Motor Control Notes
Motor Control
Introduction
Motor control is the study of how the nervous system controls movement. Movements can range from simple reflexes to complex actions. The primary purpose of the brain is to guide movement.
Movement Terms
Reflexes: Simple, brief muscle activations (e.g., eyeblink, hiccup, finger twitch).
Acts/Action Patterns: Complex, sequential movements (e.g., honking a car horn, writing your name, playing guitar).
Motor Plan/Motor Program: A set of muscle commands established before an action occurs.
Control Mechanisms
Two control mechanisms optimize accuracy and speed:
Open-Loop Control
Maximizes speed by using pre-programmed instructions without external feedback. Ballistic movements are rapid and completed regardless of sensory feedback. No guiding external feedback.
Closed-Loop Control
Maximizes accuracy by using feedback from the controlled action to guide movements. Ramp movements are smooth, slower, and sustained, and are guided by feedback.
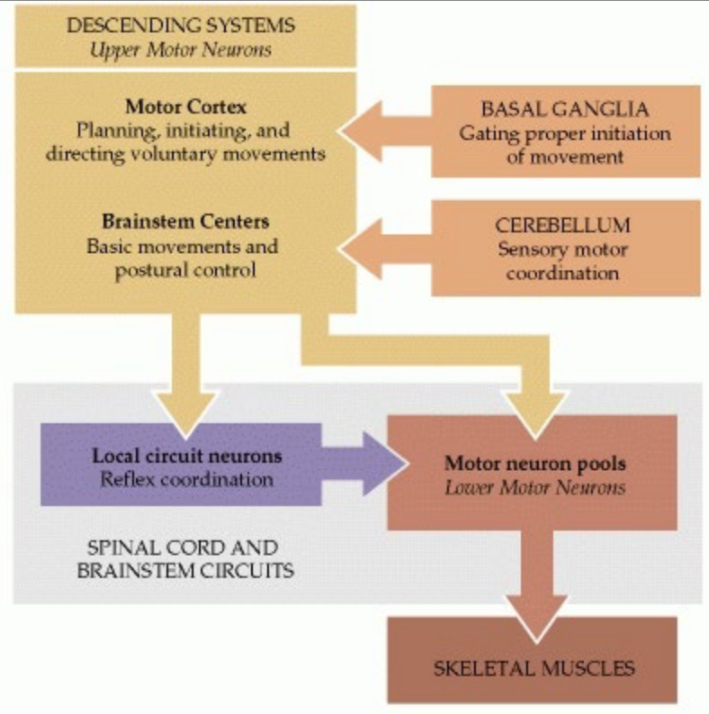
Hierarchy of Motor Control
Nonprimary Motor Cortex: Initiates cortical processing.
Primary Motor Cortex: Initiates commands for action.
Brainstem: Integrates motor commands.
Cerebellum and Basal Ganglia: Tweak these systems.
Spinal Cord: Controls skeletal muscles.
Skeletal Muscles: Power movement.
Muscle Mechanics
Antagonists: Biceps and triceps are antagonists.
Balance:At rest, flexor and extensor muscles are balanced.
Tremor: Alternation of flexor-extensor (antagonist)/bicep-tricep contraction. Normally present, but debilitating if poorly regulated.
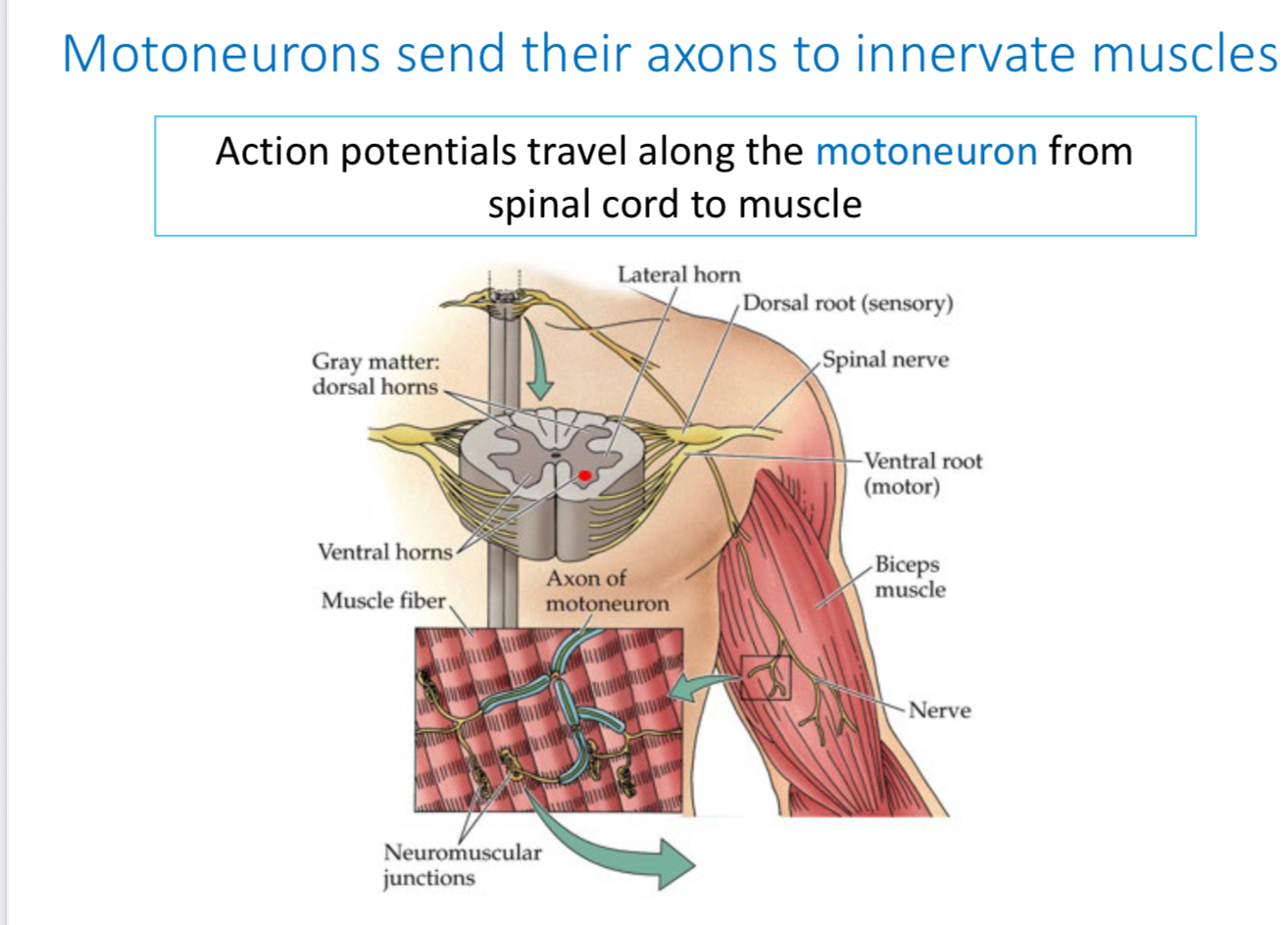
Motoneurons
Motoneurons send their axons to innervate muscles. Action potentials travel along the motoneuron from the spinal cord to the muscle.
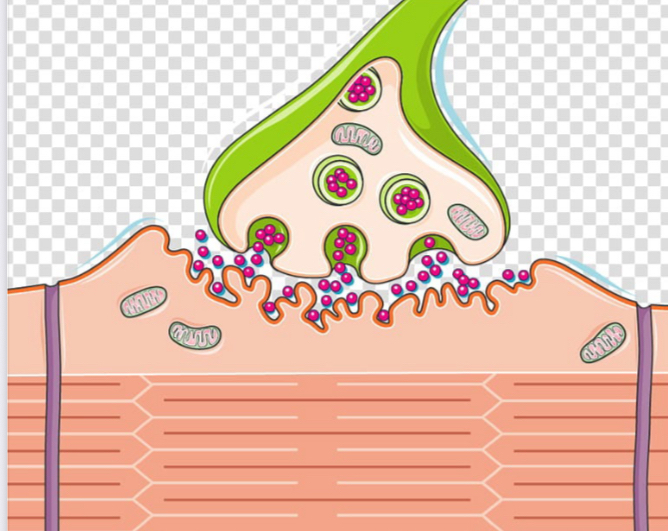
Neuromuscular Junction
Neuromuscular Junction: Point where a motor neuron terminal and muscle fiber meet.
Acetylcholine: Neurotransmitter released at the neuromuscular junction.
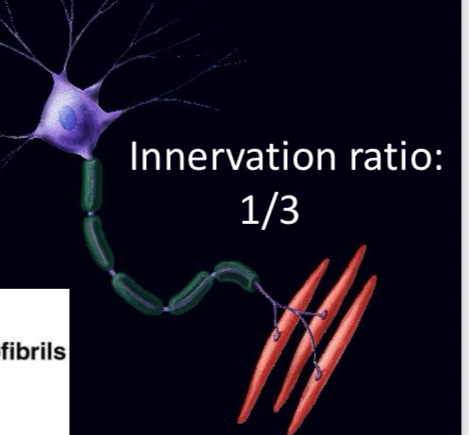
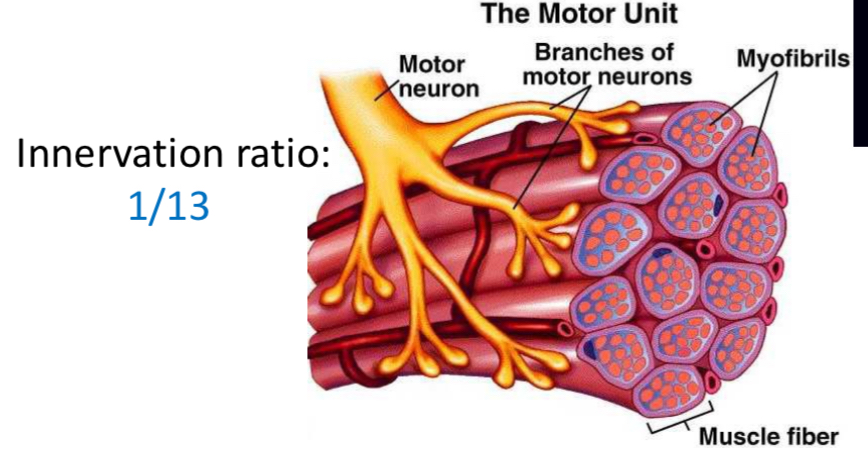
Motor Units
Motor Unit: One motor neuron's axon and all its target fibers.
Fine Movements: Muscles that make fine, precise movements have only a few muscle fibers per axon.
Innervation Ratio: Examples include 1/3 and 1/13, which describe the ratio of motor neurons to muscle fibers.
1 axon and 3 fibers attached will produce fine movements
1 axon and 13 movements will NOT
Sensory Feedback
Action of muscles is guided by sensory feedback:
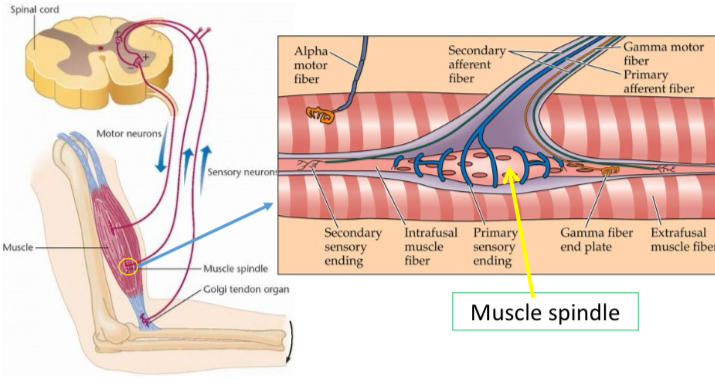
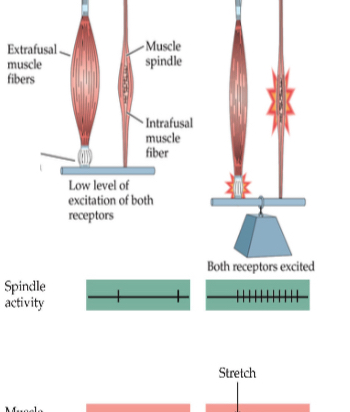
Muscle Spindles: Responsive to muscle stretch.
Golgi Tendon Organs: Respond to muscle contraction, less to stretch.
Proprioception: Information about body movements and position.
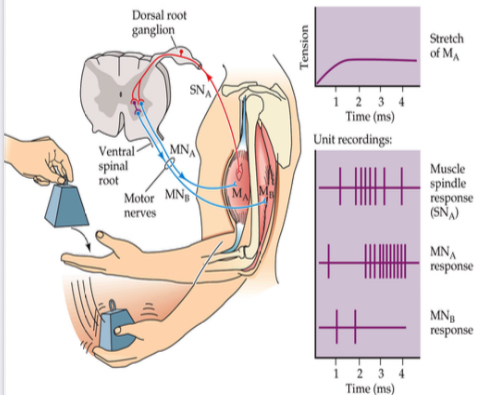
Muscle Spindles
Muscle spindles provide feedback on muscle length and stretch.
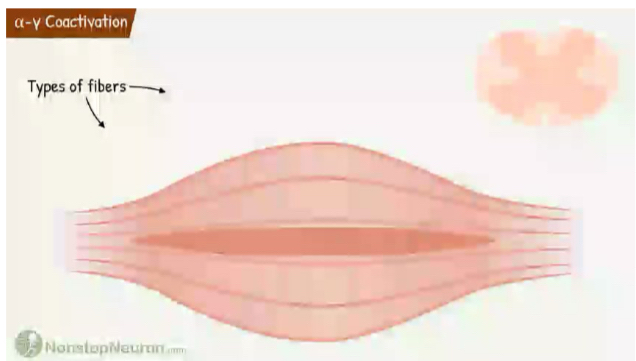
α-γ Coactivation
alpha-gamma Coactivation mechanism involving sensory neuron, \alpha motor neuron, and \gamma motor neuron.
Muscle Spindle Stretch Reflex
Muscle is stretched.
Excitation of muscle spindle afferents. muscle spindles stretching and excite.
Excitation of \alpha -motoneurons. Beta and alpha neurons are excited.
Agonist muscle (biceps and triceps) stimulated to oppose stretch.
Antagonist muscle is inhibited. Muscle goes to relaxed state neither stretching or contractions.
This reflex prevents you from falling over when you extend your arm.
Spasticity
Impaired control of the stretch reflex. Motor cortex normally inhibits reflex behavior. When cortical input is cut off, spinal cord is released from inhibition, exaggerating reflexes. Hyperreflexia, Clonus.

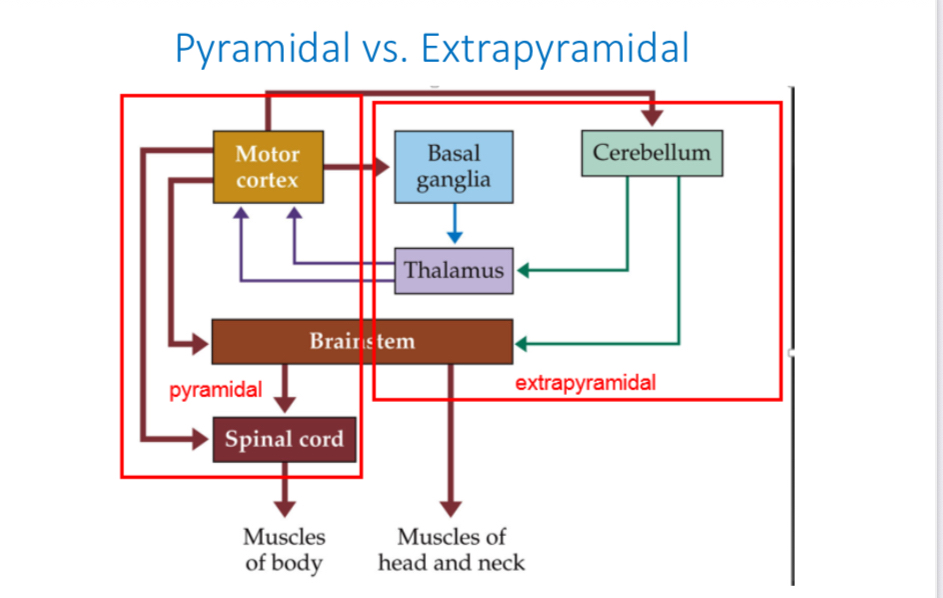
Pyramidal vs. Extrapyramidal Motor Systems
Pyramidal System: Includes the primary motor cortex, and is responsible for voluntary movement.
Extrapyramidal System: Includes the basal ganglia and cerebellum, modulates and tweaks movements.
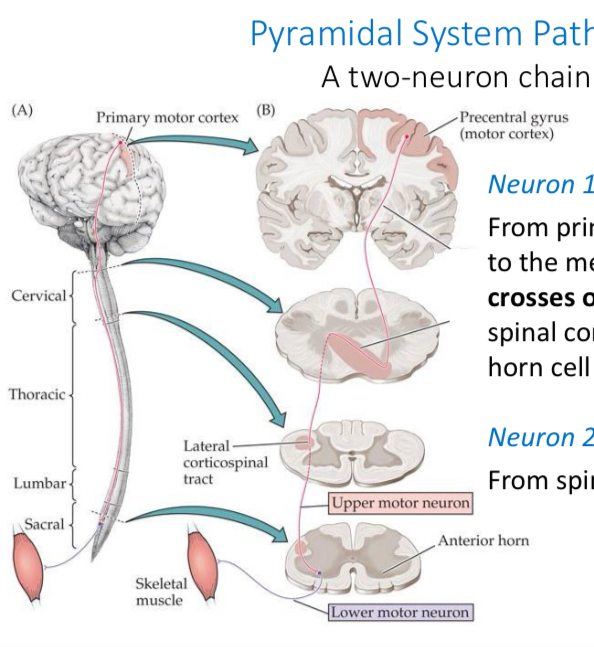
Pyramidal System Pathway
Upper Motor Neuron: From primary motor cortex to the medulla, where it crosses over (decussation), then down the spinal cord to the anterior horn cell (lower motoneuron).
Lower Motor Neuron: From spinal cord to muscle.
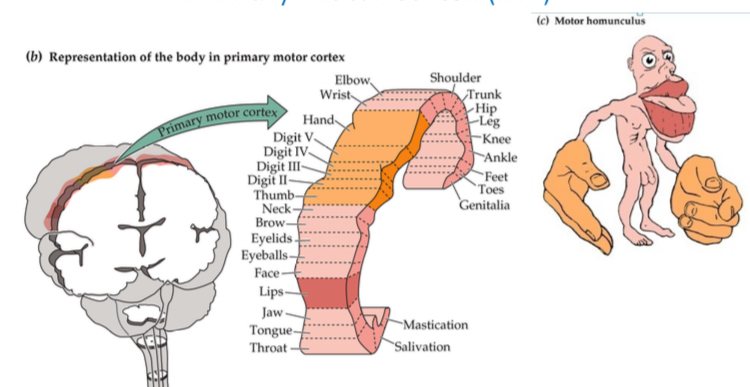
Primary Motor Cortex (M1)
Primary motor cortex changes as a result of learning. Early music training results in expansion of motor cortex.
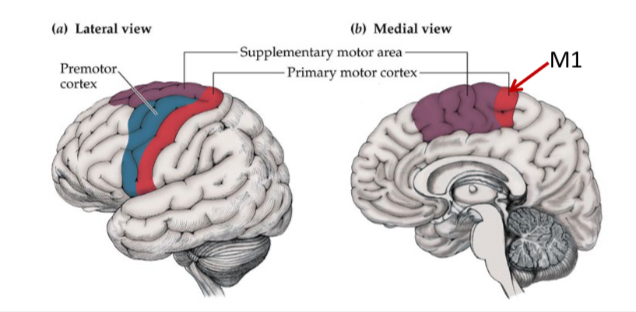
Nonprimary Motor Cortex
Learns and plans movement:
Supplementary Motor Area (SMA): Encodes sequences of movements during skill acquisition.
Premotor Cortex: Neurons fire just before performing an activity.
Extrapyramidal System - Basal Ganglia/Cerebellum
Basal Ganglia
Includes the caudate nucleus, putamen, globus pallidus, subthalamic nucleus, and substantia nigra.
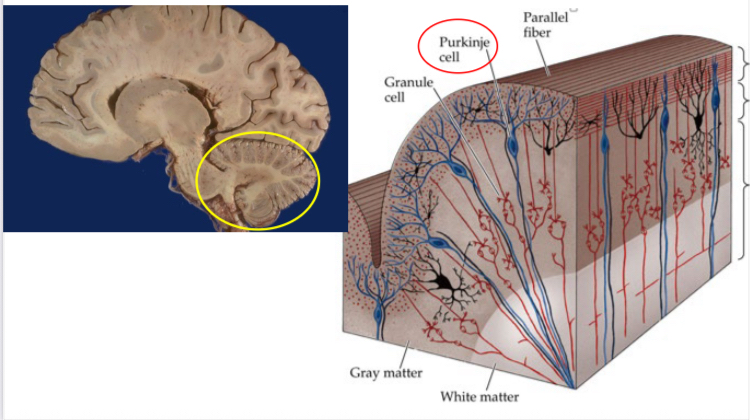
Cerebellum
Guides movement through inhibition via Purkinje cells, which send inhibitory messages.
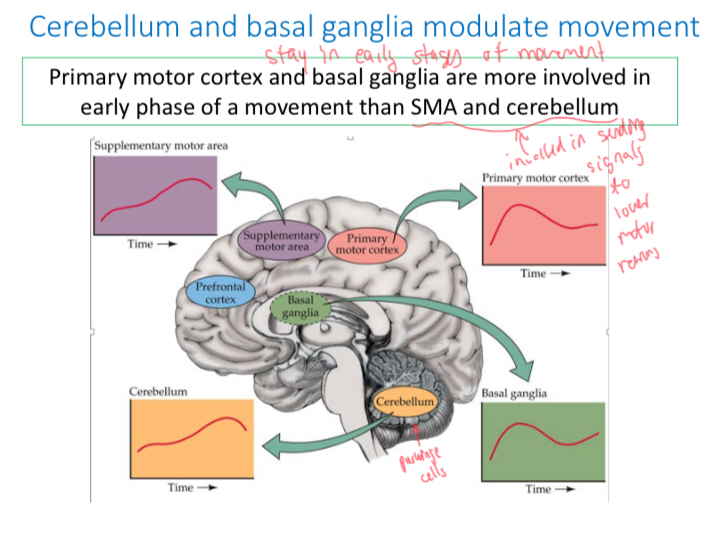
Cerebellum and Basal Ganglia
Primary motor cortex and basal ganglia are more involved in early phase of a movement than SMA and cerebellum.
Postural Adjustment
Basal ganglia and cerebellum (extrapyramidal system) predict postural consequences of planned (pyramidal) movement and act to prevent loss of balance.
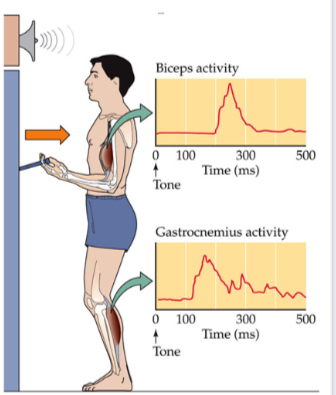
Gastronemius is activated before he lifts bell? Why? Because of extrapyrimidal movements.
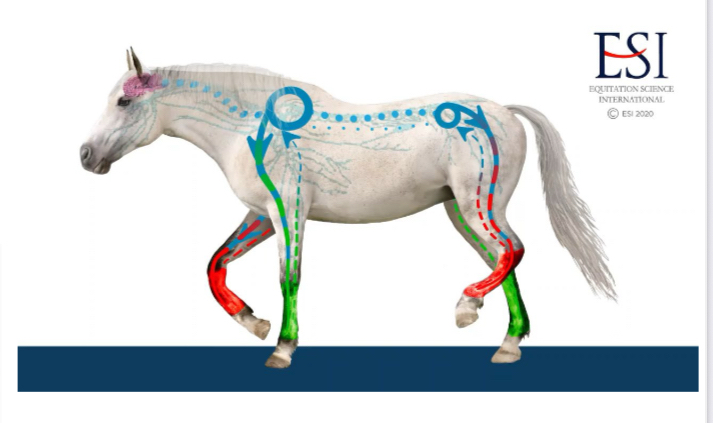
Central Pattern Generators
Neural circuits generate rhythmic behaviors (e.g., walking) in the spinal cord.
Input to Output
A visual task that requires a simple choice and a button push involves a complex cascade of processes.
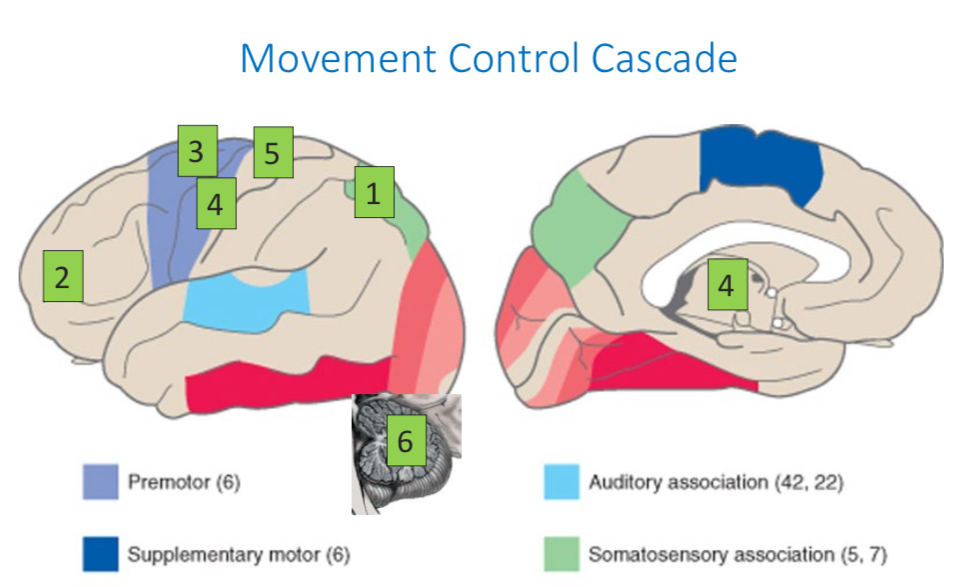
Movement Control Cascade
What is the current state of the body?
Should I move?
Select the motor plan.
Load the motor plan.
Execute the plan.
Feedback on how the plan is going. Change it?
Clinical Neurology of Movement
Strength vs. Tone
Strength: Largely a pyramidal function (power).
Tone: Largely an extrapyramidal function (posture).
These are not independent.

Pyramidal vs. Extrapyramidal Damage
Pyramidal damage causes weakness.
Extrapyramidal damage impairs movement control.
What Goes Wrong with the Motor System?
Myopathy
Primary disorder of muscle.
Muscular Dystrophy
Dystrophin is a protein needed for normal muscle function, produced by the X chromosome. Patients make no dystrophin or an abnormal dystrophin molecule, leading to progressive degeneration of muscle.
Myasthenia Gravis
Autoimmune disorder where patients develop antibodies to their own ACh receptors. This causes weakness of skeletal muscles that develops over the day and resolves with rest/sleep.
Polio
Poliovirus destroys spinal motoneurons and sometimes cranial motoneurons. There is no treatment for polio.
Amyotrophic Lateral Sclerosis (ALS)
Lou Gehrig disease, degeneration of motoneurons and consequent loss of their target muscles. Fasciculations.
Spina Bifida and Spinal Cord Injuries
Spinal cord injuries result in paralysis; reflexes, sensation, and strength below the level of the injury are lost.
Apraxia
Higher-level (motor processing) disorder: inability to sequence movements, though no muscle paralysis exists. New acts are ramped (feedback-controlled) - slow, variable - frontal and parietal cortex. Well-learned acts are ballistic - fast, consistent - cortex and basal ganglia.
Parkinson Disease
Tremor
Bradykinesia
Shuffling gait
Postural instability
Degeneration of dopamine cells in the substantia nigra, which project to the basal ganglia. L-dopa, a precursor to dopamine, improves symptoms. Environmental exposures, especially pesticides, contribute.
Huntington Chorea
Progressive destruction of the caudate nucleus and putamen. Cerebral cortex also is impaired. The gene responsible (HTT) has a trinucleotide repeat (CAG). If CAG repeats too many times, the disease develops.
Ataxia
Cerebellar damage impairs motor control. Purkinje cells die. Causes include childhood tumors of the cerebellar vermis, alcoholism, and inherited degeneration of the cerebellum.
Dystonia
Abnormal sustained posture due to basal ganglia dysfunction.
Tourette Syndrome
Tics and Obsessive-Compulsive Disorder. Basal ganglia and cortex disorder. Clinical features: more common in boys, tics usually end by adulthood, tics affect face and shoulders more than hands and legs, coprolalia is rare in children.
Hemiparetic Gait
Motor cortex damage, such as stroke, causes motor impairment. Weakness (paresis) of voluntary movements.