Untitled Flashcards Set
GDC standards
Raise concerns
Sharing information
Multidisciplinary/multi-agency approach
Escalating concerns
Oral health promotion
Every contact counts
May be only regular health professional contact
Local support → you should have an understanding of the process in your local region.
In your practice
Safeguarding policy
made aware of this at induction
Named safeguarding lead
Regular safeguarding training
Whole tema
Level 2(minimum 3 hours) [Level 3 if specialising in Paeds]
Three yearly update
On clinic
A patient presents with concern
Inform tutotr of your concerns in an appropriate way
The tutor will support/lead the following BEFORE THE PATIENT LEAVES:
Documentation
Documentation of facts in a contemporaneous way
If disclosure, then important that patients own words used where possible
Raise concern with safeguarding team - ICE and telephone call
Completion of datix
Logbook for safeguarding incidents
Debrief
Making disclosures/sharing ideas
Assessment of capacity
If patient lacks capacity, appropriate level of information can ba shared with others, if it is in the patients best interests (in line with the MCA 2005)
If the patient has capacity, where possible their wishes should be respected
Exception include legal issues (e.g. court orders) or public interest (e.g. matter of safety)
The proportionality principle - information shared should be proportional to situation and your response proportional to risk
Can be a challenging conversation
Do you always inform the patient/carer/family?
Assessing the patient
history:
details from the child and carer of any injury or presenting complaint
Past dental history
medical history
family and social circumstances
Features of concern would include:
a delay in the presentation (e.g. previous trauma not addressed)
Discrepancies between the history and examination findings
Developmentally inappropriate findings (does not fit with the age of the child)
Previous concerns about the child or sibling
Examination
Any dental, oral of facial injuries, their site, extent and any specific patterns
The general appearance of the child, their state of hygiene, whether they appear to be growing well or are failing to thrive
Their demeanour and interaction with their parents or carers and others (e.g. look for signs of ‘frozen watchfulness’ - where the child seems to take in everything going on, but in a detached, wary or fearful manner.
Managing dental neglect
Recognise and record concerns - clear case notes and maintain clinical correspondence
record dental history
Record UTA/WNB/FTA
Raise concerns with parents, don't blame, offer support, set targets, keep records, monitor progression
Preventative multi-agency response 0 liase with other professionals
Discuss with senior colleague/names professionals
Inform GMP and other relevant professionals
Assess whether there are signs of general/ wilful neglect/ risk of significant harm and refer to social services if so/ the situation is deteriorating
Escalating concerns
important that patients are provided with safe and effective car within your practice
There should be robust measures in place to ensure your environment is safe e.g. Ensuring waters are run through, cleaning schedule, dating of instruments, electric equipment checked annually and documented.
There are external agencies who are involved in regulation
Documentation of concerns
Follow local policy for raising concerns
This should be discussed at induction
Actions that will be taken
Timeframe
Escalating concerns
Local area team
CQC
GDC
Case
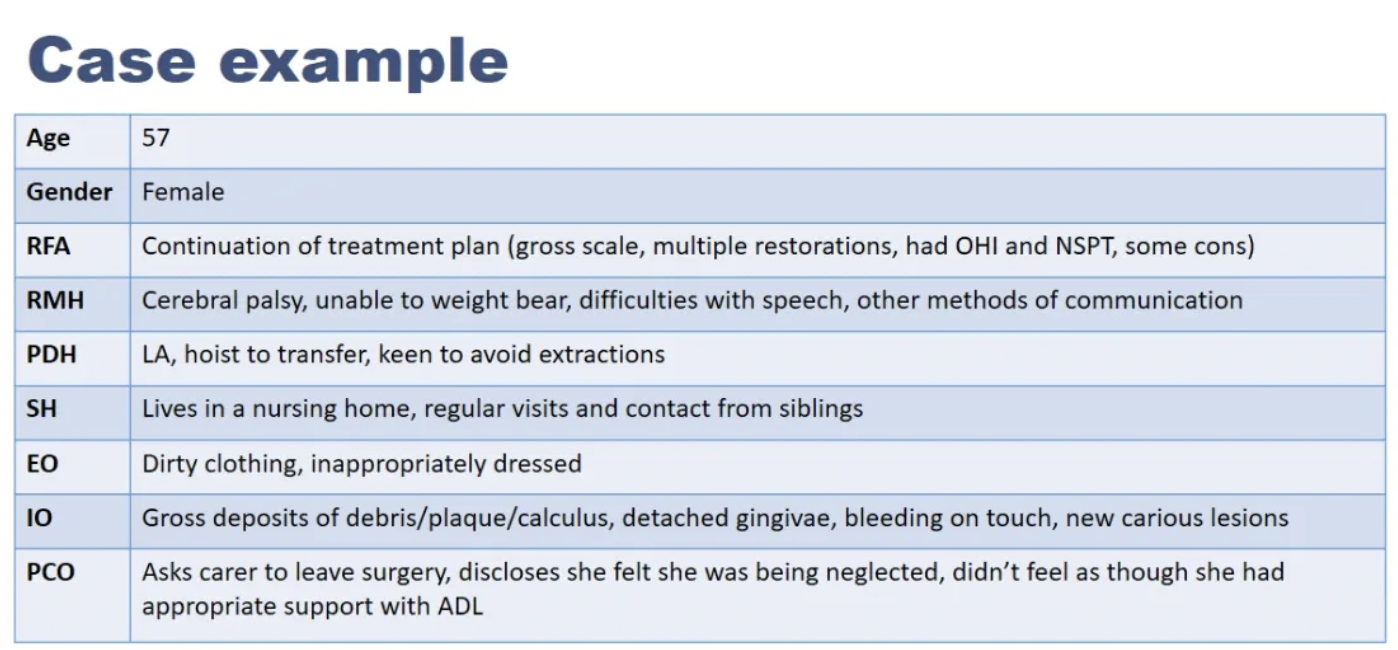
Case RED FLAGS
Poor OH despite OHI/NSPT has been given/completed
New carious lesions
Unkempt appearance Inappropriate clothing
Uncomfortable relationship with carers
Disclosure by patient
What to do?
Complete treatment planned (if patient happy/able)
Ask the patient is she feels able to return to the home Contact her NoK (with the patients consent) and others involved in her care
Alert safeguarding team at LUHFT
Documentation
notes
logbook
datix
Write a letter to care home manager