Chapter 7 - Quality Assessment and Management in the Urinalysis Laboratory
- The term quality assessment (QA) refers to the overall process of guaranteeing quality patient care and is regulated throughout the total testing system.
- Included in a QA program are procedure manuals, internal quality control and external quality control, standardization, proficiency testing (PT), record keeping, equipment maintenance, safety programs, training, education and competency assessment of personnel, and a scheduled and documented review process.
Urinalysis Procedure Manual
- When new procedures are adopted, they must be reviewed and signed by the heads, notified to the laboratory personnel, and the review process documented and reviewed by designated authority.
Pre-Analytical Factors
This includes documentation from collection to receipt in the laboratory, patient information and preparation, instructions for general procedures, and policies for specimen rejection.
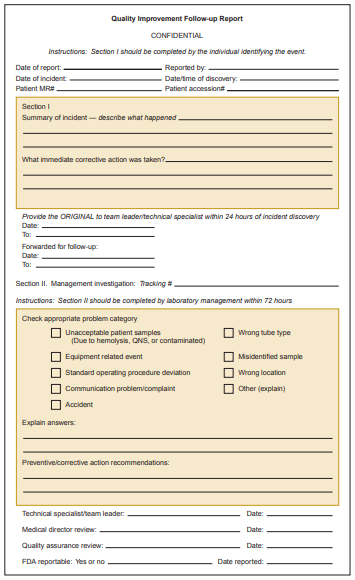
Any problems and corrective actions leading to problems in such should be documented in an internal laboratory quality improvement form.
Analytical Factors
- This includes methodological information for reagents, calibration and operating procedures for instruments and equipment, testing procedures and materials needed, personnel education and information accessibility, quality control procedures, and general safety precautions for all aspects.
- Positive and negative quality control values are inputted into a recording sheet.
- The standard deviations of every control measurement are plotted on Levy-Jennings control charts to visually monitor control values, and it should be within ±2 SD or ±3 SD of the mean.
- All corrective actions are followed according to protocol, documented and then reviewed by designated authority.
Post-Analytical Factors
- This includes the standardization and formatting of reports, and the methods of reporting and correction.
Regulatory Issues
- Clinical Laboratory Improvement Amendments ‘88 (CLIA’ 88) stipulate that all laboratories that perform testing on human specimens for the purposes of diagnosis, treatment, monitoring, or screening must be licensed and obtain a certificate from the CLIA program that corresponds to the complexity of tests performed.
- Tests are assigned to the following categories: waived, provider-performed microscopy, moderate complexity, and high complexity.
- Non-waived testing replaces the terms “moderate” and “high complexity” testing when referring to requirements that pertain to both levels of testing.
- Waived tests are considered easy to perform and interpret, require no special training or educational background, require only a minimum of standardization and QC, and are not considered critical to immediate patient care.
- Provider-performed microscopy (PPM) includes certain microscopic procedures that can be performed in conjunction with any waived test to avoid disruption in the patient visit but authorize only physicians, physician’s assistants, nurse practitioners, and dentists to perform the tests.
- Moderate-complexity tests are more difficult to perform than are waived tests and require documentation of training in testing principles, instrument calibration, periodic proficiency testing and on-site inspections.
- High-complexity tests require sophisticated instrumentation and an increased level of interpretation by the testing personnel.
- CLIA regulations specify required components for QA that include patient test management assessment, QC assessment, proficiency testing assessment and personnel assessment.
- CLIA are jointly administered by the Centers for Medicare and Medicaid Services (CMS), FDA and CDC, and accrediting agencies that have been approved by the federal government after demonstrating equivalency with CLIA standards include COLA (which is popular with physician office laboratories), the JCAHO, CAP (which serves large laboratories), AOA, AABB, and ASHI.
Quality Management
- It is based on Continuous Quality Improvement (CQI), Improving Organizational Performance (IOP), Total Quality Management (TQM) and Six Sigma.
- TQM is a systematic problem-solving approach using visual tools to identify the steps in the process for meeting customer satisfaction of quality care in a timely manner at reduced costs.
- CQI aims to improve patient outcomes by providing continual quality care in a constantly changing health-care environment, and it is visualized using flowcharts, cause-and-effect diagrams (fishbone diagrams), pareto charts, histograms, run charts, control charts, and scatter diagrams.
- The most widely used plan for quality improvement in health care is the Plan-Do-Check-Act (PDCA) strategy also known as the Plan-Do-Study-Act (PDSA) cycle.
- The “Plan” step is the process of making a change by identifying the customers and customer expectations, describing the current process, measuring and analyzing, focusing on improvement opportunities, identifying the root cause, and generating a solution.
- The “Do” step is the process of testing the improvement by mapping out a trial run, implementing that run, collecting data, and analyzing the data.
- The “Check” or “Study” step involves evaluating the results and drawing conclusions as to the effect of the change.
- The “Check” or “Study” step involves evaluating the results and drawing conclusions as to the effect of the change.
- IOP includes work and management processes for the various departments of an organization to work together.
- The five essential elements for performance improvement, known as PDMAI, provides standards PI.1 through PI.5 (plan, design, measure, assess, and improve) to outline a specific cycle for improving performance.
- Plan (PI.1): The hospital has a planned, systematic, hospital-wide approach to process design and performance measurement, assessment, and improvement.
- Design (PI.2): New processes are designed well.
- Measure (PI.3): The organization has a systematic process in place to collect data.
- Assess (PI.4): The hospital uses a systematic process to assess collected data.
- Improve (PI.5): The hospital systematically improves its performance.
- Six Sigma Quality Management emphasizes a more quantitative methodology utilizing power function graphs, critical-error graphs, and OPSpecs charts.
Medical Errors
- The JCAHO has issued a new standard referred to as “Sentinel Event Policies and Procedures” requiring reporting of sentinel events, or any unanticipated death or major permanent loss of function not related to the natural course of the patient’s illness or underlying condition.
- Sentinel events must be reported to the JCAHO within 45 days of the event and must include a root cause analysis and an action plan.