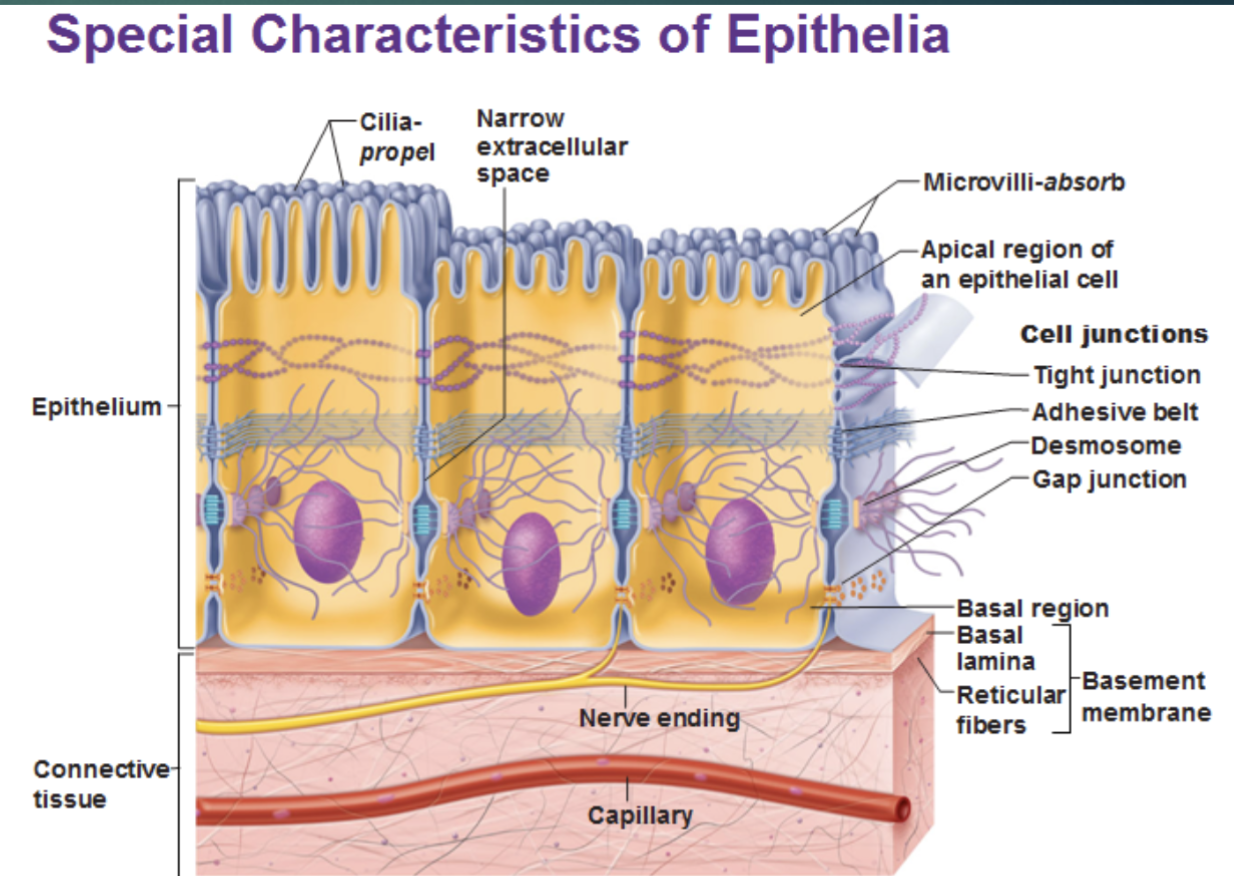
Intercellular Junctions:
Gap Junction: Cells connected by connexins that make pores so the cytoplasm of one connects to the cytoplasm of another (Cytoplasmic bridge)
Occuluding Junctions (Tight Junction) - made up of claudins or occuldins; involve the cytoskeleton and the actin holding them together, blocks the movement of large molecules between the cells. Mainly ions and water getting through but nothing big. Can tend to be more selective depending on where they are located.
Anchoring Junction: 3 types:
Desmosome- cadherins, involved intermediate filaments actin
Adherin Junctions- proteins are also cadherins
Hemidesmosomes- basement membrane specifically, proteins are integrins