Lecture 9
Lymphoid Anatomy
Three tiers (levels) of Lymphoid Structures
Primary Lymphoid Tissues – Generate lymphoid cells
Secondary Lymphoid Tissues – Facilitate antigen sampling from tissues and organs in the body. Facilitates the activation of antigen specific responses
Tertiary Lymphoid Tissues – Specialized immune responses in inflamed tissues
Primary: RED ; Secondary: BLUE ; Tertiary: ?
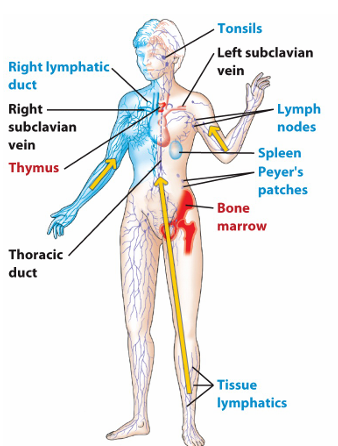
Primary Lymphoid Tissues: Bone Marrow and Thymus
*Specialized structures to facilitate the differentiation of antigen-specific lymphocytes
Bone Marrow
Primary site of hematopoiesis in adults
Produces both myeloid and lymphoid cells
Houses Hematopoietic Stem Cells (HSCs) in the perivascular niche, HSCs divide to become progenitor cells
Progenitor Cells:
Myeloid Progenitors → innate immune cells
Lymphoid Progenitors → adaptive immune cells
Some mature and effector cells return to the bone marrow for long-term survival
Thymus
Specialized for T cell development
Secondary Lymphoid Tissues (2° LTs)
* Specialized structures to educate and activate antigen-specific lymphoid cells, they’re organized to facilitate this process.
Facilitate antigen recognition and lymphocyte activation
T cells (T cell zone) and B cells (follicles) have separate zones in these structures
Connected with the local environment/tissue in order to sample antigens.
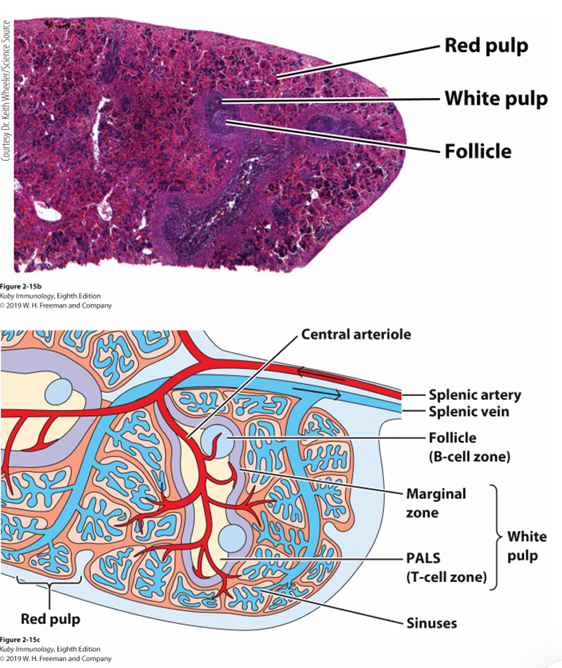
Spleen
*Largest of the secondary Lymphoid tissues and it’s integrated into the circulation.
Red Pulp – Open sinusoids with no endothelium, slow moving blood, filters blood, old RBCs specially.
White Pulp – contains T cell zones and B cell follicles. Ideally placed to sample Antigens in the blood. Antigens enters via marginal zone
Marginal Zone – antigen entry point. part of the white pulp
Lymph Nodes
Composed by the lymphatic system and lymphatic vessels
Embedded in most tissues and organs
One main function is to return extracellular interstitial fluid to the circulation
Lymphatic vessels collect and transport antigens to nodes
Lymph nodes are located in junctions where they can effectively filter lymph and initiate immune responses.
Afferent lymphatics (Lymph goes in)
Efferent lymphatics (Lymph goes out)
Antigens and some immune cells enter lymph nodes through afferent lymphatic vessels
High Endothelial Venules (HEV) allow T and B cell entry to lymph nodes. These venules allow immune cells to move from the bloodstream into the lymph nodes.
Mucosal-Associated Lymphoid Tissues (MALT / GALT)
Located in mucosal surfaces (intestines, airways, reproductive tract)
M cells capture and transport antigens for immune activation
Important for microbiota regulation
Tertiary Lymphoid Tissues (3° LTs)
Form in chronically inflamed tissues
Can be organized (follicles, T cell zones) or disorganized clusters
Key Questions:
Do they worsen or improve inflammation?
Are they a result of tissue remodeling?
Lymphoid Lineage and Cell Types
Lymphoid Lineage Development
Begins in the bone marrow
Common Lymphoid Progenitor → Differentiate into immune cells
Covered in Lectures 10-11, 14, and 15
Innate Lymphoid Cells (ILCs)
Do not have antigen-specific receptors
Act similar to myeloid cells but belong to the lymphoid lineage
Key example: Natural Killer (NK) Cells
Natural Killer (NK) Cells
Target Recognition
Identify stressed or infected self-cells
Balance between activating (kill) and inhibitory (don’t kill) signals
“Missing Self” Hypothesis
Some viruses and tumors reduce MHC expression to evade detection
NK cells detect this loss and trigger killing
Important NK Cell Receptors
NKG2D (activating receptor) – detects stress-induced molecules
KIR / Ly49 family (inhibitory receptors) – recognize MHC class I
Effector Mechanisms
Kill infected/tumor cells by inducing apoptosis
FasL pathway
Perforin/Granzyme B pathway
Cytokine production:
TNF-α
IFN-γ
Lymphoid Cells and Anatomy Summary
Innate Lymphoid Cells function like myeloid cells and distribute widely
Adaptive Lymphoid Cells (B and T cells) require specialized lymphoid structures
Lymphoid structures integrate into tissues to detect antigens
Lecture 9 Outline
Lymphoid Cells
T and B cells (antigen-specific)
NK cells & innate lymphocytes
Target recognition & effector functions
Lymphoid Tissues
Primary (Bone Marrow, Thymus)
Secondary (Spleen, Lymph Nodes, MALT)
Organization & antigen access