W7: Neonatal Chest Radiography Notes
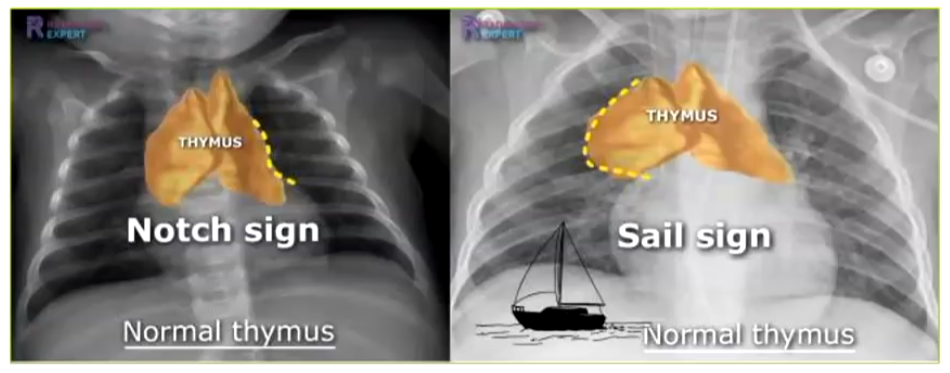
Thymus
Notch sign: Associated with a normal thymus.
Sail sign: Associated with a normal thymus.
Terminology and Abbreviations
Most neonatal radiography is performed in the Neonatal Intensive Care Unit (NICU), also known as the Intensive Care Nursery (ICN), typically on preterm infants.
A preterm infant is defined as a child born prematurely at less than 37 weeks gestation.
Classification and abbreviations of preterm infants:
Low birthweight (LBW): 2500-1500 grams
Very low birthweight (VLBW): 1500-1000 grams
Extremely low birthweight (ELBW): Less than 1000 grams
Foetal Lung Development and Thermoregulation
Foetal lung development occurs in 5 stages:
Embryonic: 3-7 weeks
Pseudoglandular: 5-17 weeks
Canalicular: 16-26 weeks
Saccular: 26-36 weeks
Alveolar: Greater than 32 weeks
Preterm infants often lack mature surfactant production. This deficiency impacts the alveoli, leading to:
Insufficient mature surfactant to reduce surface tension.
Alveoli collapse or partial collapse during inspiration, causing atelectasis.
Poor oxygenation of the lungs.
Neonates struggle to thermoregulate.
In utero, a foetus maintains a temperature 0.3-0.5 °C higher than the mother due to placental heat transfer.
Upon birth, neonates enter a colder environment, requiring heat production via lipolysis within their brown fat, known as thermogenesis.
This process requires adequate oxygenation to function effectively.
Surfactant
Surfactant prevents alveoli and acini from collapsing and sticking together during expiration, thus preventing atelectasis.
Surfactant (Continued)
Natural surfactant production begins around week 24 of gestation and increases with gestational age.
Infants born after 32 weeks usually have sufficient surfactant production to breathe naturally.
Preterm infants born with insufficient mature surfactant may present with respiratory distress and develop Neonate Respiratory Distress Syndrome (NRDS).
In preterm infants with NRDS, surfactant may be delivered via an endotracheal tube.
Responses to surfactant delivery can vary:
Good initial response followed by relapse — would be from rupturing the alveoli and creating pneumothorax
No response.
Very good response.
Severity, Incidence, and Survival of Preterm Infants
Severity and incidence of complications are inversely related to gestational age (GA).
92% of neonates born at 24-25 weeks
88% of neonates born at 26-27 weeks
76% of neonates born at 28-29 weeks
57% of neonates born at 30-31 weeks
Survival rates based on gestational age at birth:
Less than 23 weeks: nearly zero.
23 weeks: approximately 15%.
24 weeks: approximately 55%.
25 weeks: approximately 80%.
Severity, Incidence, and Survival of Preterm Infants (Continued)
Chances of surviving unimpaired or with minimal impairment:
6-20% for less than 25 weeks gestation.
Less than 5% for less than 23 weeks.
Range of adverse outcomes:
Usually neurodevelopmental.
Some may result from treatment (treatment injury), which is different from a nosocomial infection
Examples: blindness (retinal burns from high O₂ levels), compromised respiratory function (high PEEP or long-term intubation).
PEEP: Positive End Expiratory Pressure
Nosocomial infection: an infection acquired while receiving healthcare in a facility like a hospital or clinic
Role of Incubator/Humidicrib/Isolette
Provides a stable, temperature-controlled environment.
Provides a controlled humidity environment.
Provides a controlled oxygen environment.
Preterm infants have an immature thermoregulation system.
Preterm infants under 30 weeks have an immature epidermis, increasing the risk of transepidermal water loss.
High humidity can lower oxygen levels in the incubator.
Types of Beds in NICU
Radiant Warmer
Giraffe Bed
Incubator/Isolette
Basic Principles for Radiographers in NICU
Production of high-quality radiographs with minimal radiation dose to the infant is paramount.
The radiograph must be achieved with minimal disturbance to the infant.
Infants in open or closed incubators MUST NOT be treated as regular patients having portable/ward radiographs.
The life of the infants relies heavily upon the quality of the radiographs.
Basic Principles for Radiographers in NICU (Continued)
Neonatal radiography in NICU requires:
Strict attention to infection control by the radiographer.
Removal of watches and jewelry.
Hand washing before and after the radiographic exam.
Cleaning the detector and placing it in a protective cover.
The radiographer must function as a team member with the neonatal nursery and the neonatal intensive care nurse.
The radiographer must be aware that handling can provoke episodes of bradycardia, hypoxia, possible heat loss, and damage to the delicate skin.
ALL HANDLING NEEDS TO BE KEPT TO A MINIMUM; EXCESSIVE HANDLING CAN CAUSE A RESPIRATORY OR CARDIAC ARREST.
Important Points to Remember
Respiratory infection is the major cause of illness and death in infants and children.
The risk of low-level radiation from a chest or abdomen radiograph is far outweighed by the potential outcome of undiagnosed pulmonary disease.
However:
Don’t disregard good collimation, good exposure technique, and good diagnostic images.
Don’t stress the neonate.
Don’t allow the infant to suffer thermal stress.
Don’t ignore infection control.
Guidance Points for a Neonatal Chest
Adapted from European Guidelines:
Focal spot: 0.6 mm (≤ 1.3 mm)
FDD: 80-100 cm
kVp: 60-65
Exposure time: < 4 mS
Filtration: 1 mm Al and 0.1 mm or 0.2 mm Cu
Grid: Not used
Collimation: < 1 cm tolerance around anatomy
Skinfolds
Care must be exercised with positioning the infant, as skin folds can be created which mimic pathology — especially pneumothorax

Radiography in Closed Incubator
Head must be maintained straight with lead rubber placed on top to protect hands and neonates gonads.
Method of Restraint
Note: tilt on cassette, head straight, arms out from the body, and legs resting over a roll — better visualisation of apices
Internal Tubes and Catheters
Endotracheal (ET) tube
Nasogastric (NG) tube
Umbilical artery catheter
Temperature probe
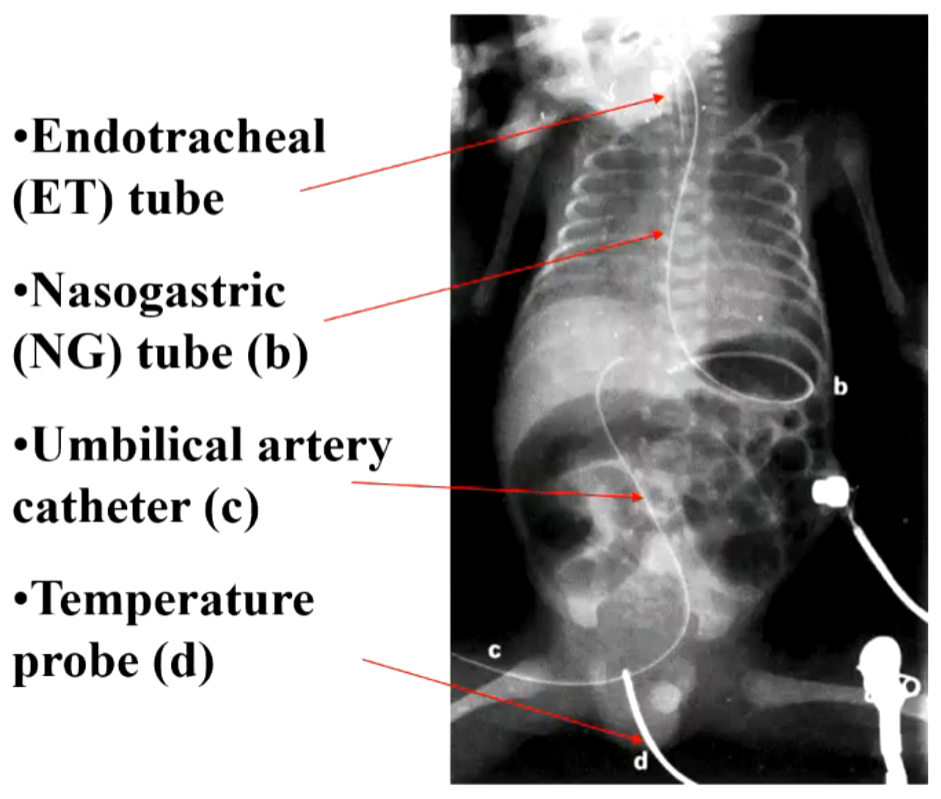
Internal Tubes and Catheters (Endotracheal (ET) Tube)
Distal tip of the ET tube should be at the level of T2 – approximately 1-2 cm above the carina.
Movement (rotation, flexion, extension) of the infant's head will alter the location of the tip.
Radiographically, the head should be straight and not rotated, BUT the infant's head should be kept in the position in which they are being nursed.
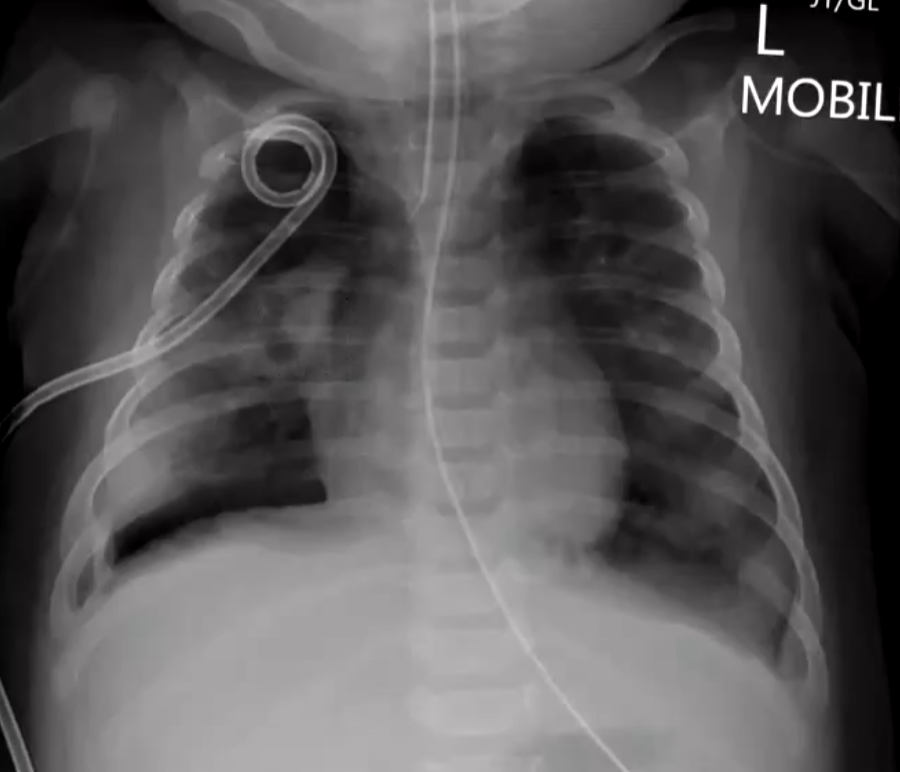
Internal Tubes and Catheters (Umbilical Arterial Catheter)
Enters through the umbilicus and is used to monitor blood and infuse fluids.
Correctly positioned, it should be at L3 or T12.
The entire length of the catheter needs to be demonstrated, requiring a combined chest and abdomen radiograph.
There are two umbilical arteries that enter the right and left common iliac arteries, functioning in-utero by carrying blood from the ductus arteriosus to the placenta for oxygenation.
In the provided image, the catheter is in the umbilical vein, approximately at T12.
External Catheters
ECG leads
Cutaneous temperature electrode
Oxygen and carbon dioxide electrodes
NJ (nasojejunal) tube (NJ indicates tip of tube). Feeding tube.
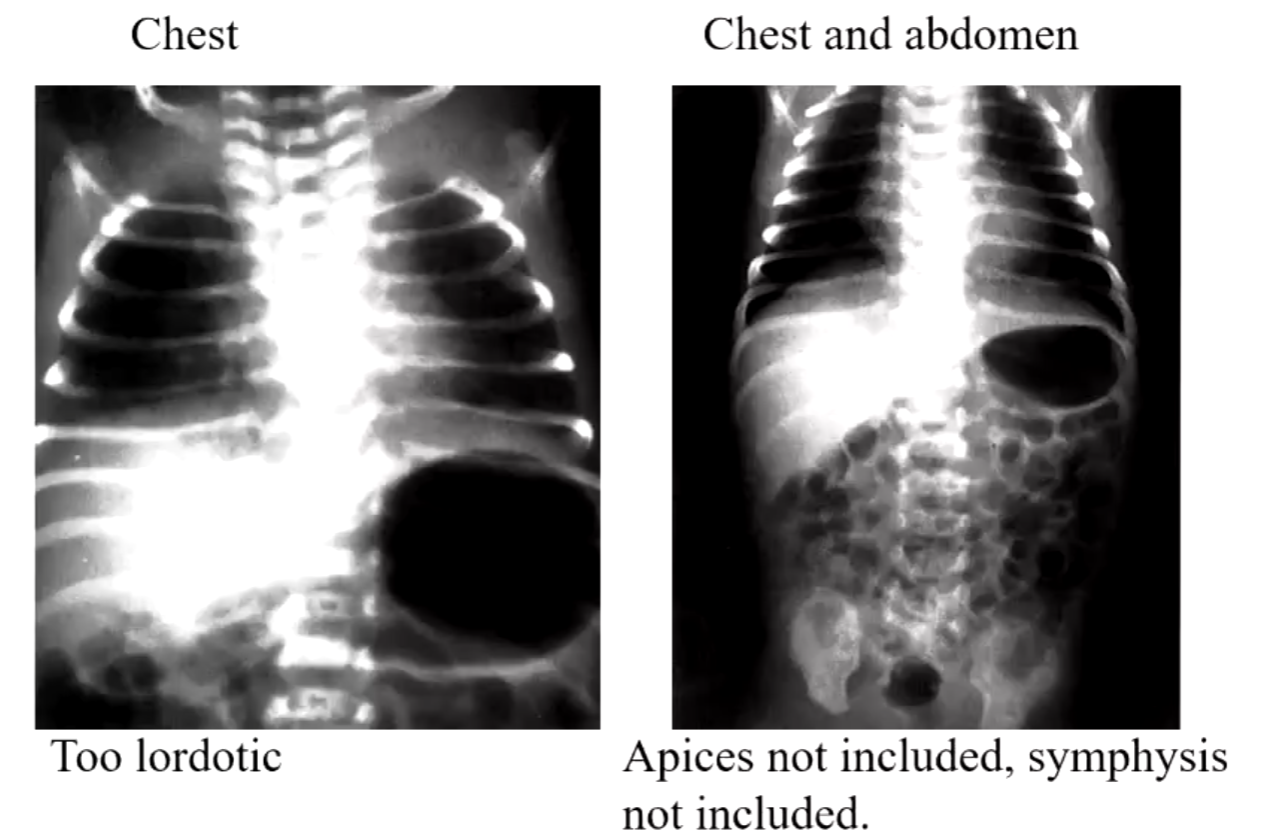
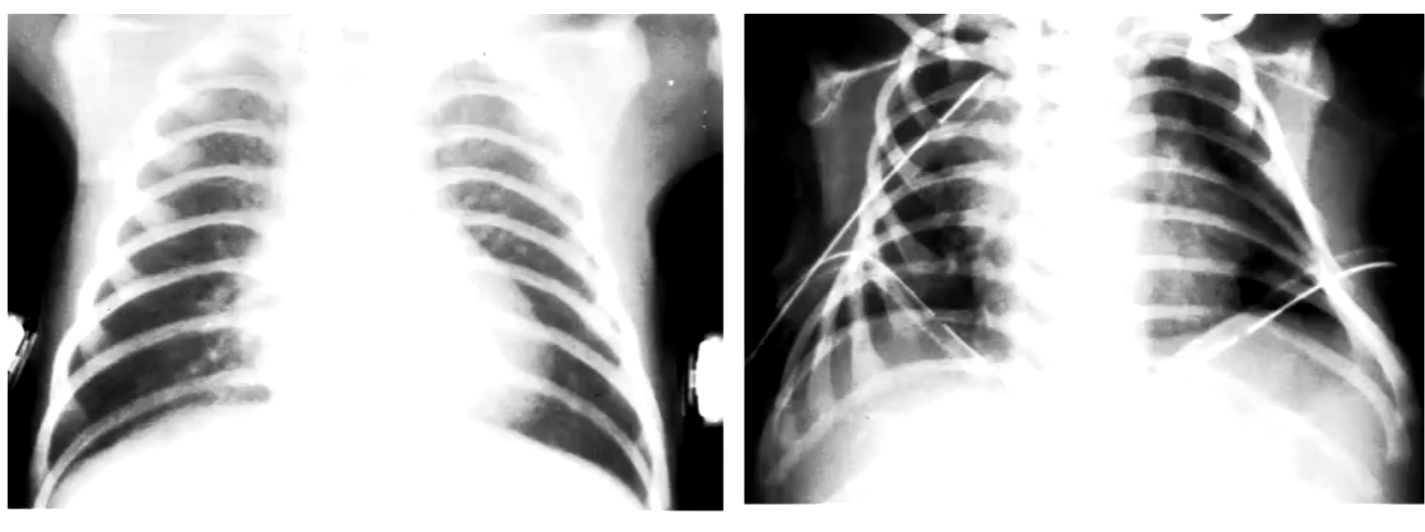
Positioning Errors
Examples of positioning errors in neonatal radiography.

Posterior Costophrenic Angle
The posterior costophrenic angle is steeper on a neonate than on an adult.
Tube angle 10-15 degree caudaltilt may be necessary to accurately visualize the costophrenic angles without causing distortion of the diaphragm.
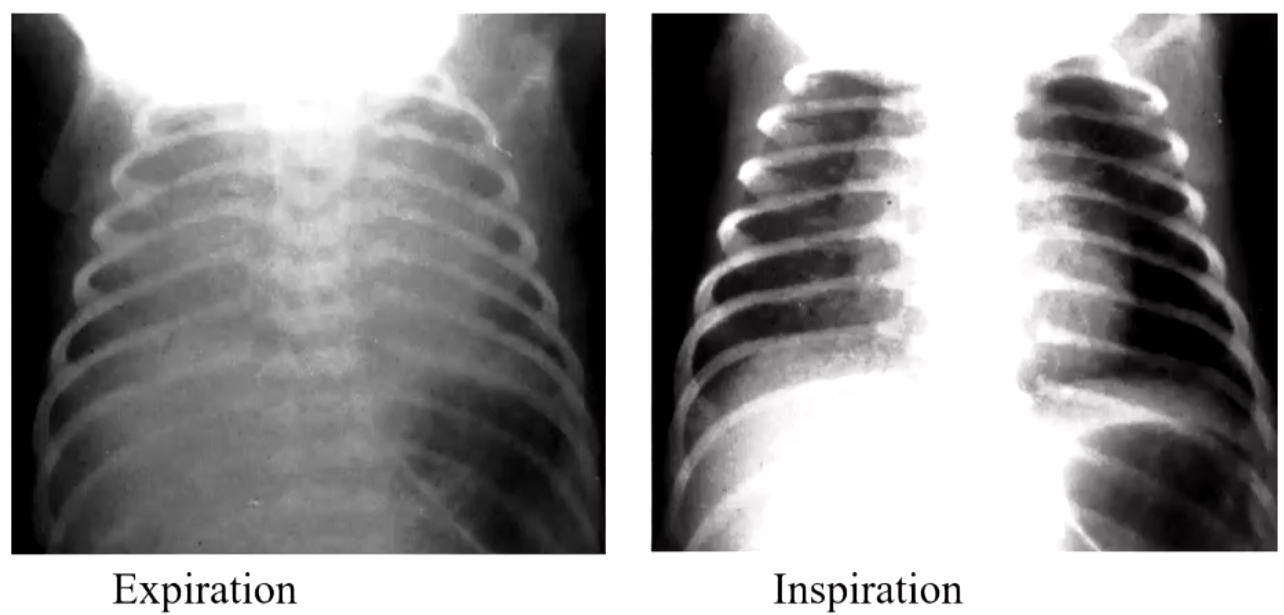
Positioning (Incorrect vs. Correct)
Examples of incorrect and (nearly) correct positioning in neonatal radiography.
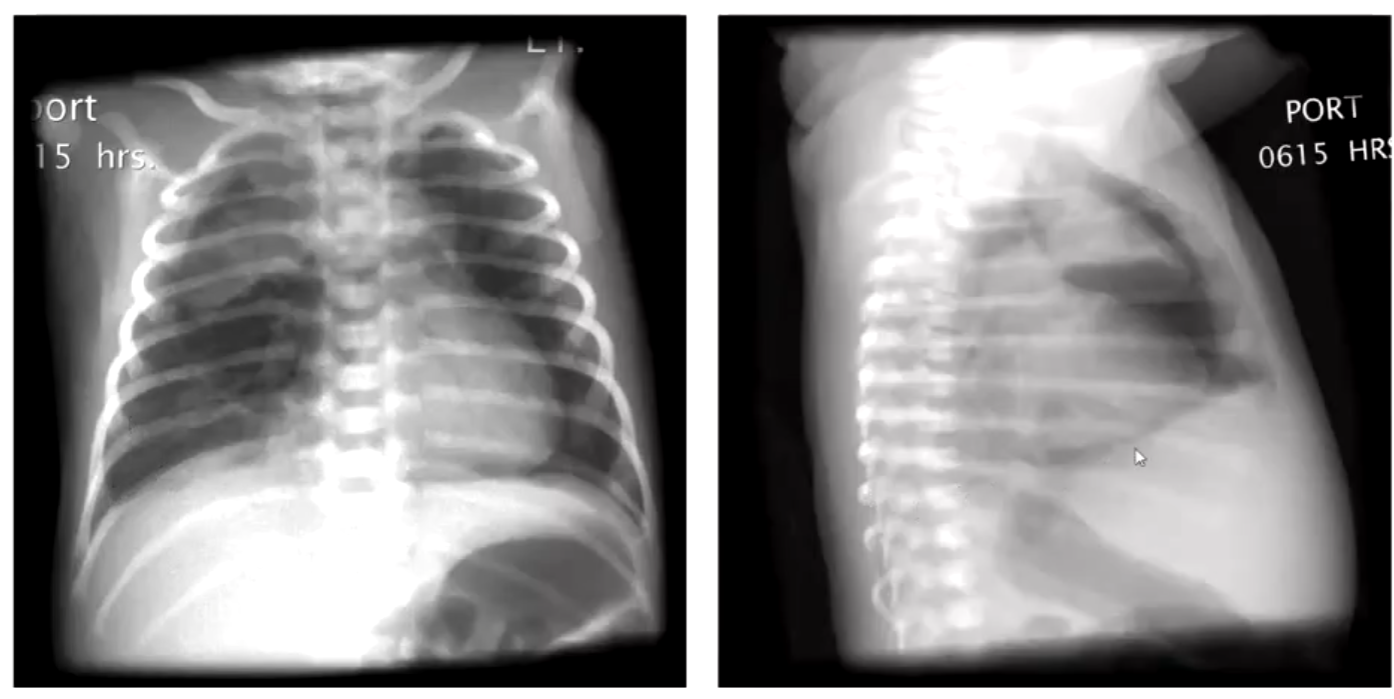
Effect of Respiration Phase on CXR
Comparison of CXR appearance during expiration and inspiration.
Specific Respiratory Diseases Onset During the First Few Days
Diffuse or bilateral conditions:
Transient tachypnea of the newborn (TTN) – term newborn
Neonatal Respiratory Distress Syndrome (NRDS) - preterm
Neonatal pneumonia – preterm and term
Meconium aspiration syndrome (MAS) - term
Persistent pulmonary hypertension - term
Focal or unilateral conditions:
Diaphragmatic hernia - congenital
Pleural effusion (chylothorax) – preterm and term
Neonatal Respiratory Distress Syndrome (NRDS)
Clinical Symptoms:
(Central) cyanosis – blue tint to skin due to low oxygen saturation.
Tachypnoea – fast breathing.
Nasal flaring – widening of nostrils.
Expiratory “grunting” noise.
Intercostal retraction – due to negative intrapulmonary pressure.
Radiological Signs:
Lungs will be under-inflated.
Lungs appear opaque or mottled – ground-glass appearance.
Air bronchograms present.
The degree of opacity or mottling determines the severity of NRDS (mild, moderate, or severe).
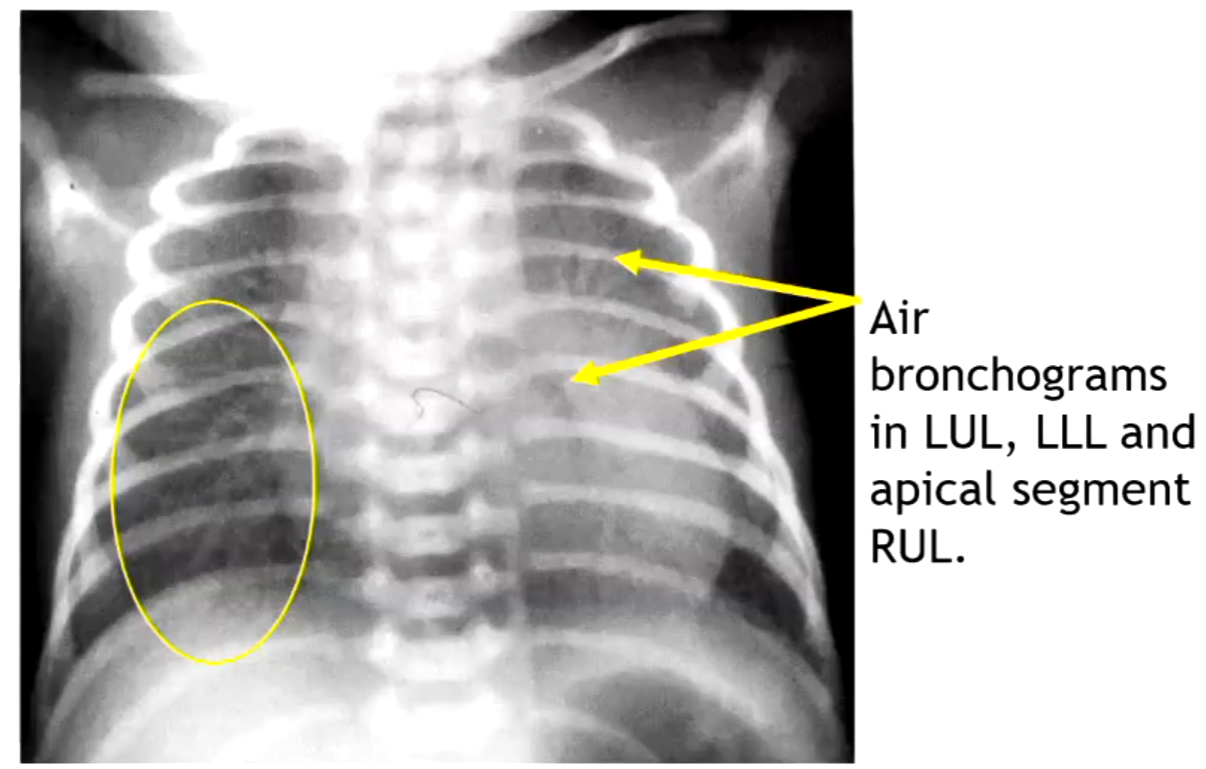
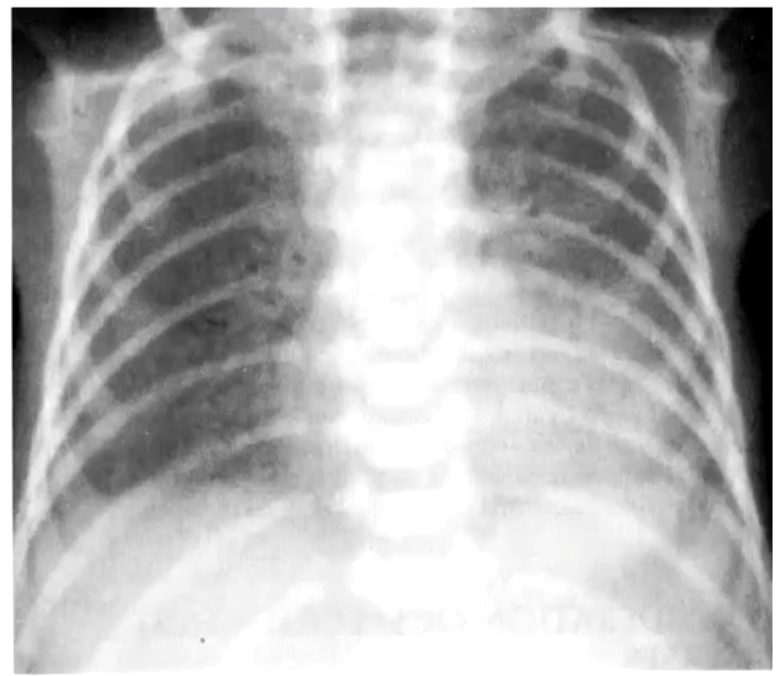
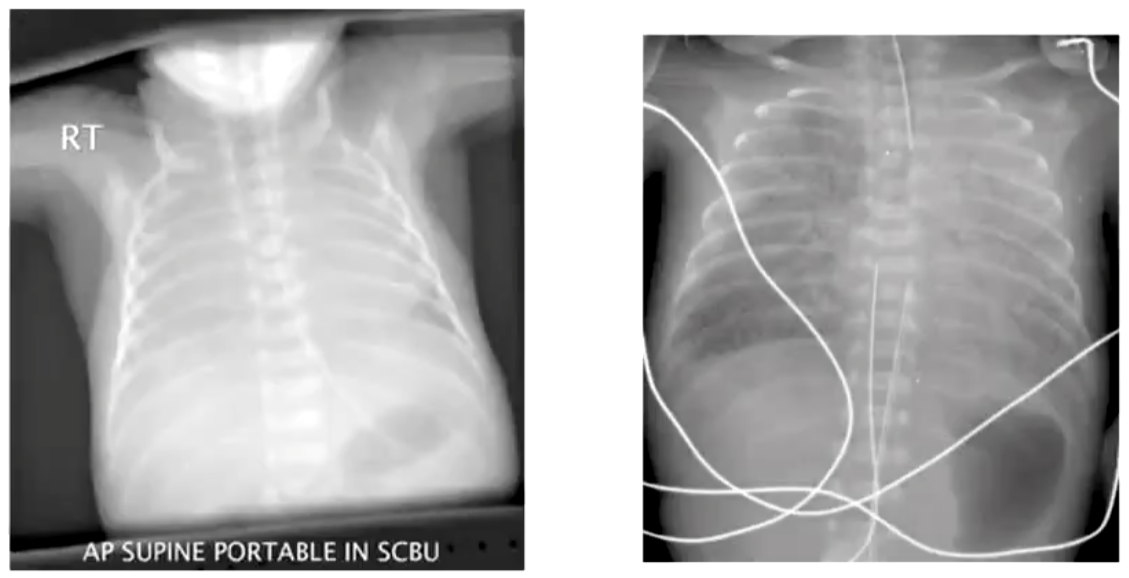
NRDS - MILD
Air bronchograms in LUL, LLL, and apical segment of RUL.
Faint ground-glass appearance in both lung fields.
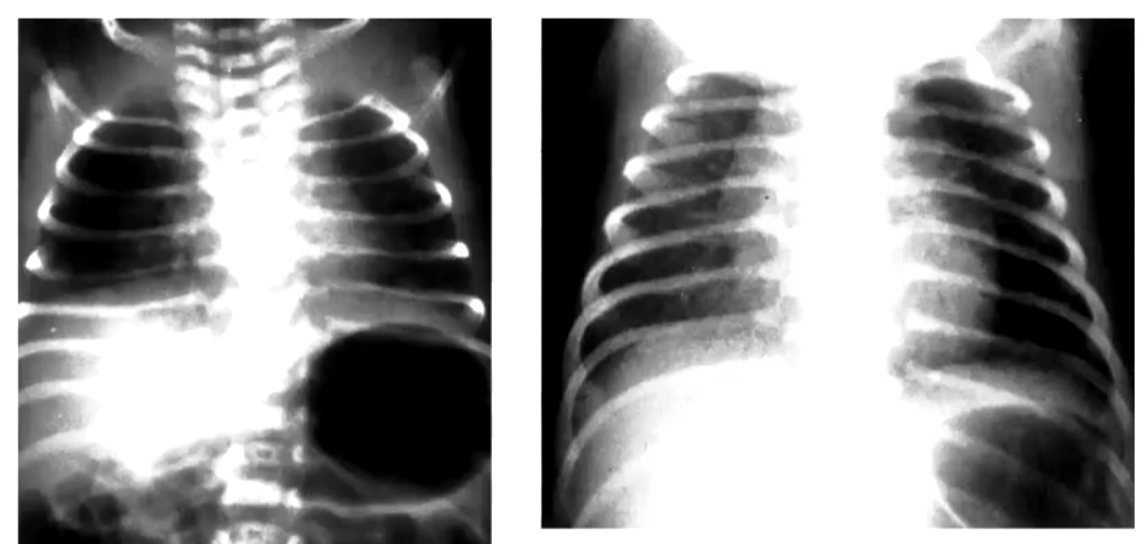
NRDS - MODERATE
Radiographic appearance of moderate NRDS.
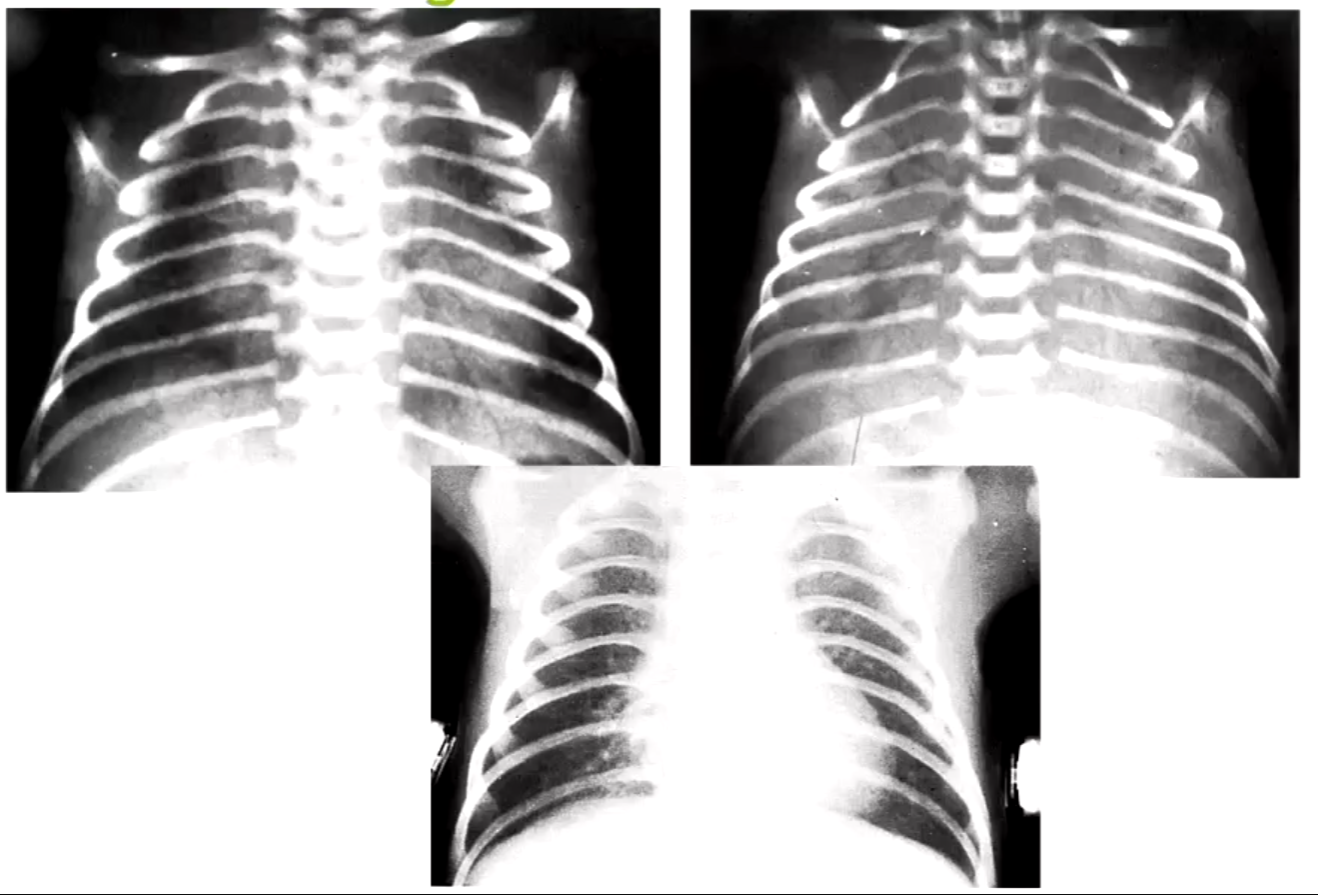
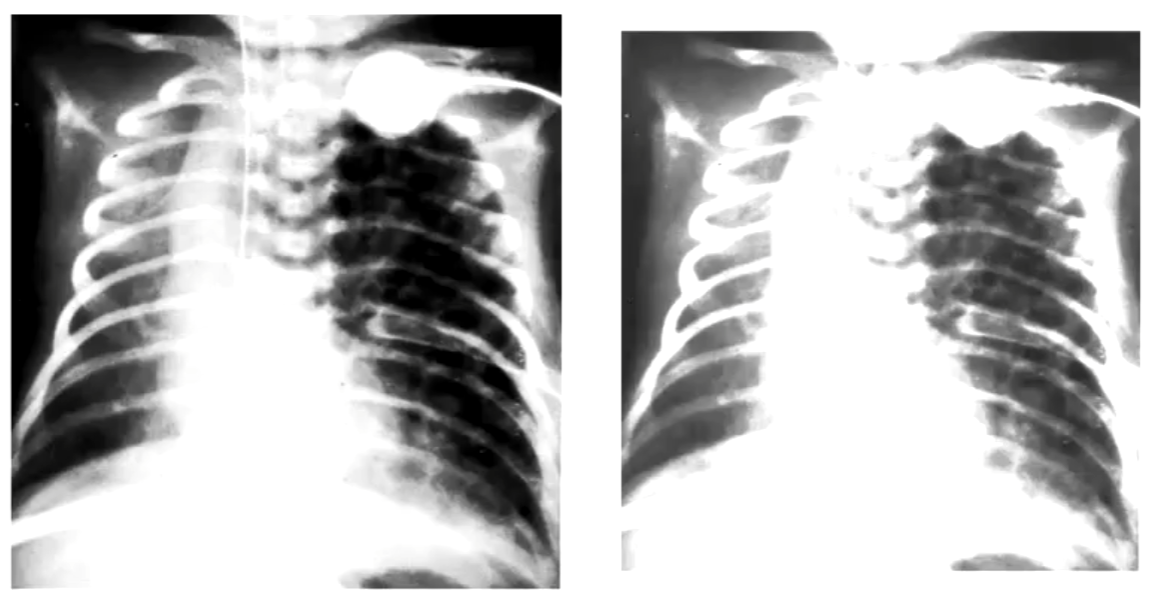
NRDS - SEVERE
Radiographic appearance of severe NRDS.
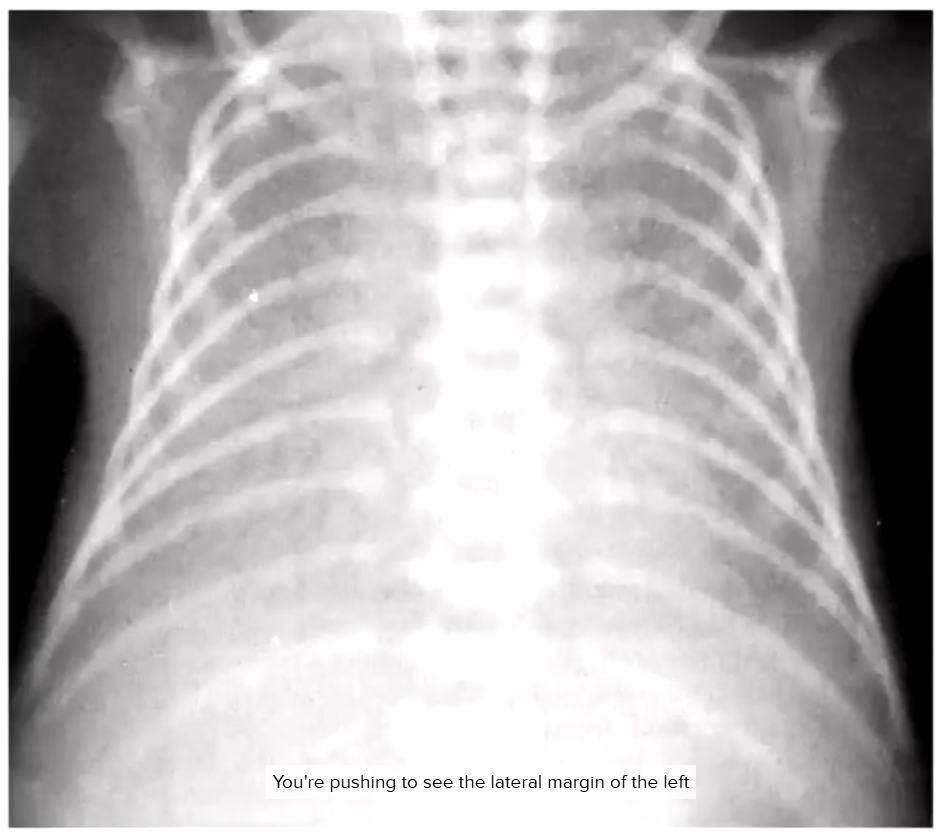
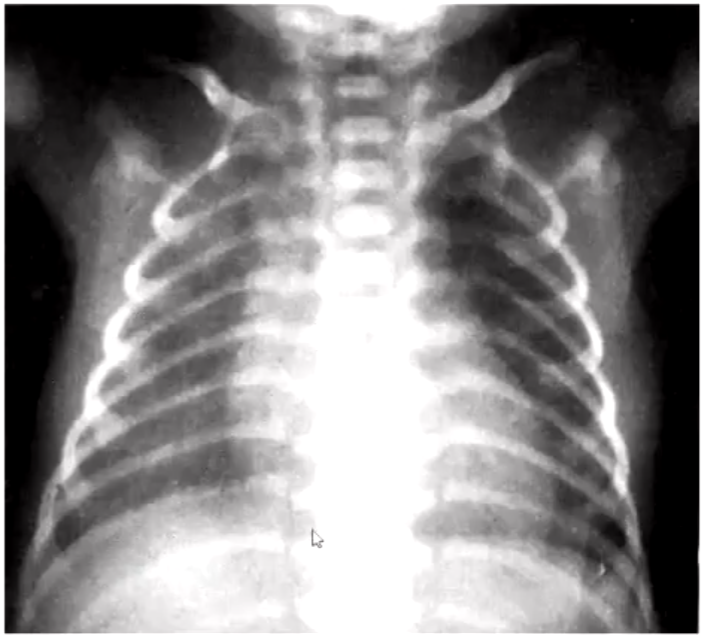
Shape of Thoracic Rib Cage
Normal vs. Abnormal ('bell-shape')
Abnormal bell shape: indicates poor lung aeration — lungs unable to push ribcage outwards
Lungs
Normal fully developed aerated lungs.
Underdeveloped lungs.
Air Bronchogram on NRDS
Illustration of air bronchograms in NRDS.
Gas-filled bronchi become visible due to increased density in the surrounding lung tissue
Meconium Aspiration Syndrome (MAS)
Meconium is a dark green, tarry collection of dead bowel cells contained within the full-term foetus, typically passed as a stool within the first 24 hours.
If foetal distress occurs during labour, meconium can be discharged into the amniotic fluid.
In some cases, a small amount can be aspirated, leading to respiratory obstruction and respiratory distress.
MAS can range from mild respiratory distress to severe respiratory failure, with approximately 50% requiring Continuous Positive Airway Pressure (CPAP).
Meconium Aspiration Syndrome (Continued)
If meconium-stained amniotic fluid is aspirated, it can result in:
Chemical pneumonitis.
Obstruction of bronchi by a ball-valve mechanism, potentially leading to a pneumothorax.
Surfactant deactivation.
Severe hypoxemia (low oxygen level in the blood, different from hypoxia, which is low oxygen level in body tissues) leading to hypoventilation.
Bronchopulmonary Dysplasia (BPD) / Chronic Lung Disease of Prematurity (CLDP)
A long-term complication resulting from barotrauma from sustained ventilator pressure and oxygen toxicity.
Defined by the neonate requiring supplemental oxygen for >28 days in a preterm infant born <32 weeks or a VLBW preterm infant.
Symptoms vary but can include continued respiratory distress or the need for ventilation after initial RDS treatment.
BPD is a complex and serious cardio-pulmonary morbidity.
Congenital Diaphragmatic Hernia
Typically left-sided (5-9:1 ratio).
Posterolateral defect.
May involve bowel, spleen, left lobe of liver, kidney, pancreas, with stomach being rare.

Pulmonary Haemorrhage
Can have a dramatic appearance on onset.
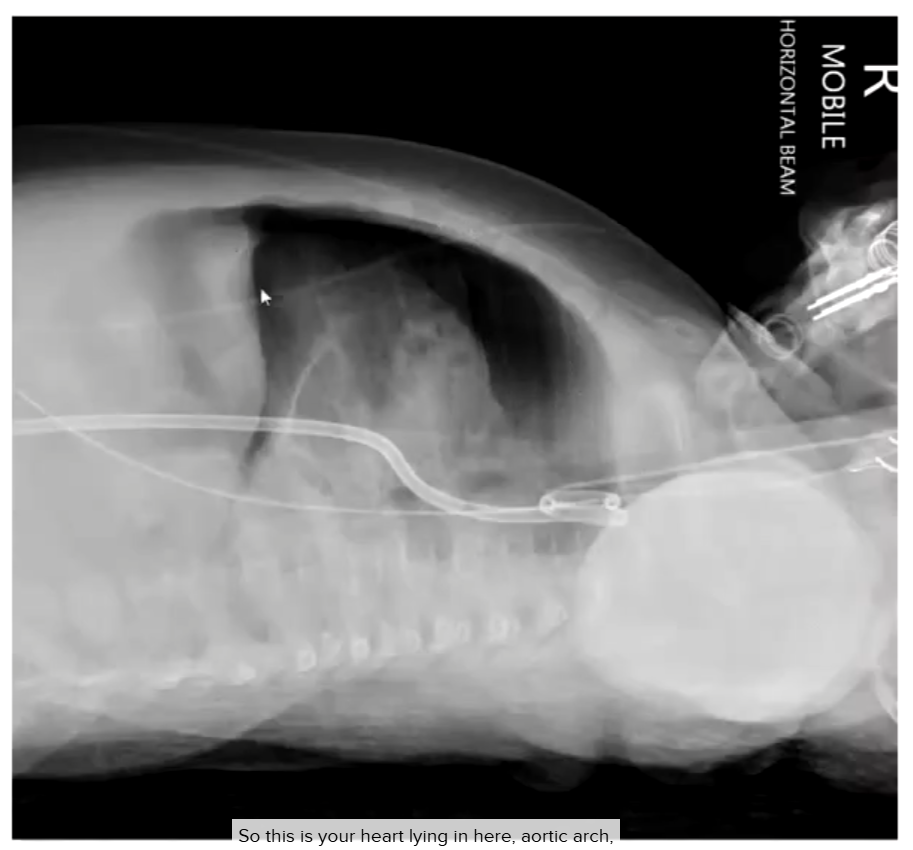
30-week infant, treated for NRDS, sudden worsening - ? massive aspiration, Pulmonary oedema from PDA (patent ductus arteriosus), pulmonary haemorrhage. Resolved after 3 days.
Pulmonary Interstitial Emphysema (PIE)
Results from CPAP and poor lung compliance (stiff lung), leading to alveolar distension and rupture with dissection of air into the lung's interstitial space, forming small cysts that may combine into larger air collections.
Often an incidental finding before respiratory signs appear, leading to vascular compromise and progressive hypoxia.
Occurs in 20-30% of premature infants, more common in VLBW infants, and frequently precedes a pneumothorax.
Radiographic appearance: areas of translucency within the lungs and areas of atelectasis.
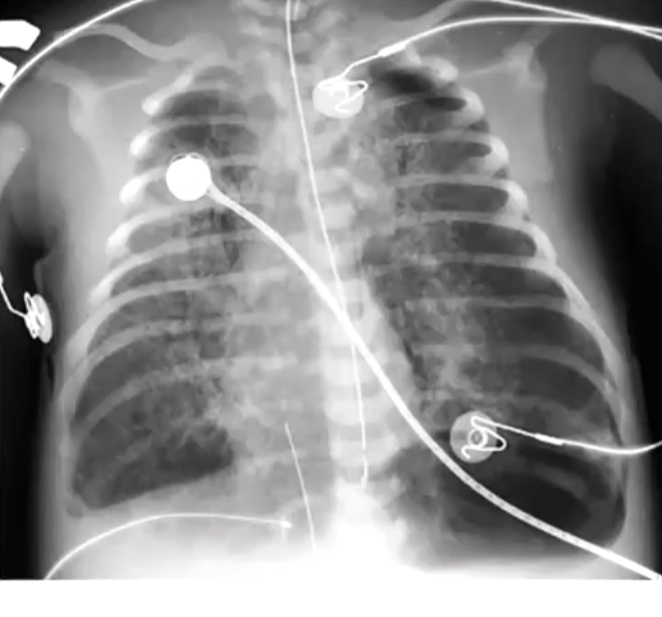
Neonatal Pneumothorax - Supine AP
Radiographic example.
Pneumothorax Symptoms
Sharp stabbing pain on inspiration
Shortness of breath
Bluish skin due to decreased oxygen sats – hypoxia
Fatigue
Rapid breathing and tachycardia
Hyper-resonance to percussion
Decreased breath sounds
Observable on a neonate:
#3 would be picked upon on the oxygen monitor
#5 heart rate would be on the monitor
maybe #6 and #7 would be using stethoscope listening to breath sounds
On an adult in A&E #1 and #2 would be the initial presenting symptoms
Easier to identify on a child or adult but much less easy on a preterm neonate with NRDS.
Dorsal Decubitus for Lateral CXR
*Radiographic example.
Lateral Chest Projection
Performed as a dorsal decubitus (horizontal beam lateral).
Dorsal decubitus is preferred as it doesn't require changing the infant's position, especially if pneumothorax is suspected, and it demonstrates the anatomic position of the pneumothorax.
If pneumothorax is not suspected, a supine rolled lateral can be performed.
Pathologies for Lateral or Decubitus Chest
Pneumothorax – horizontal beam lateral query anterior mediastinal air on some occasions and AP or PA with side being queried raised.
Pleural effusion – horizontal beam AP or PA with side with ? Effusion lowered.
Chest mass – supine rolled lateral.
Atelectasis - supine rolled lateral.
Pneumomediastinum - Overt
Radiographic example.
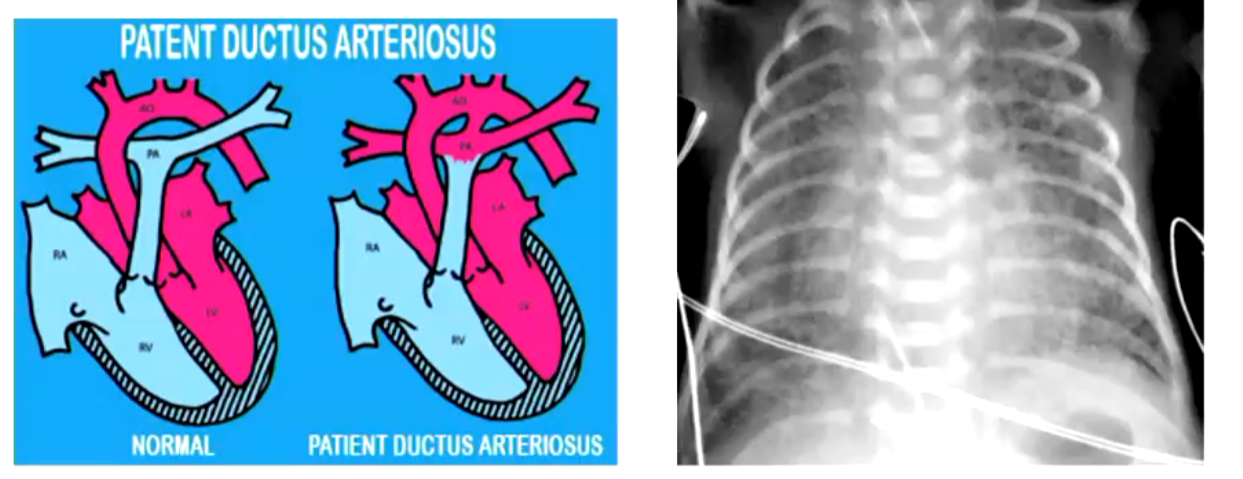
Patent Ductus Arteriosus (PDA)
Ductus arteriosus doesn’t undergo automatic muscular hypertrophy in a premature infant.
If the lungs become high resistance in a preterm infant with RDS, the ductus arteriosus will remain patent, resulting in complications for the preterm infant’s treatment.
Jacqueline Kennedy and NRDS Research
In 1963, Jacqueline Kennedy gave birth to a baby nearly six weeks early. The baby developed breathing difficulties and was diagnosed with hyaline membrane disease (now called neonatal respiratory distress syndrome).
He was treated in a hyperbaric chamber but died two days later.
This case heightened public awareness and spurred further research into respiratory distress and its treatment.
Jacqueline was married to John F. Kennedy, who was assassinated in Dallas, Texas.