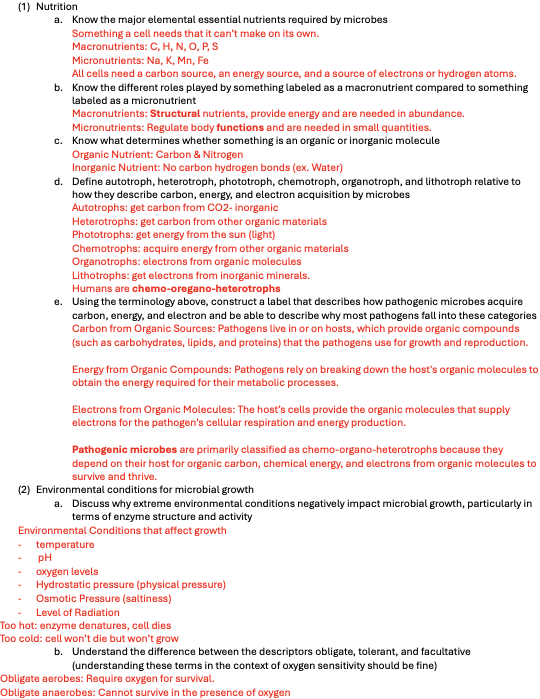
(1) Nutrition
a. Know the major elemental essential nutrients required by microbes
Something a cell needs that it can’t make on its own.
Macronutrients: C, H, N, O, P, S
Micronutrients: Na, K, Mn, Fe
All cells need a carbon source, an energy source, and a source of electrons or hydrogen atoms.
b. Know the different roles played by something labeled as a macronutrient compared to something labeled as a micronutrient
Macronutrients: Structural nutrients, provide energy and are needed in abundance.
Micronutrients: Regulate body functions and are needed in small quantities.
c. Know what determines whether something is an organic or inorganic molecule
Organic Nutrient: Carbon & Nitrogen
Inorganic Nutrient: No carbon hydrogen bonds (ex. Water)
d. Define autotroph, heterotroph, phototroph, chemotroph, organotroph, and lithotroph relative to how they describe carbon, energy, and electron acquisition by microbes
Autotrophs: get carbon from CO2- inorganic
Heterotrophs: get carbon from other organic materials
Phototrophs: get energy from the sun (light)
Chemotrophs: acquire energy from other organic materials
Organotrophs: electrons from organic molecules
Lithotrophs: get electrons from inorganic minerals.
Humans are chemo-oregano-heterotrophs
e. Using the terminology above, construct a label that describes how pathogenic microbes acquire carbon, energy, and electron and be able to describe why most pathogens fall into these categories
Carbon from Organic Sources: Pathogens live in or on hosts, which provide organic compounds (such as carbohydrates, lipids, and proteins) that the pathogens use for growth and reproduction.
Energy from Organic Compounds: Pathogens rely on breaking down the host's organic molecules to obtain the energy required for their metabolic processes.
Electrons from Organic Molecules: The host’s cells provide the organic molecules that supply electrons for the pathogen’s cellular respiration and energy production.
Pathogenic microbes are primarily classified as chemo-organo-heterotrophs because they depend on their host for organic carbon, chemical energy, and electrons from organic molecules to survive and thrive.
(2) Environmental conditions for microbial growth
a. Discuss why extreme environmental conditions negatively impact microbial growth, particularly in terms of enzyme structure and activity
Environmental Conditions that affect growth
- temperature
- pH
- oxygen levels
- Hydrostatic pressure (physical pressure)
- Osmotic Pressure (saltiness)
- Level of Radiation
Too hot: enzyme denatures, cell dies
Too cold: cell won’t die but won’t grow
b. Understand the difference between the descriptors obligate, tolerant, and facultative (understanding these terms in the context of oxygen sensitivity should be fine)
Obligate aerobes: Require oxygen for survival.
Obligate anaerobes: Cannot survive in the presence of oxygen
Tolerant: Can survive less-than-ideal conditions but don’t prefer them (e.g., aerotolerant anaerobe survives in oxygen but doesn’t use it).
Facultative anaerobes: Can grow with or without oxygen, using oxygen when it is available but switching to anaerobic metabolism in its absence.
c. Define neutrophiles, acidophiles, alkaliphiles, barophiles, and halophiles
Neutrophiles- like neutral pHs between 6-8, usally 7
Acidophiles- prefer acidic pHs, like 1-4
Alkaphiles- like pH of 9 or greater
Barophiles- organisms that can survive in high levels of pressure
Halophiles- microorganism that prefers or can tolerate high levels of salt
d. Recall that microbes in the environment are often found in biofilms, which make them more resistant to certain environmental and physical assaults
Biofilms: multicellular community of one type or multiple types of microbes covered by exopolysaccharide (external layer of sugar).
e. Temperature
i. Be able to describe the effects of temperature on microbial growth and enzyme activity as the temperature changes from the minimum, optimal, and maximum temperatures
Minimum Temperature: Growth is slow, enzyme activity is minimal.
Optimal Temperature: Fastest growth, enzymes work at peak efficiency.
Maximum Temperature: Enzyme activity decreases, denaturation occurs, leading to cell death.
ii. Define extreme thermophiles, thermophiles, mesophiles, psychrotrophs, and psychrophiles
Extreme Thermophiles: Thrive at extremely high temperatures (65–121°C).
Thermophiles: Prefer high temperatures (40–70°C).
Mesophiles: Grow best at moderate temperatures (20–45°C), human body range.
Psychrotrophs: Grow in cold but can survive at moderate temps (0–30°C).
Psychrophiles: Prefer cold environments (below 15°C).
iii. Explain why microbes that mesophiles are or psychrotrophs are of the most concern in medical microbiology
Mesophiles: Grow at body temperature (37°C), making them common human pathogens.
Psychrotrophs: Can grow at refrigerator temperatures, causing food spoilage and infections.
iv. Understand the differences between autoclaving, boiling, pasteurization, and ultrahigh temperature sterilization, particularly in the control of microbial growth
Autoclaving: High pressure and steam (121°C), kills all microbes and spores.
Boiling: Kills most pathogens but not endospores; not sterilization.
Pasteurization: Reduces microbial load without sterilizing (e.g., 72°C for 15 sec) destroys pathogens but not microbes.
Ultrahigh Temperature Sterilization (UHT): 135°C for a few seconds, sterilizes taste is changed.
v. Discuss how the existence of extreme thermophiles and endospores relate to the observation that boiling water is not sterilization
Extreme Thermophiles and endospores can survive boiling because they resist high heat, requiring more intense methods like autoclaving.
vi. Compare the relative effectiveness of moist heat and dry heat and know examples of each
Moist Heat: More effective (e.g., autoclaving, boiling) destroys membranes and denatures proteins, penetrates more deeply than dry heat, more efficient.
Dry Heat: Less effective, requires longer exposure and higher temperatures (e.g., oven sterilization at 160-170°C) : oxidizes molecules (disrupts bonds in proteins).
f. Understand why oxygen is important for energy generation and dangerous because of the production of oxygen radical species that can damage biological molecules
i. Define capnophile
Needa high levels of CO2
ii. Define obligate anaerobe, aerotolerant anaerobe, facultative anaerobe, microaerophile, and obligate aerobe
Obligate Anaerobe: Cannot survive in the presence of oxygen; relies on anaerobic processes.
Aerotolerant Anaerobe: Does not use oxygen but can tolerate its presence; grows equally well with or without oxygen.
Facultative Anaerobe: Prefers oxygen but can grow without it by switching to fermentation or anaerobic respiration.
Microaerophile: Requires low levels of oxygen (2-10%) for growth; higher concentrations are toxic.
Obligate Aerobe: Requires oxygen for survival and growth; cannot grow without it.
iii. Discuss where each of the above might be found in a thioglycolate broth or in a lab experiment using plates;
Obligate Anaerobe: Bottom of the tube (no oxygen).
Aerotolerant Anaerobe: Uniformly distributed (grows in the presence of oxygen).
Facultative Anaerobe: Grows throughout but more concentrated at the top (utilizes oxygen when present).
Microaerophile: Grows just below the surface (needs low oxygen).
Obligate Aerobe: Grows at the top (requires oxygen)
iv. Understand what each of the oxygen categories tells us about how these organisms use oxygen for energy or their capability for detoxifying oxygen radicals (do they have no, some, or all detoxifying enzymes)
Obligate Anaerobe: No detoxifying enzymes (cannot handle oxygen).
Aerotolerant Anaerobe: Some detoxifying enzymes (can tolerate oxygen).
Facultative Anaerobe: All detoxifying enzymes (can detoxify and utilize oxygen).
Microaerophile: Some detoxifying enzymes (requires low oxygen).
Obligate Aerobe: All detoxifying enzymes (depends on oxygen).
(3) Microbial (bacterial growth)
a. Discuss what is meant by binary fission, the general events that occur during the process of binary fission, and how this replication strategy results in exponential growth
Taking one cell and dividing it into two, microbial growth is the increase in number of microbes, not size. Exponential growth.
Events: ring forms in the middle of the cell, tightening and pinching inwards, resulting in 2 cells, creates 2 daughter cell that are virtually identical to mother cell
b. Microbial (bacterial) growth curve
i. Name and label the four phases of bacterial culture growth in lab, and describe what the cells are doing during each phase
Lag phase: microbes are doing the most processes, period of time between getting nutrients vs. actually being able to utilize them. Can manipulate conditions to change growth of lag phase,
Log Phase: number of new cells is greater than number of during cells, endospores usually start growing late in this phase
Stationary Phase: number of new cells is equal to number of dying cells
Death/decline Phase: number of new cells is less than number of dying cells
c. Properly display bacterial growth on a graph (with correctly labeled axes)
d. Correlate changes in nutrient concentrations in natural environments with the four phases of a microbial growth curve
Lag Phase: Nutrient concentrations are stable.
Log Phase: Nutrients are consumed rapidly.
Stationary Phase: Nutrients deplete, waste accumulates.
Death Phase: Nutrients are exhausted.
e. Define generation (doubling) time and discuss how it changes over the four phases of growth; be able to determine a final cell number, if given a starting number, the doubling time, and a length of time of incubation; understand that a given doubling time is usually assumed to be during exponential growth unless explicitly told otherwise
Definition: The time it takes for a population to double in number.
Phases: Shortest during the log phase.
f. Know how to enumerate bacterial cells for the Y-axis of the bacterial growth curve; discuss why sampling must be used, and what it means to use a direct or indirect method of counting; understand the difference between methods that determine viable numbers of cells and total number of cells and what the implications of choosing one method over the other on determining the shape of the growth curve
Y-axis Enumeration: Measured in CFU/mL or cells/mL.
Sampling: Necessary because it’s impractical to count all cells.
Direct Methods: Count all cells (e.g., hemocytometer).
Indirect Methods: Measure turbidity or metabolic activity.
Viable vs. Total Counts: Viable counts determine living cells (can underrepresent the actual population), while total counts include dead and alive, affecting growth curve interpretation.
Module 6 (Microbial control)
(1) Physical and chemical control of microbes
a. Understand how temperature can be used to control microbial growth (as (2e) above).
b. Know the terminology around physical and chemical control: sterilization, disinfection, antisepsis, and sanitization/degermation.
Sterilization: complete removal of viable microorganisms and endospores
Disinfection: removal of all biological entities except endospores, used on inanimate objects
Antisepsis: removal of vegetative pathogens, used on animate living things
c. Describe the relative susceptibility of microbes (you do NOT need to know the exact placement of each group of organisms, but you should know that endospores are the most generally resistant to physical and chemical control and enveloped viruses are the least)
d. Know the suffixes -cidal, and -static in reference to whether a control agent kills the microbes or just inhibits new growth of the microbes
Cidal- will kill
Static- inhibit growth (stops growth or freezes and slows it down)
e. Discuss the factors that should be considered when choosing a physical or chemical method of control
i. Understand how to choose the level of control that would be needed to control microbial growth on an instrument relative to how that instrument will be used on a patient (will the instrument be used in a critical, semi-critical, or non-critical manner)
Critical instruments: Direct contact with sterile body areas (e.g., surgical tools) require sterilization.
Semi-critical instruments: Contact mucous membranes; need high-level disinfection (e.g., endoscopes).
Non-critical instruments: Contact intact skin; require low-level disinfection (e.g., blood pressure cuffs).
ii. Understand how environmental or use conditions (temperature, pH, concentration, length of exposure) can affect the potency of a chemical control method
Temperature: Higher temperatures increase effectiveness.
pH: Affects the activity of the control agent.
Concentration: Higher concentrations often increase potency.
Exposure time: Longer exposure enhances effectiveness.
iii. Be able to identify factors that should be considered when selecting an ideal chemical control method
Effectiveness against target microbes.
Safety for human use.
Stability and shelf-life.
Cost-effectiveness.
Residual effects or toxicity.
f. Explain what is meant by the death rate of a microorganism under a given condition and describe the implications for how a microbial population decreases when exposed to that condition
The death rate is the constant percentage of microbes killed per time unit under certain conditions.
Microbial populations decrease (a constant fraction dies in each time interval).
i. Relate the death rate and determining when something that is being treated is considered sterile
Sterility occurs when no viable microbes remain. The death rate helps calculate how long a treatment must last to achieve sterility. The death rate indicates how long to apply a treatment to reduce the population to zero, ensuring sterility.
g. Describe what microbial targets are affected by chemical and physical control methods
Cell membrane: Disruption leads to loss of integrity.
Proteins/Enzymes: Denaturation halts microbial functions.
DNA/RNA: Damage prevents replication and function.
Cell wall: Weakening causes lysis (especially in bacteria).
(2) Antimicrobial control of microbes
a. Explain how the selection of physical and chemical control methods for preventing infections differs from the choice of antimicrobials for chemotherapy of infections
Control methods: Prevent infections via sterilization or disinfection (e.g., heat, chemicals).
Antimicrobials: Treat infections inside the body by killing/inhibiting pathogens (e.g., antibiotics).
b. Define the term ‘antibiotic’ and contrast natural, semi-synthetic, and synthetic antibiotics
Antibiotic: Substance that kills/inhibits microbes.
Natural: Produced by microbes (e.g., penicillin).
Semi-synthetic: Chemically modified natural antibiotics.
Synthetic: Fully lab-made (e.g., sulfa drugs).
c. Define the term selective toxicity and how it applies to antimicrobial chemotherapy
Ability of a drug to target microbes without harming the host, crucial for effective chemotherapy.
d. Describe what is meant by spectrum of activity
Range of pathogens a drug affects (e.g., bacteria, fungi).
e. Compare and contrast broad and narrow spectrum antimicrobial agents and when you might choose to treat an infection with one vs the other
Broad-spectrum: Effective against many pathogens, used when pathogen is unknown.
Narrow-spectrum: Targets specific pathogens, used when pathogen is identified.
f. Discuss the three different groups of resistant bacteria (inherently resistant, those that develop resistance through spontaneous mutations, and those that acquire resistance from other resistant microbes via transformation, transduction, or conjugation)
Inherent: Naturally resistant (e.g., no target structure).
Spontaneous mutations: Random mutations create resistance.
Acquired: Resistance from other bacteria via transformation, transduction, or conjugation.
g. Explain how antibiotic-resistant microbes resist antibiotics (by degrading the antibiotic, changing transport structures, etc.)
Bacteria resist by degrading antibiotics, modifying targets, or altering drug transport.
h. Identify the major targets of antibiotics in bacteria
Cell wall, protein synthesis, nucleic acids, metabolic pathways, cell membrane.
i. Discuss how antimicrobial resistance arises within a bacterial population and consider the major contributors to the rise of resistance and potential ways to slow that rise
Resistance arises through overuse, misuse, and incomplete treatments. Reducing unnecessary use and proper dosage can slow resistance.
j. Discuss the effect of antibiotics on members of the human microbiome and the principles underlying those affects (i.e., the role of broad-spectrum antibiotics in both killing members of the human microbiome and increasing the chance for antibiotic resistance)
Broad-spectrum antibiotics disrupt the microbiome, killing beneficial microbes and promoting resistance.
k. Explain why using multiple antibiotics can delay or inhibit resistance
Combines different mechanisms, reducing the likelihood of bacteria developing resistance.
Module 7 (intro to the immune system and immunizations)
(1) General immune system information
a. Describe the role of the immune system, particularly in protection against microbial pathogens
Protects against microbial pathogens by identifying and eliminating harmful invaders.
b. Explain how the 3 lines of defense of the immune system participate in the protection against pathogens (physical barriers, innate cellular immunity, adaptive immunity)
Physical barriers: Skin, mucous membranes, and normal microbiota block pathogen entry.
Innate immunity: From birth, fast, non-specific response; includes phagocytic cells and inflammation.
Adaptive immunity: Slow, specific response; includes B cells, T cells, and memory.
c. List the three physical barriers and discuss why skin is a better physical barrier than the mucous membranes
Skin (epidermis): the best barrier, semi permeable, viruses can’t penetrate dead skin
Mucous Membranes: mucous, stomach acid, saliva
Normal Microbiota: they are there so that potentially more pathogen microbes can’t be
d. Explain how the normal microbiota of a human acts as a physical barrier (microbial antagonism)
Microbial antagonism: Competes with harmful microbes, reducing pathogen colonization.
e. Understand the importance of the immune system being able to distinguish self from non-self
Essential to prevent attacking the body’s own cells while eliminating pathogens.
f. Understand innate cellular immunity
i. Discuss the defining characteristics of the innate immune system (why it is good)
Good: available from birth, fast-acting, offers resistance to any microorganism encountered by the host, will recognize wide variety of organisms
Bad: does not change in intensity, lacks to ability to selectively respond to a specific pathogen, lack immunological memory
ii. Discuss the major deficiencies of the innate immune system (why it is bad)
Innate Defense not good: does not change in intensity, lacks effectiveness in response to specific pathogens, will cause damage to you as well, cannot differentiate between pathogens. No immunological memory.
iii. Discuss what the point of innate cellular immunity is.
First line of defense, available from birth, initiates quick response (minutes to hours).
g. Understand adaptive immunity
i. Discuss the defining characteristics of the adaptive immune system (why it is good)
Has memory, specificity, diversity- can recognize 100 billion things.
ii. Discuss the major deficiencies of the adaptive immune system (why it is bad)
Not present at birth, takes time to develop in response to infection with a specific pathogen (5 days-2 weeks or longer) When it goes bad it goes very bad (Lupus, MS, etc.)
iii. Define the term antigen and understand how foreign antigens drive the adaptive immune response
Antigen: molecules that trigger an immune response
iv. Know the major roles of B cells, helper T cells, and cytotoxic T cells
B cells: Produce antibodies.
Helper T cells: Activate other immune cells.
Cytotoxic T cells: Kill infected cells.
v. Understand the importance of antibodies in targeting and eliminating foreign antigens
Antibodies bind specifically to antigens on pathogens, neutralizing them or marking them for destruction by other immune cells.
vi. Explain what it means to say the adaptive immune response has ‘memory’
The adaptive immune system remembers previously encountered pathogens, leading to a faster, more effective response upon re-exposure.
vii. Discuss how the immune response is able to specifically recognize and remember foreign antigens and how that contributes to the success of immunizations (understand the memory graph in your presentation and drawn on the board)
The immune system creates memory cells after exposure to a pathogen or vaccine, allowing it to recognize and respond more rapidly to future infections. This principle underlies immunization, where vaccines introduce antigens to train the immune system.
(2) Immunizations
a. Understand the difference between passive and active immunization
Active immunization: receive vaccine, protects against a future providing antigen infection, when you get sick, immune system recognizes and prevents against future infections
b. Discuss what passive immunization is and when it might be used
Passive immunization: Immediate but temporary protection, used in emergencies or when immediate immunity is needed (e.g., after exposure to a toxin or virus).
i. Give an example of natural passive immunization and artificial passive immunization
Passive immunization: Immediate but temporary protection, used in emergencies or when immediate immunity is needed (e.g., after exposure to a toxin or virus).
c. Discuss what active immunization is and when it might be used
Active immunization: Stimulates the immune system to produce memory cells, providing long-term protection.
i. Give an example of natural active immunization and artificial active immunization
d. Describe the following types of vaccines
i. Whole agent vaccines
1. Differentiate between attenuated live vaccines and whole agent inactivated vaccines
Whole agent attenuated: less likely to cause disease but still active
Inactive: agent is killed or inactivated before being given
2.
3. Discuss the benefits and concerns about attenuated live vaccines
Benefits: activate T cells and b cells, most long lasting
Concerns: can have virulence restored (becomes stronger) and begin growing and multiplying inside persion, has weakened virulence in regard to a healthy person but an immunocompromised individual may not be able to survive it, pregnant people
4.
ii. Subunit vaccines
1. Differentiate between toxoid vaccines (only a modified toxin is used to elicit an immune response) and protein subunit vaccines (only one or a few proteins from a pathogen are used to elicit an immune response)
Toxoid vaccines: Use modified toxins to elicit an immune response.
Protein subunit vaccines: Use specific proteins from the pathogen.
2. Describe viral vectors vaccines and how/why they blend both whole agent and subunit vaccines (part of a pathogen cloned into the backbone of a non-pathogenic virus)
Viral vector vaccines use a non-pathogenic virus to deliver pathogen antigens. They combine:
Whole Agent Features: Mimic natural infections, inducing strong immune responses.
Subunit Features: Present only specific antigens, minimizing disease risk while still providing immunity.
3. Know that nucleic acid vaccines (DNA and mRNA) can be used to elicit an immune response
Nucleic acid vaccines (DNA and mRNA) introduce genetic material from pathogens into host cells, prompting them to produce antigens that stimulate an immune response. They are fast to develop and elicit strong immunity.
e. Discuss the potential side effects or mild adverse outcomes associated with some vaccine use in an outbred population
In outbred populations, side effects can vary due to genetic diversity.
Common mild adverse effects include:
Localized reactions: Swelling or pain at the injection site.
Systemic reactions: Fever, fatigue, or muscle aches.
Allergic reactions: Rare, but possible.
f. Discuss why we might not vaccinate a population even if an effective vaccine exists (if the risk of even mild adverse outcomes outweighs the risk of acquiring the infection, then it might not be cost-effective or reasonable to vaccinate everyone)
Risk vs. Benefit: Mild or severe side effects outweigh disease risks.
Cost-effectiveness: Economic burden may not justify widespread vaccination.
Alternative Measures: Other public health strategies could be more appropriate.
g. Explain the concept of herd immunity and how this concept relates to the idea that the choice to vaccinate may not be an individual decision in all cases, but might instead be a matter of public policy
Herd immunity occurs when a significant portion of a population is immune, reducing disease spread to immunocompromised individuals who cannot be vaccinated.