
Chapter 31 (pages 638-671) - Asthma, COPD
1. Describe the pathophysiology, clinical manifestations, and interprofessional and nursing management of the patient with bronchiectasis.
2. Describe the pathophysiology, clinical manifestations, and interprofessional and nursing management of the patient with cystic fibrosis.
3. Describe the etiology, pathophysiology, and clinical manifestations of asthma.
4. Explain the difference between an acute asthma exacerbation and status asthmaticus.
5. Describe the interprofessional care and nursing management of the patient with asthma.
6. Identify the classes of drugs used in the treatment of asthma and chronic obstructive pulmonary disease (COPD).
7. Describe the etiology, pathophysiology, clinical manifestations, and interprofessional care of the patient with COPD.
8. Explain the nursing management of the patient with COPD
α1-antitrypsin deficiency (AATD)
autosomal recessive disorder that may eventually affect the lungs and liver
asthma
Asthma is a diverse disease characterized by bronchial hyperreactivity with reversible expiratory airflow limitation, either spontaneously or with treatment.
signs + symptoms variable
bronchiectasis
bronchioles are dilated, making it hard to clear secretions. It most often results from poorly treated or untreated lung infections, immune system problems, or genetic factors. Bronchiectasis affects more than 500,000 people in the US.1 It is more common in women. It affects 1 in every 150 people over age 75
chronic bronchitis
presence of cough and sputum production for at least 3 months in each of 2 consecutive years.
chronic obstructive pulmonary disease (COPD)
progressive lung disease characterized by persistent airflow limitation. COPD is associated with an enhanced chronic inflammatory response in the airways and lungs. The main causes are cigarette smoking and other noxious particles and gases
cor pulmonale
Cor Pulmonale (Right-Sided Heart Failure) Cor pulmonale is an enlarged right ventricle in your heart that happens because of a lung condition.
cystic fibrosis (CF)
Cystic fibrosis (CF) is an inherited, autosomal recessive genetic disorder, characterized by altered transport of sodium and chloride ions in and out of epithelial cells. Airway obstruction occurs because of changes in exocrine glandular secretions, resulting in increased mucus production.
emphysema
destruction of alveoli without fibrosis, describes one of several structural abnormalities in COPD.
peak expiratory flow rate (PEFR)
measured by the peak flow meter (at home or in a health care setting) is a test of lung function. PEFR measures the maximum rate of airflow after a forceful exhalation. When monitored routinely, PEFR measurements can provide a baseline of the patient’s health status. PEFR can help predict an asthma attack or monitor the severity of disease.
status asthmaticu
most extreme form of an acute asthma attack. It is characterized by hypoxia, hypercapnia, and ARF. The patient is unresponsive to treatment with bronchodilators and corticosteroids.
Key Points
BRONCHIECTASIS Bronchiectasis is characterized by permanent, abnormal dilation of one or more large bronchi. The pathophysiologic changes that occur result in dilation of the airways and destruction of the elastic and muscular structures supporting the bronchial wall.
Clinical Manifestations and Complications
The hallmark of bronchiectasis is persistent or recurrent cough with production of large amounts of purulent sputum
In some situations, sputum production may exceed 500 mL/day.
Bacterial infection of the lungs, repeated aspiration, and several systemic diseases (e.g., diabetes, inflammatory bowel disease) are associated with increased risk.
Repeated exacerbations, pulmonary hypertension, and neovascularization (development of new blood vessels post-injury), can lead to hemoptysis
Diagnosis
CT is the gold standard for diagnosis of bronchiectasis
Management
Bronchiectasis is hard to treat. Therapy is aimed at treating acute exacerbations and preventing a decline in lung function.
Antibiotics are the mainstay of treatment. Long-term suppressive therapy with antibiotics is reserved for those patients who have symptoms that recur a few days after stopping antibiotics.
An important nursing goal is to promote drainage and removal of mucus from the lungs. Rest, good nutrition, adequate hydration, and patient education are important.
CYSTIC FIBROSIS
Cystic fibrosis (CF) is an autosomal recessive, multisystem disease characterized by altered function of the exocrine glands, producing airway obstruction and an increase in mucous production.
Eventually, CF progresses to a restrictive lung disease because of the fibrosis, lung destruction, and thoracic wall changes.
CF also involves the lungs, pancreas, and sweat glands.
Clinical Manifestations and Complications
Clinical manifestations vary depending on the severity of the disease.
In adults, a frequent cough, new-onset diabetes, and infertility problems are initial non-specific symptoms
Complications from CF can also vary widely, from cor pulmonale, pulmonary hypertension, CFRD, and sinus, bone, and liver disease.
Diagnosis
Is made with the “sweat test”
Management
Major goals of therapy in CF are to promote clearance of secretions, control infection in the lungs, and provide adequate nutrition.
Nursing care for the patient revolves around relieving airway obstruction, controlling infection, and promoting drainage of mucous from the patient’s lungs
Respiratory treatment may include bronchodilators, mucolytics, chest physiotherapy (postural drainage), and antibiotics.
Systemic management of the disease may include pancreatic enzyme replacement, prokinetic agents, and laxatives.
Psychosocial support and counselling for lifestyle adaptation, and, encouraging the patient to access community resources for information and support are important teaching points.
ASTHMA
Asthma is a chronic inflammatory disorder of the airways that results in recurrent episodes of airflow obstruction. It is usually reversible.
The main pathophysiologic process in asthma is persistent but variable inflammation of the airways. Airflow is limited because the inflammation results in bronchoconstriction, airway hyperresponsiveness (hyperreactivity), and edema of the airways.
Asthma is not a psychosomatic disease.
Clinical Manifestations and Complications
Although the exact mechanisms that cause asthma remain unknown, exposure to allergens or irritants initiates the inflammatory cascade.
The characteristic manifestations of asthma are wheezing, cough, dyspnea, and chest tightness, particularly at night or early in the morning. Expiration may be prolonged.
During an acute attack, the patient usually has signs of hypoxemia.
Risk factors and triggers for asthma and asthma attacks include nose and sinus problems, allergens, cigarette smoke, air pollutants, respiratory tract infections, exercise, occupational irritants, and GERD.
Genetics and one’s immune responses may influence asthma development.
A severe asthma attack, unresponsive to treatment, is known as status asthmaticus.
Severe acute asthma attacks and status asthmaticus may require intubation and mechanical ventilation.
Asthma can be classified as mild, moderate or severe, based upon current condition of the patient, including degree of respiratory difficulty and response to treatment.
Diagnosis
A diagnosis of asthma is usually made based upon the presence of various indicators
(e.g., clinical manifestations, health history, spirometry, peak flow variability).
Management
The goal of asthma treatment is to achieve and maintain control of the disease.
Asthma can be classified as mild, moderate or severe, based upon current condition of the patient, including degree of respiratory difficulty and response to treatment.
Once the patient is diagnosed, guidelines provide direction about medications (based on steps) the patient needs. The HCP will step up the medication therapy as asthma symptoms worsen, and step down the medication as the patient achieves control.
The level of control is determined by the patient's medication use, symptoms, and PEFR or FEV1.
Pharmacologic Management of Asthma
Asthma drugs may be classified as short term “rescue” medications (to treat symptoms during an acute attack) and long term “controller” medications (to achieve and maintain control of asthma after the acute episode has subsided).
All persons with asthma should always carry rescue medication.
Short-acting inhaled β2-adrenergic agonists (SABAs), including albuterol, are the most effective drugs for relieving acute bronchospasm. They are used for acute asthma attacks.
Long-acting inhaled β2-adrenergic agonists (LABAs), including salmeterol and formoterol, are never to be used alone due to an increased risk of death. They are safe when combined with ICS, such as fluticasone/salmeterol (Advair) or budesonide/formoterol (Symbicort).
Because chronic inflammation is a key component of asthma, inhaled corticosteroids are more effective in improving asthma control than any other long-term drug.
Leukotriene modifiers can be used in milder asthma successfully as add-on therapy to reduce the dose of inhaled corticosteroids.
The only anti-IgE drug, omalizumab (Xolair), is used for hard to treat moderate to severe asthma unable to be controlled by inhaled corticosteroids.
Methylxanthine (theophylline) preparations are no longer recommended for asthma, as thereare much newer drugs available with less severe side effects.
Anticholinergic agents are not used in asthma treatment, except for ipratropium (Atrovent), which is only used in the ED for acute attacks.
Other Management Priorities
The overall goals are that the patient with asthma will achieve asthma control, as evidenced by (1) minimal symptoms during the day and night, (2) acceptable activity levels (including exercise), (3) maintaining greater than 80% of personal best PEFR, (4) few or no adverse effects of therapy, (5) no acute attacks of asthma, and (6) adequate knowledge to carry out the plan of care.
Education is the cornerstone of asthma management. Your role in preventing asthma attacks or decreasing the severity in your patient focuses primarily on teaching the patient and caregiver.
One of the major factors determining success in asthma management is the correct administration of drugs.
Inhalation devices include metered-dose inhalers, dry powder inhalers, and nebulizers.
Teaching should include information about medications, including the name, purpose, dosage, method of administration, schedule, side effects, appropriate action if side effects occur, how to properly use and clean devices, and consequences for breathing if not taking medications as prescribed.
Several non-prescription combination drugs are available over the counter. An important teaching responsibility is to warn the patient about the dangers associated with non-prescription combination drugs.
One important goal in asthma care is to maximize the ability of the patient to safely manage acute asthma episodes through a written asthma action plan developed in conjunction with the HCP.
Written asthma action plans are shared with caregivers, especially for those patients with moderate or severe persistent asthma or a history of severe attacks.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease characterized by airflow limitation that is not fully reversible. It is almost always progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases, primarily caused by cigarette smoking.
COPD is characterized by chronic inflammation in the airways, lung parenchyma (respiratory bronchioles and alveoli), and pulmonary blood vessels.
The pathogenesis of COPD is complex and involves many mechanisms, with an inflammatory process different from that of asthma.
The defining features of COPD are not fully reversible airflow limitation during forced exhalation, caused by loss of elastic recoil and airflow obstruction from mucus hypersecretion, mucosal edema, and bronchospasm.
Gas exchange abnormalities can result in hypoxemia and hypercapnia.
COPD has systemic manifestations.
Clinical Manifestations and Complications
A chronic intermittent cough is the earliest symptom. As the disease progresses, the cough is present every day.
Sputum may or may not be produced. Symptoms are progressive.
Risk factors for developing COPD include smoking and cigarette smoke, occupational chemicals, air pollution, severe recurring respiratory infections, and α1-antitrypsin deficiency (an autosomal recessive disorder).
Complications may include exacerbations of COPD, signalled by a change in the patient’s usual dyspnea, cough, and/or sputum, that is different than the usual daily patterns. These flare-ups require changes in management and can have significant mortality if not appropriately treated.
Cor pulmonale is hypertrophy of the right side of the heart, with or without
heart failure, resulting from pulmonary hypertension and is a late manifestation of chronic pulmonary heart disease.
Patients with severe COPD who have exacerbations are at risk for the development of “acute on-chronic” respiratory failure.
Diagnosis
A diagnosis of COPD should be considered in any patient over the age of 40 with a smoking history of 10 or more pack years or who has symptoms of cough, sputum production, or dyspnea, and/or a history of exposure to risk factors for the disease.
The diagnosis of COPD is confirmed by spirometry.
COPD can be classified as mild, moderate, severe, and very severe.
An FEV1/FVC ratio of less than 70% establishes the diagnosis of COPD. The severity of obstruction (as indicated by FEV1) determines the stage of COPD.
Validated questionnaires such as the COPD Assessment Test (CAT) and Clinical COPD Questionnaire (CCQ) are recommended for a comprehensive assessment of symptoms.
Management
The main goals of care for the COPD patient are to: (1) relieve symptoms, (2) improve exercise tolerance to help facilitate ADLs, (3) avoid complications, (4) implement a long term treatment plan, (5) prevent progression of the disease, and (6) improve one’s overall quality of life.
Cessation of cigarette smoking in all stages of COPD is the intervention that can have the biggest impact to reduce the risk of developing COPD and influence the natural history of the disease.
Pharmacological Management of COPD
Although patients with COPD do not respond as dramatically as those with asthma to bronchodilator therapy, bronchodilator therapy can reduce the dyspnea and increase the FEV1.
Presently no drug modifies the decline of lung function in patients with COPD.
Inhaled anticholinergics or LABAs may be used or combined with inhaled corticosteroids.
Monotherapy with inhaled corticosteroids is not recommended due to the side effects.
Possible Surgical Options for COPD
Four different surgical procedures have been used in severe COPD, but not all COPD patients are considered candidates for the following procedures.
Lung volume reduction surgery (LVRS) reduces the size of the lungs by removing the most diseased lung tissue so that the remaining healthy lung tissue can perform better.
Bronchoscopic lung volume reduction surgery works by placing 1-way valves in the airways leading to the diseased parts of the lung. The valves let air out but not in. This collapses a certain segment of the lung and has a similar result as LVRS.
A bullectomy is used for certain patients and can result in improved lung function and reduction in dyspnea.
Lung transplantation can improve functional capacity and enhance quality of life in appropriately selected patients with very advanced COPD.
Other Management Priorities
O2 therapy is used in the treatment of COPD and many other problems associated with hypoxemia. Long-term O2 therapy may improve survival, exercise capacity, cognitive performance, and sleep in hypoxemic patients.
For most patients, the goal of O2 therapy is to keep the SaO2 greater than 90% during rest, sleep, and exertion, or, the PaO2 greater than 60 mm Hg. These goals may be modified for the patient with moderate to severe COPD.
Weight loss and malnutrition are common in the patient with severe COPD. The patient with weight loss needs extra protein and calories and tips on energy conservation while eating and preparing food.
Pursed-lip breathing is a technique that is used to prolong exhalation and thereby prevent bronchiolar collapse and air trapping.
Airway clearance techniques include effective coughing techniques, chest physiotherapy, and airway clearance devices. Airway clearance devices include those using positive airway pressure, such as Flutter. No one is better than the other, but it depends on patient preference.
Huff coughing is an effective technique that the patient can be easily taught. Effective coughing conserves energy, reduces fatigue, and promotes removal of secretions.Chest physiotherapy consists of percussion, vibration, and postural drainage.
Pulmonary rehabilitation should be considered for all patients with COPD or having functional limitations. The overall goal is to increase exercise capacity and improve the quality of life.
The patient with COPD will require acute care for complications, such as exacerbations, cor pulmonale, and acute respiratory failure.

1. Recognize: What manifestations show H.M. had a COPD exacerbation?
Increased dyspnea, increased work of breathing (at rest) and a change in the color, amount, or other characteristics of one’s sputum (e.g., becoming thick, purulent, when patient normally expectorates thin, clear secretions).
2. Analyze: What is the most likely cause of her exacerbation?
Smoking and air pollution exposure as a police officer.
3. Analyze: Why would H.M. “feel full fast” when eating? What could you do to address this issue?
Sensations of feeling full after consuming small amounts can be attributed to swallowing air while eating, side effects of medication (especially corticosteroids), and the abnormal position of the diaphragm relative to the stomach (in association with hyperinflation of the lungs).
4. Analyze: What symptoms indicate overuse of inhalers? Which drug would cause the symptoms described?
“Jitters” and “racing heart”; the Ventolin HFA would be the primary cause.
5. Analyze: Interpret the ABG on admission and 24 hours post-admission. In comparing both ABGs, do you see a pattern?
ABG in ED: Partially compensated respiratory acidosis:
pH: 7.34: low, thus acidosis (normal 7.35 to 7.45)
PaCO2: 59 mm Hg: high (normal 35 to 45 mm Hg), thus the cause of the acidosis
HCO3-: 27 mEq/L (normal 22 to 26 mEq/L): one point over normal, thus the kidneys are just beginning to compensate by conserving bicarbonate and trying to bring the pH to normal.
PaO2 68 mm Hg, she is hypoxemic (normal: 80 to 100 mmHg)
24 Hours after admission: pH: 7.30 (H.M.is becoming more acidotic)
PaCO2: 63 mmHg (increasing, indicating a worsening acidosis)
HCO3-: 29 (above normal, but not much change)
PaO2: 64 (continues to indicate hypoxemia).
This is described as an “acute-on-chronic” exacerbation, as evidenced by worsening acidosis and hypoxemia, and relatively little change in bicarbonate.
6. Prioritize: Based on the assessment data presented, what are the priority clinical problems?
Impaired respiratory system function, nutritionally compromised, activity intolerance, deficient knowledge, substance abuse (e.g., continued cigarette smoking)
7. Act: What is one suggestion you could make to H.M. that could halt the progression of her COPD?
stop smoking
8. Act: What should you include in her discharge planning and teaching?
Several important priorities for discharge teaching and planning must be considered before H.M. can return home. Most priorities will involve the nurse confirming existing knowledge, enhancing with newer knowledge, and validating retention of new knowledge.
Activity:
Confer with HCP about pulmonary rehabilitation order, or, at minimum a one-time consult with PT to develop home exercise program for patient.
Encourage daily walking with increasing time and distance.
Confer with HCP if patient qualifies for oxygen during exercise. Suggest a 6-minute walk test.
Nutrition:
5 to 6 small meals per day with lower carbohydrate and calories from protein/fats
Nutritional supplements if tolerated
Weigh weekly; if weight trends downward, contact HCP
Oxygen Therapy:
Review O2 therapy with the patient and her husband. Include its purpose, how to safely administer within the home setting, and re-ordering information. Assess the patient and her caregiver for any questions.
Respiratory Medications:
Explain the action of the Ventolin HFA and how the symptoms she had were a direct result of too much. Explain how the medication should be dosed.
Explain the purpose of Ipratropium HFA, and how this medication is also to be used.
Reinforce the use of the counter on the MDI. Ask the patient to show how she uses and cleans her MDI and how she tells if it is empty (e.g., look at the counter).
Explain the Advair DPI diskus and have her show use. Explain the difference between the DPI and MDI. Explain why mouth rinses are important after the Advair and provide written points on the difference. Explain that the Advair will prevent her from having as many exacerbations.
Explain that the long-acting β2-adrenergic agonists (LABA) should prevent night-time dyspnea.
Other Medications:
Explain about Prednisone, and its role as a steroid in helping reduce inflammation in COPD exacerbations.
Teach about Doxycycline, and its role in helping prevent repeated exacerbations in chronic COPD. Ensure patient is aware that even though feeling better, it is important to finish the full 10-day course of therapy.
Explain the purpose of Lasix, it’s role in helping in helping reduce the overall amount of fluid in the body (including the lungs), to help breathe easier. Explain important adverse effects of Lasix.
Other Important Teaching Points:
Teach and/or gently reinforce the patient huff coughing and pursed lip breathing. Give written materials on these techniques and have her return the demonstration.
Discuss the cardinal symptoms of COPD exacerbation, including increased dyspnea, increased volume and purulence of sputum, and what and when she should report to the HCP.
9. Develop a conceptual care map for H.M
1. The nurse teaches a patient with bronchiectasis that which problem would warrant a call to the clinic?”
a. Blood clots in the sputum
b. Sticky sputum on a hot day
c. Producing large amounts of sputum daily
d. Increased shortness of breath after eating a large meal
If hemoptysis occurs, the patient should contact the HCP. In some patients, a spot of blood is usual. The HCP should give specific instructions about when emergency contact is needed. The other indicators listed are to be expected in the patient with bronchiectasis, and do not need urgent medical attention.
2. Which treatment(s) would the nurse expect to implement in the management plan of an adult patient with cystic fibrosis? (select all that apply)
a. Airway clearance techniques
b. Bronchodilators and mucolytics
c. Pancreatic enzyme replacement
d. IV corticosteroids on a chronic basis
e. Inhaled tobramycin to combat Pseudomonas infection
Airway clearance techniques include chest physiotherapy, positive expiratory pressure devices, breathing exercises, and high-frequency chest wall oscillation systems. Bronchodilators and mucolytics are an important part of this plan. Severe constipation can be treated with polyethylene glycol (PEG) electrolyte solution, which is used to thin bowel contents. Inhaled tobramycin is effective in patients with CF who have Pseudomonas infections.
3. A 37-year-old patient is concerned they have asthma. Of the symptoms they describe to you, which ones suggest asthma or risk factors for asthma? (select all that apply)
a. Prolonged inhalation
b. Gastric reflux or heartburn
c. Cough worse at night or early in the morning
d. History of allergic rhinitis or chronic sinusitis
e. Chest pain and syncope after exercising with a stationary bicycle for 5 minutes
Allergic rhinitis is a major predictor of adult asthma. Acute and chronic sinusitis, especially bacterial rhinosinusitis, may worsen asthma. The chronic inflammation of asthma leads to recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night or in the early morning. GERD is more common in people with asthma than in the general population. GERD may worsen asthma symptoms because reflux may trigger bronchoconstriction and cause aspiration. Chest pain and syncope after five minutes of exercise are not normal for the patient with asthma, and patient should be encouraged to report these specific findings to their HCP for additional follow-up.
4. Which finding indicate that a patient with asthma is developing status asthmaticus? (select all that apply)
a. Anxiety and panic
b. Positive sputum culture
c. Unable to speak in complete sentences
d. Chest x-ray shows hyperinflated lungs
e. Lack of response to conventional treatment
Status asthmaticus is characterized by a lack of response to conventional treatment. This is potentially a life-threatening medical emergency, which may require mechanical ventilation in the ICU. As the patient is keenly aware that response to treatment is not working, anxiety and panic may be observed. If the patient can speak in complete sentences, or, has a PEFR >300L/min, then there is no immediate threat to the respiratory system. A chest x-ray with hyperinflated lungs and a flattened diaphragm is strongly suggestive of COPD. A positive sputum culture indicates lung infection.
5. Which statement indicates the patient with asthma requires further teaching about self-care?
a. “I use my corticosteroid inhaler every time I feel short of breath.”
b. “I get a flu shot every year and see my HCP if I have an upper respiratory tract infection.”
c. “I use my inhaler before I visit my aunt who has a cat, but I only visit for a few minutes because of my allergies.”
d. “I walk 30 minutes every day, but sometimes I have to use my bronchodilator inhaler before walking to prevent me from getting short of breath.”
A rescue plan for patients with asthma includes taking 2 to 4 puffs of a short acting bronchodilator (not a corticosteroid) every 20 minutes (3 times) to obtain rapid control of symptoms. All other patient statements identify to the nurse that the patient has accurate knowledge about his condition.
6. Which medication would be appropriate to administer to a patient experiencing an acute asthma attack?
a. IV theophylline
b. Montelukast (Singulair)
c. Inhaled hypertonic saline
d. Albuterol (Proventil HFA)
The mainstay of acute asthmatic treatment is inhalation of short-acting β2adrenergic agonist (SABA) bronchodilators, such as albuterol (ProAir HFA, Proventil HFA, Ventolin HFA). In patients with a moderate to severe attack, inhaled ipratropium (Atrovent) is used in conjunction with SABA. Salmeterol (Serevent Diskus) and montelukast (Singulair) are long-term control medications. Inhaled hypertonic saline is used in cystic fibrosis and bronchiectasis to help thin secretions. IV Theophylline is no longer recommended for the treatment of acute asthma attacks or in COPD exacerbations because of a very narrow therapeutic window, the availability of newer and more effective drugs, and, significant adverse effects (e.g., seizures and dysrhythmias).
7. The plan of care for the patient with chronic obstructive pulmonary disease (COPD) would include (select all that apply)
a. exercise such as walking.
b. high flow rate of O2 administration.
c. low-dose oral corticosteroid therapy.
d. use of monthly chest x-rays to monitor the progression of COPD.
e. breathing exercises, such as pursed-lip breathing that focus on exhalation.
Breathing exercises may assist the COPD patient during rest and activity (e.g., lifting, walking, stair climbing) by decreasing dyspnea, improving oxygenation, and slowing the respiratory rate. Walking (or other endurance exercises, such as cycling), combined with strength training, when possible, are probably the best interventions to strengthen muscles and improve the endurance of a patient with chronic obstructive pulmonary disease (COPD). Low dose oral corticosteroids may be appropriate for chronic COPD patients. Frequent chest x-rays are not needed.
8. What would the nurse include when teaching a patient how to use a metered-dose inhaler (MDI)?
a. After activating the MDI, breathe in as quickly as you can.
b. Estimate the amount of remaining medicine in the MDI by floating the canister in water.
c. Disassemble the plastic canister from the inhaler and rinse both pieces under running water every week.
d. To determine how long the canister will last, divide the total number of puffs in the canister by the puffs needed per day.
The patient needs to know the correct way to determine if the metered-dose inhaler (MDI) is empty. The patient should divide the total number of puffs in the canister by the puffs needed per day. The other three statements are not correct.
When caring for a patient with chronic obstructive pulmonary disease (COPD), the nurse determines that the patient’s nutrition status is impaired after noting a weight loss of 30 lb. Which intervention would the nurse add to the plan of care?
Order fruits and fruit juices to be offered between meals.
Order a high-calorie, high-protein diet with six small meals a day.
Provide a high-calorie, high-carbohydrate, nonirritating, frequent feeding diet.
Encourage the patient to double carbohydrate consumption and decrease fat intake.
Because the patient with COPD needs to use greater energy to breathe, there is often decreased oral intake because of dyspnea. A full stomach also impairs the ability of the diaphragm to descend during inspiration, thus interfering with the work of breathing. For these reasons, the patient with COPD would eat 6 small meals per day taking in a high-calorie, high-protein diet, with nonprotein calories divided evenly between fat and carbohydrate. The other interventions will not increase the patient’s caloric intake
A patient with chronic obstructive pulmonary disease (COPD) becomes dyspneic at rest. The baseline ABG results are PaO2 70 mm Hg, PaCO2 52 mm Hg, and pH 7.34. After assessing the patient, what new finding would require the nurse’s priority intervention?
Arterial pH 7.26
PaCO2 50 mm Hg
Patient in tripod position
Increased sputum expectoration
The patient’s pH shows acidosis that supports an exacerbation of COPD along with the worsening dyspnea. The PaCO2 has improved from baseline, the tripod position helps the patient’s breathing, and the increase in sputum expectoration will improve the patient’s ventilation.
Normal aterial ph range: 7.38 to 7.42. ph
During an assessment of a patient with asthma, the nurse notes wheezing and dyspnea. The nurse interprets that these symptoms are related to what pathophysiologic change?
Laryngospasm
Pulmonary edema
Narrowing of the airway
Overdistention of the alveoli
Narrowing of the airway by persistent but variable inflammation leads to reduced airflow, making it difficult for the patient to breathe and producing the characteristic wheezing. Laryngospasm, pulmonary edema, and overdistention of the alveoli do not produce wheezing
The nurse is evaluating if a patient understands how to safely determine whether a metered-dose inhaler (MDI) is empty. The nurse decides the patient understands this important information when the patient describes which method to check the inhaler?
Place it in water to see if it floats.
Keep track of the number of inhalations used.
Shake the canister while holding it next to the ear.
Check the indicator line on the side of the canister.
It is no longer appropriate to see if a canister floats in water or not because this is not an accurate way to determine the remaining inhaler doses. The best method to determine when to replace an inhaler is by knowing the maximum puffs available per MDI and then replacing it after the number of days when those inhalations have been used (100 puffs/2 puffs each day = 50 days)
Which test result identifies that a patient with asthma is responding to treatment?
An increase in CO2 levels
A decreased exhaled nitric oxide
A decrease in white blood cell count
An increase in serum bicarbonate levels
Nitric oxide levels are increased in the breath of people with asthma. A decrease in the exhaled nitric oxide concentration suggests that the treatment may be decreasing the lung inflammation associated with asthma and adherence to treatment. An increase in CO2 levels, decreased white blood cell count, and increased serum bicarbonate levels do not indicate a positive response to treatment in a patient with asthma.
The nurse is teaching a patient how to self-administer ipratropium via a metered-dose inhaler (MDI). Which instruction is most appropriate to help the patient learn the proper inhalation technique?
“Avoid shaking the inhaler before use.”
“Breathe out slowly before positioning the inhaler.”
“Using a spacer should be avoided for this type of medication.”
“After taking a puff, hold the breath for 30 seconds before exhaling.”
It is important to breathe out slowly before positioning the inhaler. This allows the patient to take a deeper breath while inhaling the medication, thus enhancing the effectiveness of the dose. The inhaler should be shaken well. A spacer may be used. Holding the breath after the inhalation of medication helps keep the medication in the lungs, but 30 seconds will not be possible for a patient with COPD.
When teaching the patient with cystic fibrosis about diet and medications, what priority information would the nurse include?
Fat-soluble vitamins and dietary salt should be avoided.
Insulin may be needed with a diabetic diet if diabetes develops.
Pancreatic enzymes and adequate fat, calories, protein, and vitamins are needed.
Distal intestinal obstruction syndrome (DIOS) can be treated with increased water.
The patient must take pancreatic enzymes before each meal and snack and adequate fat, calories, protein, and vitamins should be eaten. Fat-soluble vitamins are needed because they are malabsorbed with the excess mucus in the gastrointestinal system. Insulin may be needed, but there is no longer a diabetic diet, and this is not priority information at this time. DIOS develops in the terminal ileum and is treated with balanced polyethylene glycol electrolyte solution (MiraLAX) to thin bowel contents
The nurse is assigned to care for a patient in the emergency department with an asthma exacerbation. The patient has received a β-adrenergic bronchodilator and supplemental oxygen. If the patient’s condition does not improve, what would the nurse anticipate as the most likely next step in treatment?
IV fluids
Biofeedback therapy
Systemic corticosteroids
Pulmonary function testing
Systemic corticosteroids speed the resolution of asthma exacerbations and are indicated if the initial response to the β-adrenergic bronchodilator is insufficient. IV fluids may be used but not to improve ventilation. Biofeedback therapy and pulmonary function testing may be used after recovery to assist the patient and monitor the asthma.
A patient with bronchiectasis has copious thick respiratory secretions. Which intervention would the nurse include in the plan of care?
Use the incentive spirometer for at least 10 breaths every 2 hours.
Give prescribed antibiotics and antitussives on a scheduled basis.
Increase intake to at least 12 eight-ounce glasses of fluid every 24 hours.
Provide nutritional supplements that are high in protein and carbohydrates.
Adequate hydration helps to liquefy secretions and thus make it easier to remove them. Unless there are contraindications, the nurse should teach the patient to drink at least 3 L of fluid daily. Although nutrition, breathing exercises, and antibiotics may be indicated, these interventions will not liquefy or thin secretions. Antitussives may reduce the urge to cough and clear sputum, increasing congestion. Expectorants may be used to liquefy and facilitate clearing secretions
When teaching the patient with chronic obstructive pulmonary disease (COPD) about smoking cessation, what information would the nurse include about the effects of smoking on the lungs?
Smoking causes a hoarse voice.
Cough will become nonproductive.
Decreased alveolar macrophage function.
Sense of smell is decreased with smoking.
The damage to the lungs includes alveolar macrophage dysfunction that increases the incidence of infections and thus increases patient discomfort and cost to treat the infections. Other lung damage that contributes to infections includes cilia paralysis or destruction, increased mucus secretion, and bronchospasms that lead to sputum accumulation and increased cough. The patient may already be aware of respiratory mucosa damage with hoarseness and decreased sense of smell and taste, but these do not increase the incidence of pulmonary infection.
The nurse evaluates that nursing interventions to promote airway clearance in a patient admitted with chronic obstructive pulmonary disease (COPD) are successful based on which finding?
Absence of dyspnea
Improved mental status
Effective and productive coughing
PaO2 within normal range for the patient
Airway clearance is most directly evaluated as successful if the patient can engage in effective and productive coughing. Absence of dyspnea, improved mental status, and PaO2 within normal range for the patient show improved respiratory status but do not evaluate airway clearance
When admitting a patient with a diagnosis of asthma exacerbation, the nurse would assess for what potential triggers? (Select all that apply.)
Exercise
Allergies
Emotional stress
Decreased humidity
Upper respiratory infections
Although the exact mechanism of asthma is unknown, there are several triggers that may precipitate an attack. These include allergens, exercise, air pollutants, upper respiratory infections, drug and food additives, stress, and gastroesophageal reflux disease (GERD).
An adolescent patient with a history of frequent lung and sinus infections has symptoms consistent with undiagnosed cystic fibrosis (CF). Which information would be accurate for the nurse to include when teaching the patient about a scheduled sweat chloride test?
“Sweat chloride greater than 60 mmol/L is consistent with a diagnosis of CF.”
“The test measures the amount of sodium chloride in your postexercise sweat.”
“If sweating occurs after an oral dose of pilocarpine, the test result for CP is positive.”
“If the sweat chloride test result is positive on two occasions, genetic testing will be necessary.”
The diagnostic criteria for CF involve a combination of clinical presentation, sweat chloride testing, and genetic testing to confirm the diagnosis. Values above 60 mmol/L for sweat chloride are consistent with the diagnosis of CF. However, a second sweat chloride test is recommended to confirm the diagnosis, unless genetic testing identifies a CF mutation. Genetic testing is used if the results from a sweat chloride test are unclear
The patient with cystic fibrosis (CF) has been admitted to the unit. What intervention would the nurse include in the plan of care?
Strict bedrest
Fluid restrictions of 1500 mL a day
Aggressive chest physical therapy (CPT)
Limit diet intake of sodium-containing foods
Acute care for the patient with CF includes relief of bronchoconstriction, airway obstruction, and airflow limitation. Interventions include aggressive CPT, antibiotics, and O2 therapy in severe disease. Measures to optimize nutrition are important. There is no reason to limit foods containing sodium.
The nurse determines that the patient is not experiencing adverse effects of albuterol (Proventil) after noting which patient vital sign?
Temperature of 98.4°F
Oxygen saturation 96%
Pulse rate of 72 beats/min
Respiratory rate of 18/breaths
Albuterol is a β2-agonist that can sometimes cause adverse cardiovascular effects. These would include tachycardia and angina. A pulse rate of 72 beats/min indicates that the patient does not have tachycardia as an adverse effect
The nurse determines that therapy with ipratropium is effective after noting which assessment finding?
Decreased respiratory rate
Increased respiratory rate
Increased peak flow readings
Decreased sputum production
Ipratropium is a bronchodilator that should result in increased peak expiratory flow rates.
The nurse determines the patient with asthma has activity intolerance. What is the most likely reason for this problem?
Work of breathing
Fear of suffocation
Effects of medications
Anxiety and restlessness
When the patient does not have sufficient gas exchange to engage in activity, the etiologic factor is often the work of breathing. When patients with asthma do not have effective respirations, they use all available energy to breathe and have little left over for purposeful activity. Fear of suffocation, effects of medications or anxiety, and restlessness are not etiologies for activity intolerance for a patient with asthma
you are assessing your patient who is having difficulty breathing. For any patient with an acute asthmatic attack, which of the following medications should you offer for immediate relief of symptoms?
Beta blocker
Angiotensin-converting enzyme (ACE) inhibitor
Anti-immunoglobulin (IgE) antibodies
Beta 2 agonist, inhaled corticosteroids
The best options for treating a patient with an acute asthma attack would be either an inhaled β2-adrenergic agonist or corticosteroid. Beta blocker, ACE inhibitor, or IgE antibody therapies are not part of acute asthma management.
The nurse determines that the patient understood medication instructions about the use of a spacer device when taking inhaled medications if the patient states:
“I will pay less for medication because it will last longer.”
“More of the medication will get down into my lungs to help my breathing.”
“Now I will not need to breathe in as deeply when taking the inhaler medications.”
“This device will make it so much easier and faster to take my inhaled medications.”
A spacer assists more medication to reach the lungs, with less being deposited in the mouth and the back of the throat. It does not affect the cost or increase the speed of using the inhaler
In which position would the nurse place a patient experiencing an asthma exacerbation?
Supine
Lithotomy
High Fowler’s
Reverse Trendelenburg
The patient experiencing an asthma attack would be placed in high Fowler’s position and may need to lean forward to allow for optimal chest expansion and enlist the aid of gravity during inspiration. The supine, lithotomy, and reverse Trendelenburg positions will not facilitation ventilation.
The nurse is teaching a patient how to self-administer beclomethasone, 2 puffs inhaled every 6 hours. What would the nurse teach the patient to do to prevent oral infection while taking this medication?
Chew a hard candy before the first puff of medication.
Ask for a breath mint after the second puff of medication.
Rinse the mouth with water before each puff of medication.
Rinse the mouth with water after the second puff of medication.
Because beclomethasone is a corticosteroid, the patient should rinse the mouth with water after the second puff of medication to reduce the risk of fungal overgrowth and oral infection
The nurse has administered a first dose of oral prednisone to a patient with asthma. What parameter would the nurse begin to monitor?
Apical pulse
Daily weight
Bowel sounds
Deep tendon reflexes
Corticosteroids such as prednisone can lead to weight gain. For this reason, it is important to monitor the patient’s daily weight. The drug should not affect the apical pulse, bowel sounds, or deep tendon reflexes
The nurse supervises a team including another registered nurse (RN), a licensed practical/vocational nurse (LPN/VN), and assistive personnel (AP) on a medical unit in caring for many patients with respiratory problems. In what situation would the nurse intervene?
LPN/VN obtained a pulse oximetry reading of 94% but did not report it.
AP report to the nurse that the patient is reporting of difficulty breathing.
RN taught the patient about home oxygen safety in preparation for discharge.
LPN/VN changed the type of oxygen device based on arterial blood gas results.
It is not within the LPN scope to change oxygen devices based on analysis of lab results. It is within the scope of practice of the RN to assess, teach, and evaluate. The LPN provides care for stable patients and may adjust oxygen flow rates depending on desired oxygen saturation levels of stable patients. The AP may obtain oxygen saturation levels, assist patients with comfort adjustment of oxygen devices, and report changes in patient’s level of consciousness or difficulty breathing
When planning teaching for the patient with chronic obstructive pulmonary disease (COPD), the nurse understands the manifestations of the disease are related to what process?
An overproduction of the antiprotease a1-antitrypsin
Hyperinflation of alveoli and destruction of alveolar walls
Hypertrophy and hyperplasia of goblet cells in the bronchi
Collapse and hypoventilation of the terminal respiratory unit
In COPD, structural changes include hyperinflation of alveoli, destruction of alveolar walls, destruction of alveolar capillary walls, narrowing of small airways, and loss of lung elasticity. An autosomal recessive deficiency of antitrypsin may cause COPD. Not all patients with COPD have excess mucus production by the increased number of goblet cells
A patient has been receiving oxygen per nasal cannula while hospitalized for chronic obstructive pulmonary disease (COPD). The patient asks the nurse whether oxygen use will be needed at home. What is the most appropriate response by the nurse?
“Long-term home oxygen therapy should be used to prevent respiratory failure.”
“Oxygen will not be needed unless you are in the terminal stages of this disease.”
“Long-term home oxygen therapy should be used to prevent heart problems related to COPD.”
“You will not need oxygen until your oxygen saturation drops to 88% and you have symptoms of hypoxia.”
Long-term oxygen therapy in the home will not be considered until the oxygen saturation is less than or equal to 88% and the patient has signs of tissue hypoxia, such as cor pulmonale, erythrocytosis, or impaired mental status. PaO2 less than 55 mm Hg will also allow home oxygen therapy to be considered.
What symptoms would the nurse teach the patient with bronchiectasis to report to the health care provider?
Increasing dyspnea
Temperature below 98.6°F
Decreased sputum production
Unable to drink 3 L of low-sodium fluids
The significant manifestations to report to the health care provider include increasing dyspnea, fever, chills, increased sputum production, bloody sputum, and chest pain. Although drinking at least 3 L of low-sodium fluid will help liquefy secretions to make them easier to expectorate, the health care provider does not need to be notified if the patient cannot do this one day.
Before discharge, the nurse discusses activity levels with an older adult patient with chronic obstructive pulmonary disease (COPD) and pneumonia. Which exercise goal is most appropriate after the patient has recovered from this episode of illness?
Slightly increase activity over the current level.
Swim for 10 min/day, gradually increasing to 30 min/day.
Limit exercise to activities of daily living to conserve energy.
Walk for 20 min/day, keeping the pulse rate less than 130 beats/min.
The patient will benefit from mild aerobic exercise that does not stress the cardiorespiratory system. The patient should be encouraged to walk for 20 min/day, keeping the pulse rate less than 75% to 80% of maximum heart rate (220—patient’s age).
The nurse determines that a patient is experiencing common adverse effects from the inhaled corticosteroid beclomethasone after what occurs?
Hypertension and pulmonary edema
Oropharyngeal candidiasis and hoarseness
Elevation of blood glucose and calcium levels
Adrenocortical dysfunction and hyperglycemia
Oropharyngeal candidiasis and hoarseness are common adverse effects from the use of inhaled corticosteroids because the medication can lead to overgrowth of organisms and local irritation if the patient does not rinse the mouth following each dose
While teaching a patient with asthma about the appropriate use of a peak flow meter, what would the nurse teach the patient to do?
Keep a record of the peak flow meter numbers if symptoms of asthma are getting worse.
Increase the dose of the long-term control medication if the peak flow numbers decrease.
Use the flowmeter each morning after taking medications to evaluate their effectiveness.
Empty the lungs and then inhale quickly through the mouthpiece to measure how fast air can be inhaled.
It is important to keep track of peak flow readings daily, especially when the patient’s symptoms are getting worse. The patient should have specific directions as to when to call the provider based on personal peak flow numbers. Peak flow is measured by exhaling into the flowmeter and would be assessed before and after medications to evaluate their effectiveness.
The provider has prescribed salmeterol (Serevent) for a patient with asthma. In reviewing the use of dry powder inhalers (DPIs) with the patient, what instructions would the nurse provide?
“Close lips tightly around the mouthpiece and breathe in deeply and quickly.”
“To administer a DPI, you must use a spacer that holds the medicine so that you can inhale it.”
“You will know you have correctly used the DPI when you taste or sense the medicine going into your lungs.”
“Hold the inhaler several inches in front of your mouth and breathe in slowly, holding the medicine as long as possible.”
The patient would be instructed to tightly close the lips around the mouthpiece and breathe in deeply and quickly to ensure the medicine moves down deeply into the lungs. Dry powder inhalers do not require spacer devices. The patient may not taste or sense the medicine going into the lungs
The nurse is caring for a patient with an acute exacerbation of asthma. After initial treatment, what assessment finding indicates to the nurse that the patient’s respiratory status is improving?
Wheezing becomes louder.
Cough remains nonproductive.
Vesicular breath sounds decrease.
Aerosol bronchodilators stimulate coughing.
The primary problem during an exacerbation of asthma is narrowing of the airway and subsequent diminished air exchange. As the airways begin to dilate, wheezing gets louder because of better air exchange. Vesicular breath sounds will increase with improved respiratory status. After a severe asthma exacerbation, the cough may be productive and stringy. Coughing after aerosol bronchodilators may indicate a problem with the inhaler or its use
Which statement made by the patient with chronic obstructive pulmonary disease (COPD) indicates a need for further teaching about the use of an ipratropium inhaler?
“I should wait at least 1 to 2 minutes between each puff of the inhaler.”
“I can rinse my mouth following the two puffs to get rid of the bad taste.”
“Because this medication is not fast acting, I cannot use it in an emergency if my breathing is worse.”
“If my breathing gets worse, I should keep taking extra puffs of the inhaler until I can breathe more easily.”
The patient should not just keep taking extra puffs of the inhaler to make breathing easier. Excessive treatment could trigger paradoxical bronchospasm, which would worsen the patient’s respiratory status. Rinsing the mouth after the puffs will eliminate a bad taste. Waiting 1 to 2 minutes between each puff will facilitate the effectiveness of the administration. Ipratropium is not used in an emergency for COPD.
A middle aged patient with asthma is brought to the emergency department by automobile. He is short of breath and appears frightened. During the initial nursing assessment, which finding would be an early sign of an asthma exacerbation?
Anxiety
Cyanosis
Bradycardia
Hypercapnia
An early manifestation of an asthma attack is anxiety because the patient is acutely aware of the inability to get sufficient air to breathe. He will be hypoxic early on with decreased PaCO2 and increased pH as he is hyperventilating. If cyanosis occurs, it is a later sign. The pulse and blood pressure will be increased.
The nurse is assigned to care for a patient who has anxiety and an asthma exacerbation. What is the primary reason for the nurse to carefully inspect the patient’s chest wall?
Giving care will calm the patient
Observing for signs of diaphoresis
Evaluating the use of intercostal muscles
Monitoring the patient for bilateral chest expansion
The nurse physically inspects the chest wall to evaluate the use of intercostal (accessory) muscles, which gives an indication of the degree of respiratory distress. The other options may also occur, but they are not the primary reason for inspecting the chest wall of this patient.
The nurse teaches a patient with chronic obstructive pulmonary disease (COPD) how to administer fluticasone by metered-dose inhaler (MDI). Which statement indicates a correct understanding of the instructions?
“I should not use a spacer device with this inhaler.”
“I will rinse my mouth each time after I use this inhaler.”
“I will feel my breathing improve over the next 2 to 3 days.”
“I should use this inhaler immediately if I have trouble breathing.
Fluticasone may cause oral candidiasis (thrush). The patient should rinse the mouth with water or mouthwash after use or use a spacer device to prevent oral fungal infections. Fluticasone is an inhaled corticosteroid and it may take 2 weeks of regular use for effects to be evident. This medication is not recommended for an acute asthma attack.
Assessment findings of jugular venous distention and pedal edema would be indicative of what complication of chronic obstructive pulmonary disease (COPD)?
Acute respiratory failure
Secondary respiratory infection
Fluid volume excess from cor pulmonale
Pulmonary edema caused by left-sided heart failure
Cor pulmonale is a right-sided heart failure caused by resistance to right ventricular outflow resulting from lung disease. With failure of the right ventricle, the blood emptying into the right atrium and ventricle would be slowed, leading to jugular venous distention and pedal edema.
1. Describe the pathophysiology, clinical manifestations, and interprofessional and nursing management of the patient with bronchiectasis.
2. Describe the pathophysiology, clinical manifestations, and interprofessional and nursing management of the patient with cystic fibrosis.
3. Describe the etiology, pathophysiology, and clinical manifestations of asthma.
4. Explain the difference between an acute asthma exacerbation and status asthmaticus.
5. Describe the interprofessional care and nursing management of the patient with asthma.
6. Identify the classes of drugs used in the treatment of asthma and chronic obstructive pulmonary disease (COPD).
7. Describe the etiology, pathophysiology, clinical manifestations, and interprofessional care of the patient with COPD.
8. Explain the nursing management of the patient with COPD
α1-antitrypsin deficiency (AATD)
autosomal recessive disorder that may eventually affect the lungs and liver
asthma
Asthma is a diverse disease characterized by bronchial hyperreactivity with reversible expiratory airflow limitation, either spontaneously or with treatment.
signs + symptoms variable
bronchiectasis
bronchioles are dilated, making it hard to clear secretions. It most often results from poorly treated or untreated lung infections, immune system problems, or genetic factors. Bronchiectasis affects more than 500,000 people in the US.1 It is more common in women. It affects 1 in every 150 people over age 75
chronic bronchitis
presence of cough and sputum production for at least 3 months in each of 2 consecutive years.
chronic obstructive pulmonary disease (COPD)
progressive lung disease characterized by persistent airflow limitation. COPD is associated with an enhanced chronic inflammatory response in the airways and lungs. The main causes are cigarette smoking and other noxious particles and gases
cor pulmonale
Cor Pulmonale (Right-Sided Heart Failure) Cor pulmonale is an enlarged right ventricle in your heart that happens because of a lung condition.
cystic fibrosis (CF)
Cystic fibrosis (CF) is an inherited, autosomal recessive genetic disorder, characterized by altered transport of sodium and chloride ions in and out of epithelial cells. Airway obstruction occurs because of changes in exocrine glandular secretions, resulting in increased mucus production.
emphysema
destruction of alveoli without fibrosis, describes one of several structural abnormalities in COPD.
peak expiratory flow rate (PEFR)
measured by the peak flow meter (at home or in a health care setting) is a test of lung function. PEFR measures the maximum rate of airflow after a forceful exhalation. When monitored routinely, PEFR measurements can provide a baseline of the patient’s health status. PEFR can help predict an asthma attack or monitor the severity of disease.
status asthmaticu
most extreme form of an acute asthma attack. It is characterized by hypoxia, hypercapnia, and ARF. The patient is unresponsive to treatment with bronchodilators and corticosteroids.
Key Points
BRONCHIECTASIS Bronchiectasis is characterized by permanent, abnormal dilation of one or more large bronchi. The pathophysiologic changes that occur result in dilation of the airways and destruction of the elastic and muscular structures supporting the bronchial wall.
Clinical Manifestations and Complications
The hallmark of bronchiectasis is persistent or recurrent cough with production of large amounts of purulent sputum
In some situations, sputum production may exceed 500 mL/day.
Bacterial infection of the lungs, repeated aspiration, and several systemic diseases (e.g., diabetes, inflammatory bowel disease) are associated with increased risk.
Repeated exacerbations, pulmonary hypertension, and neovascularization (development of new blood vessels post-injury), can lead to hemoptysis
Diagnosis
CT is the gold standard for diagnosis of bronchiectasis
Management
Bronchiectasis is hard to treat. Therapy is aimed at treating acute exacerbations and preventing a decline in lung function.
Antibiotics are the mainstay of treatment. Long-term suppressive therapy with antibiotics is reserved for those patients who have symptoms that recur a few days after stopping antibiotics.
An important nursing goal is to promote drainage and removal of mucus from the lungs. Rest, good nutrition, adequate hydration, and patient education are important.
CYSTIC FIBROSIS
Cystic fibrosis (CF) is an autosomal recessive, multisystem disease characterized by altered function of the exocrine glands, producing airway obstruction and an increase in mucous production.
Eventually, CF progresses to a restrictive lung disease because of the fibrosis, lung destruction, and thoracic wall changes.
CF also involves the lungs, pancreas, and sweat glands.
Clinical Manifestations and Complications
Clinical manifestations vary depending on the severity of the disease.
In adults, a frequent cough, new-onset diabetes, and infertility problems are initial non-specific symptoms
Complications from CF can also vary widely, from cor pulmonale, pulmonary hypertension, CFRD, and sinus, bone, and liver disease.
Diagnosis
Is made with the “sweat test”
Management
Major goals of therapy in CF are to promote clearance of secretions, control infection in the lungs, and provide adequate nutrition.
Nursing care for the patient revolves around relieving airway obstruction, controlling infection, and promoting drainage of mucous from the patient’s lungs
Respiratory treatment may include bronchodilators, mucolytics, chest physiotherapy (postural drainage), and antibiotics.
Systemic management of the disease may include pancreatic enzyme replacement, prokinetic agents, and laxatives.
Psychosocial support and counselling for lifestyle adaptation, and, encouraging the patient to access community resources for information and support are important teaching points.
ASTHMA
Asthma is a chronic inflammatory disorder of the airways that results in recurrent episodes of airflow obstruction. It is usually reversible.
The main pathophysiologic process in asthma is persistent but variable inflammation of the airways. Airflow is limited because the inflammation results in bronchoconstriction, airway hyperresponsiveness (hyperreactivity), and edema of the airways.
Asthma is not a psychosomatic disease.
Clinical Manifestations and Complications
Although the exact mechanisms that cause asthma remain unknown, exposure to allergens or irritants initiates the inflammatory cascade.
The characteristic manifestations of asthma are wheezing, cough, dyspnea, and chest tightness, particularly at night or early in the morning. Expiration may be prolonged.
During an acute attack, the patient usually has signs of hypoxemia.
Risk factors and triggers for asthma and asthma attacks include nose and sinus problems, allergens, cigarette smoke, air pollutants, respiratory tract infections, exercise, occupational irritants, and GERD.
Genetics and one’s immune responses may influence asthma development.
A severe asthma attack, unresponsive to treatment, is known as status asthmaticus.
Severe acute asthma attacks and status asthmaticus may require intubation and mechanical ventilation.
Asthma can be classified as mild, moderate or severe, based upon current condition of the patient, including degree of respiratory difficulty and response to treatment.
Diagnosis
A diagnosis of asthma is usually made based upon the presence of various indicators
(e.g., clinical manifestations, health history, spirometry, peak flow variability).
Management
The goal of asthma treatment is to achieve and maintain control of the disease.
Asthma can be classified as mild, moderate or severe, based upon current condition of the patient, including degree of respiratory difficulty and response to treatment.
Once the patient is diagnosed, guidelines provide direction about medications (based on steps) the patient needs. The HCP will step up the medication therapy as asthma symptoms worsen, and step down the medication as the patient achieves control.
The level of control is determined by the patient's medication use, symptoms, and PEFR or FEV1.
Pharmacologic Management of Asthma
Asthma drugs may be classified as short term “rescue” medications (to treat symptoms during an acute attack) and long term “controller” medications (to achieve and maintain control of asthma after the acute episode has subsided).
All persons with asthma should always carry rescue medication.
Short-acting inhaled β2-adrenergic agonists (SABAs), including albuterol, are the most effective drugs for relieving acute bronchospasm. They are used for acute asthma attacks.
Long-acting inhaled β2-adrenergic agonists (LABAs), including salmeterol and formoterol, are never to be used alone due to an increased risk of death. They are safe when combined with ICS, such as fluticasone/salmeterol (Advair) or budesonide/formoterol (Symbicort).
Because chronic inflammation is a key component of asthma, inhaled corticosteroids are more effective in improving asthma control than any other long-term drug.
Leukotriene modifiers can be used in milder asthma successfully as add-on therapy to reduce the dose of inhaled corticosteroids.
The only anti-IgE drug, omalizumab (Xolair), is used for hard to treat moderate to severe asthma unable to be controlled by inhaled corticosteroids.
Methylxanthine (theophylline) preparations are no longer recommended for asthma, as thereare much newer drugs available with less severe side effects.
Anticholinergic agents are not used in asthma treatment, except for ipratropium (Atrovent), which is only used in the ED for acute attacks.
Other Management Priorities
The overall goals are that the patient with asthma will achieve asthma control, as evidenced by (1) minimal symptoms during the day and night, (2) acceptable activity levels (including exercise), (3) maintaining greater than 80% of personal best PEFR, (4) few or no adverse effects of therapy, (5) no acute attacks of asthma, and (6) adequate knowledge to carry out the plan of care.
Education is the cornerstone of asthma management. Your role in preventing asthma attacks or decreasing the severity in your patient focuses primarily on teaching the patient and caregiver.
One of the major factors determining success in asthma management is the correct administration of drugs.
Inhalation devices include metered-dose inhalers, dry powder inhalers, and nebulizers.
Teaching should include information about medications, including the name, purpose, dosage, method of administration, schedule, side effects, appropriate action if side effects occur, how to properly use and clean devices, and consequences for breathing if not taking medications as prescribed.
Several non-prescription combination drugs are available over the counter. An important teaching responsibility is to warn the patient about the dangers associated with non-prescription combination drugs.
One important goal in asthma care is to maximize the ability of the patient to safely manage acute asthma episodes through a written asthma action plan developed in conjunction with the HCP.
Written asthma action plans are shared with caregivers, especially for those patients with moderate or severe persistent asthma or a history of severe attacks.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease characterized by airflow limitation that is not fully reversible. It is almost always progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases, primarily caused by cigarette smoking.
COPD is characterized by chronic inflammation in the airways, lung parenchyma (respiratory bronchioles and alveoli), and pulmonary blood vessels.
The pathogenesis of COPD is complex and involves many mechanisms, with an inflammatory process different from that of asthma.
The defining features of COPD are not fully reversible airflow limitation during forced exhalation, caused by loss of elastic recoil and airflow obstruction from mucus hypersecretion, mucosal edema, and bronchospasm.
Gas exchange abnormalities can result in hypoxemia and hypercapnia.
COPD has systemic manifestations.
Clinical Manifestations and Complications
A chronic intermittent cough is the earliest symptom. As the disease progresses, the cough is present every day.
Sputum may or may not be produced. Symptoms are progressive.
Risk factors for developing COPD include smoking and cigarette smoke, occupational chemicals, air pollution, severe recurring respiratory infections, and α1-antitrypsin deficiency (an autosomal recessive disorder).
Complications may include exacerbations of COPD, signalled by a change in the patient’s usual dyspnea, cough, and/or sputum, that is different than the usual daily patterns. These flare-ups require changes in management and can have significant mortality if not appropriately treated.
Cor pulmonale is hypertrophy of the right side of the heart, with or without
heart failure, resulting from pulmonary hypertension and is a late manifestation of chronic pulmonary heart disease.
Patients with severe COPD who have exacerbations are at risk for the development of “acute on-chronic” respiratory failure.
Diagnosis
A diagnosis of COPD should be considered in any patient over the age of 40 with a smoking history of 10 or more pack years or who has symptoms of cough, sputum production, or dyspnea, and/or a history of exposure to risk factors for the disease.
The diagnosis of COPD is confirmed by spirometry.
COPD can be classified as mild, moderate, severe, and very severe.
An FEV1/FVC ratio of less than 70% establishes the diagnosis of COPD. The severity of obstruction (as indicated by FEV1) determines the stage of COPD.
Validated questionnaires such as the COPD Assessment Test (CAT) and Clinical COPD Questionnaire (CCQ) are recommended for a comprehensive assessment of symptoms.
Management
The main goals of care for the COPD patient are to: (1) relieve symptoms, (2) improve exercise tolerance to help facilitate ADLs, (3) avoid complications, (4) implement a long term treatment plan, (5) prevent progression of the disease, and (6) improve one’s overall quality of life.
Cessation of cigarette smoking in all stages of COPD is the intervention that can have the biggest impact to reduce the risk of developing COPD and influence the natural history of the disease.
Pharmacological Management of COPD
Although patients with COPD do not respond as dramatically as those with asthma to bronchodilator therapy, bronchodilator therapy can reduce the dyspnea and increase the FEV1.
Presently no drug modifies the decline of lung function in patients with COPD.
Inhaled anticholinergics or LABAs may be used or combined with inhaled corticosteroids.
Monotherapy with inhaled corticosteroids is not recommended due to the side effects.
Possible Surgical Options for COPD
Four different surgical procedures have been used in severe COPD, but not all COPD patients are considered candidates for the following procedures.
Lung volume reduction surgery (LVRS) reduces the size of the lungs by removing the most diseased lung tissue so that the remaining healthy lung tissue can perform better.
Bronchoscopic lung volume reduction surgery works by placing 1-way valves in the airways leading to the diseased parts of the lung. The valves let air out but not in. This collapses a certain segment of the lung and has a similar result as LVRS.
A bullectomy is used for certain patients and can result in improved lung function and reduction in dyspnea.
Lung transplantation can improve functional capacity and enhance quality of life in appropriately selected patients with very advanced COPD.
Other Management Priorities
O2 therapy is used in the treatment of COPD and many other problems associated with hypoxemia. Long-term O2 therapy may improve survival, exercise capacity, cognitive performance, and sleep in hypoxemic patients.
For most patients, the goal of O2 therapy is to keep the SaO2 greater than 90% during rest, sleep, and exertion, or, the PaO2 greater than 60 mm Hg. These goals may be modified for the patient with moderate to severe COPD.
Weight loss and malnutrition are common in the patient with severe COPD. The patient with weight loss needs extra protein and calories and tips on energy conservation while eating and preparing food.
Pursed-lip breathing is a technique that is used to prolong exhalation and thereby prevent bronchiolar collapse and air trapping.
Airway clearance techniques include effective coughing techniques, chest physiotherapy, and airway clearance devices. Airway clearance devices include those using positive airway pressure, such as Flutter. No one is better than the other, but it depends on patient preference.
Huff coughing is an effective technique that the patient can be easily taught. Effective coughing conserves energy, reduces fatigue, and promotes removal of secretions.Chest physiotherapy consists of percussion, vibration, and postural drainage.
Pulmonary rehabilitation should be considered for all patients with COPD or having functional limitations. The overall goal is to increase exercise capacity and improve the quality of life.
The patient with COPD will require acute care for complications, such as exacerbations, cor pulmonale, and acute respiratory failure.
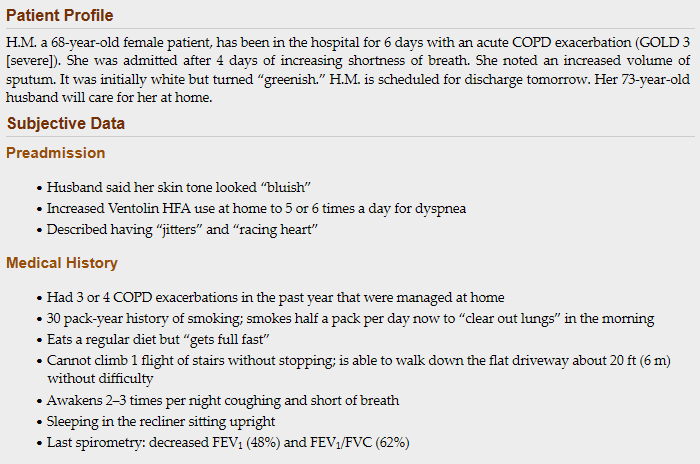

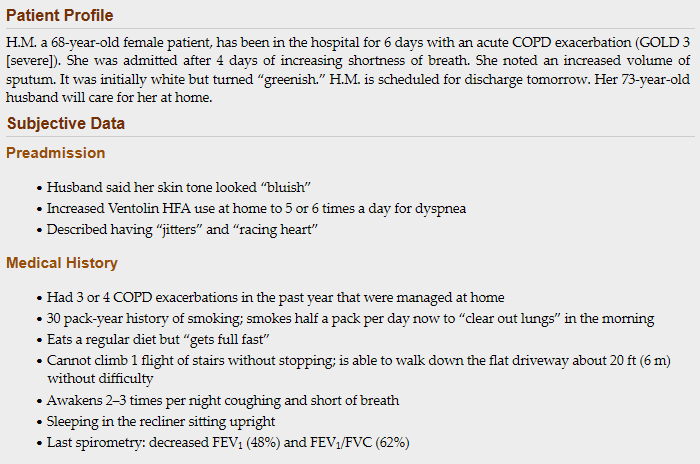
1. Recognize: What manifestations show H.M. had a COPD exacerbation?
Increased dyspnea, increased work of breathing (at rest) and a change in the color, amount, or other characteristics of one’s sputum (e.g., becoming thick, purulent, when patient normally expectorates thin, clear secretions).
2. Analyze: What is the most likely cause of her exacerbation?
Smoking and air pollution exposure as a police officer.
3. Analyze: Why would H.M. “feel full fast” when eating? What could you do to address this issue?
Sensations of feeling full after consuming small amounts can be attributed to swallowing air while eating, side effects of medication (especially corticosteroids), and the abnormal position of the diaphragm relative to the stomach (in association with hyperinflation of the lungs).
4. Analyze: What symptoms indicate overuse of inhalers? Which drug would cause the symptoms described?
“Jitters” and “racing heart”; the Ventolin HFA would be the primary cause.
5. Analyze: Interpret the ABG on admission and 24 hours post-admission. In comparing both ABGs, do you see a pattern?
ABG in ED: Partially compensated respiratory acidosis:
pH: 7.34: low, thus acidosis (normal 7.35 to 7.45)
PaCO2: 59 mm Hg: high (normal 35 to 45 mm Hg), thus the cause of the acidosis
HCO3-: 27 mEq/L (normal 22 to 26 mEq/L): one point over normal, thus the kidneys are just beginning to compensate by conserving bicarbonate and trying to bring the pH to normal.
PaO2 68 mm Hg, she is hypoxemic (normal: 80 to 100 mmHg)
24 Hours after admission: pH: 7.30 (H.M.is becoming more acidotic)
PaCO2: 63 mmHg (increasing, indicating a worsening acidosis)
HCO3-: 29 (above normal, but not much change)
PaO2: 64 (continues to indicate hypoxemia).
This is described as an “acute-on-chronic” exacerbation, as evidenced by worsening acidosis and hypoxemia, and relatively little change in bicarbonate.
6. Prioritize: Based on the assessment data presented, what are the priority clinical problems?
Impaired respiratory system function, nutritionally compromised, activity intolerance, deficient knowledge, substance abuse (e.g., continued cigarette smoking)
7. Act: What is one suggestion you could make to H.M. that could halt the progression of her COPD?
stop smoking
8. Act: What should you include in her discharge planning and teaching?
Several important priorities for discharge teaching and planning must be considered before H.M. can return home. Most priorities will involve the nurse confirming existing knowledge, enhancing with newer knowledge, and validating retention of new knowledge.
Activity:
Confer with HCP about pulmonary rehabilitation order, or, at minimum a one-time consult with PT to develop home exercise program for patient.
Encourage daily walking with increasing time and distance.
Confer with HCP if patient qualifies for oxygen during exercise. Suggest a 6-minute walk test.
Nutrition:
5 to 6 small meals per day with lower carbohydrate and calories from protein/fats
Nutritional supplements if tolerated
Weigh weekly; if weight trends downward, contact HCP
Oxygen Therapy:
Review O2 therapy with the patient and her husband. Include its purpose, how to safely administer within the home setting, and re-ordering information. Assess the patient and her caregiver for any questions.
Respiratory Medications:
Explain the action of the Ventolin HFA and how the symptoms she had were a direct result of too much. Explain how the medication should be dosed.
Explain the purpose of Ipratropium HFA, and how this medication is also to be used.
Reinforce the use of the counter on the MDI. Ask the patient to show how she uses and cleans her MDI and how she tells if it is empty (e.g., look at the counter).
Explain the Advair DPI diskus and have her show use. Explain the difference between the DPI and MDI. Explain why mouth rinses are important after the Advair and provide written points on the difference. Explain that the Advair will prevent her from having as many exacerbations.
Explain that the long-acting β2-adrenergic agonists (LABA) should prevent night-time dyspnea.
Other Medications:
Explain about Prednisone, and its role as a steroid in helping reduce inflammation in COPD exacerbations.
Teach about Doxycycline, and its role in helping prevent repeated exacerbations in chronic COPD. Ensure patient is aware that even though feeling better, it is important to finish the full 10-day course of therapy.
Explain the purpose of Lasix, it’s role in helping in helping reduce the overall amount of fluid in the body (including the lungs), to help breathe easier. Explain important adverse effects of Lasix.
Other Important Teaching Points:
Teach and/or gently reinforce the patient huff coughing and pursed lip breathing. Give written materials on these techniques and have her return the demonstration.
Discuss the cardinal symptoms of COPD exacerbation, including increased dyspnea, increased volume and purulence of sputum, and what and when she should report to the HCP.
9. Develop a conceptual care map for H.M
1. The nurse teaches a patient with bronchiectasis that which problem would warrant a call to the clinic?”
a. Blood clots in the sputum
b. Sticky sputum on a hot day
c. Producing large amounts of sputum daily
d. Increased shortness of breath after eating a large meal
If hemoptysis occurs, the patient should contact the HCP. In some patients, a spot of blood is usual. The HCP should give specific instructions about when emergency contact is needed. The other indicators listed are to be expected in the patient with bronchiectasis, and do not need urgent medical attention.
2. Which treatment(s) would the nurse expect to implement in the management plan of an adult patient with cystic fibrosis? (select all that apply)
a. Airway clearance techniques
b. Bronchodilators and mucolytics
c. Pancreatic enzyme replacement
d. IV corticosteroids on a chronic basis
e. Inhaled tobramycin to combat Pseudomonas infection
Airway clearance techniques include chest physiotherapy, positive expiratory pressure devices, breathing exercises, and high-frequency chest wall oscillation systems. Bronchodilators and mucolytics are an important part of this plan. Severe constipation can be treated with polyethylene glycol (PEG) electrolyte solution, which is used to thin bowel contents. Inhaled tobramycin is effective in patients with CF who have Pseudomonas infections.
3. A 37-year-old patient is concerned they have asthma. Of the symptoms they describe to you, which ones suggest asthma or risk factors for asthma? (select all that apply)
a. Prolonged inhalation
b. Gastric reflux or heartburn
c. Cough worse at night or early in the morning
d. History of allergic rhinitis or chronic sinusitis
e. Chest pain and syncope after exercising with a stationary bicycle for 5 minutes
Allergic rhinitis is a major predictor of adult asthma. Acute and chronic sinusitis, especially bacterial rhinosinusitis, may worsen asthma. The chronic inflammation of asthma leads to recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night or in the early morning. GERD is more common in people with asthma than in the general population. GERD may worsen asthma symptoms because reflux may trigger bronchoconstriction and cause aspiration. Chest pain and syncope after five minutes of exercise are not normal for the patient with asthma, and patient should be encouraged to report these specific findings to their HCP for additional follow-up.
4. Which finding indicate that a patient with asthma is developing status asthmaticus? (select all that apply)
a. Anxiety and panic
b. Positive sputum culture
c. Unable to speak in complete sentences
d. Chest x-ray shows hyperinflated lungs
e. Lack of response to conventional treatment
Status asthmaticus is characterized by a lack of response to conventional treatment. This is potentially a life-threatening medical emergency, which may require mechanical ventilation in the ICU. As the patient is keenly aware that response to treatment is not working, anxiety and panic may be observed. If the patient can speak in complete sentences, or, has a PEFR >300L/min, then there is no immediate threat to the respiratory system. A chest x-ray with hyperinflated lungs and a flattened diaphragm is strongly suggestive of COPD. A positive sputum culture indicates lung infection.
5. Which statement indicates the patient with asthma requires further teaching about self-care?
a. “I use my corticosteroid inhaler every time I feel short of breath.”
b. “I get a flu shot every year and see my HCP if I have an upper respiratory tract infection.”
c. “I use my inhaler before I visit my aunt who has a cat, but I only visit for a few minutes because of my allergies.”
d. “I walk 30 minutes every day, but sometimes I have to use my bronchodilator inhaler before walking to prevent me from getting short of breath.”
A rescue plan for patients with asthma includes taking 2 to 4 puffs of a short acting bronchodilator (not a corticosteroid) every 20 minutes (3 times) to obtain rapid control of symptoms. All other patient statements identify to the nurse that the patient has accurate knowledge about his condition.
6. Which medication would be appropriate to administer to a patient experiencing an acute asthma attack?
a. IV theophylline
b. Montelukast (Singulair)
c. Inhaled hypertonic saline
d. Albuterol (Proventil HFA)
The mainstay of acute asthmatic treatment is inhalation of short-acting β2adrenergic agonist (SABA) bronchodilators, such as albuterol (ProAir HFA, Proventil HFA, Ventolin HFA). In patients with a moderate to severe attack, inhaled ipratropium (Atrovent) is used in conjunction with SABA. Salmeterol (Serevent Diskus) and montelukast (Singulair) are long-term control medications. Inhaled hypertonic saline is used in cystic fibrosis and bronchiectasis to help thin secretions. IV Theophylline is no longer recommended for the treatment of acute asthma attacks or in COPD exacerbations because of a very narrow therapeutic window, the availability of newer and more effective drugs, and, significant adverse effects (e.g., seizures and dysrhythmias).
7. The plan of care for the patient with chronic obstructive pulmonary disease (COPD) would include (select all that apply)
a. exercise such as walking.
b. high flow rate of O2 administration.
c. low-dose oral corticosteroid therapy.
d. use of monthly chest x-rays to monitor the progression of COPD.
e. breathing exercises, such as pursed-lip breathing that focus on exhalation.
Breathing exercises may assist the COPD patient during rest and activity (e.g., lifting, walking, stair climbing) by decreasing dyspnea, improving oxygenation, and slowing the respiratory rate. Walking (or other endurance exercises, such as cycling), combined with strength training, when possible, are probably the best interventions to strengthen muscles and improve the endurance of a patient with chronic obstructive pulmonary disease (COPD). Low dose oral corticosteroids may be appropriate for chronic COPD patients. Frequent chest x-rays are not needed.
8. What would the nurse include when teaching a patient how to use a metered-dose inhaler (MDI)?
a. After activating the MDI, breathe in as quickly as you can.
b. Estimate the amount of remaining medicine in the MDI by floating the canister in water.
c. Disassemble the plastic canister from the inhaler and rinse both pieces under running water every week.
d. To determine how long the canister will last, divide the total number of puffs in the canister by the puffs needed per day.
The patient needs to know the correct way to determine if the metered-dose inhaler (MDI) is empty. The patient should divide the total number of puffs in the canister by the puffs needed per day. The other three statements are not correct.
When caring for a patient with chronic obstructive pulmonary disease (COPD), the nurse determines that the patient’s nutrition status is impaired after noting a weight loss of 30 lb. Which intervention would the nurse add to the plan of care?
Order fruits and fruit juices to be offered between meals.
Order a high-calorie, high-protein diet with six small meals a day.
Provide a high-calorie, high-carbohydrate, nonirritating, frequent feeding diet.
Encourage the patient to double carbohydrate consumption and decrease fat intake.
Because the patient with COPD needs to use greater energy to breathe, there is often decreased oral intake because of dyspnea. A full stomach also impairs the ability of the diaphragm to descend during inspiration, thus interfering with the work of breathing. For these reasons, the patient with COPD would eat 6 small meals per day taking in a high-calorie, high-protein diet, with nonprotein calories divided evenly between fat and carbohydrate. The other interventions will not increase the patient’s caloric intake
A patient with chronic obstructive pulmonary disease (COPD) becomes dyspneic at rest. The baseline ABG results are PaO2 70 mm Hg, PaCO2 52 mm Hg, and pH 7.34. After assessing the patient, what new finding would require the nurse’s priority intervention?
Arterial pH 7.26
PaCO2 50 mm Hg
Patient in tripod position
Increased sputum expectoration
The patient’s pH shows acidosis that supports an exacerbation of COPD along with the worsening dyspnea. The PaCO2 has improved from baseline, the tripod position helps the patient’s breathing, and the increase in sputum expectoration will improve the patient’s ventilation.
Normal aterial ph range: 7.38 to 7.42. ph
During an assessment of a patient with asthma, the nurse notes wheezing and dyspnea. The nurse interprets that these symptoms are related to what pathophysiologic change?
Laryngospasm
Pulmonary edema
Narrowing of the airway
Overdistention of the alveoli
Narrowing of the airway by persistent but variable inflammation leads to reduced airflow, making it difficult for the patient to breathe and producing the characteristic wheezing. Laryngospasm, pulmonary edema, and overdistention of the alveoli do not produce wheezing
The nurse is evaluating if a patient understands how to safely determine whether a metered-dose inhaler (MDI) is empty. The nurse decides the patient understands this important information when the patient describes which method to check the inhaler?
Place it in water to see if it floats.
Keep track of the number of inhalations used.
Shake the canister while holding it next to the ear.
Check the indicator line on the side of the canister.
It is no longer appropriate to see if a canister floats in water or not because this is not an accurate way to determine the remaining inhaler doses. The best method to determine when to replace an inhaler is by knowing the maximum puffs available per MDI and then replacing it after the number of days when those inhalations have been used (100 puffs/2 puffs each day = 50 days)
Which test result identifies that a patient with asthma is responding to treatment?
An increase in CO2 levels
A decreased exhaled nitric oxide
A decrease in white blood cell count
An increase in serum bicarbonate levels
Nitric oxide levels are increased in the breath of people with asthma. A decrease in the exhaled nitric oxide concentration suggests that the treatment may be decreasing the lung inflammation associated with asthma and adherence to treatment. An increase in CO2 levels, decreased white blood cell count, and increased serum bicarbonate levels do not indicate a positive response to treatment in a patient with asthma.
The nurse is teaching a patient how to self-administer ipratropium via a metered-dose inhaler (MDI). Which instruction is most appropriate to help the patient learn the proper inhalation technique?
“Avoid shaking the inhaler before use.”
“Breathe out slowly before positioning the inhaler.”
“Using a spacer should be avoided for this type of medication.”
“After taking a puff, hold the breath for 30 seconds before exhaling.”
It is important to breathe out slowly before positioning the inhaler. This allows the patient to take a deeper breath while inhaling the medication, thus enhancing the effectiveness of the dose. The inhaler should be shaken well. A spacer may be used. Holding the breath after the inhalation of medication helps keep the medication in the lungs, but 30 seconds will not be possible for a patient with COPD.
When teaching the patient with cystic fibrosis about diet and medications, what priority information would the nurse include?
Fat-soluble vitamins and dietary salt should be avoided.
Insulin may be needed with a diabetic diet if diabetes develops.
Pancreatic enzymes and adequate fat, calories, protein, and vitamins are needed.
Distal intestinal obstruction syndrome (DIOS) can be treated with increased water.
The patient must take pancreatic enzymes before each meal and snack and adequate fat, calories, protein, and vitamins should be eaten. Fat-soluble vitamins are needed because they are malabsorbed with the excess mucus in the gastrointestinal system. Insulin may be needed, but there is no longer a diabetic diet, and this is not priority information at this time. DIOS develops in the terminal ileum and is treated with balanced polyethylene glycol electrolyte solution (MiraLAX) to thin bowel contents
The nurse is assigned to care for a patient in the emergency department with an asthma exacerbation. The patient has received a β-adrenergic bronchodilator and supplemental oxygen. If the patient’s condition does not improve, what would the nurse anticipate as the most likely next step in treatment?
IV fluids
Biofeedback therapy
Systemic corticosteroids
Pulmonary function testing
Systemic corticosteroids speed the resolution of asthma exacerbations and are indicated if the initial response to the β-adrenergic bronchodilator is insufficient. IV fluids may be used but not to improve ventilation. Biofeedback therapy and pulmonary function testing may be used after recovery to assist the patient and monitor the asthma.
A patient with bronchiectasis has copious thick respiratory secretions. Which intervention would the nurse include in the plan of care?
Use the incentive spirometer for at least 10 breaths every 2 hours.
Give prescribed antibiotics and antitussives on a scheduled basis.
Increase intake to at least 12 eight-ounce glasses of fluid every 24 hours.
Provide nutritional supplements that are high in protein and carbohydrates.
Adequate hydration helps to liquefy secretions and thus make it easier to remove them. Unless there are contraindications, the nurse should teach the patient to drink at least 3 L of fluid daily. Although nutrition, breathing exercises, and antibiotics may be indicated, these interventions will not liquefy or thin secretions. Antitussives may reduce the urge to cough and clear sputum, increasing congestion. Expectorants may be used to liquefy and facilitate clearing secretions
When teaching the patient with chronic obstructive pulmonary disease (COPD) about smoking cessation, what information would the nurse include about the effects of smoking on the lungs?
Smoking causes a hoarse voice.
Cough will become nonproductive.
Decreased alveolar macrophage function.
Sense of smell is decreased with smoking.
The damage to the lungs includes alveolar macrophage dysfunction that increases the incidence of infections and thus increases patient discomfort and cost to treat the infections. Other lung damage that contributes to infections includes cilia paralysis or destruction, increased mucus secretion, and bronchospasms that lead to sputum accumulation and increased cough. The patient may already be aware of respiratory mucosa damage with hoarseness and decreased sense of smell and taste, but these do not increase the incidence of pulmonary infection.
The nurse evaluates that nursing interventions to promote airway clearance in a patient admitted with chronic obstructive pulmonary disease (COPD) are successful based on which finding?
Absence of dyspnea
Improved mental status
Effective and productive coughing
PaO2 within normal range for the patient
Airway clearance is most directly evaluated as successful if the patient can engage in effective and productive coughing. Absence of dyspnea, improved mental status, and PaO2 within normal range for the patient show improved respiratory status but do not evaluate airway clearance
When admitting a patient with a diagnosis of asthma exacerbation, the nurse would assess for what potential triggers? (Select all that apply.)
Exercise
Allergies
Emotional stress
Decreased humidity
Upper respiratory infections
Although the exact mechanism of asthma is unknown, there are several triggers that may precipitate an attack. These include allergens, exercise, air pollutants, upper respiratory infections, drug and food additives, stress, and gastroesophageal reflux disease (GERD).
An adolescent patient with a history of frequent lung and sinus infections has symptoms consistent with undiagnosed cystic fibrosis (CF). Which information would be accurate for the nurse to include when teaching the patient about a scheduled sweat chloride test?
“Sweat chloride greater than 60 mmol/L is consistent with a diagnosis of CF.”
“The test measures the amount of sodium chloride in your postexercise sweat.”
“If sweating occurs after an oral dose of pilocarpine, the test result for CP is positive.”
“If the sweat chloride test result is positive on two occasions, genetic testing will be necessary.”
The diagnostic criteria for CF involve a combination of clinical presentation, sweat chloride testing, and genetic testing to confirm the diagnosis. Values above 60 mmol/L for sweat chloride are consistent with the diagnosis of CF. However, a second sweat chloride test is recommended to confirm the diagnosis, unless genetic testing identifies a CF mutation. Genetic testing is used if the results from a sweat chloride test are unclear
The patient with cystic fibrosis (CF) has been admitted to the unit. What intervention would the nurse include in the plan of care?
Strict bedrest
Fluid restrictions of 1500 mL a day
Aggressive chest physical therapy (CPT)
Limit diet intake of sodium-containing foods
Acute care for the patient with CF includes relief of bronchoconstriction, airway obstruction, and airflow limitation. Interventions include aggressive CPT, antibiotics, and O2 therapy in severe disease. Measures to optimize nutrition are important. There is no reason to limit foods containing sodium.
The nurse determines that the patient is not experiencing adverse effects of albuterol (Proventil) after noting which patient vital sign?
Temperature of 98.4°F
Oxygen saturation 96%
Pulse rate of 72 beats/min
Respiratory rate of 18/breaths
Albuterol is a β2-agonist that can sometimes cause adverse cardiovascular effects. These would include tachycardia and angina. A pulse rate of 72 beats/min indicates that the patient does not have tachycardia as an adverse effect
The nurse determines that therapy with ipratropium is effective after noting which assessment finding?
Decreased respiratory rate
Increased respiratory rate
Increased peak flow readings
Decreased sputum production
Ipratropium is a bronchodilator that should result in increased peak expiratory flow rates.
The nurse determines the patient with asthma has activity intolerance. What is the most likely reason for this problem?
Work of breathing
Fear of suffocation
Effects of medications
Anxiety and restlessness
When the patient does not have sufficient gas exchange to engage in activity, the etiologic factor is often the work of breathing. When patients with asthma do not have effective respirations, they use all available energy to breathe and have little left over for purposeful activity. Fear of suffocation, effects of medications or anxiety, and restlessness are not etiologies for activity intolerance for a patient with asthma
you are assessing your patient who is having difficulty breathing. For any patient with an acute asthmatic attack, which of the following medications should you offer for immediate relief of symptoms?
Beta blocker
Angiotensin-converting enzyme (ACE) inhibitor
Anti-immunoglobulin (IgE) antibodies
Beta 2 agonist, inhaled corticosteroids
The best options for treating a patient with an acute asthma attack would be either an inhaled β2-adrenergic agonist or corticosteroid. Beta blocker, ACE inhibitor, or IgE antibody therapies are not part of acute asthma management.
The nurse determines that the patient understood medication instructions about the use of a spacer device when taking inhaled medications if the patient states:
“I will pay less for medication because it will last longer.”
“More of the medication will get down into my lungs to help my breathing.”
“Now I will not need to breathe in as deeply when taking the inhaler medications.”
“This device will make it so much easier and faster to take my inhaled medications.”
A spacer assists more medication to reach the lungs, with less being deposited in the mouth and the back of the throat. It does not affect the cost or increase the speed of using the inhaler
In which position would the nurse place a patient experiencing an asthma exacerbation?
Supine
Lithotomy
High Fowler’s
Reverse Trendelenburg
The patient experiencing an asthma attack would be placed in high Fowler’s position and may need to lean forward to allow for optimal chest expansion and enlist the aid of gravity during inspiration. The supine, lithotomy, and reverse Trendelenburg positions will not facilitation ventilation.
The nurse is teaching a patient how to self-administer beclomethasone, 2 puffs inhaled every 6 hours. What would the nurse teach the patient to do to prevent oral infection while taking this medication?
Chew a hard candy before the first puff of medication.
Ask for a breath mint after the second puff of medication.
Rinse the mouth with water before each puff of medication.
Rinse the mouth with water after the second puff of medication.
Because beclomethasone is a corticosteroid, the patient should rinse the mouth with water after the second puff of medication to reduce the risk of fungal overgrowth and oral infection
The nurse has administered a first dose of oral prednisone to a patient with asthma. What parameter would the nurse begin to monitor?
Apical pulse
Daily weight
Bowel sounds
Deep tendon reflexes
Corticosteroids such as prednisone can lead to weight gain. For this reason, it is important to monitor the patient’s daily weight. The drug should not affect the apical pulse, bowel sounds, or deep tendon reflexes
The nurse supervises a team including another registered nurse (RN), a licensed practical/vocational nurse (LPN/VN), and assistive personnel (AP) on a medical unit in caring for many patients with respiratory problems. In what situation would the nurse intervene?
LPN/VN obtained a pulse oximetry reading of 94% but did not report it.
AP report to the nurse that the patient is reporting of difficulty breathing.
RN taught the patient about home oxygen safety in preparation for discharge.
LPN/VN changed the type of oxygen device based on arterial blood gas results.
It is not within the LPN scope to change oxygen devices based on analysis of lab results. It is within the scope of practice of the RN to assess, teach, and evaluate. The LPN provides care for stable patients and may adjust oxygen flow rates depending on desired oxygen saturation levels of stable patients. The AP may obtain oxygen saturation levels, assist patients with comfort adjustment of oxygen devices, and report changes in patient’s level of consciousness or difficulty breathing
When planning teaching for the patient with chronic obstructive pulmonary disease (COPD), the nurse understands the manifestations of the disease are related to what process?
An overproduction of the antiprotease a1-antitrypsin
Hyperinflation of alveoli and destruction of alveolar walls
Hypertrophy and hyperplasia of goblet cells in the bronchi
Collapse and hypoventilation of the terminal respiratory unit
In COPD, structural changes include hyperinflation of alveoli, destruction of alveolar walls, destruction of alveolar capillary walls, narrowing of small airways, and loss of lung elasticity. An autosomal recessive deficiency of antitrypsin may cause COPD. Not all patients with COPD have excess mucus production by the increased number of goblet cells
A patient has been receiving oxygen per nasal cannula while hospitalized for chronic obstructive pulmonary disease (COPD). The patient asks the nurse whether oxygen use will be needed at home. What is the most appropriate response by the nurse?
“Long-term home oxygen therapy should be used to prevent respiratory failure.”
“Oxygen will not be needed unless you are in the terminal stages of this disease.”
“Long-term home oxygen therapy should be used to prevent heart problems related to COPD.”
“You will not need oxygen until your oxygen saturation drops to 88% and you have symptoms of hypoxia.”
Long-term oxygen therapy in the home will not be considered until the oxygen saturation is less than or equal to 88% and the patient has signs of tissue hypoxia, such as cor pulmonale, erythrocytosis, or impaired mental status. PaO2 less than 55 mm Hg will also allow home oxygen therapy to be considered.
What symptoms would the nurse teach the patient with bronchiectasis to report to the health care provider?
Increasing dyspnea
Temperature below 98.6°F
Decreased sputum production
Unable to drink 3 L of low-sodium fluids
The significant manifestations to report to the health care provider include increasing dyspnea, fever, chills, increased sputum production, bloody sputum, and chest pain. Although drinking at least 3 L of low-sodium fluid will help liquefy secretions to make them easier to expectorate, the health care provider does not need to be notified if the patient cannot do this one day.
Before discharge, the nurse discusses activity levels with an older adult patient with chronic obstructive pulmonary disease (COPD) and pneumonia. Which exercise goal is most appropriate after the patient has recovered from this episode of illness?
Slightly increase activity over the current level.
Swim for 10 min/day, gradually increasing to 30 min/day.
Limit exercise to activities of daily living to conserve energy.
Walk for 20 min/day, keeping the pulse rate less than 130 beats/min.
The patient will benefit from mild aerobic exercise that does not stress the cardiorespiratory system. The patient should be encouraged to walk for 20 min/day, keeping the pulse rate less than 75% to 80% of maximum heart rate (220—patient’s age).
The nurse determines that a patient is experiencing common adverse effects from the inhaled corticosteroid beclomethasone after what occurs?
Hypertension and pulmonary edema
Oropharyngeal candidiasis and hoarseness
Elevation of blood glucose and calcium levels
Adrenocortical dysfunction and hyperglycemia
Oropharyngeal candidiasis and hoarseness are common adverse effects from the use of inhaled corticosteroids because the medication can lead to overgrowth of organisms and local irritation if the patient does not rinse the mouth following each dose
While teaching a patient with asthma about the appropriate use of a peak flow meter, what would the nurse teach the patient to do?
Keep a record of the peak flow meter numbers if symptoms of asthma are getting worse.
Increase the dose of the long-term control medication if the peak flow numbers decrease.
Use the flowmeter each morning after taking medications to evaluate their effectiveness.
Empty the lungs and then inhale quickly through the mouthpiece to measure how fast air can be inhaled.
It is important to keep track of peak flow readings daily, especially when the patient’s symptoms are getting worse. The patient should have specific directions as to when to call the provider based on personal peak flow numbers. Peak flow is measured by exhaling into the flowmeter and would be assessed before and after medications to evaluate their effectiveness.
The provider has prescribed salmeterol (Serevent) for a patient with asthma. In reviewing the use of dry powder inhalers (DPIs) with the patient, what instructions would the nurse provide?
“Close lips tightly around the mouthpiece and breathe in deeply and quickly.”
“To administer a DPI, you must use a spacer that holds the medicine so that you can inhale it.”
“You will know you have correctly used the DPI when you taste or sense the medicine going into your lungs.”
“Hold the inhaler several inches in front of your mouth and breathe in slowly, holding the medicine as long as possible.”
The patient would be instructed to tightly close the lips around the mouthpiece and breathe in deeply and quickly to ensure the medicine moves down deeply into the lungs. Dry powder inhalers do not require spacer devices. The patient may not taste or sense the medicine going into the lungs
The nurse is caring for a patient with an acute exacerbation of asthma. After initial treatment, what assessment finding indicates to the nurse that the patient’s respiratory status is improving?
Wheezing becomes louder.
Cough remains nonproductive.
Vesicular breath sounds decrease.
Aerosol bronchodilators stimulate coughing.
The primary problem during an exacerbation of asthma is narrowing of the airway and subsequent diminished air exchange. As the airways begin to dilate, wheezing gets louder because of better air exchange. Vesicular breath sounds will increase with improved respiratory status. After a severe asthma exacerbation, the cough may be productive and stringy. Coughing after aerosol bronchodilators may indicate a problem with the inhaler or its use
Which statement made by the patient with chronic obstructive pulmonary disease (COPD) indicates a need for further teaching about the use of an ipratropium inhaler?
“I should wait at least 1 to 2 minutes between each puff of the inhaler.”
“I can rinse my mouth following the two puffs to get rid of the bad taste.”
“Because this medication is not fast acting, I cannot use it in an emergency if my breathing is worse.”
“If my breathing gets worse, I should keep taking extra puffs of the inhaler until I can breathe more easily.”
The patient should not just keep taking extra puffs of the inhaler to make breathing easier. Excessive treatment could trigger paradoxical bronchospasm, which would worsen the patient’s respiratory status. Rinsing the mouth after the puffs will eliminate a bad taste. Waiting 1 to 2 minutes between each puff will facilitate the effectiveness of the administration. Ipratropium is not used in an emergency for COPD.
A middle aged patient with asthma is brought to the emergency department by automobile. He is short of breath and appears frightened. During the initial nursing assessment, which finding would be an early sign of an asthma exacerbation?
Anxiety
Cyanosis
Bradycardia
Hypercapnia
An early manifestation of an asthma attack is anxiety because the patient is acutely aware of the inability to get sufficient air to breathe. He will be hypoxic early on with decreased PaCO2 and increased pH as he is hyperventilating. If cyanosis occurs, it is a later sign. The pulse and blood pressure will be increased.
The nurse is assigned to care for a patient who has anxiety and an asthma exacerbation. What is the primary reason for the nurse to carefully inspect the patient’s chest wall?
Giving care will calm the patient
Observing for signs of diaphoresis
Evaluating the use of intercostal muscles
Monitoring the patient for bilateral chest expansion
The nurse physically inspects the chest wall to evaluate the use of intercostal (accessory) muscles, which gives an indication of the degree of respiratory distress. The other options may also occur, but they are not the primary reason for inspecting the chest wall of this patient.
The nurse teaches a patient with chronic obstructive pulmonary disease (COPD) how to administer fluticasone by metered-dose inhaler (MDI). Which statement indicates a correct understanding of the instructions?
“I should not use a spacer device with this inhaler.”
“I will rinse my mouth each time after I use this inhaler.”
“I will feel my breathing improve over the next 2 to 3 days.”
“I should use this inhaler immediately if I have trouble breathing.
Fluticasone may cause oral candidiasis (thrush). The patient should rinse the mouth with water or mouthwash after use or use a spacer device to prevent oral fungal infections. Fluticasone is an inhaled corticosteroid and it may take 2 weeks of regular use for effects to be evident. This medication is not recommended for an acute asthma attack.
Assessment findings of jugular venous distention and pedal edema would be indicative of what complication of chronic obstructive pulmonary disease (COPD)?
Acute respiratory failure
Secondary respiratory infection
Fluid volume excess from cor pulmonale
Pulmonary edema caused by left-sided heart failure
Cor pulmonale is a right-sided heart failure caused by resistance to right ventricular outflow resulting from lung disease. With failure of the right ventricle, the blood emptying into the right atrium and ventricle would be slowed, leading to jugular venous distention and pedal edema.