Block Two baby
Diet Guidance for HTN and CVD prevention
DASH - Dietary Approaches to Stop Hypertension
A diet rich in fruits, veggies, and low fat dairy foods, can substantially lower bp in individuals with HTN and high normal bp. The greatest potential is in African Americans and the elderly
Control Macros and fiber
Increased fruits and veggies to 8.5 servings
Decrease in systolic and diastolic in ENTIRE study group
Combination - add 2-3 servings of low fat dairy to fruit and veggie diet
Significant decrease in systolic and diastolic bp in both groupes
greatest drop was in systolic in HTN group (11.4 mmhg)
Study outcomes
Follow up was up to 10 years.
Linked to 27% less strokes
15% decrease in heart disease
Implications of the study means that the diet compares to pharm management in mild HTN peeps.
What the diet includes
7-8 servings of grains
4-5 servings of veggies
4-5 servings of fruit
2-3 servings of low fat dairy
2 (or less) servings of meat, poultry, fish
2-3 servings of fats and oils
limit sweets
nuts, seeds, and dry beans 4-5 times/week
AHA recommendations for risk reduction
Try to balance calorie intake and physical activity - know what calorie content to achieve a healthy weight.
Consume a diet rich in fruits and veggies.
Try to pick canned veggies without added sauces, salt, and sugar
Choose whole grain and high fiber foods over bleached breads.
Increase fiber with beans, whole grains, fruits, and veggies
Consume fish (extra oily) 2x a week.
Minimize intake of things with added sugars.
Try to use less salt.
Only consume alcohol in moderation.
Eat smaller portions - know the calorie content of the foods you are consuming
Soy Proteins
Minimal evidence of CVD benefit
MAY help with cholesterol level if use to replace animal products
Fish Oil Supplements
Associated with decreased risk of CVD
Those with documented CVD should consume ~1g/day (preferably from oily fish)
Antioxidant Supplements
NOT the move - beta-carotene is linked to a higher risk of lung cancer in smokers and high dose vitamin E is linked to CHF and mortality. Just get your antioxidants the normal way, by eating them straight up.
Mediterranean Diet
The mediterranean diet is high in fat, especially olive oil, fish, nuts, low in red meat - associated with decreased risk of CVD. Emphasizes fruits, root veggies, flax and canola. AHA states that any high fat diets should be used with caution, however.
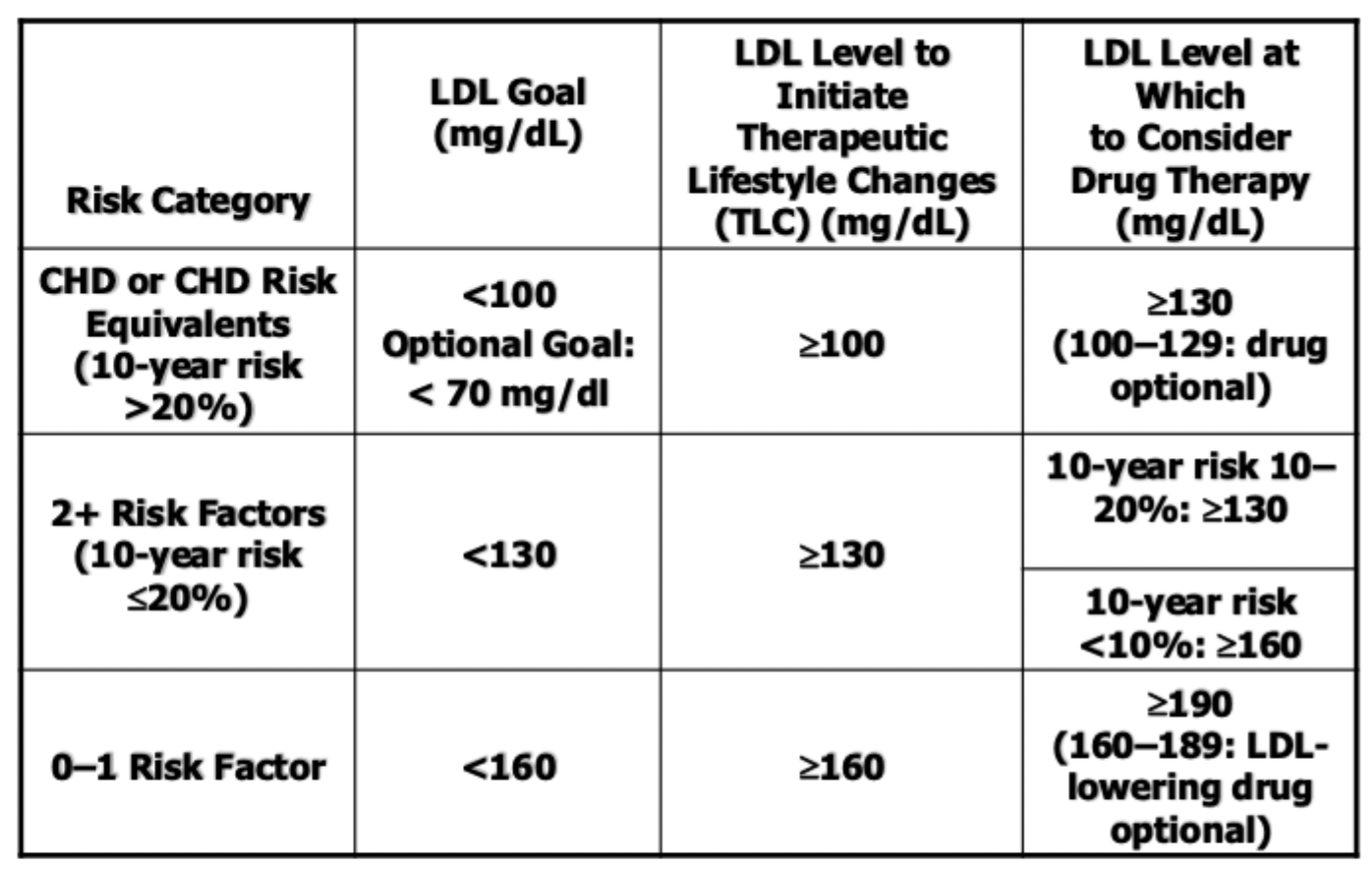
Adult Treatment Panel III (ATP III)
This study basically states that DM is a risk factor for CHD and uses the framingham projections of 10 year absolute risk to identify higher-risk patients.
Risk Factors
Cigarettes
HTN over 140/90 or medicated
Low HDL
Fam Hx of premature CHD
Male 1st degree less than 55
Female 1st degree less than 65
Age
Men over 45
Women over 55
Targeting Metabolic Syndrome
Red Flags for Metabolic Syndrome
Truncal obesity
Atherogenic dyslipidemia
elevated TGs
Small LDLs
Low HDL
Raised BP
Insulin resistance (± glucose intolerance)
Pro-inflammatory state
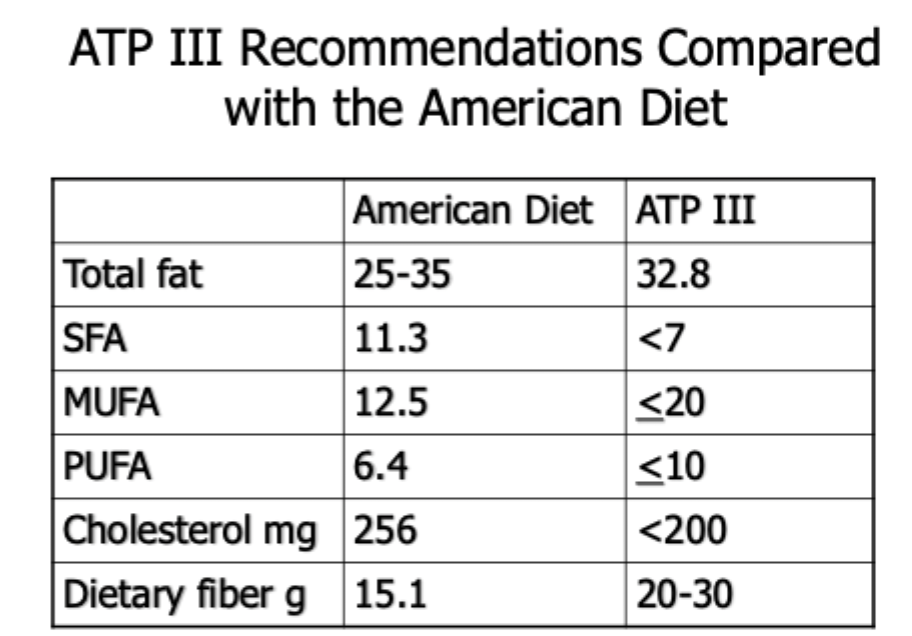
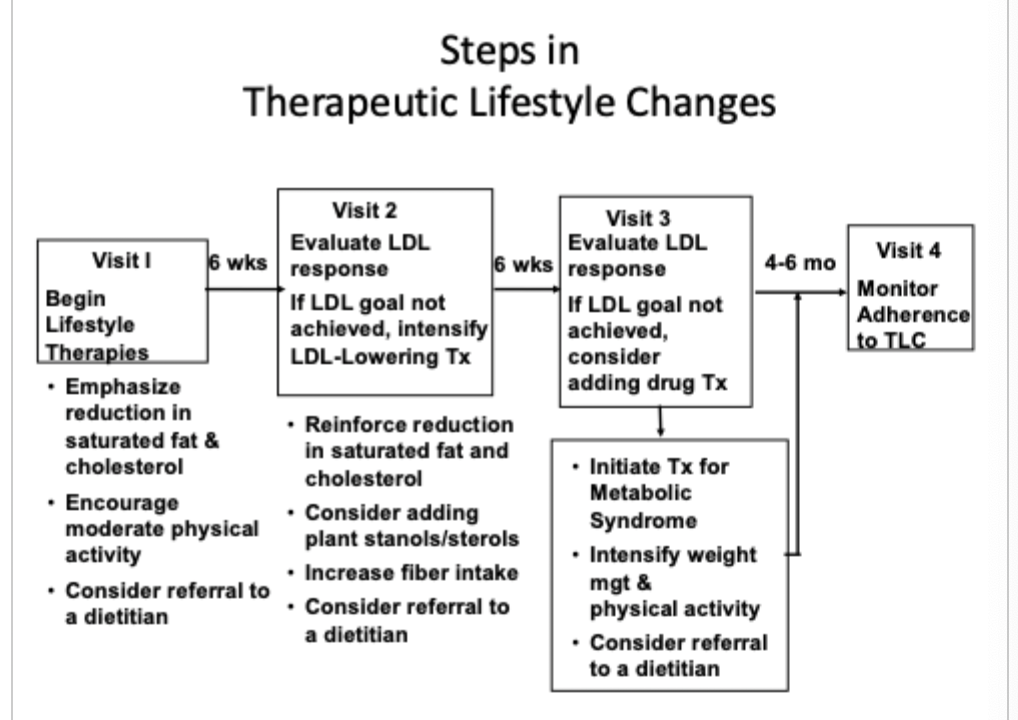
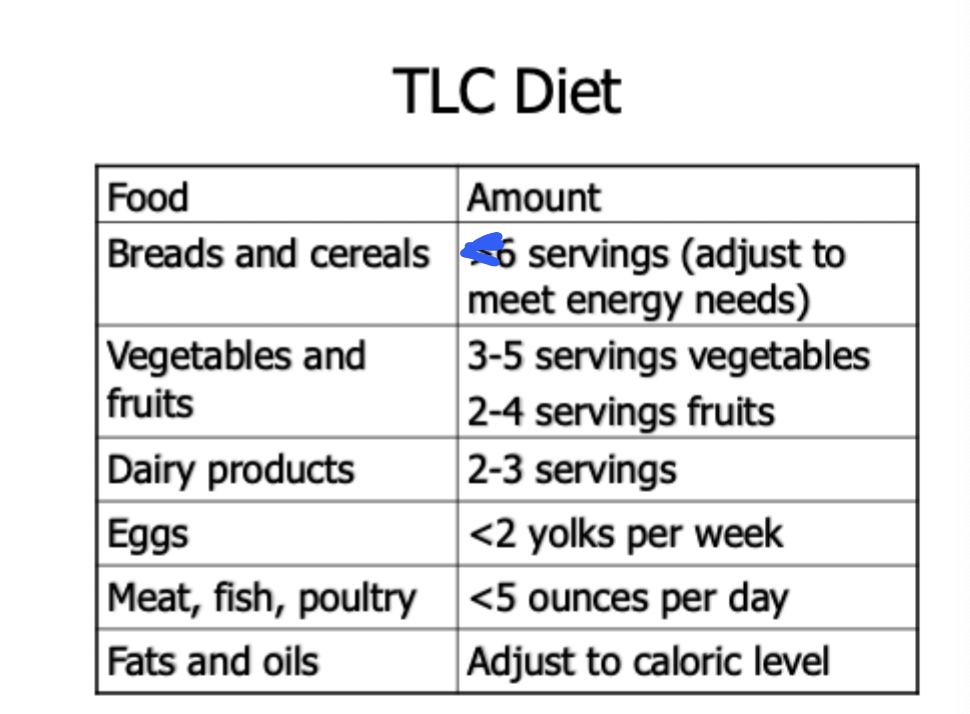
Therapeutic lifestyle changes (TLC) Diet
Sat fat - less than 7% of calories
Polyunsat fat - Up to 10% of calories
Monounsat fat - Up to 20% of calories
Total fat - 25-35% of calories
Carb - 50-60% of calories
Fiber - 20-30 g/day
Protein - 15% of total calories
Cholesterol - 200 mg/day
Total calories - balance energy intake and expenditure
Obesity (BOTH PARTS)
Prevalence in the US
Approaching epidemic proportion
No state has an adult prevalence less than 20%
Especially prevalent in Non-Hispanic Blacks (38.1%) and Hispanics (31.9%)
Weight management programs for adults have been unsuccessful (if they are successful its usually the short term)
Impact of Obesity
Rise in prevalence means rise in associated heath issues and the health care cost associated with these issues.
190 Billy in 2010
Increases the risk of morbidity and mortality from a number of causes
BMI over 28 is associated with an 4-5x increase in risk for stroke, ischemic heart disease, type II DM
Varies with age and decreases after 50
Obesity is a chronic disease that is typically under treated and is associated with CVD, HTN, Type II DM, and dyslipidemias
Effective treatment reduces these risks
Current treatments are often insufficient but can be enhanced
Obesity as a Chronic Disease
A long-term condition for most peeps with a slow progression and often periods of weight stability/loss followed by relaspe.
Etiology involves genetics, environment, metabolic factors (RMR), behavioral issues - but is an imbalance of energy intake and expenditure that favors fat accumulation
poorly understood
Genetic component evidence includes animal models and twin studies
30-40% in most studies (but as high as 80%)
Lifestyle factors may explain the recent surge
Overconsumption core with decreased energy expenditure
Nutrition - like diets high in fat contribute to over-consumption
Physical Activity decline has accompanied the prevalence of obesity
Only 22% of US adults exercise regularly
May be due to decreased manual labor, increased use of labor saving devices, decreased leisure time
Environmental factors
America may be a “toxic environment” as the food is plentiful, energy dense, and good tasting (3700 Kcal of food energy is produced everyday)
Increases the risk of other chronic conditions in a dose-dependent manner (more obese = more risk)
Management of obesity in this way impacts treatment modality
Lifestyle mods combined with pharm therapy PRN or Surgery (extreme)
Public Health
The WHO says obesity is an escalating epidemic and is one of the greatest neglected issues of our time.
May be as bad as smoking was
Prevalence has increased by 40%+ in the last 10 years (in ALL groups)
33% in the general population
African American (57%) and Hispanic Women (47%)
70% in 45-55 y/o
Prevalence is moving in the wrong direction
17% of teens/kids are obese
Consumption has risen steadily despite the recent decline in calories from fat
Comorbidities - star
CVD
Obesity correlates with a risk because of its association with dyslipidemias, HTN, and type II DM.
Appears to be a strong independent risk factor
An NHS study found that BMI is associated with CVD in a dose related response
The USMHPS found that elevated BMI was strongly associated with increased risk of CVD after controlling for other factors
The Framingham study found that obesity was a strong independent predictor of CVD in both men and women
HTN
Tons of studies have demonstrated a direct association between weight and BP
1/3 of all cases can be related to obesity
Obesity increases the risk of HTN 2-4x
The proposed theory is the there is elevated CO, reduced venous compliance and renal Na+ retention (from the hyperinsulinemia)
Dyslipidemias
HDL declines and TGs increased with increased BMI in all groups
LDL and total cholesterol increased with increased BMI in younger groups
Etiologies remain unclear but the most widely accepted theory is that the high lipolytic nature triggers the alterations
Type II DM - star
Obesity correlates strongly with type II DM and glucose intolerance - like 80% of patients are considered obese
Multiple studies (NHS and USMHPS) found that BMI correlates with the risk of developing type II DM
Over 31 BMI in women → 40x (compared to 22 BMI) - BANG
Over 35 BMI in men → 40x (compared to 23 BMI)
Adult weight gain is also strongly correlated with the risk of developing type II DM (as little as 20 lbs)
Other
Gallstones are 3-4x more frequent
Can lead to OSA and obesity hypoventilation syndrome
Associated with gout and osteoarthritis
Elevates the risk of hormone related cancers like breast and prostate
Abdominal Obesity as a Risk Factor
AKA visceral or truncal obesity
May be an independent risk for CVD and Type II DM
Strongly associated with glucose intolerance and dyslipidemias
Mechanisms not fully understood - here are the theories
elevated abd fat contributes to insulin resistance and hyperinsulinemia which cascade to other abnormalities
Also associated with hepatic dysfunction → increased gluconeogenesis
Weight Loss
Even 5-10% of body weight lost contributes to lower the risk for comorbidities
Improves glucose tolerance and type II DM
Only newly diagnosed peeps
Long term DM may respond more slowly
Weight loss has been shown to lower bp (independent of Na+ restriction)
Has been recommended as a primary therapy
Effects on dyslipidemias are less consistent
confounders include: composition of diet, satty fat, level of exercise, fitness level, energy balance
BUT moderate weight loss has be shown to have beneficial effects
reduced LDL and TGs
If the weight loss is due to diet AND exercise - then we drop total cholesterol and raise HDL
Assessment - STAR
Get adequate baseline information
Not just weight - get BMI and waist circumference
BMI = kg/height (meters)
The accepted estimate of body fatness and health risk - out of date as hell
Overweight: 25-29.99
NHANES recommendations
Men are obese at 27.8
Women are obese at 27.3
Obesity: 30-39.9
Correlates with very high risk of DM in me
Extreme obesity: 40+
The values represent 124% of “desirable weight for men” and 120% of “desirable weight for women” - 1983 tables take with grain of salt
Waist Circumference (waist to hip ratio)
Recent data suggest this may be better to estimate central adiposity
Correlates strongly with type II DM, CVD, HTN, and dyslipidemia risk
35” in women
40” in men
Treatment Plan
2 pronged approach - treat acute condition (recent weight gain with comorbidities) and manage chronic condition (period of stable weight and health)
Primary treatment is dietary intervention that restricts total energy intake using nutrient dense foods
Goals of treatment
reduce excess body fat
decrease severity of comorbidities
establish life long changes
The Team
PCP and registered dietician are key members
PCP must be willing to ask for help and respect others
coordinate overall medical care
evaluate changes in meds, labs, and other assessments
Dietician must understand the medical side of obesity
Track energy intake
make adjustments in the diet
They gotta communicate at least once a month
Diet
Needs to have a positive connotation
Healthy eating should be viewed as a lifelong process
In the acute stage → this is the medicine (reduce symptoms)
In the chronic stage → this is apart of the changes we make for stability
Target must be modest → 5-10% of body weight
get here then adjust based on patient goals
Weight loss - Reduced energy content but still needs all the nutrients
Never should be less than 800 kcal/day
After the 1st week (when you lose all the water weight) weight loss should be modest (1% at max/week)
Weight maintenance - adequate in energy and all nutrients
BOTH need the protein, vitamins, and minerals
Success factors
Adjunctive therapy (CBT) may enhance the dietary interventions since behavioral modifications and nutritional counseling are more effective
Medications can also increase the effectiveness of dietary interventions BUT are not a substitute for behavioral therapy
better than diet alone in promoting weight loss
and when added to CBT the behavioral modifications are better
However, when the meds are removed, you may see relapse
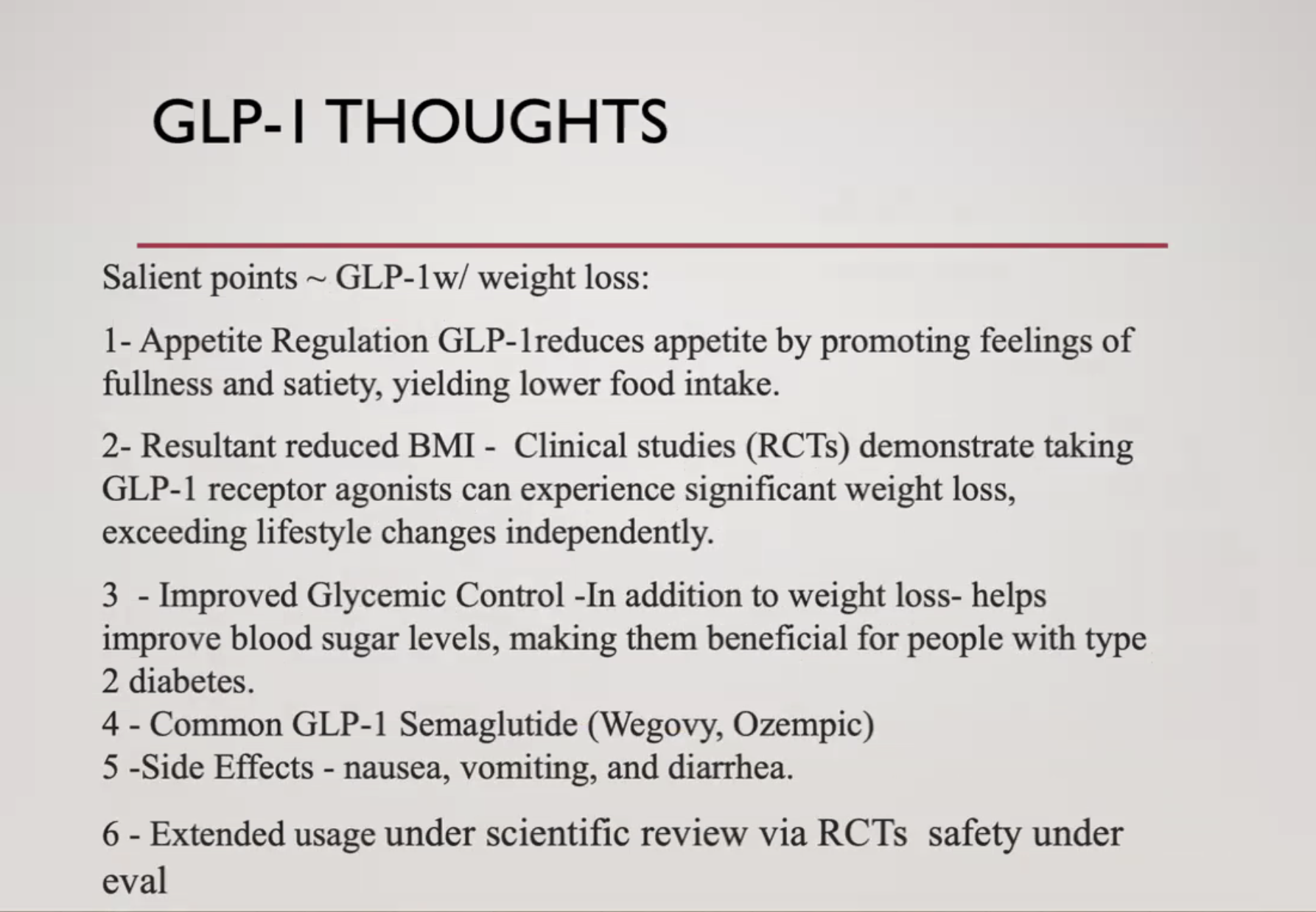
Safety of the patient becomes a concern because can they really take ozempic forever
EXERCISE
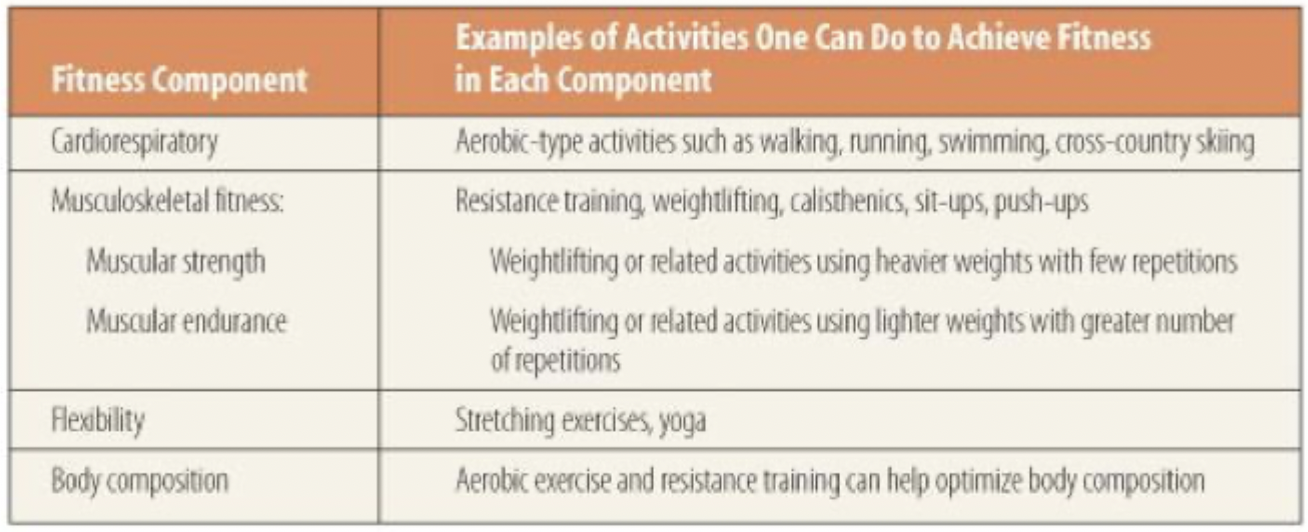
Physical Fitness star
Physical fitness: a state of being created by the interaction between nutrition and physical activity
Includes:
Cardiopulmonary fitness
MSK fitness
Flexibility
Optimal Body composition
Physical Activity star
Physical activity: muscle movement that increases energy expenditure
Leisure time physical activity: activity unrelated to person’s occupation
hiking, biking
includes exercise (purposeful, planned physical activity)
Benefits
Reduces the risk of:
Heart disease, stroke, HTN
obesity
Type II DM and metabolic syndrome
osteoporosis
certain cancers
improves mental health and mood
improves ability to perform ADLs
falls
increases the changes of living longer
Despite the benefits less than 50% of the US preform the recommended amount of physical activity
¼ of US adults admit to no leisure time physical activity
30% of high school studies participate in at least 60 min per day (data suggest this number is increasing)
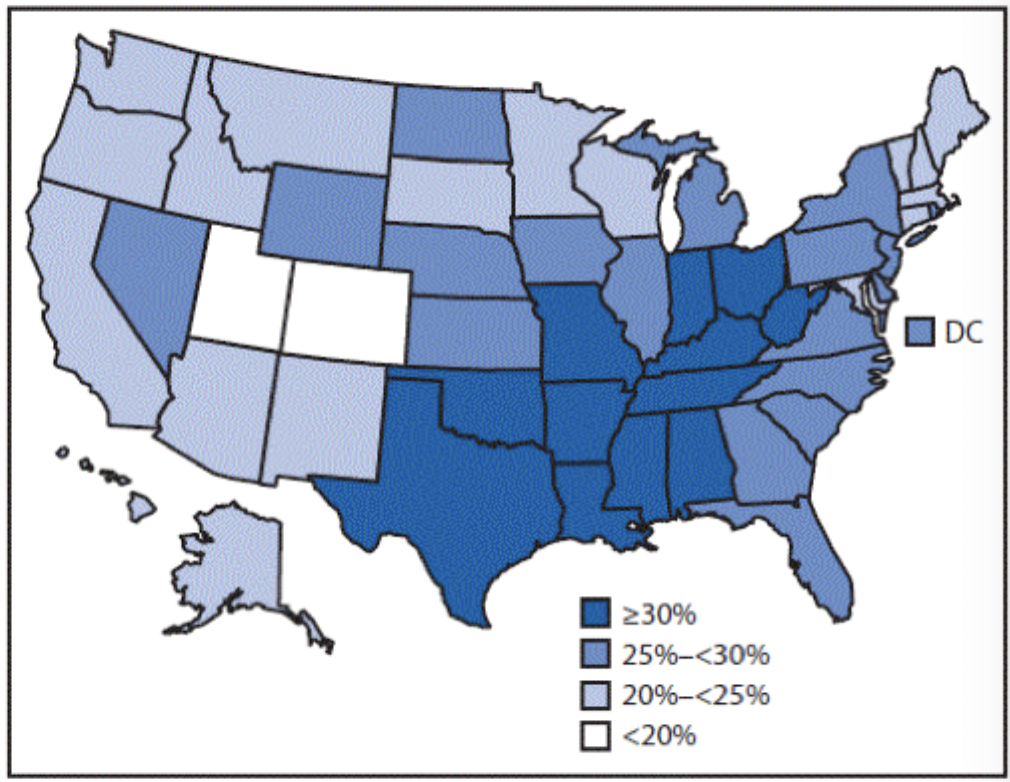
Rates of Physical Activity
Vary state by state → lower in southern states
highest in western states
Lowest in non-hispanic black adults, highest in white adults
Lower in women
Lower in older adults
Lower in those with less education
Lower in those living at the poverty level
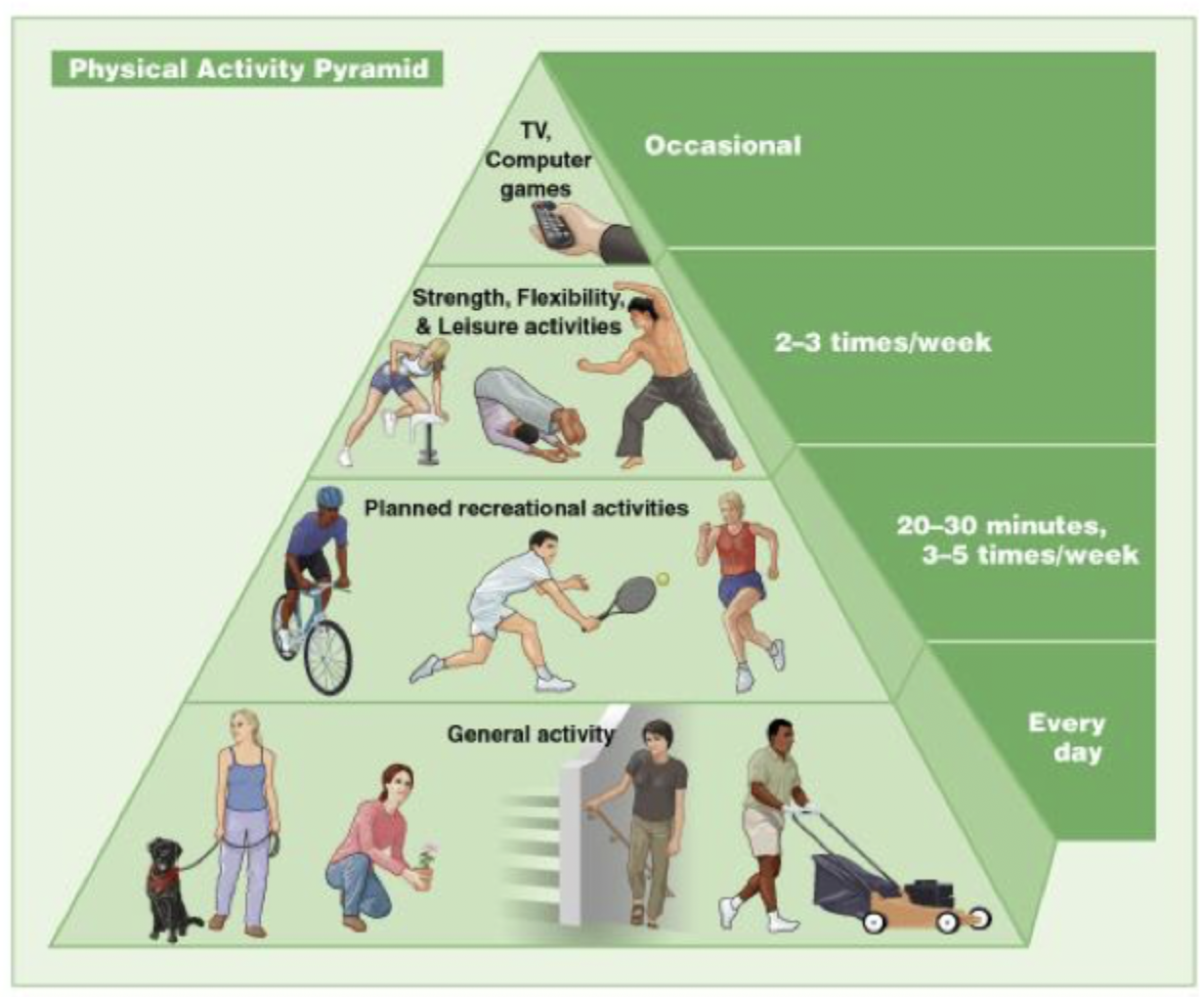
Recommendations
Children and teens should get at least 60 minutes a day
muscle strengthening 3x/week
Bone strengthening 3x/week
Adults need 150 minutes/week of moderate intensity exercise every week
2 or more days of muscle-strengthening
Fitness Program
A sound fitness program includes
Meeting personal goals
These will be different for everybody but most include maintaining/improving overall health, improving physical fitness, training for competitions
engaging
variety and consistency
Helps prevent boredome
appropriately overloads
warm up and cool down
Principles of Health Risk Assessments (HRA)
Health Risk: the severity or likelihood of an adverse health outcome due to an exposure to environmental, biological, or social conditions
Health risk appraisal: refers only to the INSTRUMENTS used to assess health risk
Health risk assessment: refers to the overall process in which the health risk appraisal instruments are used
HRAs can be uses as cost-effective tools for improving health at primary, secondary, and tertiary stages of health if utilized appropriately
Saves healthcare dollars
If used poorly - may waste resources and discourage users
Using HRAs
Provides a baseline to track health improvements in a population
Identify behavioral and environmental health risks individuals
Reduce healthcare cost
Foster a healthy QOL culture
Tracking Health Improvements
Like what percentage of your population smokes, consumes heavy amounts of EtOH, or are overweight/obese.
Also looks at diagnoses like DM, HTN, or mental healthy
Looks at diet and physical activity trends
Looks at dangerous habits → texting while driving
Identifying Risks (behavioral and environmental)
Examples: obesity, excessive worksite stress, not wearing a seat belt, unprotected sex, EtOH in excess, illicit drugs, prescription abuse, etc.
Reduce Healthcare Costs
Disease avoidance or delay
Avoiding - DUI, worksite accidents, DV, obesity, cancers
Delay - heart disease, stroke, diabetes, bone loss
Move high risk individuals into a lower risk category
Engage and empower the healthcare consumer as a manager of their own health
Always try to address underlying determinants of health
Tailor approaches to each individual’s unique environment and circumstances
Using shared decision making
Transfer day-to-day responsibility for personal healthcare management
emphasize communication and education
Fostering a Healthy QOL Culture
Normalize healthy behavior
Skill building
Changing attitudes
Social marketing
Incentives
Promoting Healthy Environments
Healthy eating options
Designed physical activity
Integrate a community activity program
Offer employee assistance programs for mental health and substance abuse
Planning Intervention and evaluations
Implement interventions based in part on HRA
Establish timelines
Collect data
Analyze data
Report the data
Types of HRAs
Lifestyle Assessments
Eating behavior
Stress management
Fitness assessment
Work style
Disease or Condition Specific
Pain
Menopause
Depression
PTSD
Insomnia
Skin Cancer
Heart Disease
Osteoporosis
Alcohol Use disorders
Uses the AUDIT
Age Based Assessment
Adolescents
Young Adults
Older adults
Seniors
Goals include
Reduce risk for diabetes, heart disease, stroke, cancer
Avoid falls and other injuries
Live longer on your own
Maintain rewarding social activities
Preventing depression
Gender Based Assessments
Cancers
Bone density loss
Depression
STDs
Environmental Risk Assessments
Safety
Lead Contamination
Sports safety
Hurricane preparedness
Depleted uranium exposure
asthams triggers
Dos and Don’ts
Do use them to be more efficient and effective
Do select the right tool
Do realized advantages and limitations
Don’t assume HRA equals clinical eval
Don’t neglect the ethics
Tobacco
Epidemiology
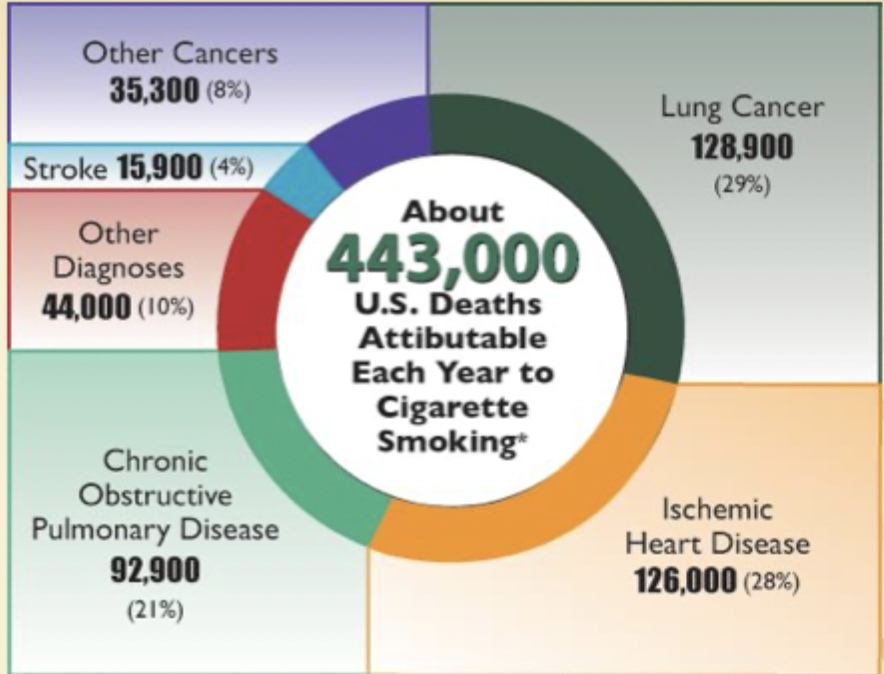
50% of smokers die from smoking related complications
440,000+ premature deaths (20% of all deaths)
Health care cost associated with smoking account for 170 billion dollars and adult productivity losses account for another 156 billion
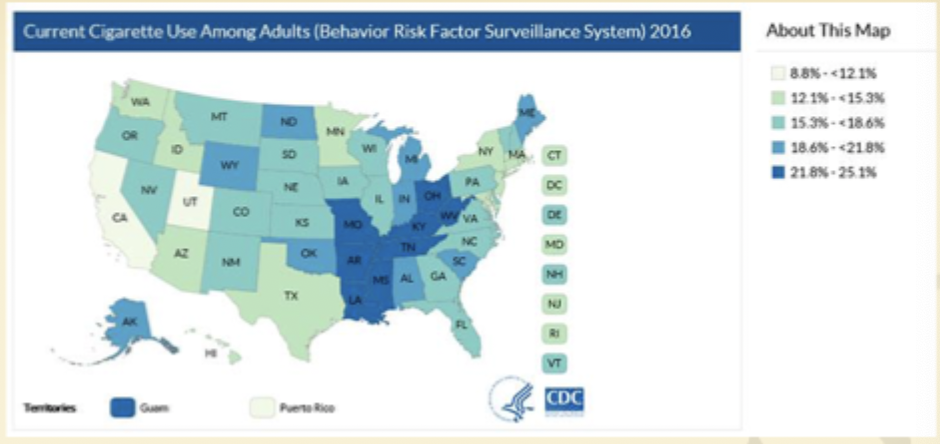
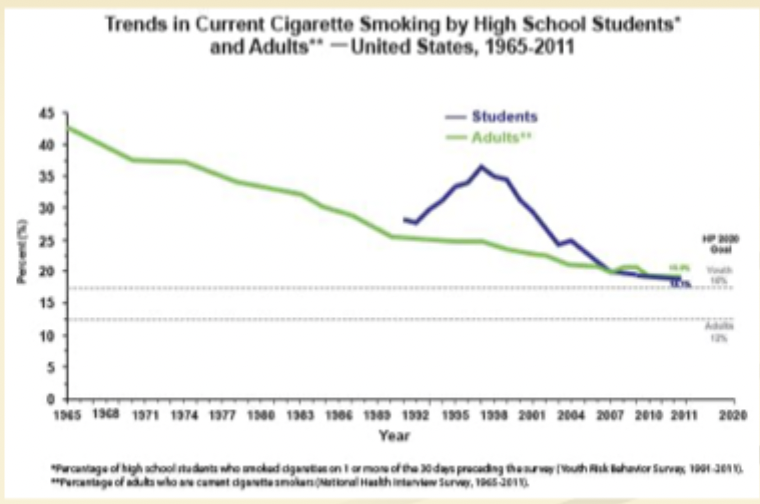
~16% of the US population smokes
8% of high school students smoker
2000 become regulars every time
Most adult smokers tried their first cigarette before 18
7% of women smoke during pregnancy
Cigarette Pricing
Average price of a pack of 20 ranged from $5.12-10.66
A 10% increase has reduced overall consumption 3-5%
Youth and Young adults are more likely to respond to the increase in prices
Quitting
Life-span averages
Years of increased life span after quitting - NEVER to late
If you quit by 30, 10 year increase
40, 8
50, 6
60, 3-4
Why people smoke?
Nicotine is highly addictive.
Effects depends on how much drug reaches brain and rate of change at receptors
euphoria
Lipid soluble and reaches the brain quickly (10-20 sec after inhalation)
Pavlovian Response
Why is it hard to quit?
Withdrawal Symptoms
Most develop within first 3 days; peak 3 days to 1 week, 1-2 weeks to wane
Dysphoria/depressed mood
Insomnia
Irritability, frustration, or anger
Anxiety
Difficulty concentrating
Restlessness
Decreased heart rate
Increased appetite/weight gain
Cravings
Likened to grief response
Long-term concern
occur within several days
Decrease in frequency, but not in intensity
Can occur years after quitting
associated with cued behavior
Interventions
5A’s - STAT
Ask
Every patient, every visit, every H&P
Include in vital signs
Congratulate never smokers, encourage former smokers, advise current to quit
Advise
even brief advice
Consistent implementation
Clear, strong, personalized
Patients reports importance of clinician advice
Assess willingness to quit
Assist those are willing to quit
Arrange for follow up
Schedule follow-up contact to provide support
smoking is a chronic disease so treat it like one
Stages of Change
Precontemplation: not interested in quitting, 30%
Education and persistent advice
Contemplation: interested but not ready
Ask patient what they like about smoking
Debunk pros
Emphasize cons
discuss smoking at every visit
Preparation: taking steps towards quitting
Action: begins the 1st day of smoking cessation; requires maintenance, or relapse will occur
Maintenance
Motivational Interviewing (5Rs)
Relevance - patient identifies personal relevance of smoking cessation
Rise - educate patient, emphasizing smoking-related cessation
Rewards - educate patient about benefits of smoking cessation
Roadblock - identify potential barriers to quitting
Repetition - follow up at each visit
Patient’s Prep for Quitting
Set a date
Tell everybody
Anticipate challenges
Remove the tobacco products
Support - social, meds, quit lines
Medications - STAR
1st line
nicotine delivery systems
Is effective
8-12 weeks of treatment
Provides steady nicotine levels to eliminate withdrawal and reinforcing “hits”
Patch, gum, lozenge, inhaler, nasal spray
For patch
10 cigs/day → highest dose then lower
Contact derm
For Gum:
less than 25 cigs - 2 mg
greater than 25 - 4 mg
Chew q 1-2 hr 1st 6 weeks then taper
For Nasal Spray
2-4 sprays/hr, up to 80 sprays/day
For inhaler
Puff or inhale deeply for up to 20 mins, 6-16 cartridges/day for 3-6 weeks then taper
Bupropion
Exact mechanism not known
Mesolimbic reward system
Dosed 150 mg/day → the twice a day
C/I in peeps with seizure or eating disorder
Caution in psychiatric patients already on antidepressant
Typically taken for 7-12 weeks (up to 6 months)
Varenicline
Partial agonist of nicotinic Ach receptors
Competes with nicotine for receptors
with better affinity
ADRs - Nausea most common
Be on alert for psychiatric effects
2nd line - modest effect
Clonidine
Nortriptyline
Lab Screenings for Public Health
To test or not to test that is the question
Healthy and 40-60 → EKG or stress test (ER VISITS DO NOT COUNT)
low risk for heart disease could be 10x more likely to a false positive
Could lead to an uncessary cath
approximately 39% of asymptomatic have had an EKG despite this
Males over 40 → PSA
If there’s no symptoms there’s no benefit
75% of tests that reveal a high PSA level turn out to be false alarm
False postive leads to stupid unneeded stuff
CONSIDER 55-69 y/o
Don’t test if they are going to die in 10 years
If you have a memory issue → PET
This is radioactive
Find the beta-amyloid protein in 30-40% of people who are asymptomatic
Unable to predict which individuals with plaques will develop the disease
All adult women → Pap smear
Only needed every 3 years
With 1 negative HPV test → only HPV test every 5 years
Over 65 y/o with normal pap smears → you can discontinue testing
Women 50-65 → DEXA (osteopenia, osteoporosis)
Mild osteopenia may not be cost effective
risk of fracture is low and the risk for significant side effects
no evidence that the medications provide much benefit
Over 75 → colonoscopy
Peeps with normal risk should begin screening at 50 and repeat every 10 years
If normal at 75 → never again
All adults → annual checkup
Little evidence that annual check up keeps people healthy
Results of specific tests should be used to determine frequency
Lower back pain →Xray, CT, MRI
Best imaging technology in the world is often inadequate at determining te cause of back pain
Most will go away in a month
imaging tests often leads to expensive procedures
Food-Borne Illness
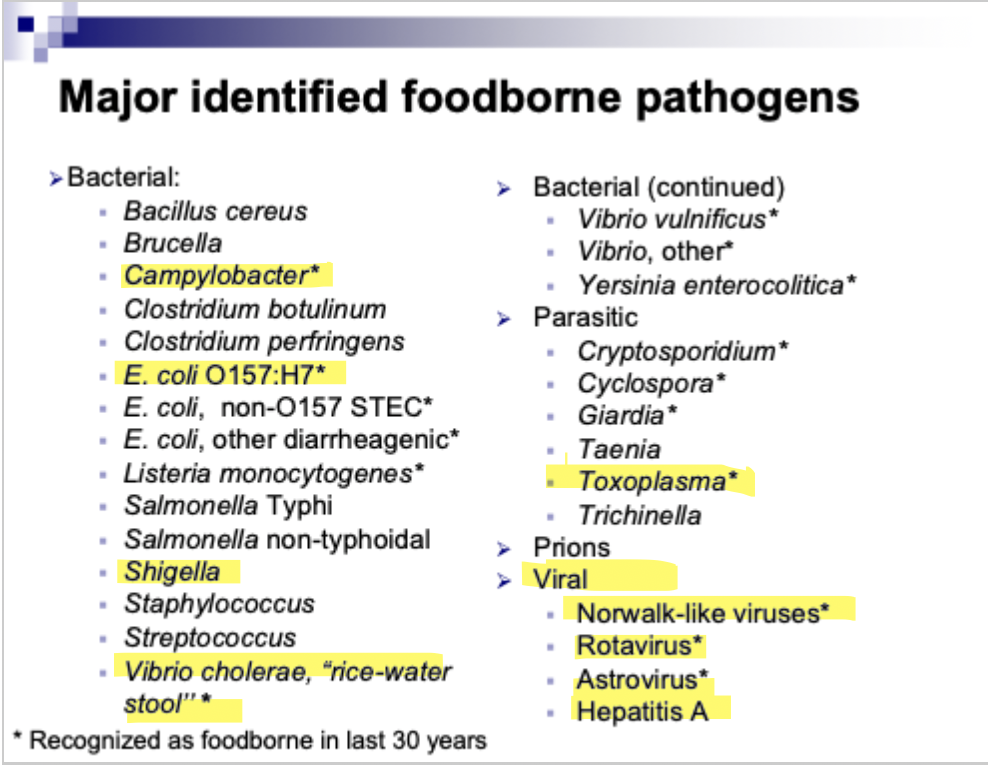
Population
Pregnancy technically means you are immunocompromised
Listeria and Toxoplasmosis → specific disease outcomes
Yersenia, Shigella, E.coli have specific implications in young children and can be prevented
Elderly is also at risk
Recent increases in infections due to contaminated produce might shift the focus of food safety educations
Strict adherence to proper food handling techniques and attention to food safety may reduce the morbidity and mortality due to foodborne illness
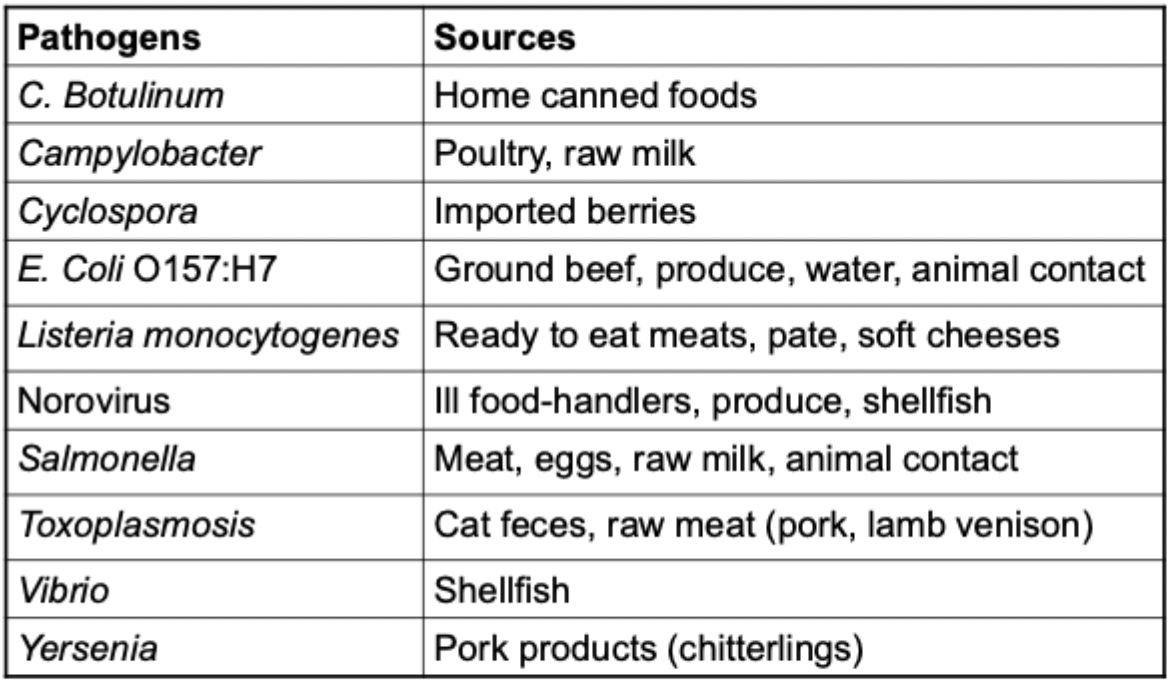
Salmonella
Bacterial illness characterized by diarrhea, abdominal cramps, tenderness, N/V, and fever.
There may be asymptomatic
Fecal-oral transmission, ingestion of contaminated food, contact with infected animals
Incubates in 8-12 hrs post consumption; 12-36 hours
Infectious throughout course; temporary carrier state for months (especially in infants)
There’s typhoidal and non-typhoidal - over 2000 serotypes
Enteritidis (contaminated egg products)
Newport (Beef, animal contact)
Typhimurium (bovine, poulty)
Treatment:IV fluids, FQs (adults), azithro (children)
Prevention: sanitation, personal hygiene, sewage treatment, infected individuals should not be handling food or working in health care while sick.
Restrictions on selling turtles or reptiles
All amphibians and reptiles are carriers
Cause ~74,000 infections/yr
Cook your food all the way
In the population
No specific risk for pregnant patients
Children are at an increased risk
Wild animals and domestic exposure also increases risk
Shigella
Bacterial illness of varying severity in which patients present with diarrhea, fever, nausea, abd cramps, and tenesmus
Transmitted by ingestion of contaminated food or water, fecal oral
Secondary household, school, and daycare cases are common
easily spread
Incubates for 1-7 days
Infectious through the acute period and until agent is not in the feces (4 weeks)
Treat with fluids and azithromycin
Prevention: sanitation, hygiene, hand washing in kids
In the population
No risk to pregnant women (except geriatric)
Children are at risk due to immature immune systems and frequent hand-mouth contact
Prompt infection control is required in daycare settings
Proper food handling techniques reduce incidents
Washing your hands
Campylobacter
Illness characterized by diarrhea, cramp, malaise, fever, nausea, vomitting
Usually carried (reservior) by animals (cattle, poultry)
Transmission: ingestion of undercooked meat, contaminated food or water, contact with infected animals
Incubates for 2-5 days on average
Infectious throughout course of infection (2-5 days on average)
Untreated may shed the virus in their stool for 7 weeks
Treatment: Fluids, azithromycin/ciprofloxacin
Prevention: proper food handling techniques, consumption of potable water
In the Population
No specific risk to pregnant women - except for geriatric
Children are at risk due to immature immune systems and frequent hand-mouth contact
Most common cause of bacterial gastroenteritis in the US
Disproportionately high burden in infants less than 1 year, with over twice the disease incidence of healthy adults
E. Coli (O157:H7 - STEC)
Shiga toxin producing E.coli (STEC) produces an illness characterized by diarrhea (often bloody) and cramps
Asymptomatic infections may occur
Number 1 cause of traveler’s diarrhea
May result in Hemolytic Uremic Syndrome (HUS) → usually in some children
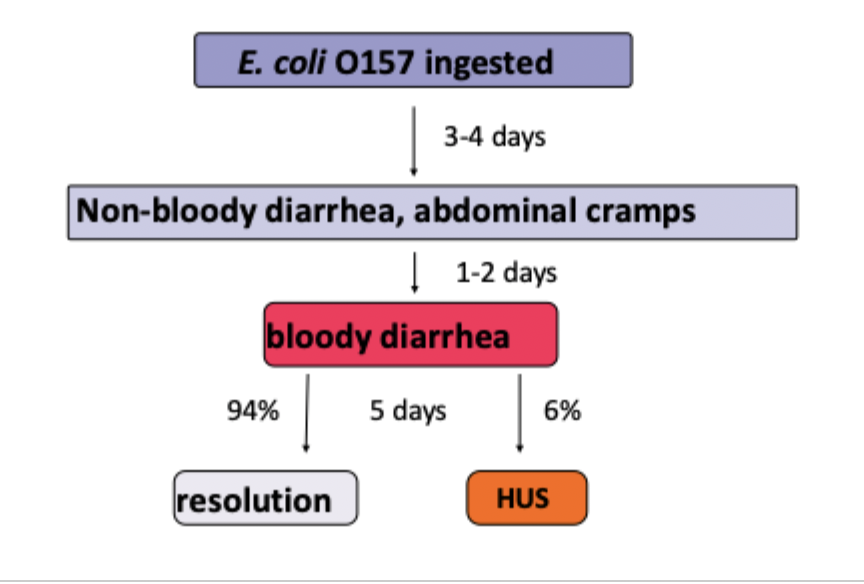
Cattle and deer act as reservoirs; humans can as well for human-human transfer
Transmitted by ingestion of contaminated food or water, contact with infected animals, or through person-person
Incubation: 2-8 days
Treatment: FQs and azithromycin
Prevention: better sanitation, adequate personal hygiene, avoid consumption of undercooked ground beef AND unpasteurized dairy and fruit juice products
Listeria Monocytogenes
Illness characterized by fever, muscle aches, stiff neck, HA, and sometimes nausea or diarrhea
Asymptomatic cases are common
Infection can lead to many clinical syndrome including stillbirth, listeriosis of a newborn, meningitis, bacteriemia, localized infections
Reservoir: soil, forage, water, mud, silage, infected animals, foul, and humans
Transmission: ingestion of contaminated food such as unpasteurized dairy, ready-to-eat-meats, raw veggies, smoked fish, fermented raw meets
Can grow and multiply at refrigeration and temperature
Incubated: 3 weeks
Treatment: Ampicllin, gentamicin
In the Population
Pregnant women are at a 20% increased risk
Newborns suffer the serious health effects like → septic abortion, stillbirth, neonatal sepsis/meningitis
Most diagnosis are made in the 3rd trimester
Theory is that most fetal deaths in the 1st and some in the 2nd are though to be due to routing causes of miscarriage and there is no testing for listeria
Incidence is highest among the hispanic population particularly in infants and women of child-bearing age
12x higher incidence
13x then non-hispanic women in the same age group
Prevention strategies should target here
General Recommendations
Thoroughly cook raw foods from animal sources
Separate raw meat from veggies and cook/ready to eat foods
Wash hands, knives, and cutting boards
Wash uncooked veggies
Do not drink raw milk → duuh
Refrigerate perishable items at 40 F or below and consume as soon as possible
Toxoplasmosis
Illness caused by a PARASITE toxoplasma gondii
Infections generally mild and symptoms may include malaise, fever, fatigue, and lymphadenopathy
Many are asymptomatic
Rare in immunocompromised peeps
Reservoir: cats, felines, intermediate hosts include swine, cattle, sheep, goats, rodents, and birds
Transmission - 3 ways
ingestion of uncooked meat
Ingestion of oocysts passed in feline feces through contact with litter or soil
Vertical transmission
Incubation: average 7 days (4-23 days)
Hep A
Acute, viral infections with fever, fatigue, malaise, loss of appetite, nausea, abdominal pain, dark urine, and jaundice
Severity of disease varies, asymptomatic are possible
Reservoir: Humans
Transmission: primarily foodborne, sexual transmission, bloodborne
Highly infectious
Incubation: 28-30 days
Treatment: thug it out
In the population
No risk to pregnant women except for geriatric
Children are an increased risk of infection due to immature immune system and frequent hand-mouth
Severity of infection generally increases with age
Children rarely have symptoms → but they are infectious
Disease is most common among school age children and young adults
Hep A is not a C/I indication for breast feeding
Perinatal transmission is rare
In the US, sporadic transmission of Hep A is frequent in daycare centers with diapered children
A vaccine is available
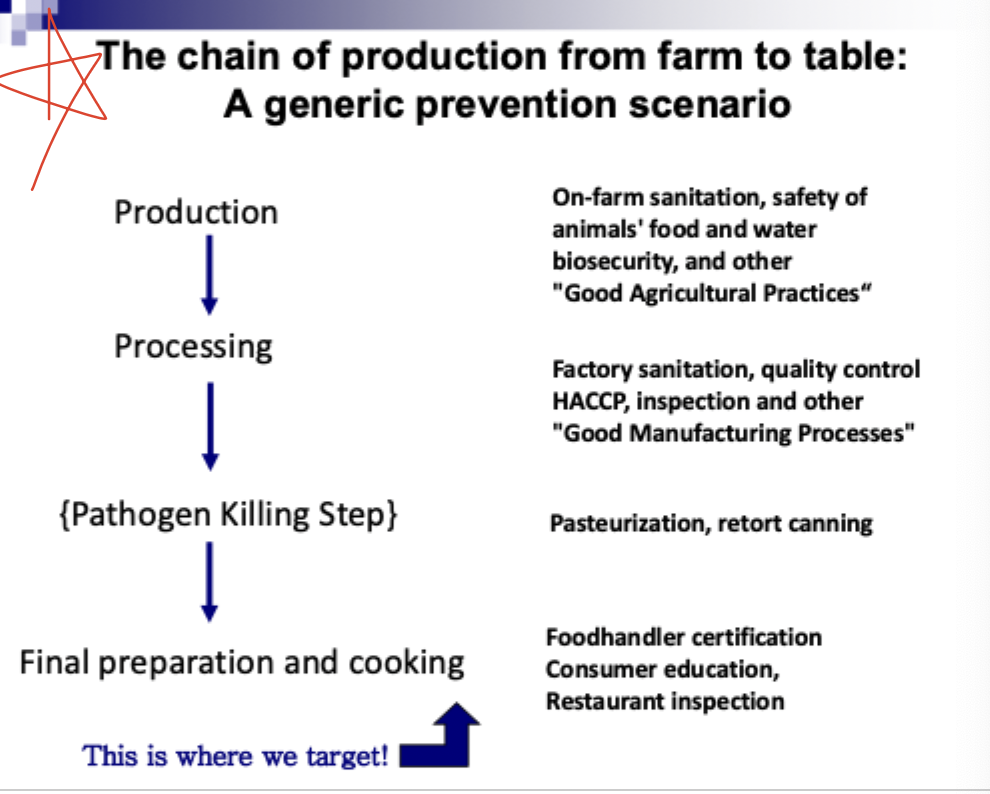
Preventing Food Borne Illness
There’s no vaccine for most pathogens
Educate consumers, food handlers, and producers
Contamination of food products can occur any where along the chain
Prevent disease through targeted strategies
Educational campaigns to certain pop
Surveillance - STAR
Many different diseases are caused by contaminated foods (250+)
For many of these, the source might be food, water, animal contact, or contact with ill people
For an individual case of illness, it is often impossible to know the source of the infection
Outbreaks let us learn specific course of infection
Individual cases are tracked regardless of whether or not they may be from food or other sources
Outbreaks of foodborne diseases, regardless of which microbes caused them (source-specific surveillance)
Food Safety
Food safety is complex and requires a multifaceted approach to ensure success
CLEAN
wash hands and surfaces often
Wash hands for 20 secs
Wash cutting boards, knives, utensils, and counter tops
Use plastic and non-porous cutting boards
SEPARATE
Don’t cross contaminate
Separate raw meat, poultry, and seafood and store these on the body shelf
COOK
Use a meat thermometer
Cook roast and steaks to 145
Cook whole poultry to 180
Cook ground meat to 160
Cook eggs until opaque and firm
Cook fish until its opaque and flakes
Heat leftovers to 165
CHILL
Refrigerate properly and promptly
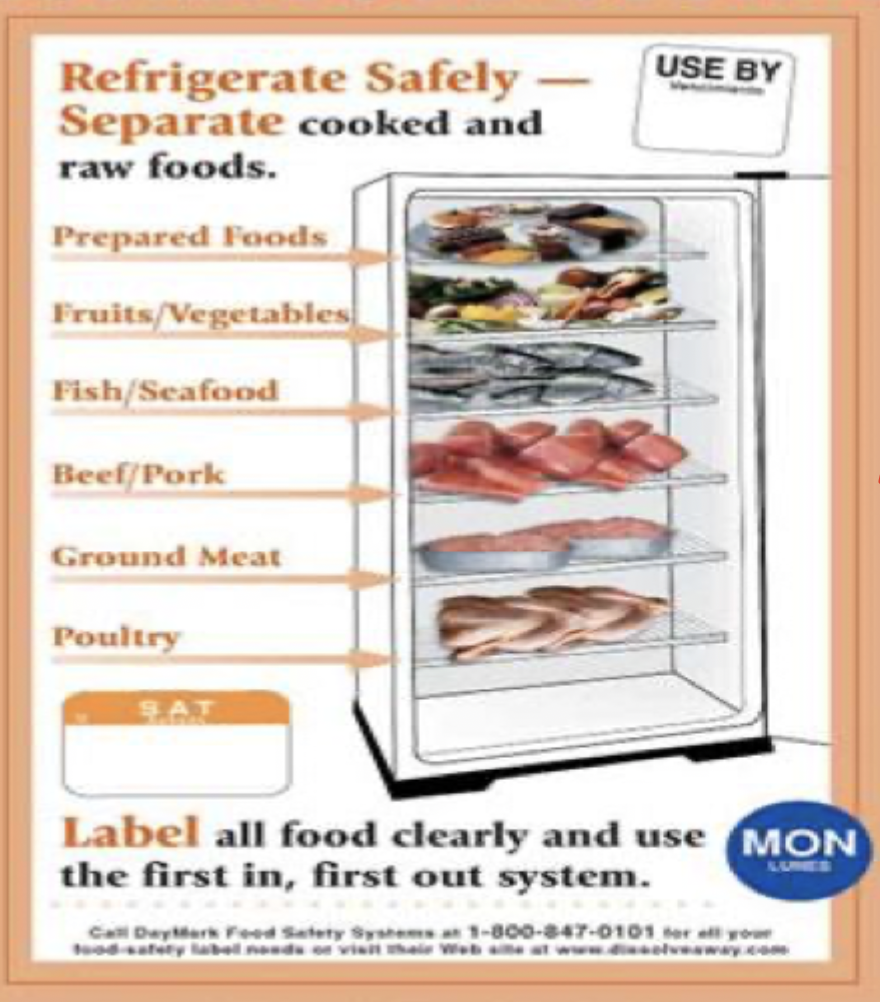
At 40 degrees or lower - one of the most effective ways to reduce risk
Microorgs grow at higher temps
Use a thermometer to monitor the temp
Refrigerate things within 2 hours of purchase/use
Never defrost at room temp
Thaw in refrigerator or submerge in water
Separate large amounts of leftovers so that they cool quicker
Don’t stuff the fridge