Chapter 28
Assessment of Cardiovascular Function
Function of the cardiovascular system- deliver oxygenated blood to the tissues and return deoxygenated blood to the heart. Done by interaction of muscular pump, the heart and large complex of arteries and veins.
The primary job of the heart- propel blood from its left side into the aorta and the systemic circulation to provide oxygen and nutrients to the tissue.
Vascular system
The delivery of oxygenated blood to the tissues
The removal and transportation of cellular waste for excretion
The return of circulatory volume to the right heart
The return of lymph fluid back into the general circulation
Arterial system
consist of a thick-walled vessel whose function is to carry oxygenated blood from the heart to the tissues, done through a series of vessels gradually decreasing in size and then entering the smallest vessels, the capillaries.
Sequence of vessels- arteries- arterioles-metarterioles- capillaries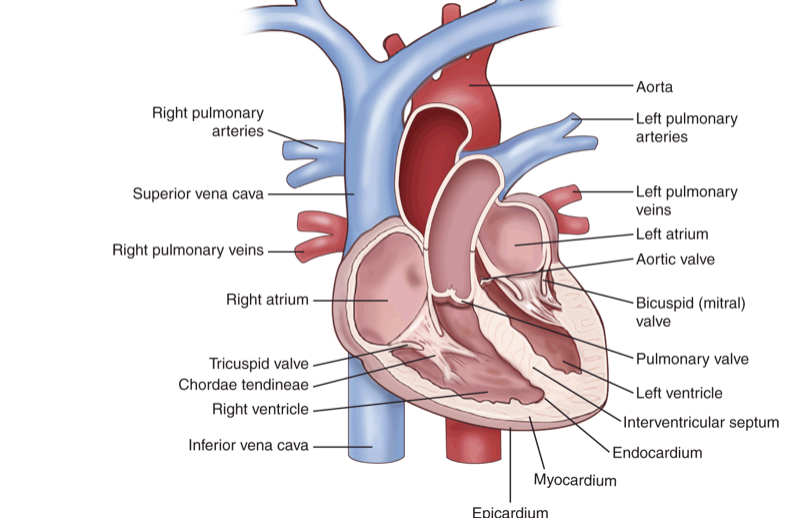 Venous system: low-pressure vascular circuit with vessels that contain valves to prevent retrograde or backward flow. Carry blood from the capillary bed through venules then veins, back to the right heart. Veins have the flexibility to adapt to changes in volume without large changes in pressure- allowing IV infusion and blood products.
Venous system: low-pressure vascular circuit with vessels that contain valves to prevent retrograde or backward flow. Carry blood from the capillary bed through venules then veins, back to the right heart. Veins have the flexibility to adapt to changes in volume without large changes in pressure- allowing IV infusion and blood products.
Capillary Bed: real work of the vascular system is done in the capillary bed. Oxygen and nutrients are delivered to the tissue and cellular waste is removed. When pre capillary sphincters are open capillaries are filled up with blood but when it closes the corresponding capillary shuts down, and blood travels through a thoroughfare channel, going directly from metarteriole to venule. blood is diverted to organs in need. e.g during exercise blood is supplied in plentiful to the skeletal but the skin is bypassed.
Anatomy of the heart
located in the thoracic cavity between the lungs in the space called mediastinum. lies behind the sternum and rest on the diaphragm. its contained in the pericardium sac.
The pericardium contains 2 layers
outer layer pericardial sac or parietal pericardium.
inner layer- the epicardium or visceral pericardium
btw the 2 layer there is a pericardial cavity that contains a serous fluid that provides a lubricant that allows the heart to beat without friction.
Layers: 3 layers
thin outer layer of the heart- epicardium
thick middle layer of the heart-myocardium (muscular layer responsible for the mechanical contractile function of the heart.)
thin inner layer- endocardium(lines the interior of the heart and heart valves)
Chambers: 4 chambers
right and left atria
right and left ventricles
The right atrium receives deoxygenated blood from the systemic circulation through the great veins, the inferior and superior vena cava.
Blood flows from the right atrium to the right ventricle.
It is then delivered to the pulmonary circuit through the pulmonary artery.
Newly oxygenated blood is returned to the left atrium via the pulmonary vein.
It flows to the left ventricle and is then ejected into the aorta to the systemic circulation.
Valves: facilitate one-way flow
The atrioventricular valves (AV)
Tricuspid valve- the valve between the right atrium and right ventricle.
Bicuspid or mitral valve- the valve between the left atrium and ventricle.
When open, the valves allow flow from the atria into the ventricle.
When the ventricles fill and the pressure within increases, the valves close to prevent retrograde flow back into the atria.
The valves are connected to a fibrous cord called chordae tendinea that prevents the valve from budging or turning inside out during ventricular contraction.
The Semilunar valves
The pulmonary valves-located between the right ventricle and pulmonary artery.
The aortic valve valves- located between the left ventricle and aorta.
Diastole: when the ventricles are relaxed during filling, the AV valves are open, allowing blood to flow into the ventricles. As the ventricles fill, the valves are forced upward and begin to close.
The pathway of blood flow through the chambers and valves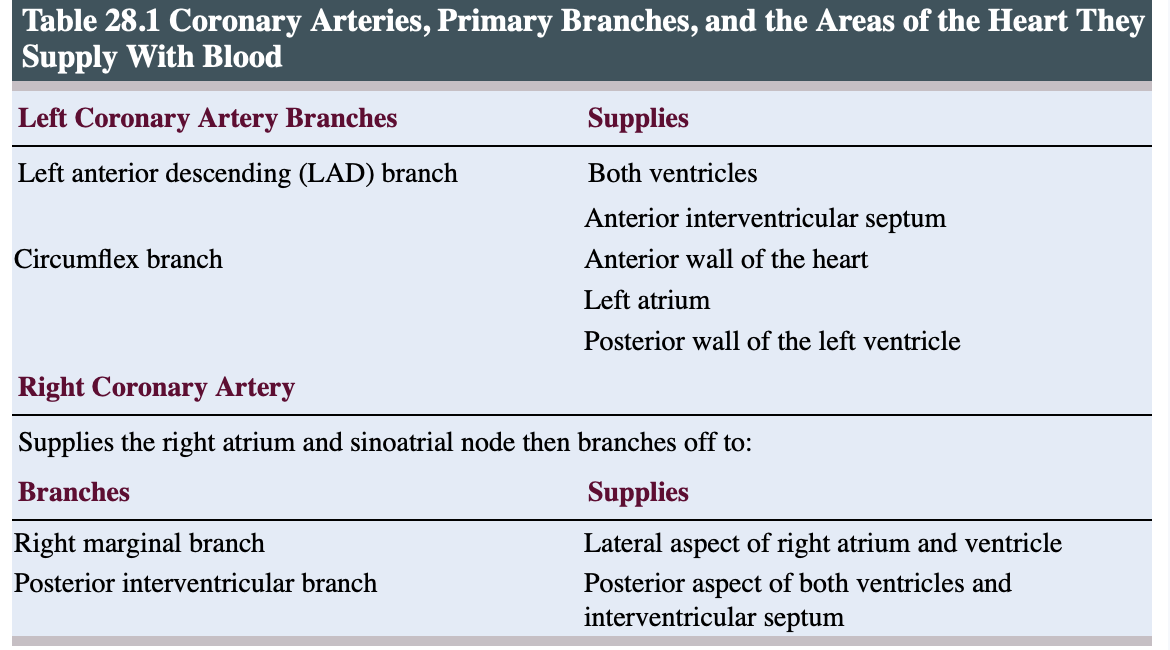 - When the increase in pressure from ventricular contraction exceeds the arterial pressure in the pulmonary circuit or aorta, the semilunar valves open, allowing blood to flow into the pulmonary or systemic circulation
- When the increase in pressure from ventricular contraction exceeds the arterial pressure in the pulmonary circuit or aorta, the semilunar valves open, allowing blood to flow into the pulmonary or systemic circulation
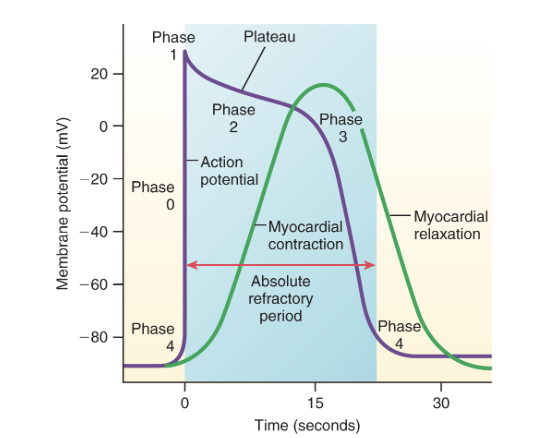
Blood supply to the heart
The major vessels that supply blood to the heart are the left and right coronary arteries.
They are the first arteries branching off of the aorta as it leaves the left ventricle, actually originating in the cusps of the aortic valve.
The arteries branch off into arterioles and capillaries, then eventually merge into capillary veins that drain the blood into a coronary sinus, which eventually empties into the right atrium.
Cardiac conduction- unique characteristics of the cardiac cells that facilitate cardiac electrical conduction are automaticity, excitability, and conductivity.
Automaticity- allows cardiac cells to generate impulses independently and rhythmically.
normal pacemaker- Sinoatrial (SA) node; 60-100bpm
Atrioventricular(AV node: 40-60bpm
and if both fail Purkinje fiber or ventricular cell can generate an impulse of 20-40bpm.
Excitability: ability to respond to a stimulus and generate an impulse
Conductivity: allows cardiac tissue to transmit impulses to neighboring connected cells.
Properties unique to cardiac muscles
Cardiac cells rely almost exclusively on aerobic metabolism for adenosine triphosphate production. Without the production of lactic acid that occurs with anaerobic metabolism, cardiac muscle can maintain its regular lifelong rhythm without tiring.
Cardiac muscle relies on extracellular calcium to facilitate calcium release from the sarcoplasmic reticulum to produce its muscular contraction. This is referred to as calcium-induced calcium release. It is regulated by the slow inward flow of positively charged calcium ions during the action potential.
Cardiac cells sustain a longer contraction, allowing the ejection of blood from the atria and ventricles.
Cardiac cells have a longer absolute refractory period, decreasing the possibility of repetitive, uncontrolled muscular contractions called tetany.
Cells of electrical conduction system- potential pathway
The impulse originates in the SA node. The SA node has an inherent rate of 60 to 100 bpm.
The impulse spreads through the atria through the internodal pathways to the
Atrioventricular node, where the impulse is delayed to allow for atrial contraction and complete ventricular filling.
It leaves the AV node through the bundle of His and branches off into the …
Right and left bundle branches, which travel down the interventricular septum to end in the …
Purkinje fibers, which extend the impulse into the ventricular tissue, facilitating ventricular contraction.
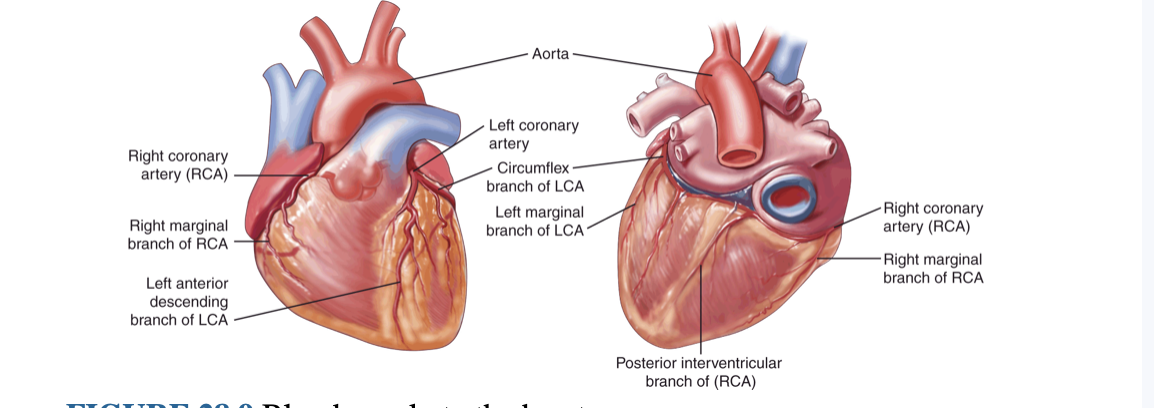
Action Potential of the Cardiac Conduction System
A stimulus begins the movement that produces the cardiac action potential: membrane potential, the difference in charge between the interior and exterior of the cell, changes or goes up and down in a consistent pattern.
Depolarization: movement of ions preceding and facilitating cardiac mechanical contraction.
Repolarization: movement of ions back to the resting state, the cardiac resting membrane potential of –90 mV, to allow for the initiation of another action potential
Five phases of action potential
Phase 0: Rapid depolarization caused by the opening of sodium (Na+) channels, allowing rapid Na+ influx, moving the membrane potential to +30
Phase 1: Decrease in Na+ influx, causing a slight movement toward negative of the membrane potential, producing an initial repolarization
Phase 2: Plateau state caused by an influx of calcium (Ca++) through the opening of Ca++ channels balanced by a slight outflow of potassium (K+)
Phase 3: Final repolarization caused by the closing of the Ca++ channels and the rapid outflow of K+
Phase 4: Return to resting membrane potential.
Absolute refractory period: represents a time when a greater-than-normal stimulus may initiate an impulse- end of phase 3
Electrocardiogram: an electrical activity that produces waveform, which is amplified and viewed on paper tracing.
Electrodes placed in the wrist, ankle, and six locations in the chest help produce a picture of the electrical activity of the heart.
Principal waveform produces P wave, QRS complex, and T waves.
Principal segments include PR segment and ST segment
Intervals include PR interval, QRS interval, and QT interval
P waves: atrial depolarization
PR interval- time required for atrial depolarization and the delay of the impulse at the AV node.
PR segment- delay at the AV node
QRS complex- ventricular depolarazation
QRS interval- time required for ventricular depolarization
T waves- atrial depolarization occurs during ventricular contraction
QT interval; time required for ventricular depolarization and repolarization
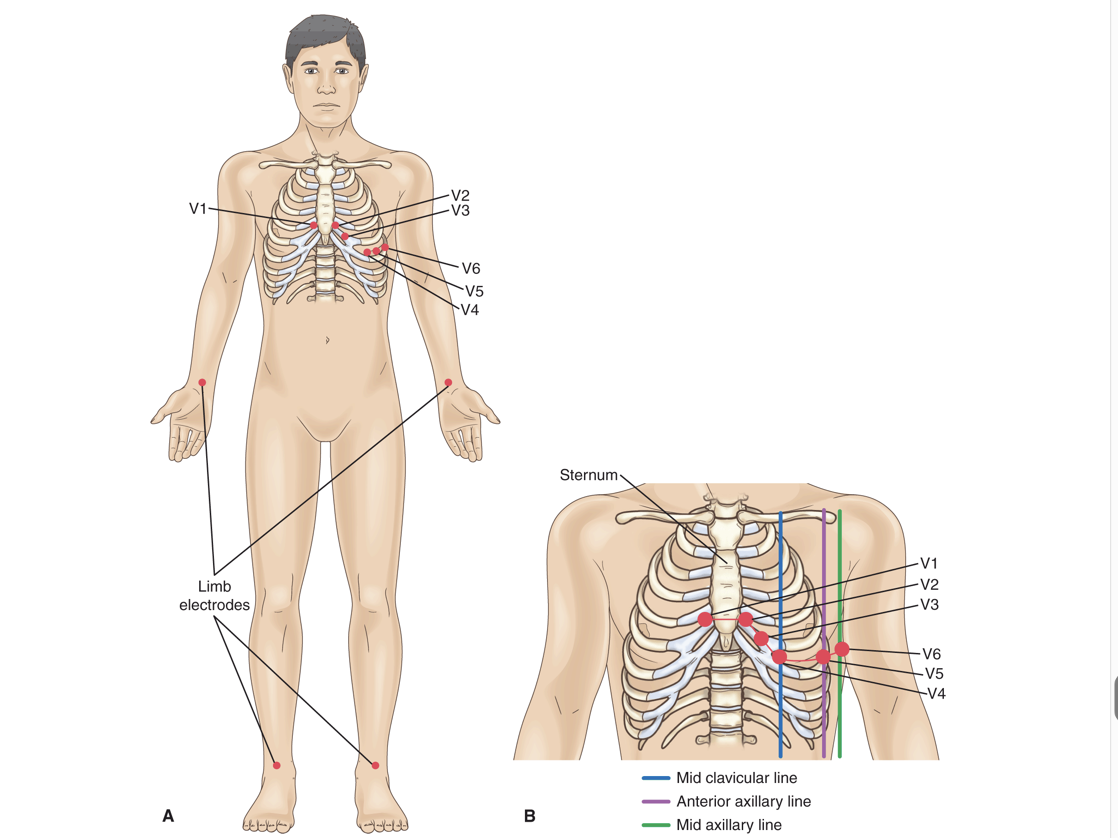 Chest placement of Electrodes
Chest placement of ElectrodesV1: 4th intercostal space, just to the right of the sternum
V2: 4th intercostal space, just to the left of the sternum
V4: On the midclavicular line and 5th intercostal space
V6: On the midaxillary line, horizontal with V4
V5: Between V6 and V4 on the anterior axillary line
V3: Between V4 and V2
Cardiac cycle: circular sequence of events that produces the eventual muscular contraction that causes the ejection of blood from the right ventricle into the pulmonary circulation or from the left ventricle to the systemic circulation.
2 parts
Systole or contraction:- facilitates the ejection of blood from the ventricles and occurs during the last one-third of the cycle.
isovolumetric contraction- pressure increases, but there are no volume changes
Diastole or relaxation:-filling of the ventricles occurs and accounts for the first two-thirds of the cycle.
the ventricle is relaxed, lower bp of atria allows the AV valve to open
Atrial systole: The final phase of ventricular filling occurs when the atria contract
Atrial kick: which accounts for the final 30% of ventricular filling
Preload: The final volume in the ventricle at the end of the diastole is the end-diastolic volume.
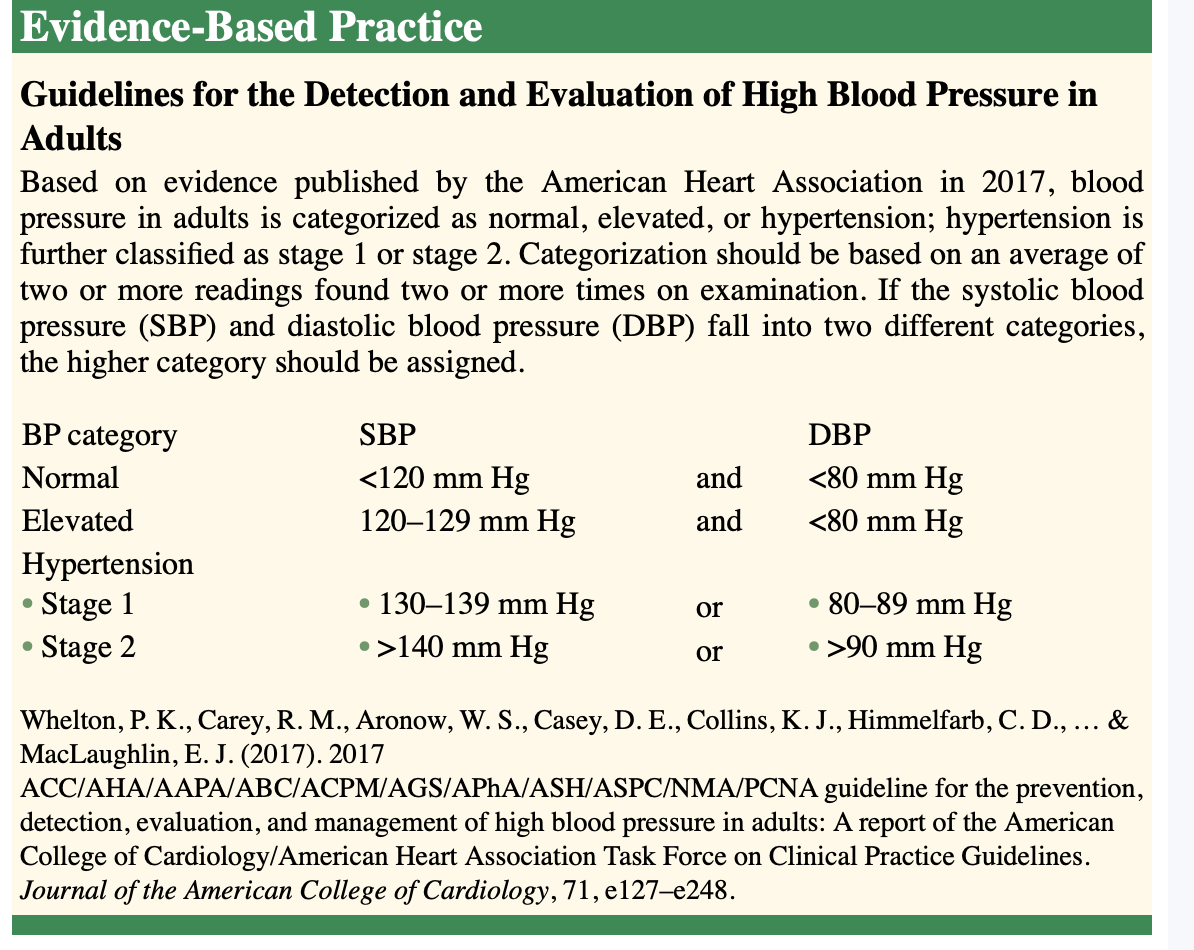
Blood pressure- a reflection of the pressures generated during a cardiac cycle. represents the force exerted against the vessel wall by blood flow. factors that influence BP are the amount of blood ejected during systole, Cardiac output and the resistance to flow in the peripheral vessels or peripheral vascular resistance.
2 pressure
Systolic: Systolic is the peak pressure generated when blood is expelled from the left ventricle during ventricular contraction.
Diastolic: minimal pressure maintained on the vessel walls during relaxation
Mean arterial pressure is the average pressure maintained throughout the cardiac cycle.
changes that influence blood pressure include- controlled by ANS
blood flow or volume and resistance to flow
increase or decrease in the blood volume
CO increases or decreases BP.
ANS respond from baroreceptor and chemoreceptors’
Baroreceptors
located in the aortic and carotid arches, are sensitive to changes in pressure.
An increase in pressure stimulates the parasympathetic nervous system to dilate vessels and reduce the heart rate (HR) to reduce BP.
The decrease in pressure stimulates the sympathetic nervous system to constrict vessels and increase the HR, which increases BP.
Chemoreceptors
contained in collections of cells called carotid bodies and aortic bodies are located in the aortic arch and in the carotid arteries.
They respond to changes in oxygen and CO2 concentrations.
Decreased levels of oxygen with increased levels of CO2 produce acidosis.
The chemoreceptors respond to decreased oxygen levels and acidosis by inducing vasoconstriction to increase BP and increase blood flow to the lungs, facilitating oxygen and CO2 exchange. The respiratory rate (RR) is also increased.
Hormonal mechanisms: exert control over BP include
Angiotensin II: created in response to low BP.
After a drop in BP, the kidneys respond by releasing the enzyme renin.
Renin reacts with angiotensinogen to create angiotensin I.
Angiotensin I is then converted in the lungs to angiotensin II via angiotensin-converting enzyme.
Angiotensin II is a potent vasoconstrictor that increases BP.
Angiotensin II also acts on the adrenals to release aldosterone
epinephrine and norepinephrine
Epinephrine and norepinephrine, catecholamines released by the adrenal medulla, cause vasoconstriction, leading to increases in BP as part of the fight-or-flight mechanism in the sympathetic nervous system.
aldosterone
The release of aldosterone promotes sodium and water reabsorption in the kidneys, which increases circulating fluid volume- renin-angiotensin-aldosterone system.
antidiuretic hormone.
released by the posterior pituitary in response to the decreased blood volume. It acts on the kidney to conserve water.
Cardiac Output: Blood ejected from the left heart each minute to facilitate the delivery of oxygen and nutrients to the tissues
normal cardiac output in adults is 4 to 8L/min
value is influenced by exercise or activity and decreased at time of rest.
Cardiac output is calculated by the formula HR × stroke volume (the amount of blood ejected with each ventricular contraction)
Heart rate: number of cardiac contractions per minute
variables that affect HR
Stimulus from the ANS
HR can be increased or decreased depending on pressure. e.g. low bp increases HR to maintain adequate CO.
Stimulation from the SNS caused by the baroreceptor increases HR through the release of norepinephrine.-Posititive chronotropic effect.
The parasympathetic nervous system slows the HR through the release of acetylcholine, a negative chronotropic effect.
Epinephrine and norepinephrine increase HR when released from the adrenal medulla.
Stroke Volume: the amount of blood ejected with each ventricular contraction. It is influenced by three variables: preload, afterload, and contractility.
preload = the central venous pressure; afterload = the systemic vascular resistance or pulmonary vascular resistance.
Preload: amount of blood in the ventricles at the end of diastole, It also refers to the amount of stretch of the muscle tissue at the end of filling. Increased volume produces increased stretch, which produces an increased contraction (Starling’s law). Extreme overfilling decreases the effectiveness of the contraction, thus decreasing CO.
Afterload: resistance to flow the ventricle must overcome to open the semilunar valves and eject its contents. related to Bp, vessel lumen diameter, and or vessel compliance.
Contractility: the force of the mechanical contraction. Contractile force can be increased with sympathetic stimulation or calcium release. It can be decreased in the face of hypoxia or acidosis.
Major risk factor of CVD
Family history of CVD
diabetes mellitus
chronic renal disease
hypertension
dyslipidemia.
Modifiable risk factor
Weight
Dietary habits
alcohol consumption
smoking history
excessive consumption of fat and sodium
sedentary lifestyle
Nonmodifiable risk factor
age
sex
ethnic background
significant complaint pertinent to heart disease
presence of chest pain- location, intensity, radiation, duration and quality.
Difficulty breathing- dyspnea at rest or exertion
cough
palpitations- abnormal heart rhythms
edema
fatigue
syncope- an indication of decreased CO due to electrical or mechanical properties of the heart.
weight gain associated with edema indicates weakened heat and the presence of heart failure.
General assessment
initial assessment: pt’s overall appearance; color, diaphoresis, edema and demeanor or restlessness, agitation, or confusion.
A patient with cardiac disease may appear pale, fatigued, or short of breath. Patients with late-stage heart failure will present with edema and appear frail and fatigued.
An apical rate can be auscultated by placing a stethoscope at the junction of the fifth intercostal space and the midclavicular line, the point of maximal impulse (PMI).
a lower HR can indicate good physical condition- efficient heart
or may indicate inadequate CO
higher HR naturally occurs with exercise and exertion
abnormal when at rest- weak heart muscle, pain, fever, inadequate fluid volume.
Pulse deficit: occurs if performed at the same time, the apical pulse rate is less than the radial pulse- arrhythmia such as AFIB, or premature ectopic beats.
High BP indicates resistance in the vessels, requiring higher pressures to produce an adequate CO.
High BP increases the risk of heart failure
myocardial infarction,
stroke
The presence of postural hypotension, a decrease of 20 mm Hg in BP when moving from a lying or seated position to a standing position accompanied by a 10% increase in HR, dizziness, SOB, and/or syncope, could indicate inadequate CO or blood volume and requires further evaluation.
Inspection
Cyanosis: poor perfusion produces a pale gray or bluish color.
In dark-skinned people, adequate perfusion produces the same pink coloring as the nailbeds.
Cyanosis appear gray
Cyanosis can be central or peripheral
Central cyanosis appears as blue coloring in the mucous membranes, lips, and tongue. It is usually caused by impaired heart or lung function.
Peripheral cyanosis, or blue discoloration of the extremities, can be caused by heart or lung failure but may also indicate peripheral vasoconstriction or obstruction
Capillary refill tested by compressing a finger or toe for a moment to stop blood flow
A return to color within 3 seconds indicates adequate peripheral circulation.
A sluggish return may indicate arterial spasm or insufficiency.
Edema may be a sign of cardiac or liver issues
Bilateral lower extremity edema, if not associated with a local injury, generally indicates venous insufficiency or heart failure.
Unilateral extremity edema, again if not associated with injury, can indicate a venous or lymphatic obstruction.
Edema is identified as pitting or nonpitting.
Pitting edema is characterized by an indenting of the skin that remains after pressure has been applied and then released.
Jugular vein distention: may be present in a patient with a constrictive disease such as pericarditis or cardiac tamponade.
It is also seen in patients with right ventricular failure, valvular disease, or hypervolemia.
It is often associated with poor contractile function of the heart that is present in heart failure
Clubbing of the fingers and or toes: indicates long-term perfusion problems produced by a decrease in oxygenated blood flow to the affected extremities.
This is typically caused by congenital heart defects or chronic pulmonary disease.
It can also be seen in patients with lung cancer.
Heart sounds- varies with age
lubb and dubb heart with auscultation- produced by the closing of the valves during the cardiac cycle.
The S1 sound heard with the closure of the AV valves- signifies the beginning of ventricular systole.
lounger and louder than the s2
S2 heart sound-closing of the semilunar valves- signifies the beginning of the diastole
short and soft
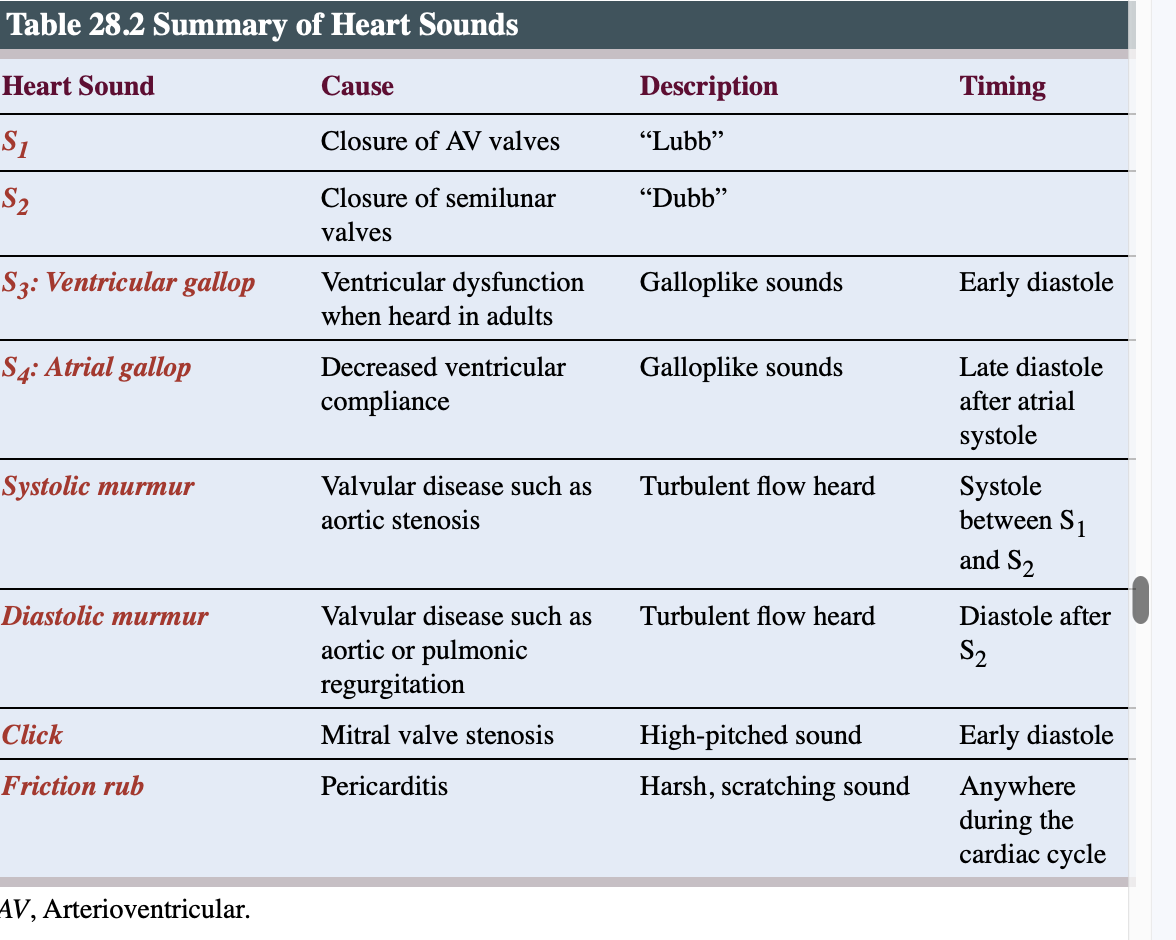
S3 heart sound, heard in children and young adults, is caused by vibration in the ventricular walls during filling or early diastole.
If heard in an adult, it may indicate decreased ventricular compliance.
Ventricular gallop is the combined sound of S1, S2, and S3.
S4 heart sound is heard in late diastole and occurs right after the atrial contracts
may indicate decreased ventricular compliance. It is known as an atrial gallop
A click is a high-pitched sound heard early in diastole and is typically caused by mitral valve stenosis.
Murmurs are usually caused by turbulent flow through the valves. That turbulence can be caused by regurgitation of blood through an incompetent valve, flow through a narrowed valve, or an increase in flow in hypermetabolic states such as hyperthyroidism or fever.
A friction rub is described as a scratching or grating sound heard during both systole and diastole. The sound is produced by inflammation of the pericardium. It is diagnostic for pericarditis and is referred to as the pericardial friction rub.
When describing heart sounds its important to note
Pitch: high, medium, or low
• Quality, such as blowing or harsh
• Intensity, such as faint, quiet, or loud
• Timing during systole or diastole
• Location where heard best on the chest wall
Lung sound
Clear breath sounds signify a healthy heart and lungs.
Auscultation of rales, rhonchi, or rubs in the lung fields indicates the presence of fluid.
Diagnostic studies
Lipid panels include: require pt to fast 8-12 hrs prior to test
Total cholesterol- lipid necessary for the synthesis of hormones and cell walls.
available through ingestion of animal products e.g meat
synthesis in the liver
not soluble in blood- combines with protein to form lipoprotein, LDLs, and HDLs to facilitate transport through the vascular system.
normal level is 200mg/dL
High-density lipoprotein (HDLs)
transport cholesterol away from the cells to the liver for excretion.
decreased levels of HDLs, less than 40 to 60 mg/dL, are a risk factor for heart disease.
Lipoproteins(LDLs): primarily transport cholesterol into the cell but can also deposit it on the walls of arterial vessels.
Elevated levels, greater than 100 mg/dL, are associated with an increased risk of heart disease.
Triglycerides: store unused ingested calories in fat cells, which may be later released as an energy source between meals.
Elevated levels, greater than 150 mg/dL, are another risk factor for heart disease.
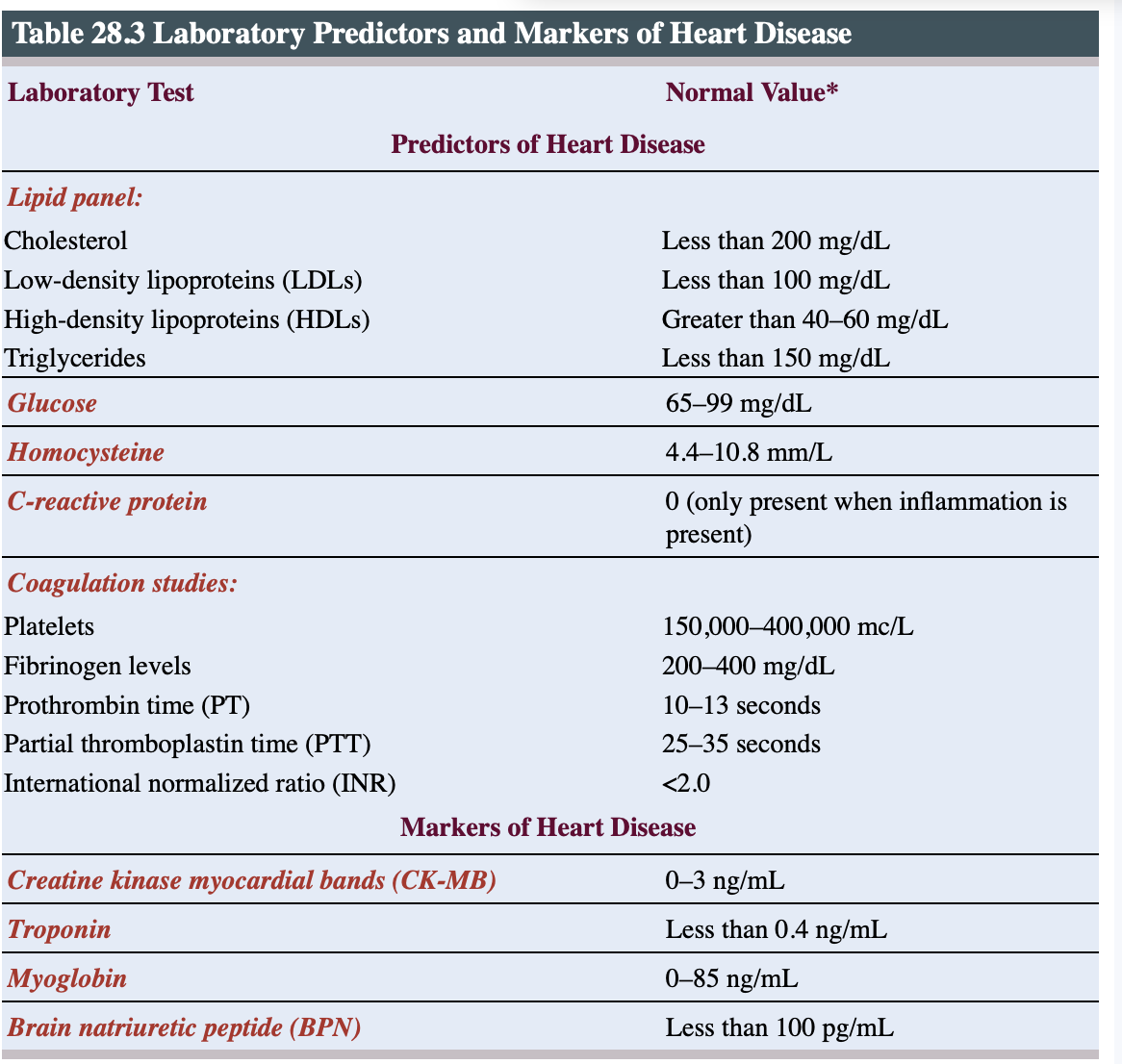
Cardiac markers that indicate cardiac damage or injury
Creatine kinase (CK): a general marker of cellular injury. release from the cells to the brain, skeletal muscle, and cardiac tissue after muscle damage has occurred. One isoenzyme of CK, creatine kinase myocardial bands (CK-MB) is the marker specific to cardiac tissue.
CKMB- CK-MB is released from the cells.
Increased levels can be seen at 3 hours after myocardial damage
Can remain elevated for up to 36 hours before returning to normal.
Troponin-preferred method of diagnosing cardiac injury
It is a protein released from damaged tissue
can elevate within 4 hours of injury.
It can stay elevated for up to 10 days.
Myoglobin is released and elevated in muscle damage but is not specific for cardiac tissue.
It can be used in conjunction with the other values to help rule out or rule out a myocardial infarction.
Brain natriuretic peptide (BNP) is released from overstretched ventricular tissue.
Physiological responses to increased levels of BNP include venous dilation, which decreases preload; arterial dilation, which decreases afterload; and diuresis.
Elevations are an indicator of heart failure
When a patient is evaluated for acute injury, laboratory tests are obtained at baseline and then at regular intervals (typically 3 to 4 hours) for approximately 12 hours. It is important to obtain samples in a timely fashion and accurately note the time each blood sample is obtained
Echocardiography: ultrasound to provide information on the size and pumping function of the heart, blood-volume status, and valve function and integrity.
2 types; of echocardiography are the transthoracic echocardiogram (TTE) and the transesophageal echocardiogram (TEE).
TEE is obtained by placing the ultrasound transducer in the patient’s esophagus
It is used when complications such as obesity or lung disease may obscure the standard TTE by interfering with the transmission of the ultrasound sound waves anteriorly.
risk factor for stroke, is more easily viewed through TEE.
Nursing implication
for a TEE exams- pts are instructed to fast 8hr prior to procedure
small sip of water with medication are exception
pt are sedated so they eed someone to drive them home.
Cardiac stress testing: done to evaluate heart functioning during times of increased workload. It is a way to evaluate the functional ability of the heart
regular stress test is done while pt is exercising on the treadmill and chemical is induced when a pt is unable to tolerate the exercise medication such as dobutamine is administered to stimulate the heart.
Isotope or nuclear stress testing is a combination of a regular stress test and a chemical stress test. In this case, the chemical is an intravenously injected nuclear isotope tracer such as thallium. The purpose of this test is to visualize areas of poor perfusion in the heart due to blocked arteries.
Nursing implication
do not drink or eat 4 hrs prior to the test
avoid smoking and caffeine prior to the test.
Catherization and angiography:
Cardiac cauterization: is an invasive x-ray procedure during which a radiopaque catheter is advanced through an artery or vein to the heart under fluoroscopy in order to evaluate cardiac filling pressures, CO, and valvular function.
A right heart catheterization can be done through a suitable vein (femoral, brachial, subclavian).
A left heart catheterization is done through a suitable artery (femoral, brachial, radial)
Coronary angiography: primary reason cardiac catheterization is performed.
It is a left-sided cardiac catheterization with the purpose of inspecting the coronary arteries for blockage and determining the necessity of revascularization procedures such as percutaneous coronary intervention or coronary bypass surgery.
It is done through a technique called cineangiography.
Once the catheter is in place, contrast dye is injected that allows visualization of the vessels. Multiple consecutive images (15 frames per second) are obtained.
Risk of cardiac catheterization
include dysrhythmia
extrasystole or irregular beat
risk for bleeding
risk for infection
myocardial infarction
perforation of the heart or great vessels
stroke
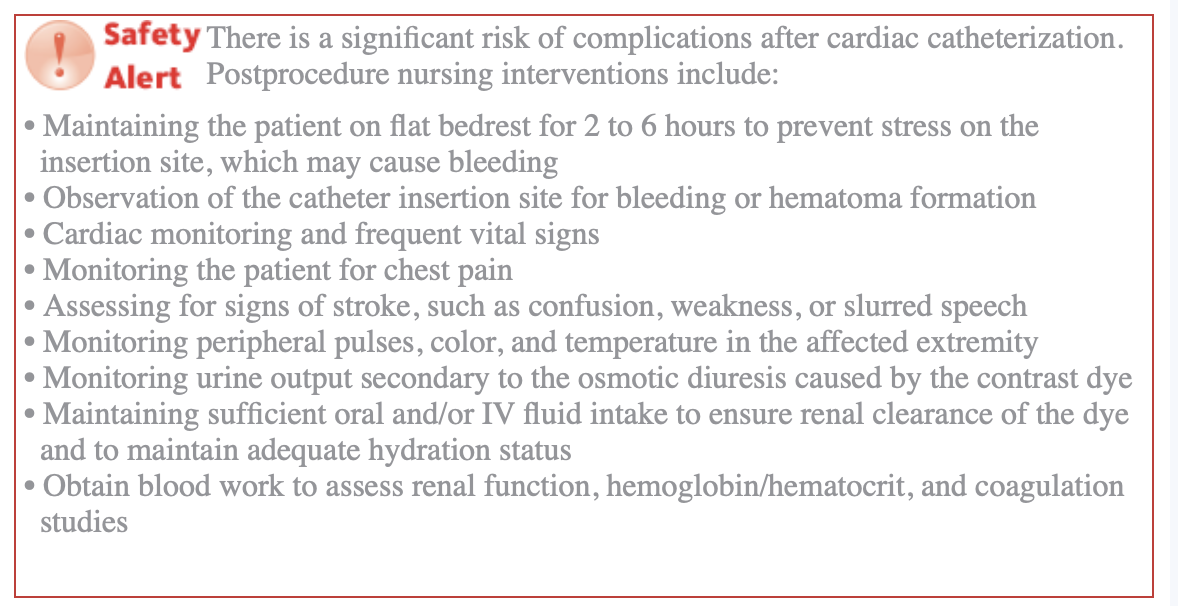
Nursing implication
Fasting 6 to 8 hours prior to procedure
• Expected duration and activities to expect (IV insertion, sedation) during procedure
• Information regarding potential sensations that may be experienced during the procedure, such as a “hot flash” as the dye is injected or palpitations if dysrhythmias occur
• Maintaining adequate fluid intake after the procedure
• Avoiding strenuous activity until your provider gives the OK to resume normal activities
• Monitoring cannula insertion site for bleeding
Pre-procedure care includes:
• Establish baseline vital signs
• Review blood work focusing on renal studies
• Complete pre-procedure checklist that includes obtaining height and weight and ensuring patient has been NPO
• Administer pre-procedure hydration
• Check glucose levels while NPO
• Anticipate holding diabetic medications
Intraprocedure nursing interventions for cardiac atheterization include:
• Psychological support of the patient during the procedure to help ease fears
• Vigilant cardiac monitoring during the procedure to observe for dysrhythmias
• Readiness and ability to respond with advanced cardiac life-support interventions should a lethal dysrhythmia occur
Age related changes
Physical deconditioning can result in atrophy of the left ventricle, decreased elasticity of the aorta, and rigidity of the valves
Stenosis of the heart valves, stiffening of the arterial walls, and increased fibrosis of the heart chambers, leading to hypertension
Formation of atherosclerotic plaques and narrowing of the arterial walls, leading to increased risk of thrombosis and stroke