Pharmacology Test #2
Nervous System, Mental Health, and Drug Therapy: Depression, Mood Disorders, and Drug Treatments
Depression: feelings of pessimism worry, intense sadness, loss of concentration, slowing of mental processes, problems eating and sleeping
Mania: mental and physical hyperactivity, disorganized behaviour, elevated mood; mood of extreme excitement, excessive elation, hyperactivity, agitation, increased psychomotor activity
Bipolar disorder: alternating episodes of depression and mania; mood swings that alternate between periods of major depression and periods of mild to severe chronic agitation
Post Traumatic Stress Disorder: Triggered by a traumatic event that leaves a person with intense, disturbing thoughts and feelings long after the event; Persistent anxiety or recurrent fear after a terrifying event
Seasonal Affective Disorder: depression which occurs in the fall and winter and remits in the spring and summer
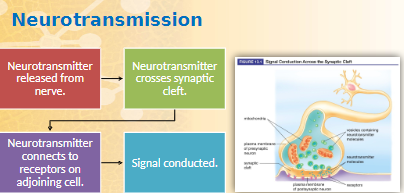
Neurotransmitters
produced by a nerve cell and transmit information
i.e. serotonin, norepinephrine, dopamine
psychiatric and mood disorders
deficiency of neurotransmitters
dysfunction of neurotransmitters
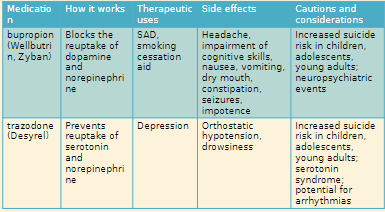
Antidepressants
goal of therapy is to change neurotransmitter levels
take 10-21 days to start working
medication Guide required
Overview of Disorders
hard to diagnose
often occur together in same patient
Need multiple medications for treatment
Good communication essential among patient family or caregivers. prescriber, pharmacist
Antidepressants
delay of onset of 10-21 days
not used on “as needed” basis
Depression
underlying causes: exogenous vs. endogenous sources
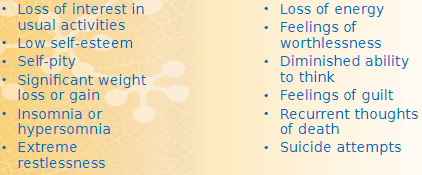
signs: crying, loss of interest in life or social activities, increased focus on death, significant weight loss or gain
symptoms: low self-esteem, pessimism, sleep disturbances, loss of energy and ability to think, feelings of worthlessness and guilt, poor memory, thoughts of suicide
neurotransmitters involved in mood: norepinephrine, serotonin, dopamine
Drug Regimens and Treatments for Depression
Patient response to drug therapy
response not immediate
may take 3-6 weeks for full response
drug therapy trial of at least 3-4 weeks
Risk for suicide
teens and young adults
highest risk is when starting drug therapy
monitor for worsening signs of depression, suicidal thoughts, unusual behaviors
Stopping Therapy
risk of acute withdrawal symptoms if stopped abruptly
worsened depression symptoms if dose not tapered
Clinical depression is the most severe psychiatric disorder
Women more likely than men to have depression
Depression occurs later in life in men
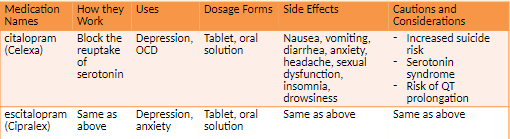
Selective Serotonin Reuptake Inhibitors (SSRI): block reuptake of serotonin, little effect on norepinephrine
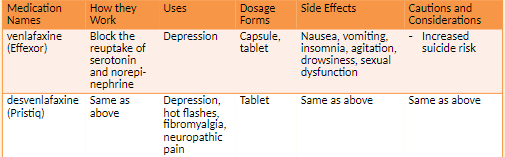
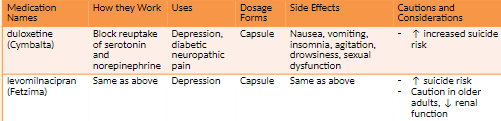
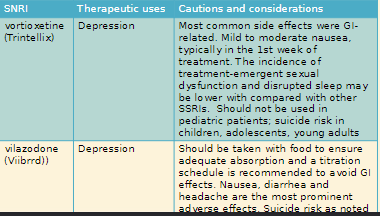
Serotonin Norepinephrine Reuptake Inhibitors (SNRI): increase both serotonin and norepinephrine
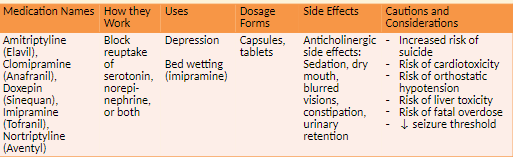
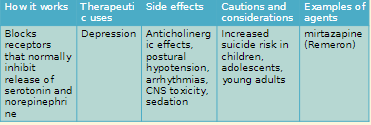
Tricyclic Antidepressants (TCA): prevent reuptake of serotonin and/or norepinephrine
Monoamine Oxidase Inhibitors (MAOIs): inhibit enzymes that break down serotonin and norepinephrine
Depression
Serotonin syndrome
Cause: presence of too much serotonin
Signs: racing heart, fever, high blood pressure, headache
Risk factors: taking more than one antidepressant, taking St. John’s wort
Prognosis: potentially fatal
Selective Serotonin Reuptake Inhibitors: block the reuptake of serotonin
classified effects: Nausea, vomiting, dry mouth, drowsiness, insomnia, headache, diarrhea, sexual dysfunction, serotonin syndrome
Patients with antidepressants worked immediately, but it is important to realize that it may take four weeks for these medications to achieve full effect. Antidepressants should help with sleep problems within a week or so, but other psychiatric effects may take longer to achieve full efficacy.
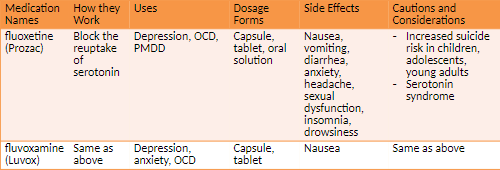
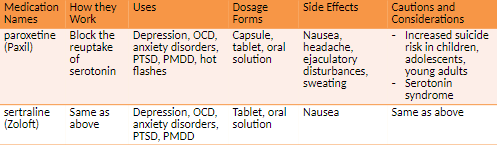
Additional uses for SSRIS Obsessive-compulsive disorder (OCD) A form of anxiety Obsessive thoughts impair function.
Repetitive behaviors relieve fears and anxiety. Premenstrual dysphoric disorder (PMDD) Emotional and behavioral changes during second half of a woman's menstrual cycle Similar symptoms to PMS but more severe Posttraumatic stress disorder (PTSD), fibromyalgia, anxiety, panic disorder, nerve pain (duloxetine)
Often confused
Celexa
Celebrex (arthritis)
Look-a-like
Prozac
Proscar (prostrated enlargement)
Do not drink alcohol
Do not stop abruptly
Serotonin and norepinephrine Reuptake inhibitors work by blocking the reuptake of serotonin and norepinephrine
Side effects: nausea, vomiting, insomnia, agitation, drowsiness
Chapter 8 day 2
Depression and Mood Disorders
2 Weeks washout period before starting new class of antidepressants
Severe hypertensive reactions with food containing high levels of tyramine
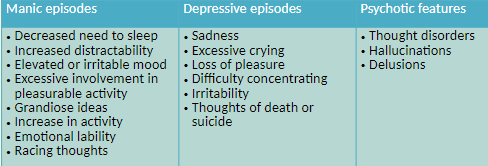
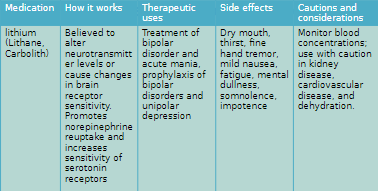
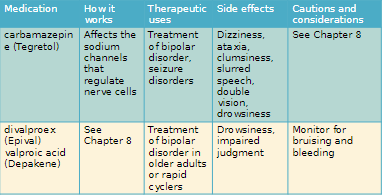
Bipolar Disorder
Periods of depression alternating with periods of mania, a state of overly high energy, excitement, hyperactivity, optimism, and increased psychomotor activity
Increased psychomotor activity can involve irritability, excessive involvement in work or other activities, grandiose ideas, racing thoughts, decreased need for sleep
Goals of Therapy
Treat acute episodes and prevent subsequent attacks
Mania: mood of extreme excitement, excessive elation, hyperactivity, agitation, and increased psychomotor activity
Bipolar Disorder: mood swings that alternate between major depression and mania
Unipolar Depression: major depression with no previous occurrence of mania
Post-traumatic stress disorder: Disorder characterized by persistent agitation or persistent,
recurrent fear after the end of a traumatic event and lasting for over a month or impairing work or relationshipSeasonal Affective Disorder: Form of depression that recurs in the fall and winter and remits in the spring and summer
The two-fold objective of drug therapy is to treat acute episodes and prevent subsequent attacks
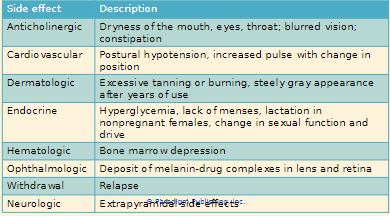
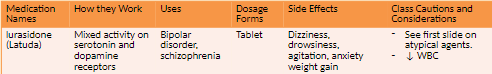
Schizophrenia, Psychosis and drug Treatments
Schizophrenia: A chronic mental health disorder characterized by delusions, disorganized speech and behavior, decrease in emotional range, neurocognitive deficit
Cause excessive dopamine levels in the limbic system
Positive symptoms include hallucinations and delusions
Negative symptoms are withdrawal, ambivalence, behaviour changes, memory loss and confusion
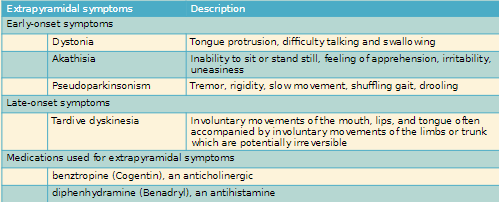
Treatment
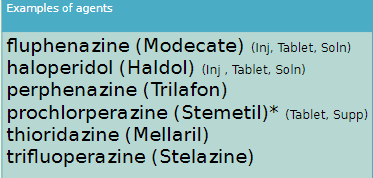
Typical antipsychotic
Block dopamine receptors in all four dopamine pathways
Lead to unfavorable side effects extrapyramidal symptoms (EPS)
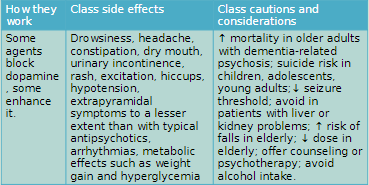
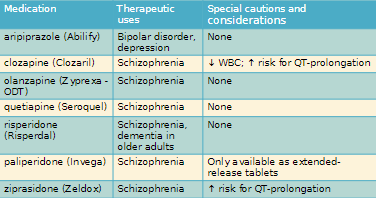
Atypical antipsychotics
Block dopamine receptors in the limbic system pathway instead of all four pathways
Improved efficacy and fewer side effects
Goals of Therapy: reduce symptoms such as thought disorder, hallucination, delusions
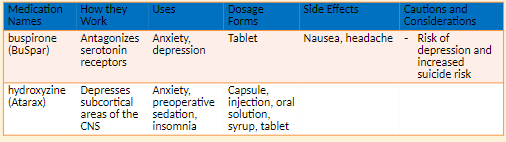
Anxiety and Drug Treatments
Anxiety: a state of uneasiness characterized by apprehension and worry about possible events
Symptoms
tension, apprehension, easy startling, uneasiness and nervous at your work or with people, nagging uncertainty about the future
can lead to chronic fatigue, headaches, insomnia
Exogenous anxiety: Develops in response to external stresses
Endogenous anxiety: Not related to any identifiable external factors
Occurs as a result of a cellular function abnormality in the CNS
Antianxiety agents:
SSRIs and SNRIs
citalopram (Celexa)
duloxetine (Cymbalta)
escitalopram (Cipralex)
paroxetine (Paxil)
sertraline (Zoloft)
venlafaxine (Effexor)
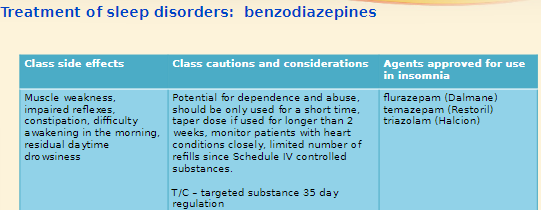
Benzodiazepines
Other antianxiety agents
Treatment Principles
monitor closely for depression
Taper to avoid withdrawal symptoms
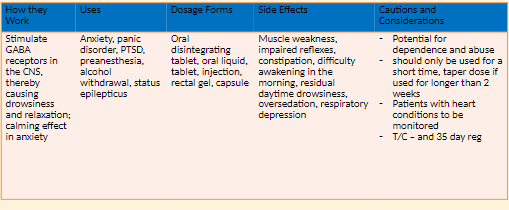

Panic Disorder
Panic Disorder: A form of intense, overwhelming, and uncontrollable anxiety
Intense fear or apprehension, may involve anticipation of a serious illness or life-threatening attack
Symptoms: Dyspnea, palpitations, chest pain, choking sensation, dizziness, feelings of unreality, tingling in hands or feet, hot or cold flashes, sweating, numbness, trembling
Cause: Heightened sensitivity to signals entering the brain; Amplification of incoming messages to a part of the brain stem resulting in excessive arousal, excessive autonomic discharges, and increased respiratory drive
Treatment
Psychotherapy
Short-Term anxiety agents
SSRIs
Benzodiazepines buspirone
Other agents
beta-adrenergic agents
diphenhydramine
hydroxyzine
TCAs
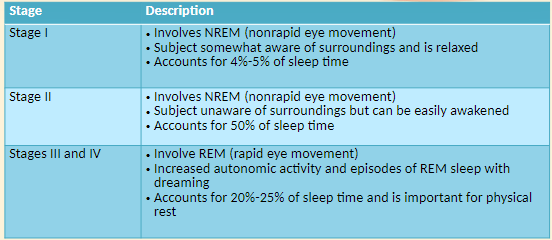
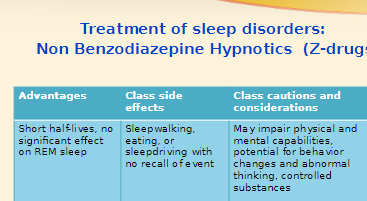
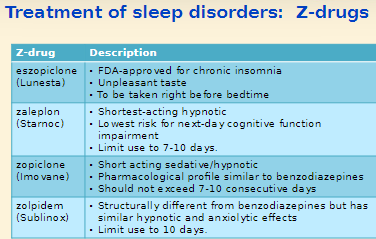
8.5 Sleep Disorders and Drug Treatments
Insomnia
Difficulty falling asleep or staying asleep
May be chronic condition, a short term problem or transient
Transient not considered a sleep disorder but a response to an acute stressful event that is expected to improve with time
Causes
Situational: job stress, hospitalization, travel
Medical: pain, respiratory problems, GI problems
Psychiatric: schizophrenia, depression, mania
Drug induced: alcohol, caffeine, sympathomimetic agents
Non Drug Therapy
Normalizing the sleep schedule
Increasing physical activity during the day
Discontinuing the use of alcohol as a sedative
Sleeping a total of only seven or eight hours in a 24-hr period
Reducing caffeine and nicotine intake
Eliminating any drug that could lead to insomnia
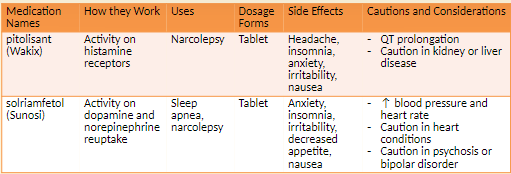
Stimulants of Narcolepsy
A sleep disorder involving recurrent inappropriate episodes of sleep during daytime hours
Characteristics symptoms
Sleepy feeling during daytime with quick progression to REM sleep
Cataplexy or short periods of muscle tone loss
Sleep paralysis when falling asleep or waking up
Vivid hallucinations at onset of sleep
Nondrug therapy
constant sleep schedule
Avoiding of shift work
Avoidance of Alcohol

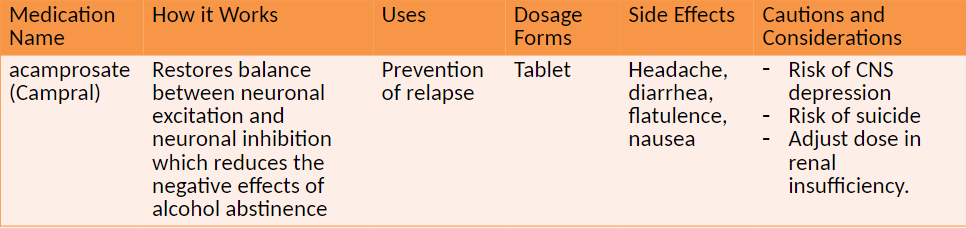
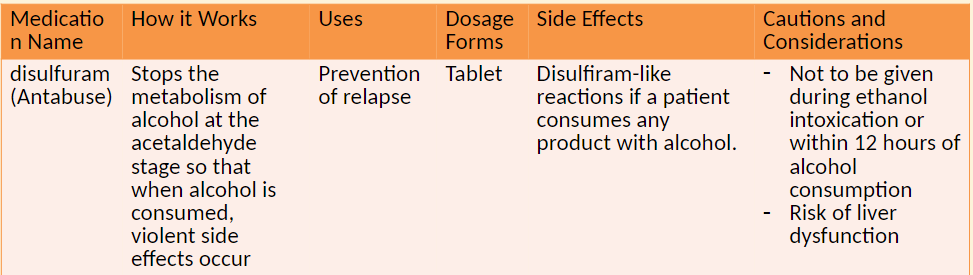
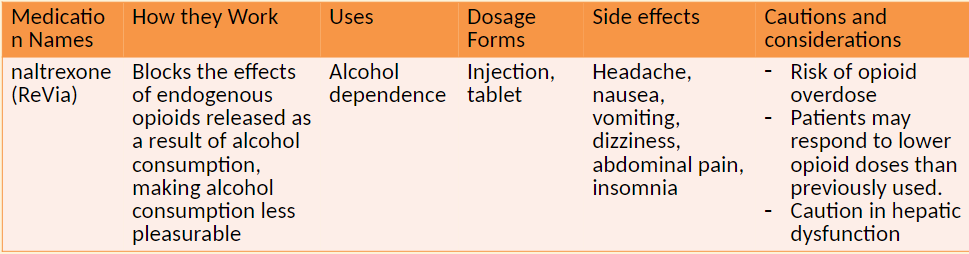
Alcohol Dependence and Drug treatment
Alcohol dependence (alcoholism): Pattern of alcohol use that involves problems controlling drinking, preoccupation with alcohol, use of alcohol even when it causes problems, drinking more to get the same effect, or having withdrawal symptoms upon rapidly decreasing or stopping drinking
Ethanol (alcohol)
The intoxicating agent in liquor, is an anesthetic
Deaths from alcohol due to cirrhosis or aspiration of vomitus
Impacts on health
Obesity, vitamin deficiency, gastritis, organic brain damage, alcoholic psychosis and dementia, cirrhosis
Alcohol Dependance
Alcohol dependence
Pattern of alcohol use involving problems controlling drinking, preoccupation with alcohol, use of alcohol even when it causes problems, drinking more to get the same effect, or having withdrawal symptoms with rapidly decreasing or stopping drinking
Alcohol tolerance
Increased ability to rapidly metabolize ethanol
Neurons in the CNS adapt to the presence of alcohol
Impact on health
Obesity
Vitamin deficiency
Gastritis
Organic brain damage
Alcoholic psychosis and dementia
Cirrhosis
Alcohol Dependance
Dependence
The inability to control the use of a physical substance.
A physical condition that cannot be controlled by willpower
Alcohol withdrawal symptoms
Agitation, circulatory disturbances, convulsions, delirium tremens, digestive disorders, disorientation, extreme fear, hallucinations, mental disturbances, nausea and vomiting, restlessness, sweating, temporary suppression of REM sleep, tremor, weakness
Treatment of alcohol withdrawal
May include benzodiazepine, anticonvulsant, beta blocker, antipsychotic
Folic acid, thiamine, multipurpose vitamin to treat underlying deficiencies
Complimentary and Alternative Therapy
Melatonin: Used for insomnia and benzodiazepine and nicotine withdrawal
Helps regulate circadian rhythms
Kava: Affects GABA and dopamine in the brain
Used for anxiety and insomnia
Risk of liver toxicity and liver failure
St. John’s Worts: Work similarly to SSRIs
Used for mild depression, psychological symptoms of menopause
Multiple drug interactions