Test UNO
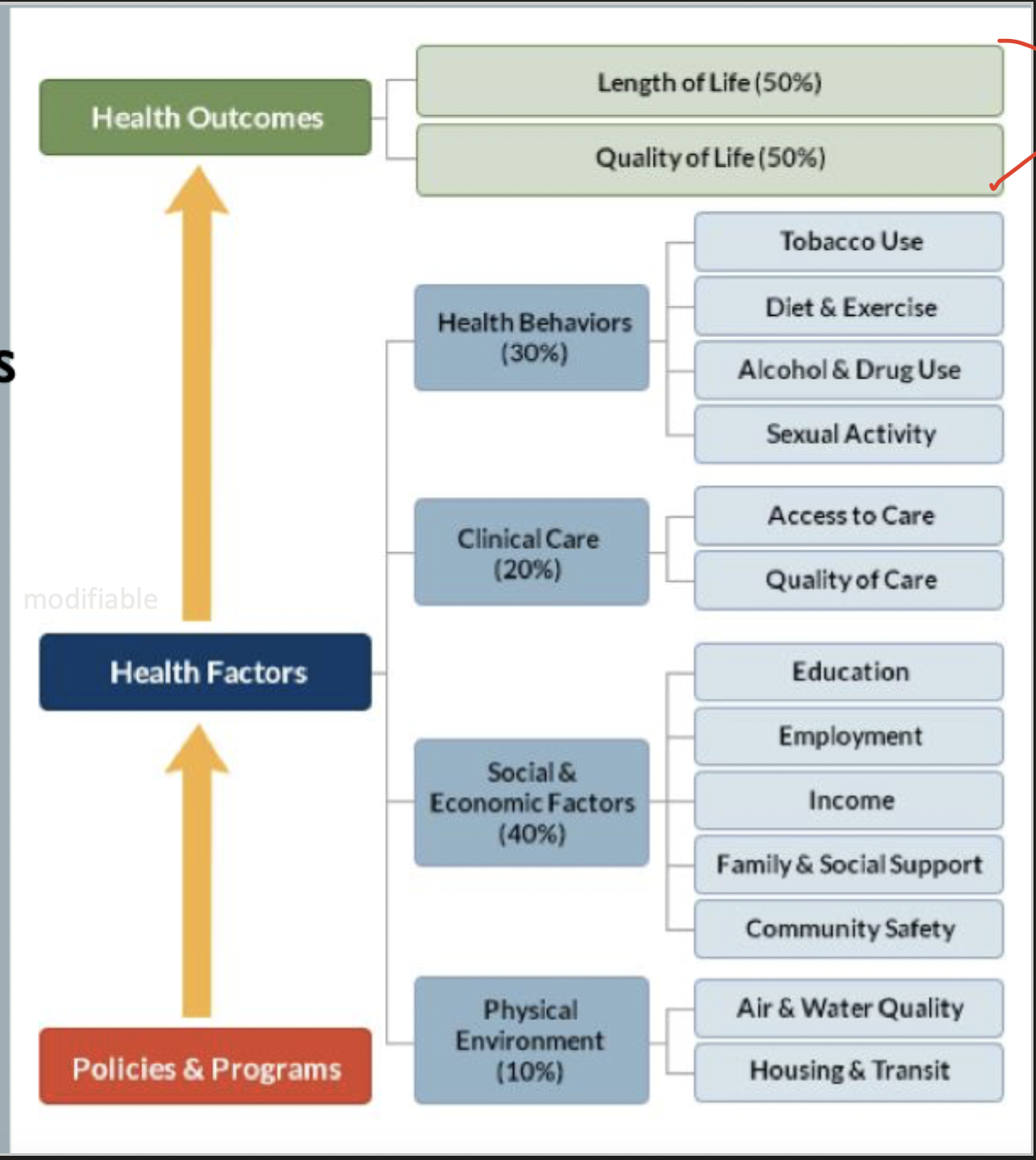
Population Health
Population health is defined as the “Health outcomes for a group of individuals, including the distribution of such outcomes within the group…”
Population health includes things like health outcomes, patterns of social determinants, and polices/interventions that link the two.
Health is determined by interactions between individual, community/groups, physical, social, and political environment
Categories of population health: health improvement, PCP redesign, panel management, population medicine
Importance
US spends 2.5x the OECD average, even when you account for our GDP
What’s the point of learning preventative medicine?
It affect’s patients’ health happens outside the clinical setting, so clinicians need to understand the issues and provide needed resources and support. Health systems are moving towards a population health posture so we must learn to link into patient’s life space and improve public health initiatives .
Learning population health
4 domains of competency: public health, community engagement, critical thinking, and team skills (patient centered care).
3 Levels of competency: foundational awareness (basic), skilled participation (applied), independent practice (proficient)
Wheels of wellness
Organization for Economic Co-Operation and Development (OECD)
Database that includes information on health expenditure, health outcomes, healthcare resources, access to healthcare information, health policies.
Used by policymakers, researchers, and healthcare pros to analyze health systems, compare performance across countries, and inform decision making in health policy
Let’s exercise those critical thinking skills
Basically we are just using data to improve health. Study → act → plan → Do → repeat.
Act: what changes need to be made
Plan: objective, predictions, plan to carry out the cycle, plan for data collection
Do: carry out the plan, document observations, record data
Study: analyze data, compare results to predictions, summarize what we learned
Everybody’s favorite → IPE
Remember that in patient care - the patient is the the CENTER.
Nutrients in a Healthy Diet
Nutrition is the study of food including - how food nourishes our bodies and influences our health. Nutrition contributes to wellness (absence of disease) and is a critical component of physical health along with physical activity. Nutrition plays a role in many diseases such as nutrient deficiencies (scurvy), influences chronic diseases (heart disease), and plays a role in many more.
So what are these nutrients I keep hearing about
Nutrients: the chemicals in food that are critical to human growth and function
Organic nutrients (have a carbon atom) → carbs, lipids, proteins, vitamins
Inorganic nutrients → minerals, water
Macronutrients: required in large amounts (carbs, protein, fats) and provide energy
Micronutrients: nutrients required in smaller amounts (vitamins, minerals)
Kilocalories: amount required to raise the temp of water 1 degree Celsius.
Carbs
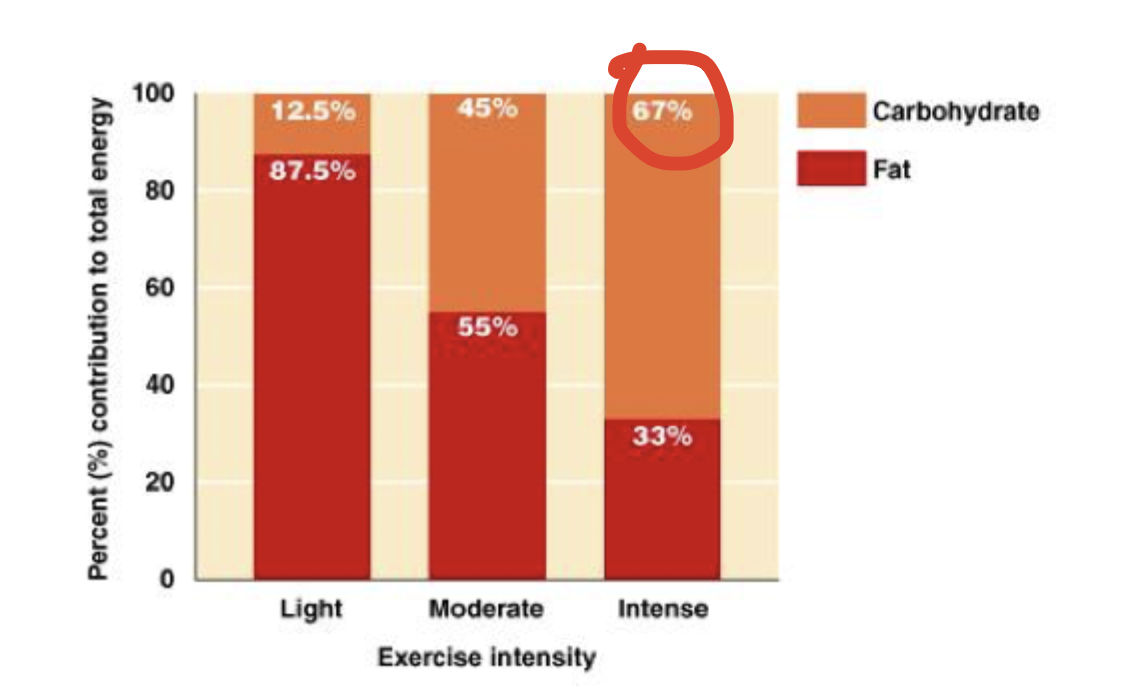
Sole source of energy for the brain and principle source of energy for strenuous physical activity. 4 kcal/g. Found in things like grains, veggies, fruits, and legumes
Fats and Oils → the Lipids
Molecules are insoluble in water. 9 kcal/g. Important energy source during moderate to low intensity exercise. Concentrated in lard, butter, etc.
Proteins
Made up of amino acid chains. 4kcal/g but are not a primary energy source, but are an important source of nitrogen for maintaining and repairing tissues. Concentrated in meats, dairy products, etc.
Proteins are used for building cells/tissues, maintaining bones, repairing damage, regulating metabolism and fluid balance, and participating in immune responses.
Vitamins
Organic molecules that assist in regulating body processes but DO NOT supply energy. Can be water or fat (ADEK) soluble. Only fat soluble vitamins can be store (water soluble ones are excreted by the kidneys).
Minerals
Inorganic substances required for body processes. Include things like iron, sodium, calcium, potassium, and magnesium. Lots of functions such as fluid regulation, bone structure, muscle movement, and nerve functioning.
With the macrominerals (calcium, phosphorus, potassium, sodium, magnesium, and chloride) we need at least 100 mg/day. With the trace minerals (copper, zinc, iron, iodine, fluoride) we need less than that
Water
Critical for health and survival. Necessary for fluid balance, nerve impulses, muscle contractions, nutrient transports, removal of wastes, and chemical reactions.
How are nutrient needs determined?
Dietary reference intakes (DRIs): are updated nutritional standards that expand on traditional RDA values and set standards for nutrients without RDA values
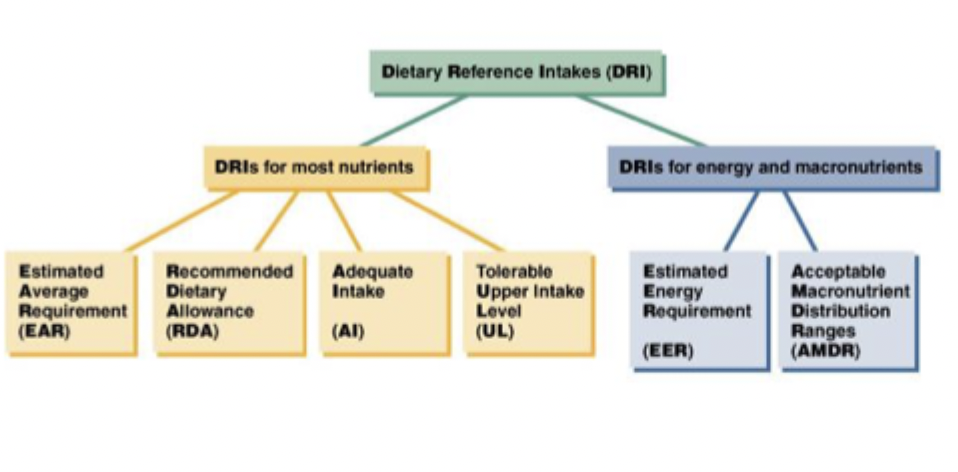
EAR (estimated average requirement): the daily intake of a nutrient that will meet the needs of ½ of the people in a particular category and is used to determine RDA (recommended daily allowance)
RDA (recommended daily allowance): the daily intake required to meet the needs of 97-98% of people in a particular category.
AI (adequate intake): recommended average daily intake level for a nutrient based on experimentation. Used when RDA is not established (calcium, vitamin D, vitamin K, fluoride)
UL (Tolerable upper limit): highest average daily amount that is not likely to have adverse effects and consumption above this level is unsafe.
EER (estimated energy requirement): average dietary energy intake to maintain energy balance - based on age, gender, weight, height, and level of activity.
AMDR (acceptable macronutrient distribution ranges): what portion of energy intake that should come from each macro (carbs 45-65%, fat 20-35%, protein 10-35%).
General Guidance - Healthful Diet
A healthful diet is adequate, moderate, balance, and varied. Adequate meaning we have enough calories, nutrients, fiber, and vitamins. Moderate meaning we are eating the right type of foods to maintain a proper weight. Balanced meaning we have the right combinations to provide the proper balance of nutrition. Variety meaning we eat multiple colors each day.
Designing the Diet
*also includes food guides but he didn’t separate that and dietary guidelines
Nutrition Facts
Nutrition facts panel contain the information required by the FDA and can be used in planning a healthful diet.
Includes serving per container (plan amounts), calories per serving/calories from fat per serving (how much fat does this contain), list of nutrients/food constituents (fat, cholesterol, sodium, carbs, protein, vitamins and minerals), Percent daily values (how much a serving contribute to your total intake of a nutrient)
Dietary Guidelines
Published by the department of health and is general advice for nutrition and health. Gives graphic representations - think Myplate or the food pyramid.
Key food groups: focus on fruits, vegetables, calcium rich foods, make ½ your grains whole, lean with protein, know the limits of sugars, fats, and salts
Diet Plans (not tested apparently)
Fruits and Veggies Matter More: Based on evidence linking cancer prevention and fruits/veggies. Goal is 9 servings a day.
DASH diet: dietary approach to stop hypertension.
Exchange system: Used for diabetics and based on a caloric goal for a certain number of servings - 6 food groups/exchange list. Exchange lists are based on content of calories, carbs, proteins and fat
Carb deep dive
Carbs are a primary energy source, espcially for nerve cells. Carbs are composed for C, H, O - 1 molecule of water per carbon atom. Carbs are made by plants as an end product of photosynthesis.
Simple Carbs STAR
Contain 1 (monosacch) or 2 (Disacch) sugar molecules. Monosaccharides include things like glucose (most abundant), fructose, and galactose. Disaccharides are lactose, maltose, sucrose. Lactose is glucose + galactose. Maltose is 2 glucose. Sucrose is glucose + fructose.
Complex Carbs STAR
Polysaccharides: Long chains of sugar (usually glucose) molecules are usually longer than 10.
Plants produce starch and fiber. Animals produce glycogen, cellulose, and most other fibers.
Starch
Storage form of glucose for plants, includes amylose and amylopectin. Comes from grains, legumes, and tubers.
Glycogen
Animals store glucose as glycogen - produced by the liver and muscles. Not a significant source in the diet.
Fiber
Components of the cell wall and includes carb and non-carb molecules. Cellulose is most abundant. There is soluble and insoluble fibers. Good sources include whole grains, seeds, nuts, legumes, fruits, and veggies.
Digestion of Carbs
Most of digestion is done in the small intestine - pancreatic amylase is doing most of the work (digest glucose polymers to maltose). Other enzymes from the brush border digest disaccharides to monosaccharides - maltase, sucrase, and lactase. Only monosaccharides are absorbed into cells lining the small intestine.
These then get converted to glucose by the liver. Glucose circulates in the blood stream to provide energy, excess is converted to glycogen by the muscles and liver. Once these storage forms run out we switch to gluconeogenesis.
Regulation of Blood Glucose
Regulated by insulin and glucagon. Insulin is produced by the beta cells of the pancreas and promote the transport of glucose into cells as well as stimulating glucose metabolism in the liver. Glucagon is produced by the alpha cells of the pancreas to stimulate the breakdown of glycogen in the liver as well as gluconeogenesis.
Glycemic index is a food’s ability to raise blood sugar - can be influenced by many factors. Meals with low glycemic index may be better for peeps with diabetes, are generally higher in fiber, and may reduce the risk of heart and colon disease.
Role of Carbs
Each gram is 4kcal/g. Along with fats, carbs supply a majority of the energy for daily activities. RBCs rely on glucose ONLY for energy. Brain and nervous tissue like glucose the best but will use other things. Glucose is especially important in intense exercise
If we get enough carbs in the diet, then we can avoid the production of ketones → ketoacidosis → damage to body tissues.
Proteins are often used for gluconeogenesis → therefore carbs are protein sparing
Fiber
May reduce risk of colon cancer, heart disease, enhance weight loss, and prevent hemorrhoids, constipations, and diverticulosis. AI is 14 g/1000 Kcal. Found in whole grains, legumes, nuts, fruits and veggies.
How Much
RDA is 130 g/day → minimum amount to prevent reliance on ketones.
AMDR is 45-65% of daily intake (225-325)
Try to focus on complex carbs versus simple sugars, less than 25% of calories should be from added sugars.
Simple vs. Complex
Diets high in simple sugars may contribute to dental issues, associated with increased levels of LDL and decreased HDL. BUT DO NOT cause hyperactivity or obesity
Whole grain products are a more healthful choice (lower GI, more nutrients and fiber)
Fats deep dive
Fats are the energy yielding subset of lipids (insoluble in water) - not easily digestible
There are 3 types of fats in foods - triglycerides, phospholipids, and sterols
Triglycerides
Composed of 3 fatty acid chains (fatty acids are just chains of carbon) surrounded by hydrogen atoms hooked to a glyceride
Saturated fatty acid: every carbon atom has the max number of H atoms
Monounsaturated: lack H atoms at 1 locations (single C=C)
Polyunsaturated: lack H atoms at multiple spots (multiple C=C)
Phospholipids
Glycerol backbone with 2 fatty acids and a phosphate group. Manufactured in-house and not required in the diet.
Sterols
Lipids containing rings of carbon atoms. Cholesterol is the most common one found in the diet → essential component of cell membranes, hormone synthesis. However, cholesterol can be made in house so it is not essential in the diet.
Digestion of fats
Stomach works to break fat into small droplets, but most digestion and absorption occurs in the small intestine. As fat enters the small intestine, bile is secreted and disperses triglycerides into smaller fat droplets. Pancreatic enzymes break these into 2 free fatty acids and a monoglyceride - micelles are formed and absorbed.
Role of fats
Very energy dense (9kcal/g) and much of energy used at rest comes from fat. Used in light-moderate intensity exercise. Storage form of energy.
Essential for cell membrane structure, nerve cell transmissions, protection of internal organs, and retention of body heat.
Provides flavor and texture to foods and help us feel satiated (take longer to digest and more dense)
Omega 3s!
Vitamins
ADEK require fat for their transport and absorption - especially D and K apparently
How much?
AMDR: 20-35% of calories should come from fat. Active people may need to reduce this to 20-25% so they get more carbs.
Type of fat is also important saturated fats should be no more than 7%. Trans fatty acids should be reduced to the minimum.
Food sources
Visual → things like butter that we knowingly
Invisible → fats hidden within foods, naturally occuring or added in processing
Associations
Associated with CVD → dysfunction of heart/blood vessels → heart attack/stroke
Some fats may protect from CVD.
Risk factors include: overweight, physical inactivity, smoking HTN, diabetes, diets high in saturated and trans fat.
Protein deep dive
Proteins are large molecules comprised of amino acids - amino acids contain C, H, O, N. Proteins are the primary source of N in our diets.
Proteins’ functions → cell growth/repair/maintenance, builds muscle, hormones, fluid and electrolyte balance, pH balance, antibodies to protect against disease, and low grade energy source
Amino Acids
There are 20 amino acids - 9 are essential and must be eaten; the other 11 can be made by our bodies (nonessential)
In the diet
A complete protein has all 9 essential amino acids in sufficient amounts (high quality). Incomplete protein does NOT contain all the essential amino acids. Complementary food like beans, rice, peanut butter, and whole bread can fill in the gaps.
Digestion
Begins in the stomach with the denaturing by HCL (HCL also activated pepsin). Pepsin is an enzyme that breaks down proteins into short polypeptides and amino acids.
Continues in the small intestine → pancreatic proteases digest proteins into tripeptides, dipeptides, and amino acids. Mucosal cells release amino acids into the blood stream. (Less digestible proteins are of lower nutritional value)
How Much
Depends on body weight, activity, age, and health status. Children, adolescents, pregnant/lactating women, vegetarians, and athletes should eat more
RDA: 0.8 g/kg (12-20% of daily intake)
Risks of TOO much
High cholesterol and heart disease → animal sources are often high in saturated fat
Bone loss → increases calcium excretion
Kidney Disease → in susceptible people
Not Enough Protein STAR
Protein-energy malnutrition: a disorder caused by inadequate intake of protein and energy
Marasmus: severely inadequate intakes of protein, energy, and other nutrients resulting in severe wasting of muscle, stunted growth, stunted brain development, and anemia.
Kwashiorkor: severely low protein intake resulting in weight loss, muscle wasting, edema (distention of the belly), retarder growth and development. (often seen in developing countries)
Bone Health
Bones have a unique tissue structure → provide support to the body but also. flexibility. Hardness of bones is provided by minerals (65%). Flexibility, durability, and strength is maintained by organic substances like collagen (35%)
Cortical bone: compact bone, very dense tissues, 80% of skeleton
Trabecular bone: spongy bone, scaffolding inside that supports cortical bone, 20% of skeleton
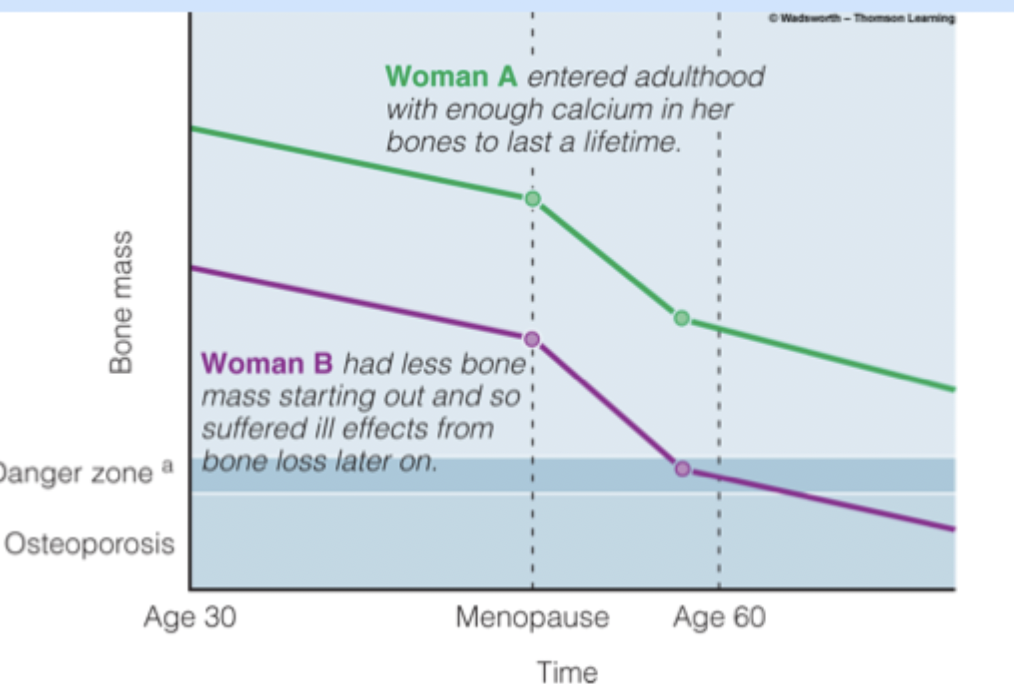
Phases of development
Bone growth: increase length → usually finished by 14 in girls and 17 in boys
Bone modeling: shaping of bone, finishes by early adulthood (increased thickness)
Bone remodeling: recycling of bone, occurs in adulthood. Involves resorption (osteoclast) and formation of new bone (osteoblast)
Peak bone density occurs by age 30, remodeling maintains this over the next decades. Bone density decreases after age 40 because clasts > blasts.
Calcium
The most abundant mineral in the body (99% is stored in the bones). Functions include maintaining bones/teeth, acid-base balance assistance, transmission of nerve impulses, and assist in muscle contraction.
NO RDA - AI recommends 1000-1300 mg/day. Sources include milk, cheese, yogurt, leafy greens
Bone remodeling is critical in maintaining calcium levels
Vitamin D
Fat soluble vitamin that is stored in the liver and fat tissue. Can be made by the body with exposure to sunlight - hormone like activity.
Functions: regulate blood calcium (promotes absorption and regulates movement in/out of bone)
Sources: very little in foods (unless fortified dairy), the sun, supplements, fortified soy
Vitamin K
Fat soluble and stored in the liver. Phylloquinone is the plant form. Menaquinone is the form produced by the bacteria of the large intestine. Functions include blood coagulation and bone metabolism.
AI values 120 mg/day for men, 90 for women. Sources include leafy greens and vegetable oils
Phosphorus
Primary negatively charged intracellular electrolyte. Functions include mineral composition of bone, fluid balance, and ATP, DNA and membrane components.
Magnesium
50-60% of the body’s mag is in the bones. Functions as a co-factor for tons of enzymes, muscle contraction and blood clotting, supports vitamin D metabolism, makes up mineral crystals in the structure of bone.
RDA 310 mg/day for women, 400 for men. Sources include leafy greens, whole grains, seeds, nut, seafood, beans, dairy
Osteoporosis
Characterized by low bone mass, deterioration of bone tissues, fragile bones leading to bone fractures, compaction of bones (decreased height), shortening and hunching of the spine
Prevention measures: vitamin D, calcium, weight bearing exercise, walking, build up bone levels early in life
Blood health
Reminder - vitamins and minerals do not directly provide energy but are necessary to obtain energy from the macronutrient.
Many minerals act as coezymes, while minerals function as cofactors. A enzyme speeds up a chemical reaction. Coenzymes combine with enzymes to facilitate requires coenzyme.
B Complex Vitamins → Know deficiencies
Important for mineral metabolism - includes thiamin, folate, riboflavin, niacin, B6, B12, panthothenic acid
Thiamin B1
Coenzyme needed for glucose metabolism, metabolism of branched amino acids, production of DNA, RNA, and neurotransmitters.
Source: enriched grain, whole grains, and pork
Deficiencies result in: Beriberi (muscle wasting and nerve damage)
Riboflavin B2
Coenzyme for oxi-reduction reactions and a component of antioxidant enzyme system.
Source: milk
Deficiencies result in: Ariboflavinosis (sore throat, swollen mucous membranes, irritated patches of skin)
Niacin (Nicatinamide and Nicotinic acid)
Coenzyme assisting with metabolism of carbs and fatty acids
Source: meat, fish, poultry, enriched grains - toxicity can result from supplements
Deficiencies result in: Pellagra
Pyridoxine B6
A group of 6 related compounds that act as coenzymes in amino acid metabolism. Also play a role in carb metabolism and Hgb synthesis.
Sources: enriched cereals, meat, fish, poultry, starchy veggies
Toxicity can result in nerve damage and skin lesions
Folate
Involved in DNA synthesis, amino acid metabolism, and cell division of early embryos
Source: leafy greens, legumes, ready-to-eat cereals, enriched bread products
Deficiency can result in anemia and neural tube defects
High levels mask B12 deficiency
Cobalamin B12
Coenzyme associated with blood formation, required for nerve functioning, and metabolism of homocysteine.
Source: animal based foods
Deficiency results in pernicious anemia, long term results in irreversible damage to the nervous system
Pantothenic Acid
Coenzyme for fatty acid metabolism - required for building new fatty acid.
Sources: chicken, beef, egg yolks, potatoes, oat cereals, tomato products
No toxicities and deficiencies are rare
Biotin
Coenzyme involved in metabolism of carb, fat, and protein - important in gluconeogenesis.
Deficiencies are rare → symptoms include hair thinning, loss of hair color, red rash on face
Iodine
Trace mineral that is critical the synthesis of thyroid hormones which regulate body temperature and resting metabolic rate.
Source: saltwater fish, shrimp, iodized salt, milk, dairy products
Deficiencies result in: hypothyroidism, goiter, cretinism (iodine deficiency during embryonic development)
Excess iodine occurs from supplement - blocks synthesis of thyroid hormones
Chromium
Trace mineral necessary for proper functioning of insulin
Source: mushrooms, prunes, dark chocolate, nuts, whole grain
Deficiency: inhibits glucose absorption and/or utilization
Manganese
Trace mineral that acts for a cofactor involved in energy metabolism and is part an antioxidant enzyme system
Source: whole-grain foods, brown rice, pineapple, pine nuts, okra, spinach
Toxicity impairs the nervous system (spasms and tremors)
Blood
The only fluid tissue in the body that functions to transport of oxygen and nutrient to cells and removal of wastes from tissues.
Components - STAR
Erythrocytes: RBCs for transporting oxygen through the body
Leukocytes: WBCs of the immune system
Platelets: cell fragments that assist in blood clotting
Plasma: the fluid portion of the blood
Vitamin K - star
Fat soluble is a coenzyme for the synthesis of proteins involved in blood clotting (easy bruising, oozing, excessive bleeding- can be a sign of clotting issues). Can be produced by intestinal bacteria,
Source: leafy greens vegetable oils
Deficiencies can result from diseases that disturb absorption of fats
Iron
A trace mineral that functions as a component of the protein Hgb which carries oxygen in erythrocytes, a component of myoglobin which carries O2 in muscle cells, and a cofactor involved in energy metabolism of carb, fats, and proteins.
Excess iron is stored in the body bound to the proteins ferritin or homosiderin (usually in the liver, bone marrow, intestinal mucosa, and spleen)
Heme iron is only found in animal foods (more absorbable)
Non-heme iron found in plants (less absorbable)
RDA varies on age and gender 8 mg/day for men; 27 mg/day for pregnant women
Iron OD is the most common cause of poisoning death for children under 6. Toxicity symptoms include N/V/D, dizziness, and confusion. Delayed treatment of iron toxicity can result in severe damage to heart, kidneys, liver, and CNS.
Iron deficiency is the most common nutrient deficiency worldwide. High risk peeps include infants, young children, preadolescent girls, premenopausal women, and pregnant women
Zinc
Zinc is a trace mineral needed for Hgb production, antioxidant enzyme system, development and function of the immune system, and cell replication/normal growth.
RDA is 8mg/day for females, 11 for males
Sources: red meats, seafood, whole grains, enriched grains and cereals
Too much → intestinal pain, cramps, nausea, vomiting, loss of appetite, can impair copper status
Too little → growth retardation, diarrhea, delayed sexual maturation
Copper
A trace mineral required as a cofactor for energy metabolism, collagen production, antioxidant enzyme system, and iron transport.
RDA 900 mg/day
Source: organ meats, seafood, nuts, seeds, whole grains
Too much → Wilson’s disease (intestinal pains, cramps, nausea, vomiting, liver damage)
Too little → RARE (anemia, WBCs are decreased, osteoporosis in children)
Deficiency Deep Dive
Neural tube defect
Folate need is increased in pregnancy. Folate is required for cell division and proper formation of the neural tube (brain and spinal cord). All pregnant women need 400 µg/day.
Vascular disease
Folate and B12 are required for the metabolism of homocysteine. High levels are associated with CVD and cerebrovascular disease.
Anemia → star
Just anything with low Hgb
Iron-deficiency: late stage results in small pale RBCs that do not have enough Hgb, symptoms include fatigue, pale skin, impaired work performance, depressed immune function, impaired memory
Pernicious: Macrocytic anemia as a result of a lack of intrinsic factor
Macrocytic: Deficiency of folic acid (often secondary to B12 deficiency) resulting in large RBCs. Symptoms include weakness, SOB, fatigue, difficulty concentrating, irritability, HA. Can be prevented by increasing folate intake
Electrolytes
Reminder: 50-70% of a healthy adults body is composed of fluids. Body composition varies by tissue type, gender, and age.
Body fluid is composed of water and electrolytes. Sodium and potassium are positively charged. Chloride and phosphorus are negatively charged.
Function of Fluid
Blood volume → amount of fluid in the blood, can affect bo
Can help maintain body temp (water has a high heat capacity, sweating releases heat)
Protects and lubricates → CSF (brain and spinal cord), amniotic fluid (fetus), synovial fluid (joints), digestive secretions allow for easy passage
Functions of Electrolytes
Regulate fluid balance (osmosis)
Help nerves respond to stimuli (movement of K and Na lead to action potentials)
Signal muscle contraction (Ca2+)
Water
Functions: essential for life, major component of body fluids
RDA 1.0-1.5 ml/kcal expended (varies based on environment, health status, and activity level)
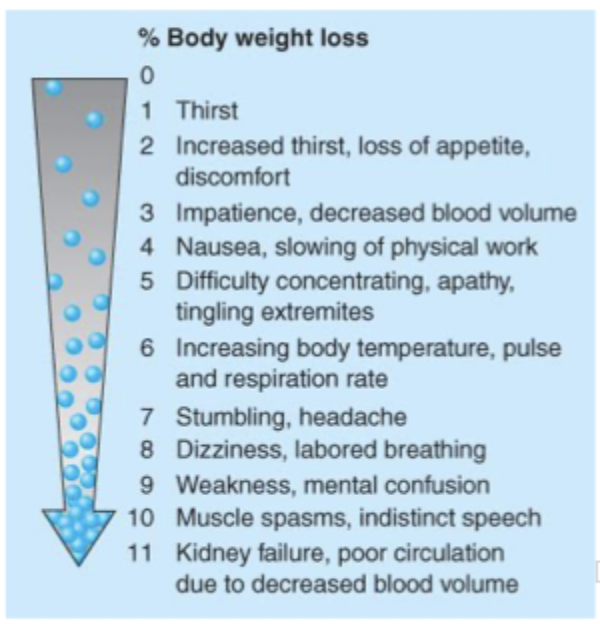
Dehydration
Water is lost through: urine, sweat, exhalation, feces (urine is usually the most)
Water is gained through: beverages, food, metabolic
Hyperhydration (water intoxication)
Rare but can occur under conditions like kidney disease or overconsumption of water. Can result in dilutional hyponatremia.
Sodium
Functions: fluid/electrolyte balance, maintain bp and acid-base balance, nerve impulse transmission, aids in muscle contraction, assist in transport of glucose into the cells
RDA: 500-2400 mg/day
Sources: naturally occurring, typically higher in processed foods
Too much → raises bp, increase excretion of Ca, hypernatremia (usually secondary to CHF or cirrhosis), excessive blood volume, edema, malignant HTN
Too little → hyponatremia can result from prolonged diarrhea/vomiting or excessive sweating or overconsumption of water. (HA, dizziness, fatigue, nausea, vomitting, muscle cramps)
Potassium
Functions: fluid/electrolyte balance, muscle contraction, transmission of impulses, helps maintain a lower bp
RDA: 2,000 mg/day
Sources: fresh fruit/veggies, whole grains, dairy
Too much → hyperkalemia (CKD) can lead to peaked T waves and heart attack
Too little → hypokalemia (secondary to kidney disease or DKA; triggered by dehydration, excessive vomiting or diarrhea or medications) can lead to an abnormal heart rhythm
Chloride
Function: fluid/electrolyte balance, HCl in the stomach, immune system, transmission of nerve impulses
RDA: 750 mg/day (no upper limit)
Too much → HTN
Too little → rare usually due to dehydration or frequent vomiting
Phosphorus
Functions: major intracellular anion, fluid/electrolyte balance, mineral component of bone, regulates biochemical pathways by activating/deactivating enzymes, found in ATP/DNA/RNA/phospholipids
RDA: 700 mg/day, no more than 4000
Sources: anything with protein
Too much → usually as a result of CKD, vitamin D supplements, antacids; may cause spasms and convulsions
Too little → Rare (premature infants, elderly, alcoholics are at risk) but can result from vitamin D deficiency, hyperparathyroidism, overuse of antacids
Nutrition throughout Life
Pregnancy
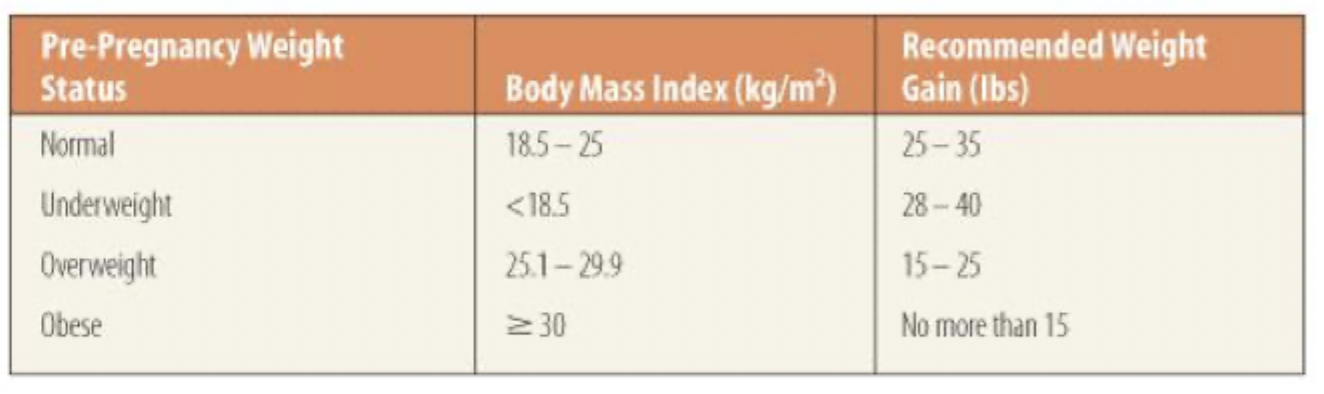
Undernourished mother is more likely to give birth to to a low-birth weight baby (less than 5.5 lbs). Low birth weight babies are at increased risk of infection, learning disabilities, impaired physical development, and death in the 1st year. Preterm babies (before 38 weeks) and may be low-birth weight.
Too much weight gain is also risky and women should not diet during pregnancy since this may deprive the fetus of critical nutrients.
LOOK AT WEIGHT GAIN - LOCK IT IN
1st trimester
Zygote (fertilized egg) travel through the fallopian tubes and implants in the wall of the uterus. We develop organs, limb buds, facial features, etc. Embryos are extremely vulnerable.
2nd trimester
Organ systems continue to develop. Growth from 3 inches to over a foot long by the end of the first trimester
3rd trimester
This is a time of considerable growth. Fetus gains 75% of weight during this time. Extensive brain growth. Lungs mature.
Dietary changes
Women need to increase macronutrients, micronutrients, and fluids.
They need 300 extra calories during the 2nd and 3rd trimester. 60 g/day of protein. 130 g/day of carbs. Calories from fat should not change, limit saturated fats and avoid trans fats. Newborns need fat for temperature regulation and energy source
Micronutrients like folate, B12, Vitamins CAD, calcium, iron, zinc, sodium, and iodine are critical.
Fluids need to increase to 3L/day (pound’em) → increase in the mother’s blood volume, regulate body temp, production of amniotic fluid, combat fluid retention and constipations, and prevents UTI (no sepsis in this house)
Nutrition Concerns
Adolescent Pregnancy: higher than that of adult women (adolescents are still growing) and are more likely to have preterm babies and low-birth weight babies
Vegetariansim: Watch intake of D, B6, B12, calcium, iron, and zinc
Diet: Trying to lose weight during pregnancy is not advisable (calorie restriction is stupid, you're eating for two).
Caffeine: Crosses the placenta. 1-2 cups of coffee is chill but anything greater than that may lead to increase risk of miscarriage and low birth weight.
Exercise: helps keep women physically fit, solid mood booster, helps compensate for increased appetite, helps keep bp down, easier to lose weight after the pregnancy
Infant nutrition
Optimal nutrition during the 1st year is critical because organs are developing, nervous system continues to develop, and babies grow 10 inches and weight 3x.
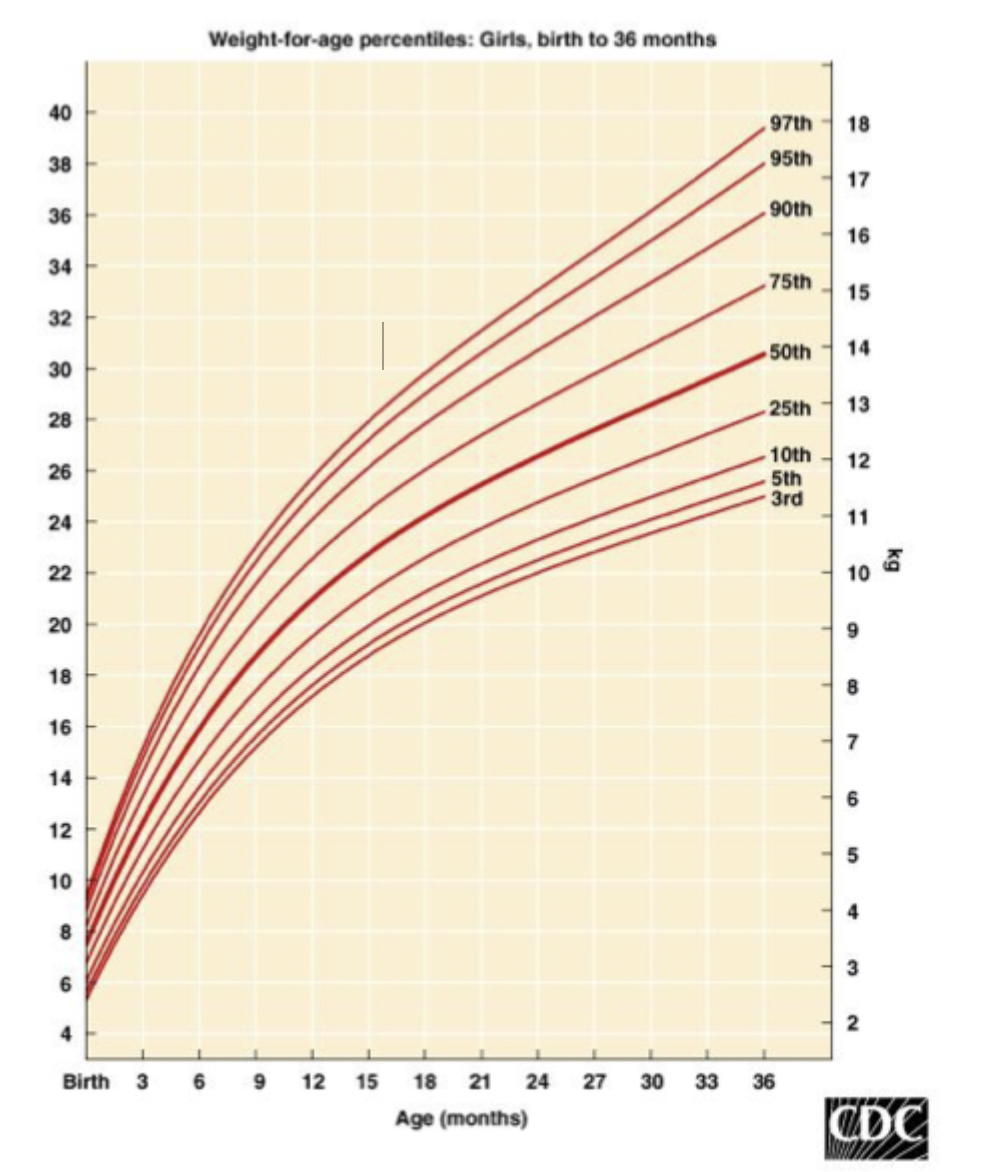
Nutritional needs are unique at this time because energy needs are high, digestive tracts and kidneys are still immature, and babies are small.
Recommendations: 50 cal/lb/day, 40% from fat, no more than 20% from protein, 2 oz/lb
WHO recommends breastfeeding for the 1st 2 years, supplement with solid food at 4-6 months
Toddlers (1-3)
Rapid growth begins to slow, gains 5.5-7.5 inches and 9-11 pounds. Higher energy expended for increased activity level.
EER: kcal/day = (89 x weight (kg) -100)+20
30-40% from fat
1.1 g of protein per kg
130 g of carbs/day
14 g of fiber per 1000
For the micronutrients, ensure adequate intake of A, B, E, calcium, iron (most common nutrient deficiency), zinc
Food choices
If you provide nutritious foods, a toddler will eat them - you don’t have to bribe them
Preschoolers
Overweight = BMI in 85th percentile
Obesity = BMI in 95th percentile
Macros
Total fat intake should mimic that of an adult. 25-35% of total energy should be from fat.
0.95 g/kg for protein
130 g/day for carbs
14 g of fiber per 1000 cal
Micro
Increase amounts of calcium, iron, and zinc
School aged (6-13)
Growth is slow and steady (2-3 inches per year), activity levels vary.
Nutrition can be influenced by peer-pressure attempt to help patients find healthy role models
Obesity - now an epidemic in the US, too much food without enough physical activity (1 hour a day is recommended)
Body image and appearance becomes important
Macronutrients
25-35% of total energy from fat
0.95 g/kg of protein
130 g of carbs, 45-60% of calories from carbs
14 g of fiber per 1000 calories
Micronutrients
Increases through age 8, needs rise sharply as puberty approaches. Ca and Fe are hella important.
Adolescents
Growth spurts occur at 10-11 for girls, 12-13 for boys. 20-25% increase is expected. Weight and body composition also change.
Physical activity is important. Disordered eating can begin around this time and drug use can also affect nutrition.
Macros
25-35% from fat
45-60% from carbs
0.85 g protein/kg
26 g/day fiber
Micros
Calcium must be sufficient for achieving peak bone density. Iron needs are high. Vitamin A is needed for rapid growth and development.
Young-Middle age adults
Concerns include maintenance of health, eating a balanced diet, staying physically active, reducing the risks of chronic disease
Older adults 65+
Changes to the body: decreased muscle mass and lean tissue, increased fat mass, decreased bone density, decreased immune function, impaired absorption of nutrients.
Chronic diseases are more prevalent in overweight or obese adults. Osteoarthritis is more symptomatic with increased weight → 3-6 lbs on the body, puts 14 lbs of pressure on the joints.
Being underweight may result from illness, disability, loss of smell/taste, depression, or social isolation. CANCER RED FLAG. Dental issues may lead to the avoidance of meats and other firm foods.
Note: some medications may alter nutrient absorption profile
A balanced diet with ample folate and B12 may decrease risk of dementia and improve memory
Macros
Energy needs usually decrease, same recommendations as young-middle adults but just less fiber. Calorie is needed for additional lean muscle mass HOWEVER
Micros
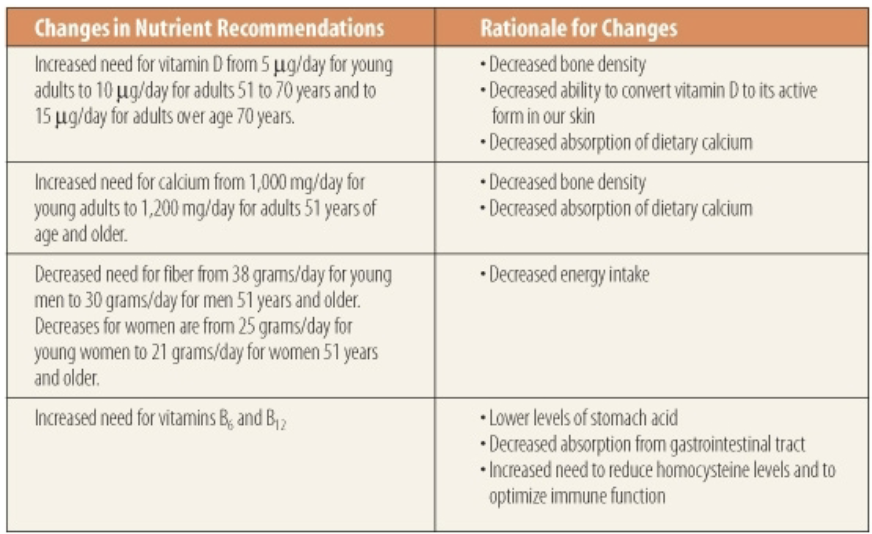
Calcium and vitamin D increase. Iron needs decrease. Zinc must be maintained. Adequate intake of B12 is a special concern.