Prenatal Development and Birth - Vocabulary Flashcards
Prenatal Development and Birth – Comprehensive Study Notes
Overview: This content covers prenatal development from conception to birth, including the three main periods (zygotic, embryonic, fetal), key structures (amnion, chorion, yolk sac, placenta, umbilical cord), milestones, potential risks (teratogens), maternal factors, birth processes, and early postnatal considerations.
Phases of Prenatal Development
Phases and timeframes:
Period of the zygote: conception through implantation (10-14 \text{days}).
Period of the embryo: weeks 3-8, major organ formation, heart begins beating.
Period of the fetus: 9^{{th}} week through birth.
The Period of the Zygote
Key events and structures:
Blastocyst: 60-80 \text{cells}.
Inner cell mass becomes the embryo; outer layer forms protective/nourishing tissues.
Implantation: 7-10 \text{days} after conception; embryo taps into the mother’s blood supply through the uterine wall.
Implantation success rate: about 25\%.
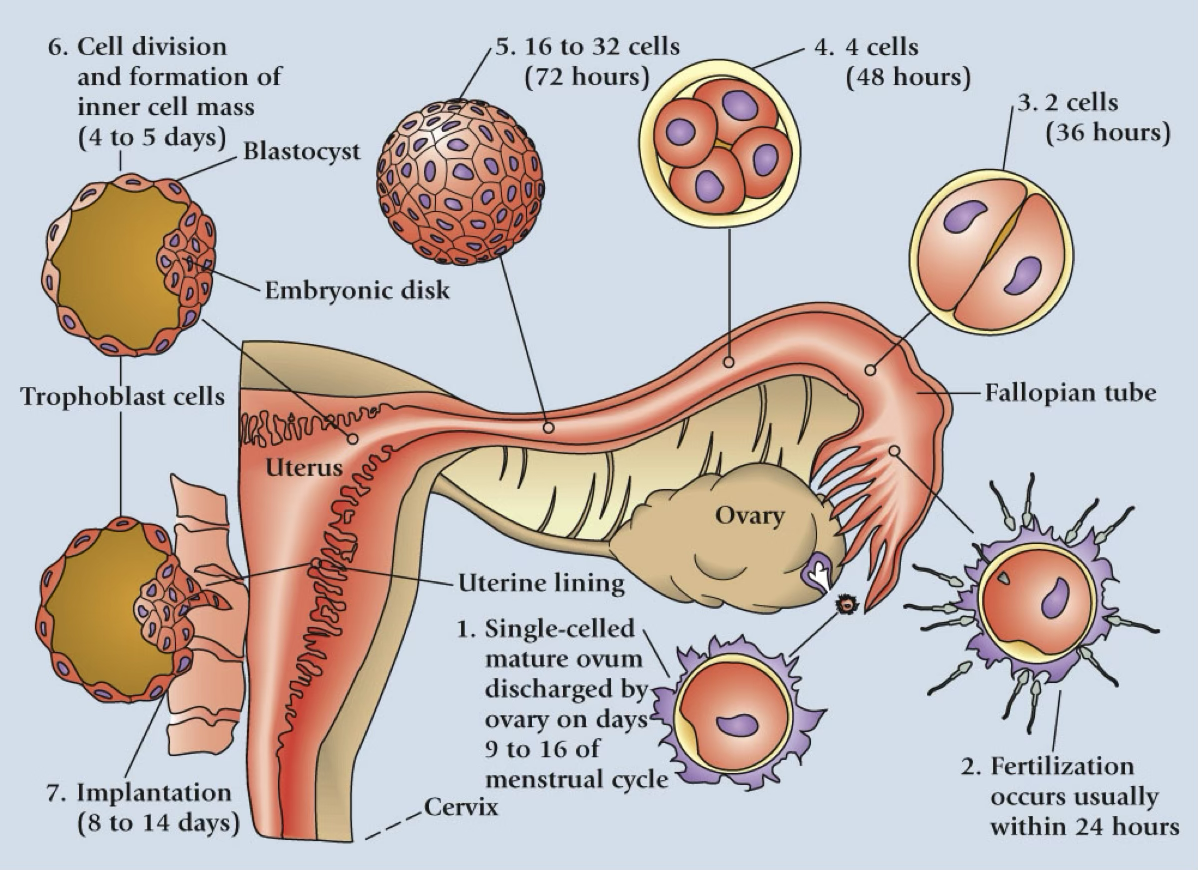
Stage-by-stage progression (from a visual sequence):
1. Single-celled mature ovum released by the ovary on days 9-16 of the menstrual cycle.
2. Fertilization typically occurs within 24 \text{hours}.
3. 3.2 cells (3.2 \text{cells}) at 36 \text{hours}.
4. 4 cells (4 \text{cells}) at 48 \text{hours}.
5. 16 to 32 cells (72 \text{hours}).
6. Blastocyst forms and implants (8-14 \text{days}).
Protective/nourishing/structural components (during the zygote period):
Amnion: watertight sac with amniotic fluid; cushions; temperature regulation; supports a weightless environment for movement.
Yolk sac: early blood cell production.
Chorion: becomes lining of the placenta.
Placenta (structure and function):
Purpose: semipermeable membrane enabling passing of nutrients and gases.
Limitation: blood cells are too large to pass through.
Site of all metabolic transactions sustaining the embryo happen through the placenta
The Period of the Embryo
Germ layer differentiation (by the third week):
Ectoderm (outer layer): nervous system; skin; hair.
Mesoderm (middle layer): muscles; bones; circulatory system.
Endoderm (inner layer): digestive system; lungs; urinary tract; vital organs (e.g., pancreas, liver).
Early developmental milestones:
Week 3: neural tube forms.
Week 4: heart begins beating.
Week 7: rudimentary skeleton appears.
Weeks 7-8: sexual development begins; if male, Y chromosome triggers testes development; otherwise ovaries form.
The Period of the Fetus
General pattern: last 7 months of pregnancy; rapid growth; refinement and maturation of organ systems; major systems begin functioning.
Growth milestones and organ maturation (overview):
Third month: organ systems continue rapid growth and interconnection; nervous and muscular coordination allows some movement (not felt by mother yet); digestive/excretory systems functioning; reproductive system contains immature ova or sperm.
Fourth to sixth months: sucking, swallowing, breathing; movements felt by mother; heartbeat detectable by stethoscope; sweat glands functioning; vernix protects skin; lanugo helps vernix adhere to skin; visual and auditory senses become functional.
Seventh to ninth months: rapid maturation of all organ systems in preparation for birth; age of viability ~ 22-28 weeks; weight around 4 \text{pounds} by end of the seventh month; activity slows and sleep increases as birth nears.
Specific prenatal development table (Table 4.1) – brief overview by trimester:
First Trimester:
Zygote (weeks 1): one-celled zygote; division leads to blastocyst.
Embryo (weeks 3-4): size about 1/4 \text{inch}.
Embryo (weeks 5-8): about 1 \text{inch}; weight 1/4 \text{oz}.
Second Trimester:
Fetus (weeks 13-24): about 3 \text{inches}; weight 1 \text{oz}; organ systems form; brain/spinal cord/heart form; rudimentary senses form.
Third Trimester:
Fetus (weeks 25-38): growth to 19-21 \text{inches}; weight around 7-8 \text{lb}; rapid maturation of organ systems; fetus reaches viability; sleep and motor patterns become more regular.
Additional notes on fetal growth: visual and external body structures form; external genitalia differentiate; fetal movements begin and are felt later in pregnancy; vernix covers the fetus and aids protection; layer of fat develops under skin near term.
Potential Problems in Prenatal Development
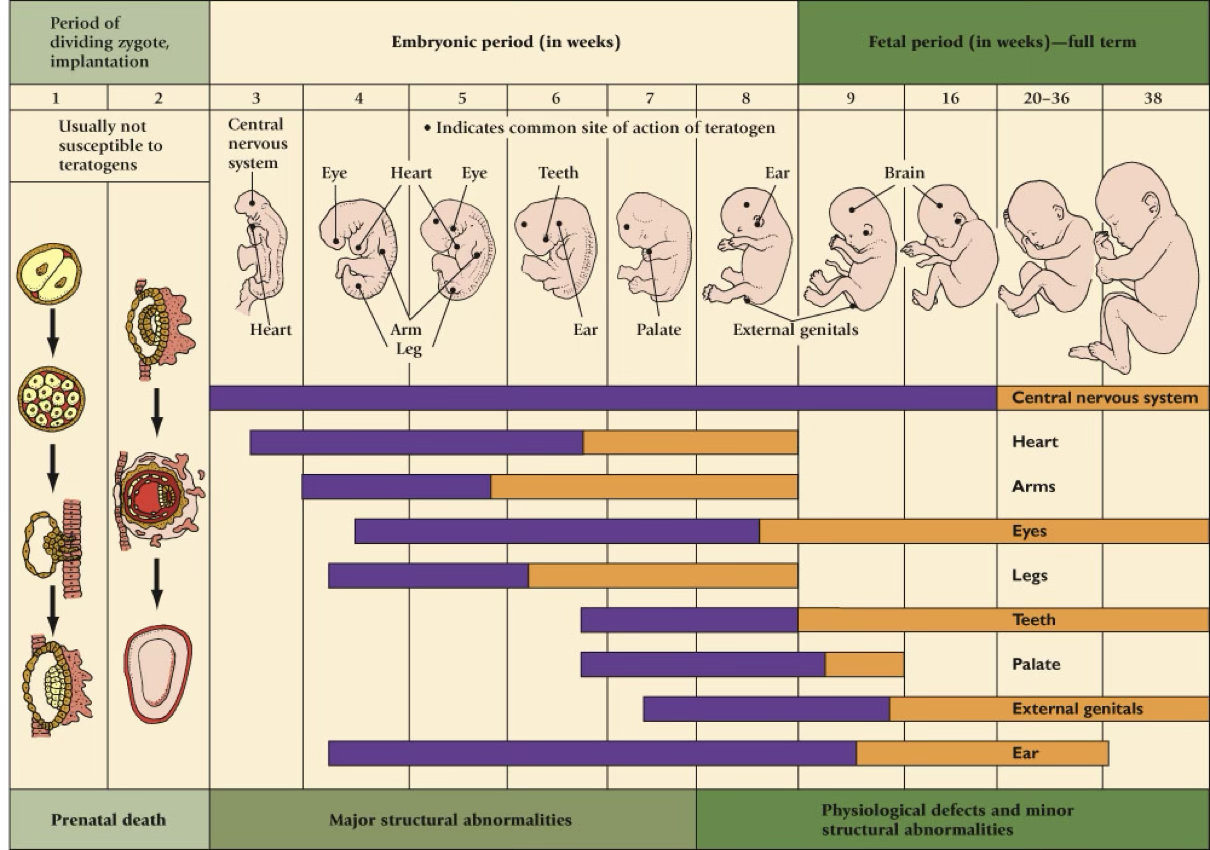
Teratogen: any agent that can harm an embryo or fetus.
General teratogen effects:
Most serious during organ formation (sensitive periods).
Susceptibility is influenced by genetic makeup of mother and embryo.
One teratogen can produce different defects; different teratogens can produce the same defect.
Longer exposure/higher dose increases harm; paternal exposure may affect the embryo; long-term effects depend on postnatal environment; some effects may be latent (apparent later in life).
Critical periods (illustrated in Figure 4.5): each organ/structure has a window of maximum sensitivity to teratogens; sensitivity bands indicate varying levels of susceptibility.
Specific teratogenic diseases and agents:
Rubella (German measles): can cause blindness, deafness, cardiac abnormalities, mental retardation; most dangerous in first trimester; vaccination or prior immunity recommended before conception.
Toxoplasmosis: parasite from animals; risk with undercooked meat or cat feces; can cause eye/brain damage in first trimester or miscarriage later.
Sexually transmitted diseases (STDs):
Syphilis: fetal damage if untreated; early treatment prevents harm (risk if untreated); can cause eye, ear, bone, heart, brain damage; miscarriage. Not be transmitted until the 18th week.
Genital herpes: can cross placenta; most infections occur at birth; high risk (33%) of neonatal death and neurological damage; cesarean delivery advised if mother has active herpes.
AIDS (HIV): placenta, birth, or breast milk transmission; antiviral ZDV reduces transmission by about 70\%; about half of HIV-infected infants survive past age 6.
Drugs:
Thalidomide: once used for nausea/vomiting; caused birth defects (eye, ear, heart, limb malformations) if taken in first two months; phocomelia observed in limbs.
Aspirin, Ibuprofen, Caffeine, Lithium, Oral contraceptives, DES: various fetal risks (growth retardation, heart defects, etc.).
Diethylstilbestrol (DES): synthetic estrogen; prescribed 1940-1971; fell out of use after later findings.
Alcohol: placental function compromised; Fetal Alcohol Syndrome (FAS) includes microcephaly, congenital heart/limb/joint/face malformations, hyperactivity, seizures, tremor, lower IQ, and long-term adjustment problems. Fetal Alcohol Effects (FAE) associated with social drinking or bingeing; father’s drinking may also affect outcomes.
Cigarette smoking: increased risk of cleft lip, abnormal lung function, hypertension, miscarriage, low birth weight, ectopic pregnancy, SIDS; nicotine and carbon monoxide impair placental gas/nutrient exchange; long-term effects include smaller size, susceptibility to respiratory infections, slightly poorer cognitive performance, and potential behavioral issues.
Marijuana: associations with emotional regulation issues in males and poorer reading/spelling at age 10; higher risks of depression/anxiety.
Narcotics (heroin, methadone): high likelihood of neonatal addiction (60-80%); early breathing/swallowing coordination problems; many progress to normal development by age 2, though boys may be more vulnerable.
Cocaine: increased risk of miscarriage, prematurity, sleep disturbances, irritability, lower IQ, language development delays; effects can be compounded by maternal vocabulary and home environment.
Environmental hazards: radiation can cause death or mental retardation; avoid X-rays unless necessary; chemicals/pollutants (lead, zinc, mercury) impair physical/mental development; PCBs in plastics can lead to smaller birth weight, reduced responsiveness, and cognitive difficulties when exposure prenatally or via breastfeeding (Figure 4.6).
Table 4.3 (partial) lists various drugs/treatments used by mothers that affect the fetus: sources include Chavkin, Chomitz, Friedman & Polifka, Kelley-Buchanan.
Maternal characteristics and exposures:
Diet: total weight gain around 25-35 \text{pounds}; malnutrition in 1st trimester linked to miscarriage/spinal cord issues; malnutrition in 3rd trimester linked to low birth weight and small heads; supplements and stimulation can mitigate prenatal malnutrition effects.
Magnesium & Zinc supplementation improves placental function and reduces certain birth complications.
Folic acid (B-complex in leafy greens, beans, liver, tuna) reduces risk of Down syndrome, spina bifida, anencephaly, and other neural tube defects; folic acid enrichment is especially critical during the first 8 \text{weeks}; excessive supplementation can be harmful; medical supervision advised.
Emotional well-being: temporary stress has minimal harm; prolonged/severe stress linked to stunted prenatal growth, premature delivery, irritability, irregular feeding/sleeping; stress hormones can reduce oxygen/nutrients to fetus and weaken the immune system; counseling to manage stress can be beneficial; moderate stress may aid development.
Maternal age: optimal range 16-35; younger than 15 often associated with impoverished backgrounds and higher risk, but prenatal care can mitigate; older than 35: higher risk of miscarriage due to chromosomal abnormalities; good prenatal care does not completely eliminate risk; most older mothers have healthy babies if well-nourished.
Prevention of Birth Defects
General outlook: about 95\% of newborns are normal; the remaining 5\% may have minor or correctable congenital issues.
Factors influencing congenital disorders:
Genetic makeup of parents and prenatal environment.
Table 4.4 (Reductions in risk): genetic counseling if hereditary concerns; ideal childbearing age 16-35; high-quality prenatal care in a modern hospital; rubella immunity; STD testing; avoid toxoplasmosis (undercooked meat, cat feces); avoid nonessential drugs; minimize radiation exposure; avoid smoking; nourishing diet with adequate protein/vitamins/minerals/calories.
Birth and the Perinatal Environment:
Perinatal environment includes medications given to the mother during delivery, delivery practices, and the social environment after birth.
The Birth Process and Perinatal Experience
The birth process stages:
First stage of labor: contractions begin, typically 10-15 minutes apart; ends when the cervix is fully dilated.
Second stage of labor: delivery; the baby’s head passes through the cervix into the vagina; ends when the baby is born.
Third stage of labor: afterbirth; placenta expelled from the mother.
Visual depiction (Fig. 4.9) shows the uterus, cervix dilation, birth canal, baby’s head crowning, and placenta expulsion during the three stages.
The baby’s experience during birth:
Stressful but helps with air movement and breathing after birth.
Typical appearance: around 20 \text{inches} long, 7-7.5 \text{pounds}; bluish and somewhat misshapen at birth.
Apgar test used to assess newborn status: checks Heart rate, Respiratory effort, Muscle tone, Color, and Reflex irritability.
Scoring: 0-10 total; 7+ indicates good condition; 4 or lower requires attention (0-2 for each criterion).
Neonatal Behavioral Assessment Scale (NBAS) can be administered a few days after birth to evaluate 20 reflexes and the infant’s state/reactions to social stimuli; unresponsiveness may indicate neurological problems; useful as a parenting guide.
Labor and delivery medications:
Commonly used analgesics/anesthetics/muscle relaxants to reduce pain and induce contractions; these can affect pushing ability and infant alertness; when used appropriately, they improve maternal comfort without compromising delivery.
The social environment surrounding birth:
Mother's experience in the first 6-12 hours: a sensitive period for bonding (not mandatory for bonding; adoptive parents can form strong bonds).
Maternity blues: affects 40-60% of mothers; postpartum depression affects about 10% of mothers and requires professional help due to potential negative outcomes for mother and infant.
Father’s experience: “engrossment”—intense fascination and a desire to touch/hold the baby; early contact with the newborn can strengthen the partner relationship and support mother.
Siblings’ experiences: potential sibling rivalry.
Potential problems at birth:
Anoxia (oxygen deprivation): most cases result from umbilical cord entanglement during breech deliveries or premature placental separation; RH factor incompatibility can also cause issues (now often preventable).
Long-term risks: neurological damage, permanent disabilities, and increased risk of adult heart disease in some cases.
Complications of low birth weight:
Preterm: born more than 3 \text{weeks} early but with appropriate weight for gestational age.
Small for date (small-for-gestational-age): underweight due to slow fetal growth; greater risk of serious complications than preterm birth alone.
Short-term consequences for preterm/low birth weight infants:
40-50% with birth weight less than 2.2 \text{lb} die; preterm infants face breathing difficulties due to surfactant deficiency (respiratory distress syndrome) and often require isolettes.
Interventions for preterm infants:
Early acquaintance programs (touching, rocking, talking) promote development.
Parent training in responsiveness; combined with stimulating daycare can improve cognitive growth and reduce behavioral issues.
Long-term outcomes depend on postnatal environment:
Stimulating, supportive homes can offset early risk; poorer environments may lead to smaller size but also greater cognitive/behavioral challenges.
Reproductive risk and recovery (Kauai Longitudinal Study, Werner & Smith):
At birth: 16\% severe complications; 31\% mild complications.
At age 2: severity predicted progress, but emotional support and educational stimulation improved outcomes.
At age 10: severity less predictive; now home environment becomes more predictive of outcomes.
Key Formulas, Numbers, and Definitions (LaTeX)
Periods by time: ext{zygotic period} = 10-14 \text{days}; ext{embryonic period} = 3-8 \text{weeks}; ext{fetal period} = 9 \text{weeks} \, ext{to} \, 40 \text{weeks}
Implantation timing: 7-10 \text{days} after conception.
Implantation success rate: 25\%.
Blastocyst cell counts: 60-80 \text{ cells}.
Fetal viability window: 22-28 \text{weeks}.
Typical birth weight and size ranges mentioned: 4 \text{lb} (end of 7th month), 7-8 \text{lb} (full term), newborn length around 20 \text{inches}, weight 7-7.5 \text{lb} at birth.
Apgar scoring: total 0-10; each criterion scores 0, 1, ext{or} 2; a score of 7+ is generally normal, while a score of 4\downarrow requires attention.
Antenatal weight gain: 25-35 \text{pounds}.
Folic acid enrichment: reduces risk of neural tube defects (e.g., spina bifida, anencephaly).
Exposure risk indicators: 70\% reduction in HIV transmission with antiviral ZDV; other teratogen effects are dose- and duration-dependent.
Connections and Practical Implications
Theory connections:
Development proceeds via germ layer differentiation (ec/to/derm) and organogenesis; disruptions during critical periods can lead to specific defects.
The placenta acts as a selective barrier; its proper function is essential for fetal development and is influenced by maternal health and nutrition.
Real-world relevance:
Prenatal care, nutrition, and avoidance of teratogens significantly reduce risk of congenital disorders.
Stress management and social support during pregnancy positively influence birth outcomes.
Early identification and intervention for preterm infants improve long-term cognitive and behavioral outcomes.
Ethical/philosophical considerations:
Balancing maternal autonomy with fetal health in decisions about medications, lifestyle, and timing of pregnancy.
Access to prenatal care and social support systems to reduce disparities in birth outcomes.