1640
Learn about different types of stigmas and any real-life examples associated with them.
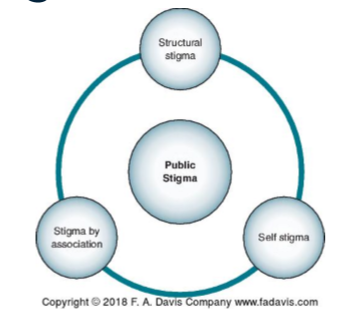
Public stigma—negative stereotypes of individuals with the specific condition by others
Self-stigma—individuals agree with and internalize negative stereotypes
Labeling Theory: judgement from people with power and authority, deciding if behaviors deviate from the norm.
Overemphasizes the process of labeling
Normalization Theory: force individuals int a deviant role, their behavior and responses determined by the expectations surrounding that label
Emphasize opportunities for social role development
Emphasizes the need of a person with disability to change and “fit in” rather than for society adapting to accept the differences.
Structural stigma: restricts opportunities for people with mental illnesses or create unintended consequences that limit opportunities for participation
OTs use skills to advocate and deconstruct stigma
Stigma in Mental Health Care
Negative attitudes and beliefs 🡪 public stigma deterring help-seeking.
Responses:
Discrimination
Social distance (excluding someone)
Poor parenting
Genetics
Substance abuse
Affects:
Negative impact on coping behaviors
Discrimination:
Housing
Education
Employment
Stigma and Culture:
Stigma is universal and, in all cultures,
OTs need to understand:
Client lived experiences of stigma
Collaborate with client and family to address impact of stigma and cultural responses
Family Stigma: family, spouse, partner, and network of friends
Key attributes:
Unusualness
Member poses danger or threat
Contamination
Measurements of Stigma:
Self-Stigma of Mental Illness Scale
Internalized Stigma of Mental Illness
Both instruments can be used to understand the level to which a person self-stigmatizes.
Practitioners should incorporate discussion of the results of these assessment tools.
Anti-Stigma Interventions:
Anti-stigma programs
Education
Social contact
Advocacy
Public Stigma
Contact based education
Self-Stigma:
Narrative enhancement and cognitive therapy
Reduction programs
Pyscho-education
Cognitive-behavioral therapy
Improves negative self-appraisal
Motivational interviewing
Social skills training
Goal attainment
Music therapy:
Stigma and Occupational Justice:
Universalism:
Marginality
Exclusion
Disaffiliation
Interventions:
Advocacy
knowledge of civil rights
Formation of strategic community alliances
Working to remove attitudinal and other barriers in “regular” work environments
Developing meaningful supported employment
Exploring volunteerism and consumer-run businesses
Pryor & Reeder’s Model of Stigma
/
System in place designed to be inequitable
Stigma attached to you
Stigma-bias
Occupational profile and what is occupational performance and its analysis?
Occupational Profile:
Occupational Performance:
Know about evaluation and its process, what to consider, and the practice model
Evaluation Process Steps:
Screen data to guide therapeutic reasoning
Whis is the person? What do I know? What are their concerns?
Choose assessments
Consider:
Utility (quality of life)
Validity (measure what intends to be measured)
Reliability (consistency of measure)
Administer assessment
Obtain consent
Gather material
Establish rapport
Occupational profile
AOTA template structure
Identify occupational importance
Analyze occupational performance
Synthesize data and set goals
Specific
Measurable
Attainable
Relevant
Time
Reevaluate
Ongoing process
Measures outcomes
Is intervention effective?
Build body of evidence that supports occupational therapy
Takeaway: Evaluations are linear & client-centered
OT Process:
Intervention
Reevaluation
Evidence-Based Practice in Mental Health
Learn about the assessment tools and how to select them
Different dimensions of wellness and examples and purpose of wellness inventory
Health Disparities of Wellness:
• High rates of smoking
• Sedentary lifestyle
• Symptom burden
• Poor self-care skills
• Higher disability status
• Lower (poorer) quality of life
• Social determinants of health
• Co-occurring medical and mental disorders
• Access to quality care
• Trauma
• Environmental contexts
• Economic factors
• Lifestyle factors
Role of Occupational Therapy:
Wellness lifestyle: balance of healthy lifestyle
Collaboration between the provide and individual in recovery
Holistic and client-centered approach
Health passport
Screening tool 🡪 mental illness & co-occurring illness
Health promoting lifestyle profile 2
Questionnaire
Wellness inventory
Likert scale 🡪 mental illness & substance abuse
THESE ARE STRATEGIES TO BUILD HEALHTY LIFESTLES
Interventions for Wellness:
Spiritual dimension
Social dimension
Intellectual dimension
Emotional dimension
Occupational dimension
Environmental dimension
Financial dimension
Evidence-based practice and its cycle
Conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients
Principles of evidence-based medicine
Cycle of EBP:
Identify the problem & ask a question (Why)
Identify the relevant evidence (use key words to search)
Evaluate the evidence (critically appraise the quality of selected studies)
Implement useful findings (use evidence to make decisions on what assessment or intervention to use)
Evaluate the outcomes (reflect on practitioner and client’s experiences to make clinical decisions)
Types of burden-Objective vs Subjective
Subjective Burden: feelings of grief, loss of hope, feelings of exhaustion through long periods of time
Objective Burden of Caring: More tangible
Stressors of caring impacts family associated with the members illness
Cultural Barriers in Mental Health:
Cognitive
Affective
Values-related
Physical or structural in nature
Family Resilience:
Building proactive and recovery factors
Reduce environmental risks that threaten family
Focus on strength-based approaches
Takeaway: coping during life transitions, stress, or adversity
Framework:
Family as central unit of attention
Maximize options and choices
Strength-focuses perspective
Recovery – process of change to improve health and well-being (being the best version of self)
4 dimensions: health, hope, purpose, and community
Role of family in mental health and its conceptualization
Conceptualization:
A dynamic social system composed of individuals whose patterns of occupations and interactions are interrelated
Terms such as family psychoeducation or support groups
Therapeutic use of self-Different types of communication with examples
Person-centered care requires collaboration
Collaboration is a process of mutual participation between the person and the practitioner and is a critical element in person centered care
This occurs within the context of a therapeutic relationship which requires therapeutic use of self
Therapeutic use of self refers to the therapist’s “planned use of his or her personality, insights, perceptions and judgments as part of the therapeutic process”
Therapeutic Modes:
Advocating: ensuring that the person’s rights are enforced and resources are secured, may require the practitioner to serve as a mediator, facilitator, negotiator, enforcer, or other type of advocate with external persons and agencies.
Collaborating: expecting the person to be an active and equal participant in therapy; ensuring choice, freedom, and autonomy to the greatest extent possible.
Empathizing: understand the person’s thoughts, feelings, and behaviors while suspending any judgment; ensuring the person verifies and experiences the practitioners understanding as truthful and validating.
Significantly correlates to MOHOST 🡪 motivation and overall participation in rehab
Encouraging: seizing the opportunity to instill hope in a person; celebrating a person’s thinking or behavior through positive comments; conveying an attitude of joyfulness, playfulness, and confidence.
Instructing: carefully structuring therapy activities and being explicit with people about the plan, sequence, and events of therapy; providing clear instruction and feedback about performance; setting limits on a person’s request or behavior as needed
Problem-solving: facilitating pragmatic thinking and solving dilemmas by outlining choices, posing strategic questions, and providing opportunities for comparative or analytical thinking.
Different types of disruptive behavior disorders, their effects on different occupations, medication effects
Oppositional defiant disorder:
Pattern of defiance lasting at least 6 months by at least 4 symptoms
Exhibited during an interaction with someone that isn’t a sibling
Intermittent Explosive Disorder:
Recurrent & represent failure to control aggressive impulses
Twice weekly for 3 months
3 outburst 🡪 property damage or physical injury to another within 12 months
Conduct disorder:
Longstanding, violates rights of other and of social norms 🡪 little to no remorse for behavior
Impairment in social, academic, or occupational functioning
Antisocial personality disorder:
18 years and older w/ history of symptoms of conduct behavior before 15 yrs old
Pattern of disregard for and violation of the rights of others
Pyromania:
Deliberate and purposeful fire setting more than once
Kleptomania:
Tension or anxiety that is relieved by stealing
Impacts on Occupational Performance:
Changing life roles require skills client might not have developed
Unable to follow protocols
Difficulty following societal rules 🡪 legal issues 🡪 incarceration
ADLs
Self-care, day to day, sleep habits, etc
Academics & employment
Requires ongoing support and development of self-management strategies
Medication:
Proper dosage
Intended to help control and enable for better participation
Side effects
Consequences of leisure activity and play participation
Exploration & Participation
Leisure: autonomy, leisure competence, and social support
Play: framing, internal locus of control, intrinsic motivation, & freedom from the limits of reality
Affecting Factors Leisure & Play:
Occupational balance
Disengagement
Partial engagement
Flow
Occupational deprivation (can’t engage due to barriers)
Stigma
Symptoms
Occupational alienation (not allowed to engage)
Takeaway: positive for mental health and mastery over environment
Assessments for Leisure & Play: (just know they exist)
Free time boredom
Leisure attitude measurement
Leisure interest measure
Leisure motivation scale
Leisure satisfaction measure
Activity card sort
Modified interest checklist
Interventions:
Children & adolescents:
Small group activities
Activity analysis
Play based intervention for ADHD
Activity scheduling
Adults:
Social media
Arts & craft
Supported socialization
Adjusting changing interests and abilities
Understanding different terms such as occupational balance, justice, deprivation, etc.
How to run group sessions, lack of participation in groups, types of groups and leadership styles
Leading OT Groups:
Step 1: Introduction
Set tone/ground rules
Introduction & icebreaker
Step 2: Activity
Introduce sessions occupation
State length, target goals, and learning outcomes
Step 3: Sharing
Engagement
OT provides less structure in subsequent sessions
Group members provide feedback (mutual support)
OT models empathy and communication among members
Step 4: Processing
Encouragement to share feelings
Feedback to improve subsequent sessions
Step 5: Generalizing
OT leads in general principles from occupation, sharing, and processing
Therapeutic change
Group members communicate with each other not through OT
Step 6: Application
OT guides in exploring general principles
Focus on here and now and specificity
Step 7: Summary
OT invite group to participate in summarizing session
Focus on lessons learned during sharing, generalization, and application
Types of Groups:
Activity group
Build positive self-concept (improve communication among group members)
Task group
Provide shared work experience
Problem-solving – cognitive skills
Complete task – end goal
Sensory intervention
Pyscho-education group
Mental health education
Community & self-help group
Social group
Develop social skills
Reminiscence group
Preserve memories of past experiences
Fall prevention
Fall safety & catch self
Leisure
Explore leisure activities
Functional
Purposeful actions
Takeaway: client-centered
Everyone must participate
Flexible
Enable and empower clients to target occupations
Leadership Styles:
Democratic (participative): leader builds decision-making process.
Leader = resource person, participates in discussions
Autocratic (authoritarian): leader makes decisions and gives directions (efficiency, structure, and guidance)
Laissez-faire (delegative): leader provides supplies and needed information and leaves group alone.
Types of Research:
• Descriptive research
• Predictive research
• Efficacy research
• Assessment research
• Qualitative research