ap bio - the immune system
innate immunity
overview
innate: you get from just being born
barriers help an animal defend itself from many dangerous pathogens it may encounter
the immune system recognizes foreign bodies (not self) and responds with the production of immune cells and proteins.
two major kinds of defense have evolved: innate immunity vs. acquired immunity
innate immunity is present before any exposure to pathogens and is effective from birth; nonspecific responses to pathogens. innate immunity consists of external barrier, internal cellular, and chemical defenses.
acquired immunity is adaptive immunity: develops after exposure to agents such as microbes, toxins, or other foreign substances; has a very specific response to pathogens.
for innate immunity, recognition and response rely on shared traits of pathogens.
the immune system recognizes bacteria and fungi by structures on their cell walls. immune response varies with the class of pathogen encountered.
innate immunity defences of vertebraes:
innate defenses:
barrier defenses
phagocytosis
antimicrobial peptides
inflammatory response
natural killer cells
some pathogens avoid destruction by modifying their surface to prevent recognition or by resisting breakdown following phagocytosis (ex. tuberculosis)
barrier defenses
barrier defenses include
skin
mucous membranes of the respiratory, urinary, and reproductive tracts
mucus traps and allows for the removal of microbes
many body fluids including saliva, mucus, and tears are hostile to microbes
the low pH of skin and the digestive system prevents the growth of microbes.
phagocytosis
white blood cells: some leukocytes engulf pathogens in the body via phagocytosis.
a phagocytic white blood cell engulfs a microbe, then fuses with a lysosome to destroy the microbe.
there are different types of phagocytic cells:
neutrophils: engulf and destroy microbes, first on the scene and die afterward, become pus
eosinophils: discharge destructive enzymes
macrophages and dendritic cells: stimulate the development of acquired immunity. *antigen presenting cell
phagocytosis: cell eating cell that consumes any invader that doesn’t have correct cell surface marker - generic phagocytosis of a pathogen is not an antigen presenting cell
lymphatic system: part of circulatory and immune system, moves fluid from interstitial spaces back into the blood
antimicrobial peptides
peptides and proteins attack microbes directly and impede their reproduction.
interferon proteins: a virus-infected cell will release interferons causing nearby cells to heighten their anti-viral defenses, sort of like an alarm.
complement system: cause lysis of invading cells and helps trigger inflammation
inflammatory responses
following injury, mast cells release histamine, which promotes changes in blood vessels to make them leaky. this is part of the inflammatory response and can lead to swelling at the sight of an injury.
changes increase local blood supply and allow more phagocytes and antimicrobial proteins to enter tissues through dilated blood vessels caused by histamine
pus: fluid rich in white blood cells, dead microbes, and cell debris, accumulated at site of inflammation
inflammation can be either local or systemic.
fever: systemic inflammatory response triggered by pyrogens released by macrophages and toxins from pathogens.
septic shock: life-threatening condition caused by an overwhelming inflammatory response.
natural killer cells
MHC: major histocompatibility complex; surface protein marker that is part of the extracellular matrix
all nucleated body cells (except red blood cells) have a class I MHC protein on their surface (name tag)
class II MHC protein is found on specialized cells.
cancerous or infected cells no longer express this MHC protein or they’re altered in some way— natural killer cells attack these damaged cells (SHOW ME YOUR PAPERS!)
acquired immunity
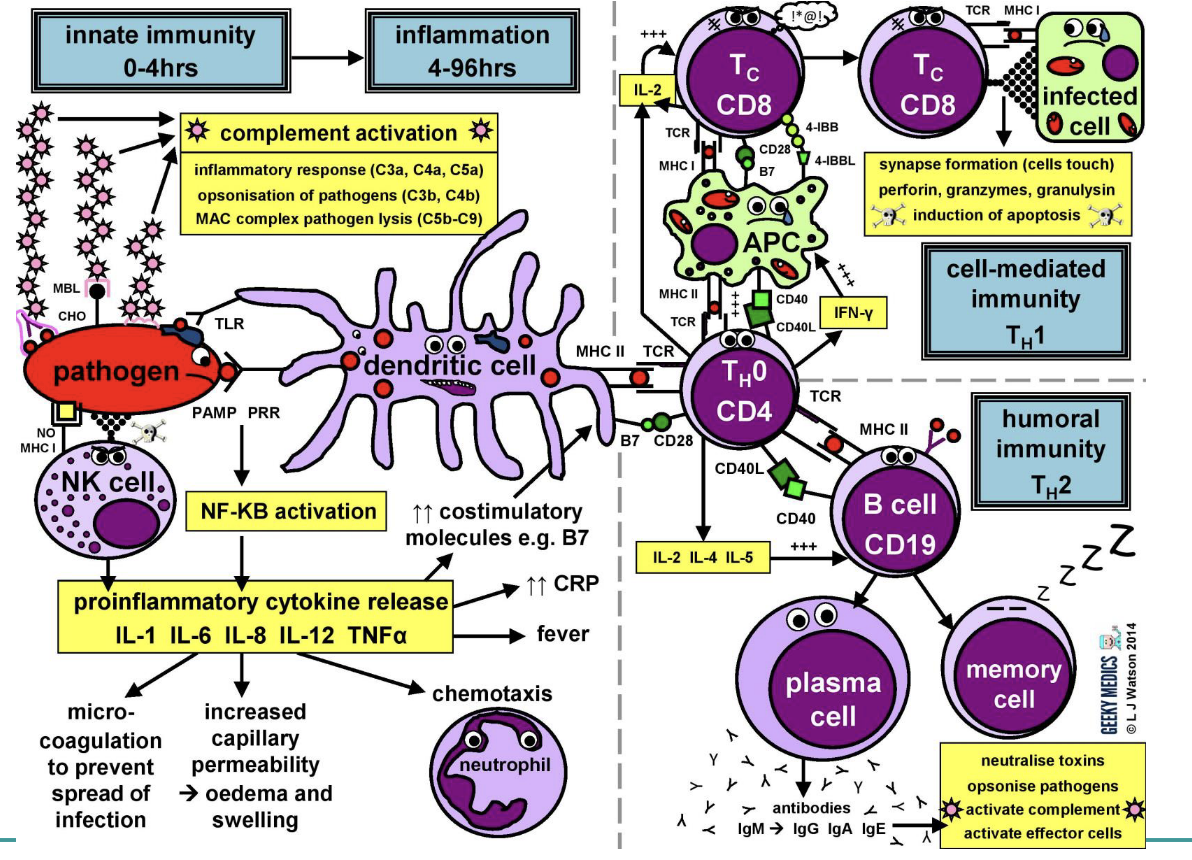
overview
in acquired immunity, lymphocyte receptors provide pathogen-specific recognition.
white blood cells called lymphocytes recognize and respond to antigens and foreign molecules.
lymphocytes:
t cells that mature in the thymus above the heart
b cells that mature in bone marrow
lymphocytes contribute to immunological memory, an enhanced response to a foreign molecule previously encountered.
active immunity: specific
b and t cells have receptor proteins that can bind to foreign molecules.
each individual lymphocyte is specialized to recognize a specific type of molecule.
antigen: any foreign molecule to which a lymphocyte responds
a single b or t cell has about 100,000 identical antigen receptors.
antigen receptors on b and t lymphocytes bind to very specifically shaped antigens.
all antigen receptors on a single lymphocyte recognize the same epitope, or antigenic determinant, on an antigen.
b cells give rise to plasma cells, which secrete proteins called antibodies or immunoglobulins.
role of MHC
all nucleated cells have a class I MHC that identifies itself (nametag / papers)
in infected cells, a portion of the pathogens antigen is presented on the MHC, thus altering its shape (surrenders for a mercy kill from the natural killer cells)
nearby t cell can detect antigen fragment being displayed on cell surface
— finish notes from day 3
day 4
active immunity
active immunity develops naturally in response to an infection
it can also develop following/from immunization, also called vaccination (actual exposure)
in immunization, a nonpathogenic form of a microbe of part of a microbe elicits an immune response to an immunological memory, which leads to the secondary immune response when encountered again.
passive immunity
passive immunity provides immediate, short-term protection from antibodies made from someone else.
it is conferred naturally:
IgG crosses the placenta from mother to fetus
IgA passes from mother to infant in breast milk
it can also be conferred artificially by injecting antibodies extracted from someone with immunity into a nonimmune person.
immune rejection
immune rejection: cells transferred from one person to another can be attacked by immune defenses
MHC molecules are different among genetically nonidentical individuals; differences in MHC molecules stimulate rejection of tissue grafts and organ transplants
chances of successful transplantation increase if donor and recipient MHC tissue types are well matched.
immunosuppressive drugs facilitate transplantation
lymphocytes in bone marrow transplants may cause the donor tissue to reject the recipient
blood groups
antigens on red blood cells surface determine whether a person has a blood type A (A antigen), B (B antigen), AB (both A and B antigens) or O (neither antigen).
antibodies to nonself blood types exist in the body; transfusion with incompatible blood leads to the destruction of the transfused cells.
recipient-donor combinations can be fatal or safe.
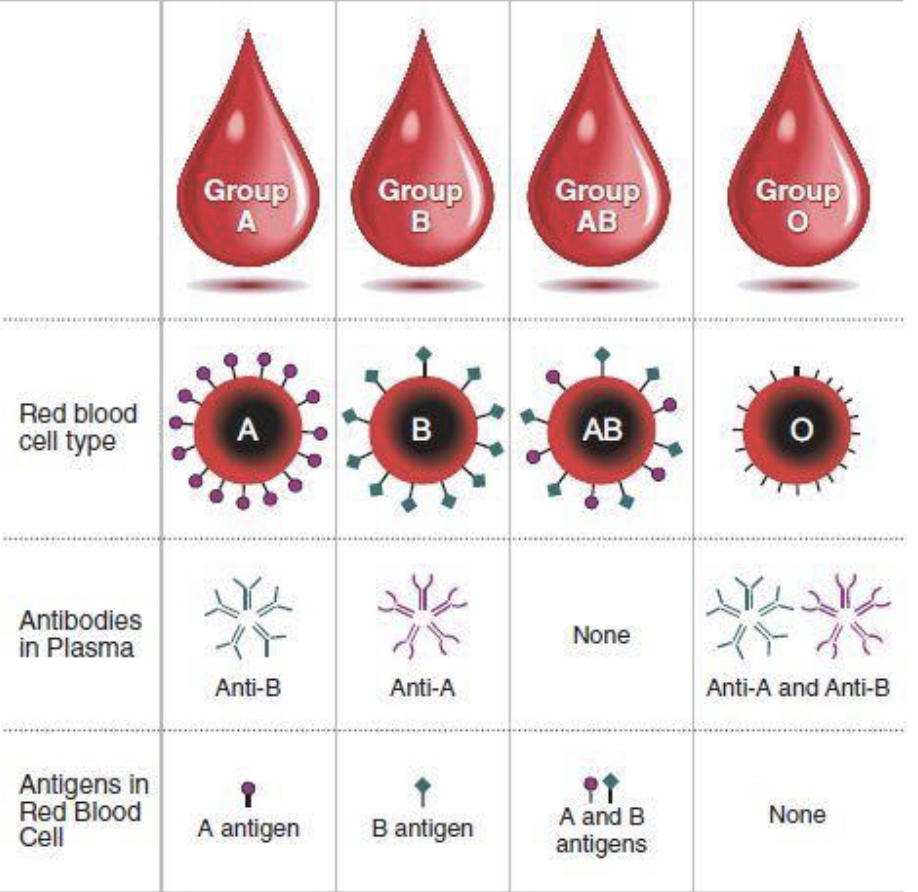
+ or - rhesus factor
allergies
allergies are exaggerated responses to antigens called allergens
in localized allergies such as hay fever, IgE antibodies produced after first exposure to an allergen attach to receptors on mast cells
the next time the allergen enters the body, it binds to mast cell-associated IgE molecules
mast cell release histamine and other mediators that cause vascular changes leading to typical allergy symptoms
an acute allergic response can lead to anaphylactic shock, a life-threatening reaction that can occur within seconds of allergen exposure