Biology 275: Basic Human Anatomy and Physiology I
Biology 275: Basic Human Anatomy and Physiology I
Anatomy vs Physiology:
Anatomy is the study of the structure and form of the body, whereas physiology is the study of function of these parts
It is effective to learn anatomy and physiology by integrating the two disciplines, rather than trying to separate the study of form from the study of function
Levels of Organization
Characteristics that describe living things:
- Organization,
- Metabolism,
- Growth and development
- Responsiveness
- Regulation
- Reproduction
Simplest to most complex:
- Chemical level
- Cellular level
- Tissue level
- Organ level
- Organ system level
- Organismal level
Polar vs. Nonpolar Molecules
- Nonpolar molecules are composed predominantly of nonpolar bonds between the atoms
- Polar molecules are composed of relatively more polar bonds between the atoms
- Amphipathic molecules are large molecules that have both nonpolar and polar regions
Properties of Water
- Cohesion is attraction between water molecules
- Surface tension is the inward pull of water molecules at the surface
- Adhesion is the attraction of water molecules for substances other than water
- Water's high specific heat and high heat of vaporization help maintain a normal body temperature
Components of Homeostatic System
- Receptor: detects a stimulus
- Control center: interprets input from the receptor and initiates changes through the effector
- Effector: the structure that brings about a change to the stimulus
Enzyme Function and Action
Function: biologically active catalysts that increase reaction rates by lowering the activation energy
Action: participate in both decomposition and synthesis reactions
Reaction Rates: dependent upon the concentrations of both the enzyme and substrate, temperature, and pH
Control: controlled by either competitive or noncompetitive inhibitors
Metabolic Pathways:
- The pathway involves numerous enzymes that subsequently convert a substrate to a final product
- Regulated by negative feedback to maintain the needed amount of the final product
Multienzyme Complexes:
- A structure composed of enzymes physically linked to convert a substrate to a final product
Cellular Respiration*
Glucose Oxidation:
- The net chemical reaction for glucose oxidation is C6H12O6 + 6O2 → CO2 to 6H2O
- ATP is produced directly through substrate-level phosphorylation and indirectly by oxidative phosphorylation
Glycolysis:
- Occurs within the cytosol, a metabolic pathway that uses 10 enzymes and does not require oxygen
- Glucose is converted to 2 pyruvate, producing 2 ATP and 2 NADH per glucose
- Fate of pyruvate is dependent upon availability of oxygen
Intermediate Stage:
- Occurs within mitochondria
- Pyruvate dehydrogenase converts pyruvate to acetyl CoA and releases 1CO2
- One NADH produced per pyruvate
- Occurs twice per the original glucose
Citric Acid Cycle:
- Occurs within mitochondria
- Breaks down acetyl CoA with 2CO2 and CoA released
- 1 ATP, 3 NADH, 1 FADH2 molecule are produced per acetyl CoA
- Occurs twice, and completes digestion of glucose
Electron Transport System:
- Involves several structures that are embedded in the cristae membrane of a mitochondrion
- H+ pumps, electron carriers, ATP synthase
- Electrons from NADH and FADH2 are transferred to electron carriers in the electron transport chain of a mitochondrion, and ultimately to O2
- Electrons, oxygen, and hydrogen ions form H2O
- A H+ ion gradient is formed: H+ ions then flow down this gradient and the energy is harnessed by ATP synthase to produce ATP through oxidative phosphorylation
ATP Production:
- Glucose oxidation produces a net of 2 ATP in glycolysis and 30 ATP in the complete breakdown of glucose
- NET: 32 total
Macromolecules
Characteristics:
- Have diverse carbon skeletons with varying amounts of hydrogen and functional groups attached to them
Polymers: complex carbohydrates, nucleic acids, proteins
- All of the classes of biological macromolecules are formed by dehydration synthesis reactions and digested through hydrolysis
Lipids:
- Fattylike, water-insoluble molecules that include triglycerides, phospholipids, steroids, and eicosanoids
Carbohydrates:
- Include monosaccharides, disaccharides, and polysaccharides
- Glucose is the most common monosaccharide in the human body and is used for energy
Nucleic Acids:
- Include DNA and RNA polymers formed from nucleotide monomers
Proteins:
- Polymers that differ in number and sequence of 20 different amino acid monomers arranged in a unique linear sequence
Many functions:
- Catalyze chemical reactions
- Structural support
- Body movement
- Transport in the blood
- Membrane transport
- Protection
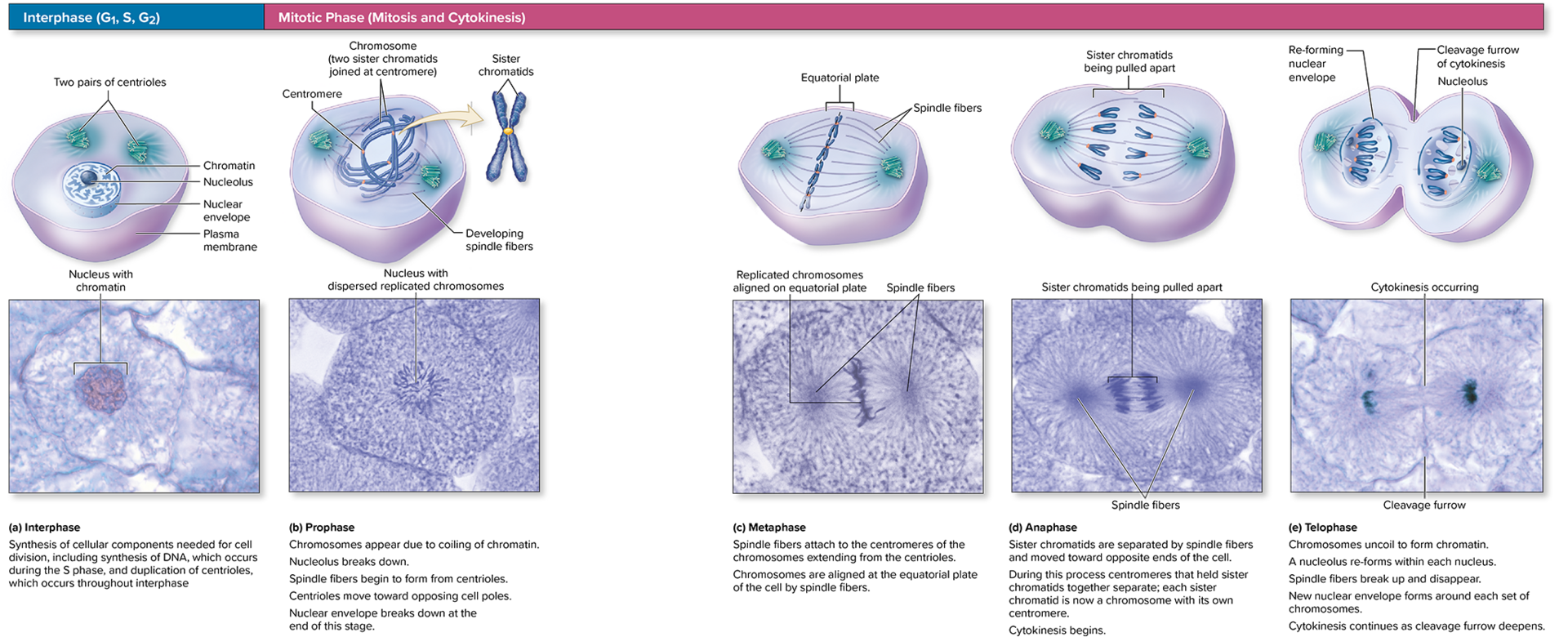
Mitosis
Function of Bone
- Support and protection
- Levers for movement
- Hematopoiesis
- Storage of minerals and energy reserves
Plasma Membrane
Lipid Components:
- Composed of a bilayer of phospholipids with embedded cholesterol molecules
- Glycolipids are lipids with carbohydrates extending from the outer surface of the cell
Membrane Proteins:
- Plasma membrane proteins are integral proteins that extend through the plasma membrane
- Peripheral proteins reside on either the internal or external surface of the plasma membrane
- Transport proteins, receptors, identity markers, enzymes, attachment sites for the cytoskeleton, cell-adhesion proteins
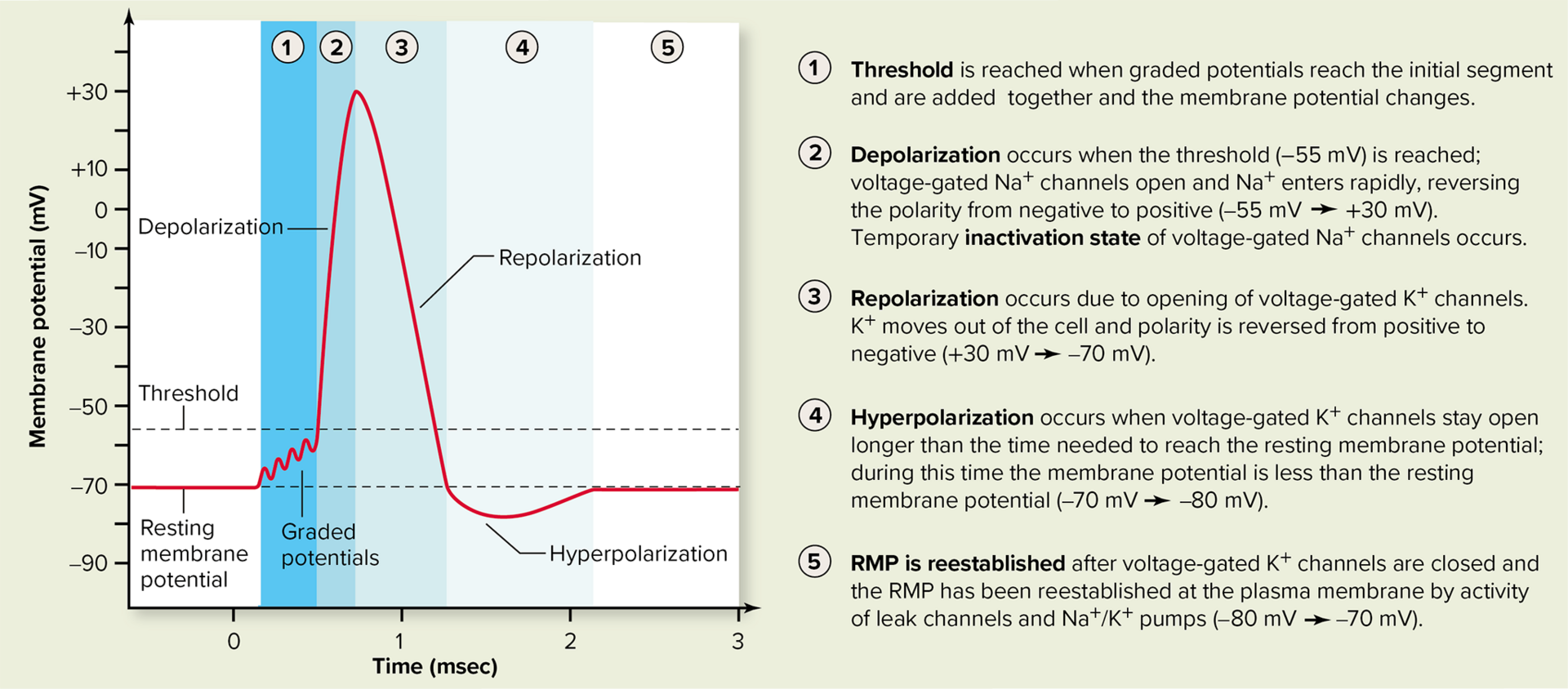
Action Potentials and Graded Potentials
- Graded potentials are short-lived electrical signals that occur in the dendrites and cell body due to the opening of chemically gated channels
- Action potentials are self-propagating electrical signals that are initiated in the initial segment, propagated along an axon, and result from the sequential opening of voltage-gated channels
Physiologic Events in the Neuron Segments:
Receptive Segment:
- Dendrites and cell body
- Formation and propagation of graded potentials (EPSP and IPSP)
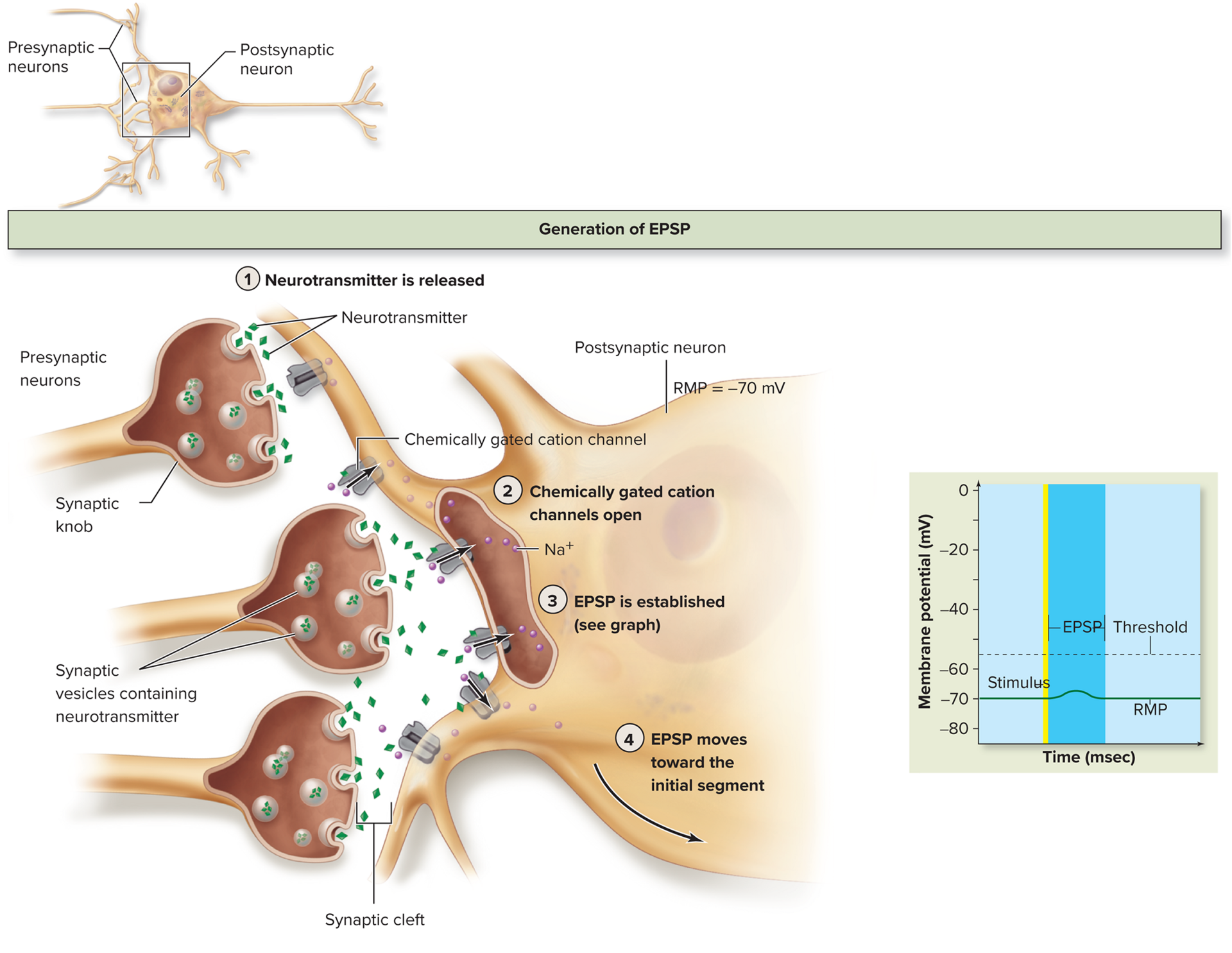
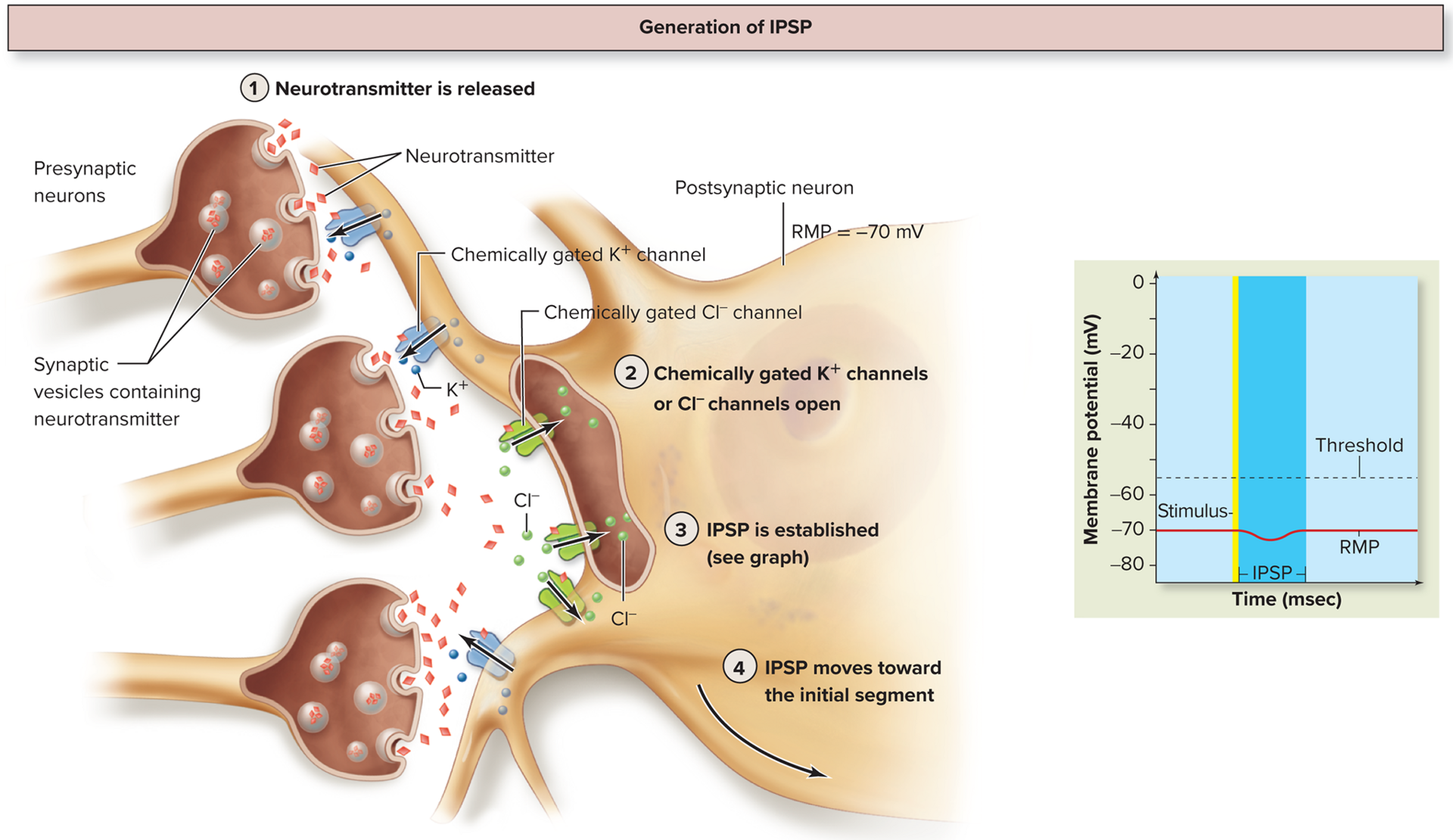
Initial Segment:
- Summation of EPSPs and IPSPs that reach the initial segment determines whether the threshold value (-55mV) is reached and an action potential is initiated
Conductive Segment:
- Propagation of an action potential along an axon (depolarization and repolarization
- The brief period of time that an axon is either incapable of generating an action potential or a greater than normal amount of stimulation is required to generate another action potential is called the refractory period
- Saltatory conduction occurs if the axon is myelinated
Transmissive Segment:
- Involves exocytosis of neurotransmitter from synaptic vesicles, which are located within synaptic knobs
The Stress Response
- Alarm Reaction:
- Hypothalamus activates the sympathetic division with subsequent stimulation of the adrenal medulla to release epinephrine and norepinephrine into the blood
Effects:
- Pupils dilate
- Bronchioles dilate
- Respiration rate increases
- Vasoconstriction
- Increased blood volume
- Increased cardiac output
- K+ and H+ ions are excreted
- Glucose and lipid levels in the blood increase
- Sweating increases
- Digestion and urine production activities decrease
- Stage of Resistance:
- Occurs after a few hours as glycogen stores in the liver deplete
- Induced by the release of glucocorticoids
- Function is to provide increased energy demands
- Glucose is needed by nervous tissue as it is a main nutrient for cellular respiration
- Gluconeogenesis is increased in liver and glucose is released into blood
- Glycerol and fatty acids increase due to increased lipolysis in adipose connective tissue
- Increased protein catabolism
- Net result: elevated glucose levels
- Stage of Exhaustion:
- Occurs after weeks or months
- Fat stores in adipose connective tissue are depleted
- Structural proteins of the body’s cells continue to be broken down for gluconeogenesis
- Body becomes weak because of this
- Elevated levels of aldosterone causes fluid, electrolyte, and pH imbalances
- This combo can cause organ failure and death
Glial Cells
CNS:
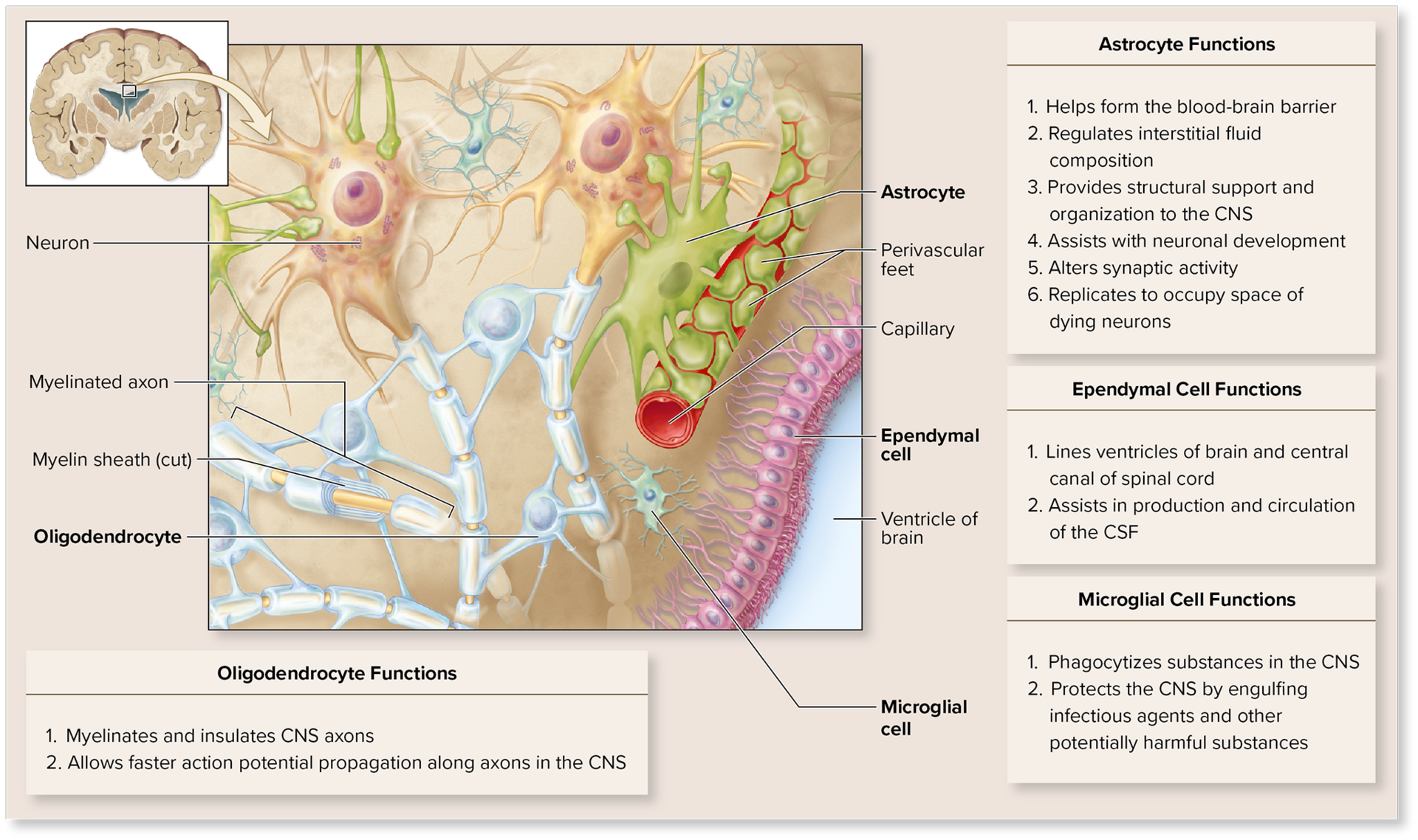
Astrocytes:
- Helps form blood-brain barrier
- Regulates interstitial fluid composition
- Structural support and organization to theCNS
- Assist with neuronal development
- Alters synaptic activity
- Replicates to occupy space of dying neurons
Ependymal Cell:
- Lines ventricles of brain central canal of spinal cord
- Assists in the production and circulation of CSF
Microglial Cell:
- Phagocytizes substances in the CNS
- Protects the CNS by engulfing infectious agents and other potentially harmful substances
Oligodendrocyte:
- Myelinates and insulates CNS axons
- Allows faster action potential propagation along axons in the CNS
PNS:
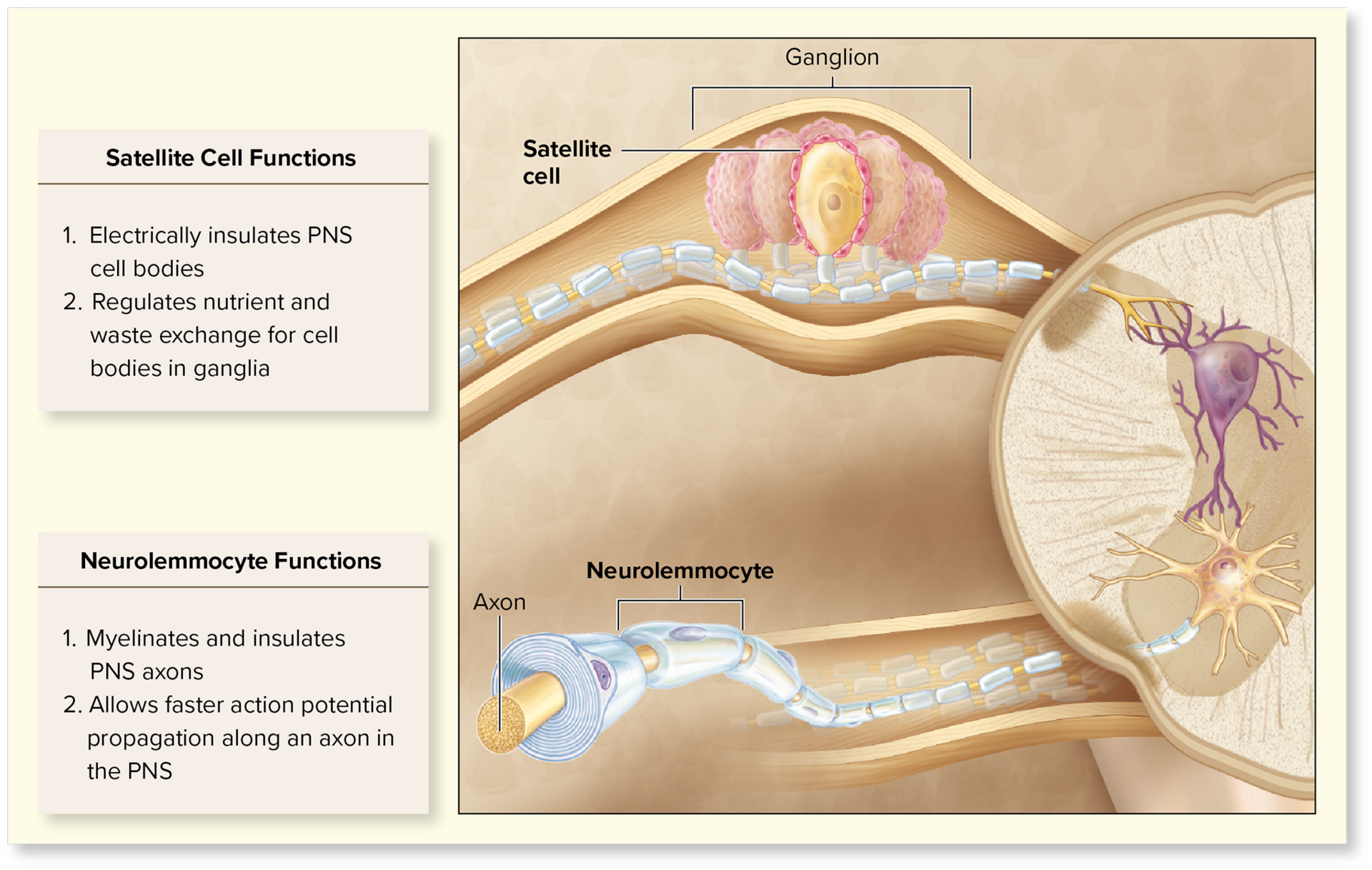
Satellite Cell:
- Electrically insulate PNS cell bodies
- Regulates nutrient and waste exchange for cell bodies in ganglia
Neurolemmocyte:
- Myelinates and insulates PNS axons
- Allows faster action potential propagation along an axon in the PNS
Types of Bone Growth
Intramembranous Ossification: bone formation that takes place within a membrane; formation of flat bones of the skull. It begins when mesenchyme becomes thickened and condensed with a dense supply of blood capillaries.
- Ossification Centers form within thickened regions of mesenchyme beginning at the 8th week of development:
- Cells thickened, mesenchyme divides, committed cells differentiate into osteoprogenitor cells
- Multiple ossification centers develop and rapid mitosis of osteoblasts occurs
- Osteoid undergoes calcification:
- Calcification entraps osteoblasts with the lacunae, these osteoblasts turn into osteocytes
- Woven bone (immature/unorganized) and its surrounding periosteum form:
- The newly formed bone connective tissue is not well organized, this is woven bone (primary bone)
- Woven bone is replaced by lamellar bone (secondary bone)
- Mesenchyme that surrounds woven bone begins to thicken and organize to form the periosteum
- Lamellar bone replaces woven bone, as compact and spongy bone form
- On the internal and external surfaces of bone, spaces between the trabeculae are modified and produce spongy bone
Endochondral Ossification: begins with a hyaline cartilage model and produces most bones of the skeleton
Weeks 8-12 Gestation:
- Fetal hyaline cartilage model develops
Fetal Period:
- Cartilage calcifies, and a periosteal bone collar forms around the diaphysis
- Primary ossification center forms in the diaphysis
Newborn to Child:
- Secondary ossification centers form in the epiphysis
Child:
- Bone replaces cartilage, except the articular cartilage, and the epiphyseal plates
Late teens to adult:
- Epiphyseal plates ossify and form epiphyseal lines
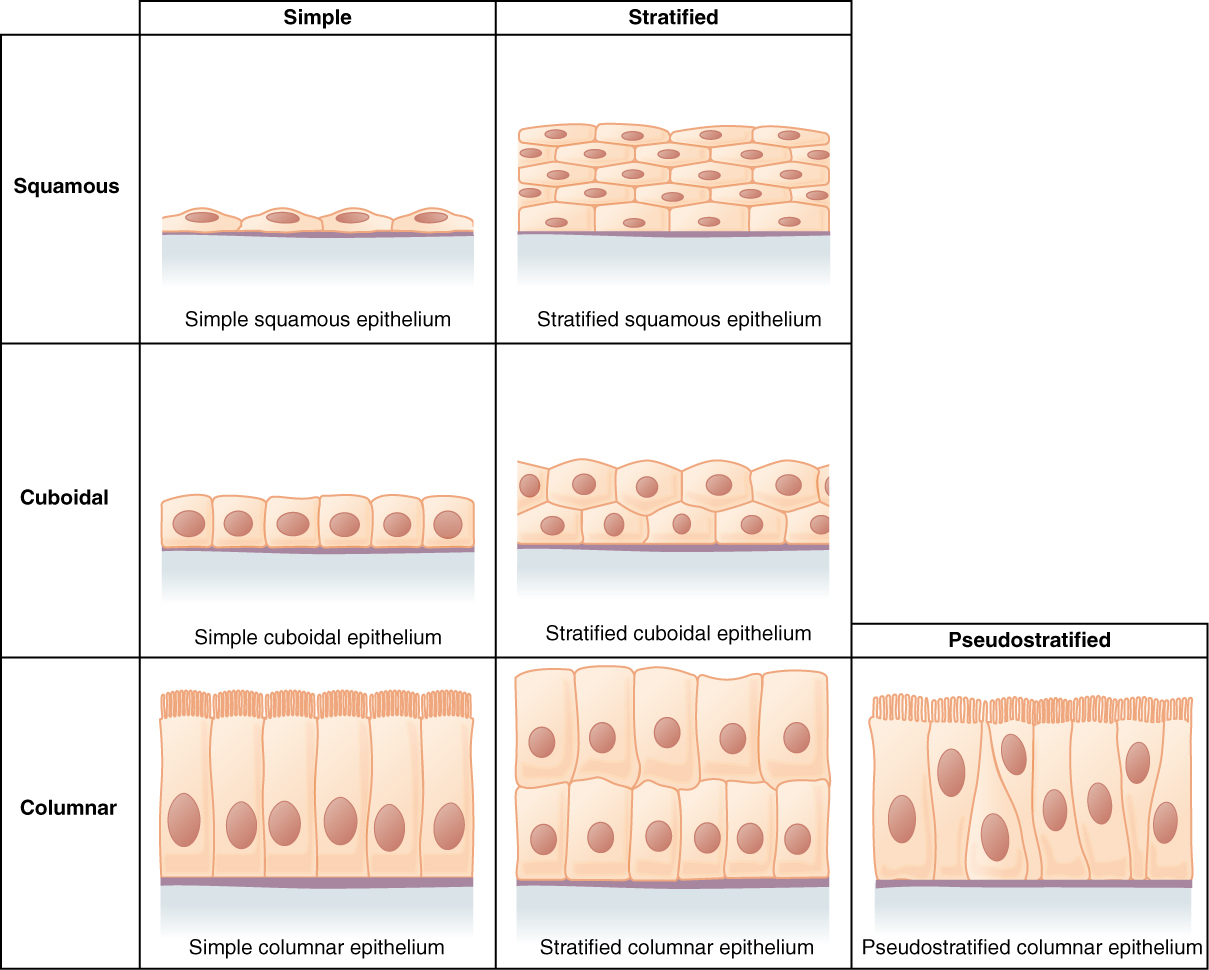
Types of Tissues
Epithelial Tissue:
- covers the surface of the body, lines body cavities and covers organs, and forms secretory structures called glands
Characteristics:
- Cellularity
- Polarity
- Attachment to basement membrane
- Avascularity
- Rich innervation
- High regenerative capacity
Functions:
- Physical protection
- Selectively permeable
- Produce secretions
- Nerve endings for stimuli
Classification:
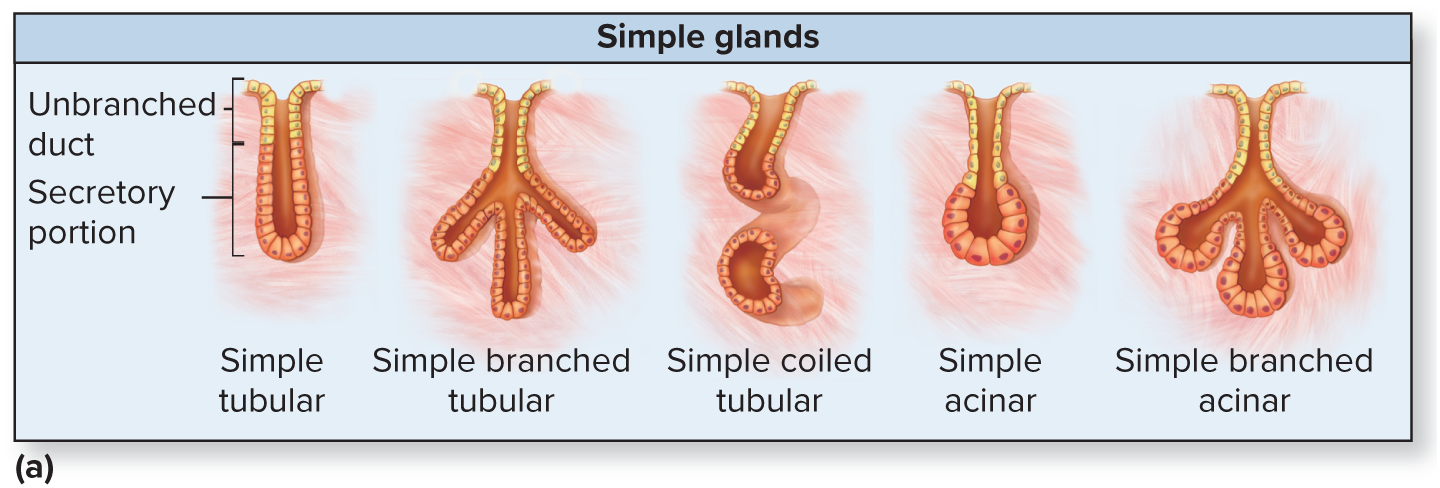
Exocrine Glands:
- Secrete products through ducts that release onto the epithelial surface
Anatomic Form:
- Simple vs. compound
- Tubular vs. acinar
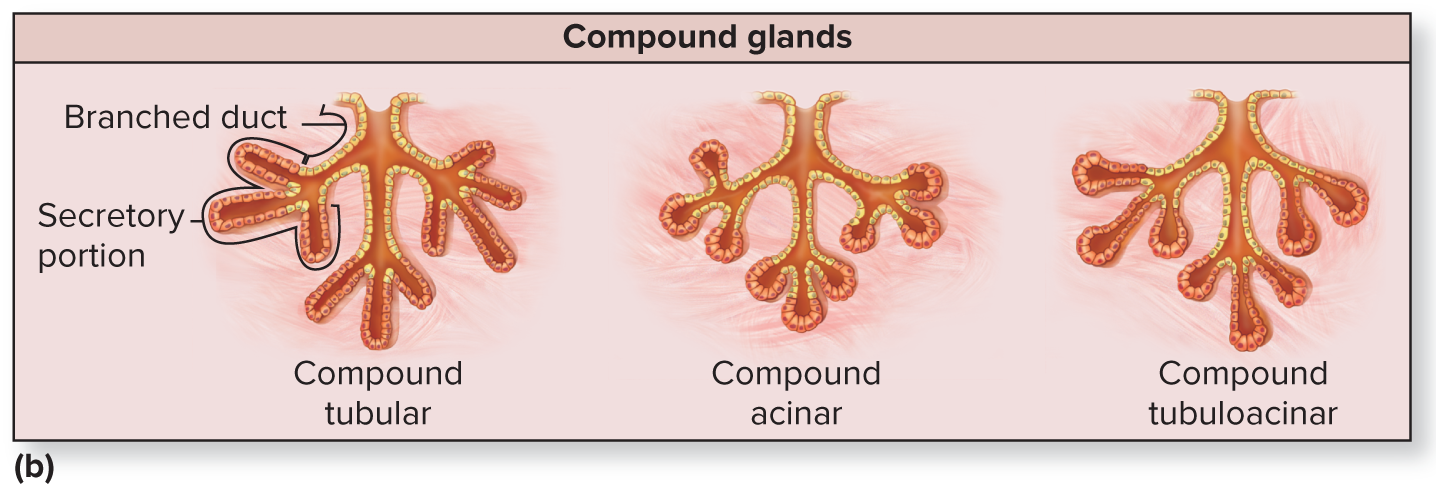
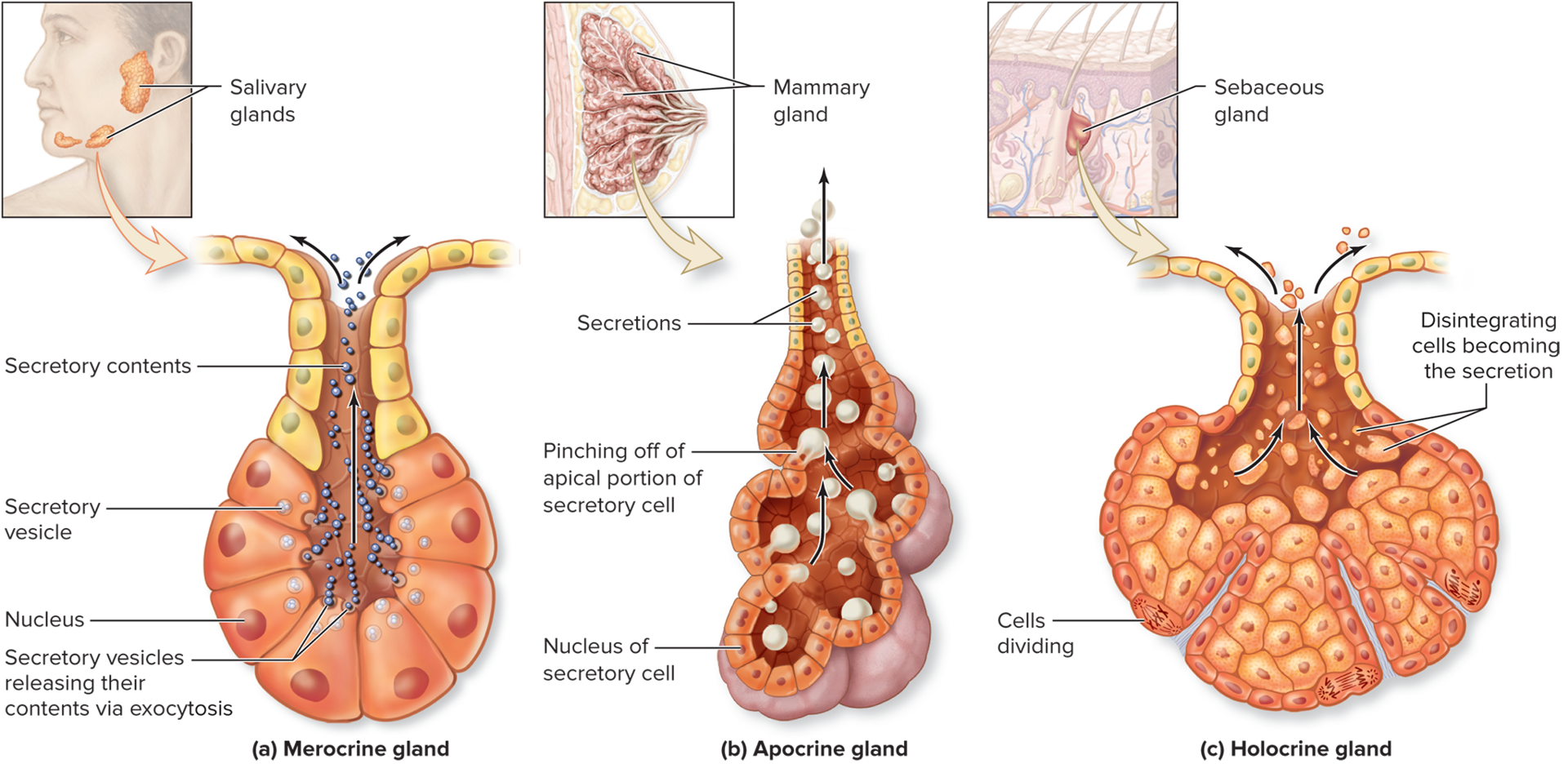
Method of Secretion:
- Merocrine
- Apocrine
- Holocrine
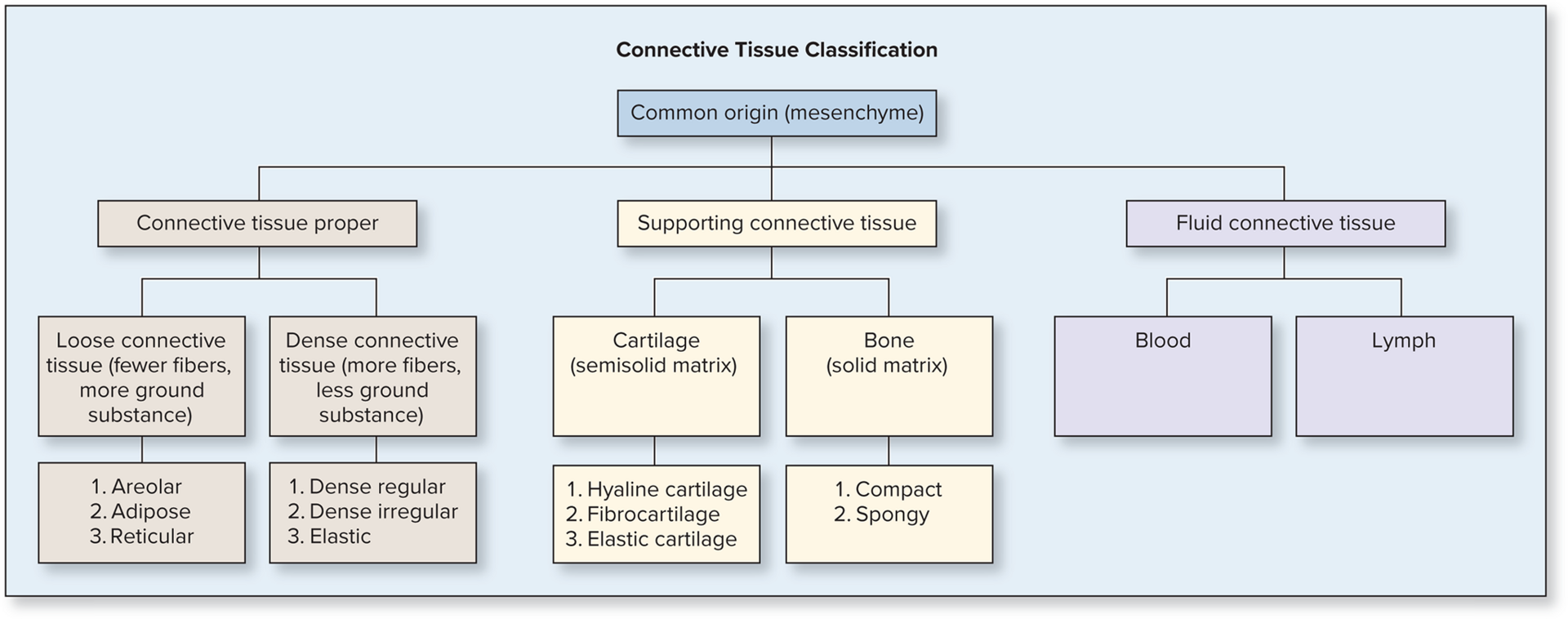
Connective Tissue:
- Supports, protects, and binds the body organs
- All derived from an embryonic connective tissue called mesenchyme
Characteristics:
- Cells
- Protein fibers
- Ground substance
Functions:
- Physical protection
- Support
- Structural framework
- Binding of structures
- Storage
- Transport
- Immune protection
Classification:
Loose connective tissue: areolar, adipose and reticular
Dense connective tissue: regular, irregular, elastic
Cartilage and bone: protection of organs
Fluid connective tissue: blood, lymph
Muscle Tissue:
- Skeletal Muscle
- Long, cylindrical, multinucleated fibers that are striated
- Under voluntary control
- Cardiac Muscle
- Branched, short, striated, contain one or two centrally located nuclei
- Under involuntary control
- Smooth Muscle
- Spindle-shaped, small, contain one centrally located nucleus
- No striations
- Under involuntary control
Nervous Tissue:
- Contains neurons and glial cells
- Forms the brain, spinal cord, and nerves
Compact vs Spongy Bone
Spongy Bone:
- Located within the interior of a bone
- Contains a latticework structure of bone connective tissue
- Strong yet lightweight
- Appears porous
- Makes up 20% of total bone mass
Compact Bone:
- Appear solid but is in fact perforated by a number of neurovascular canals
- Formed from cylindrical structures called osteons, which display concentric rings of bone connective tissue called lamellae
- Lamellae encircle a central canal that houses blood vessels and nerves
- Makes up 80% of total bone mass
Bone Cells
Osteoprogenitor - stem cells derived from mesenchyme; located within the periosteum and endosteum
Osteoblast - formed for osteoprogenitor cells, synthesize and secrete osteoid which later calcify
Osteocytes - mature bone cells derived from osteoblasts; maintain bone matrix and detect mechanical stress on bone
Osteoclasts - derived from fused bone marrow cells; break down bone (bone resorption)
Types of Hormones
Circulating Hormones:
- Are either lipid-soluble (steroids, calcitriol, thyroid hormone) or water-soluble (biogenic amine, protein hormones that are synthesized from amino acids)
Local Hormones:
- Eicosanoids stimulate the cell that produced them (autocrine) or neighboring cells (paracrine)
- Synthesized from a fatty acid
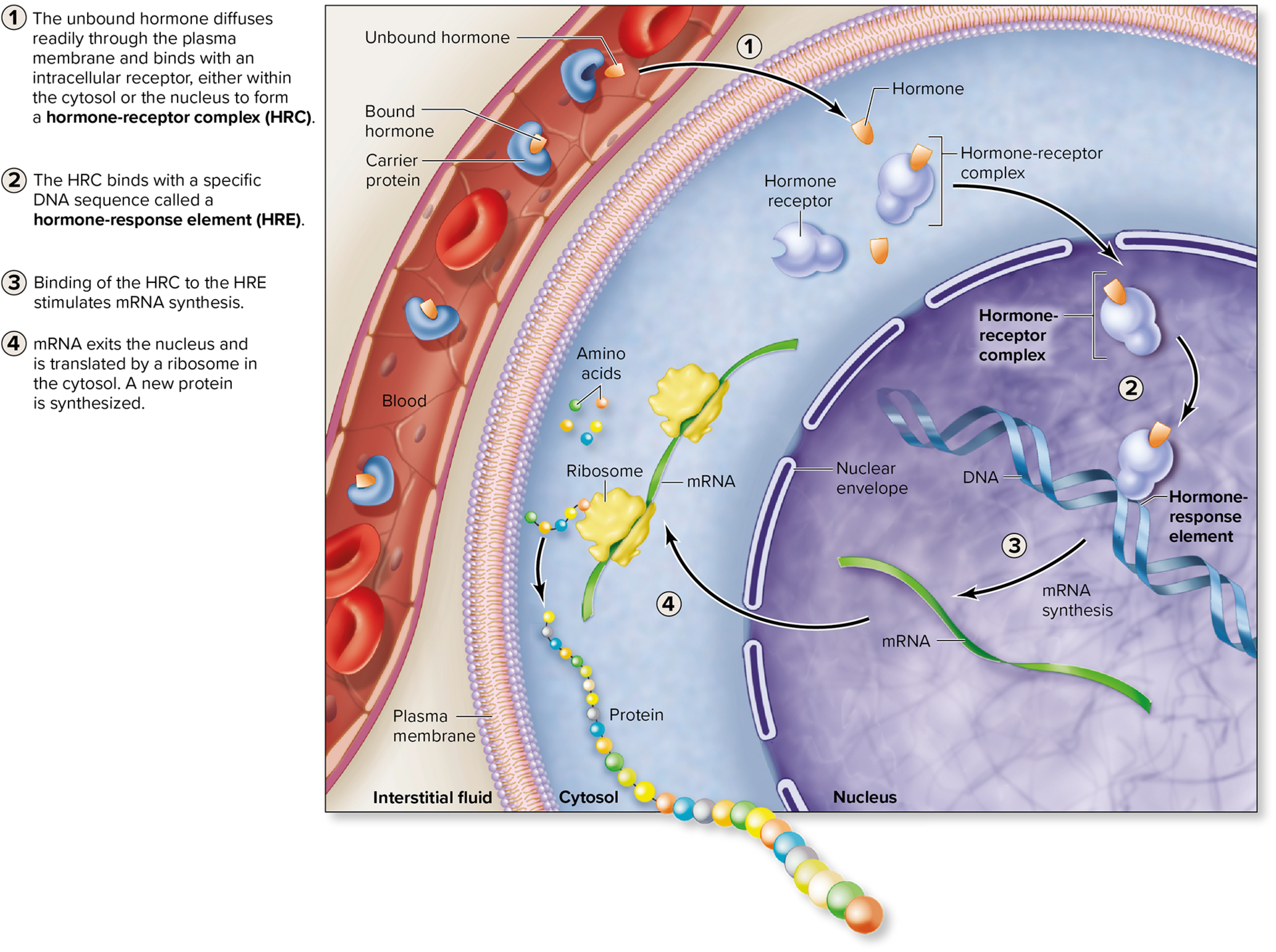
Lipid-Soluble Hormones:
- Stimulate cellular activity by binding to intracellular receptors
- The hormone receptor complex activates a region of DNA
- Produces new proteins
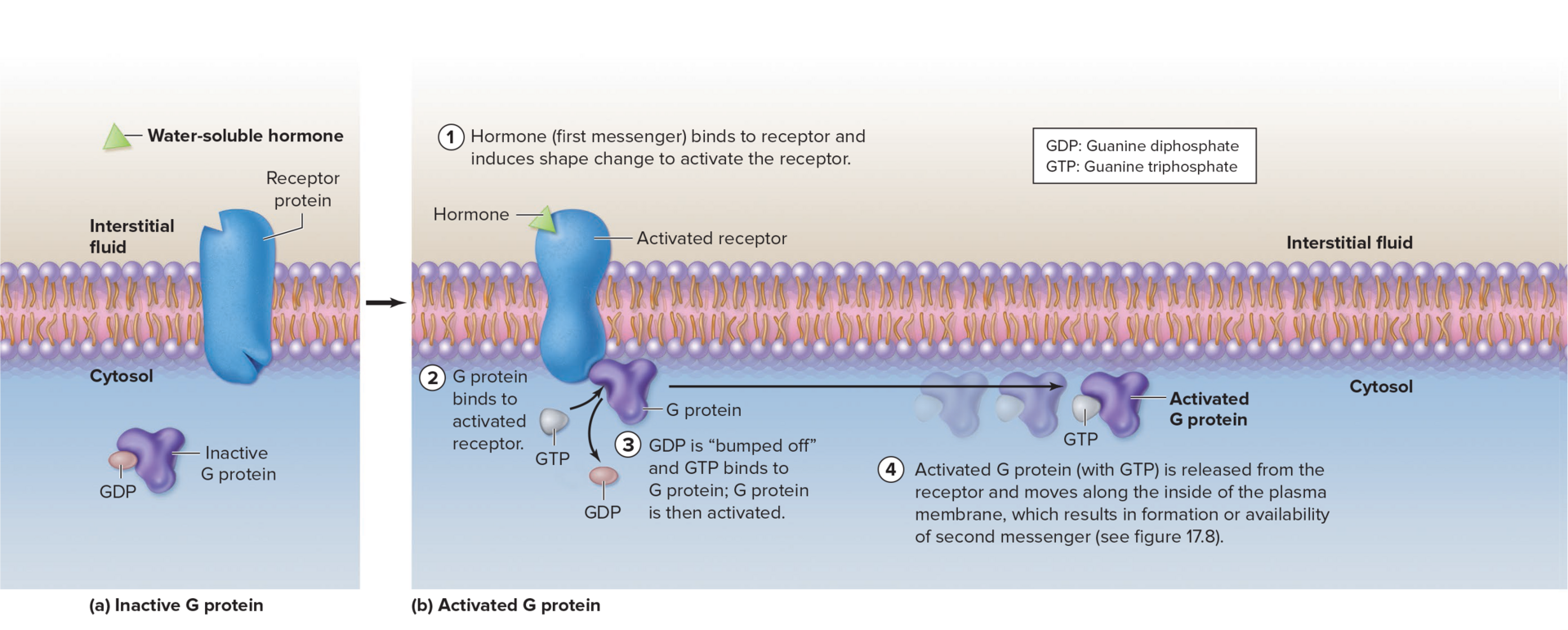
Water-Soluble Hormones:
- Bind with plasma membrane receptors
- Hormone is the first messenger
- G protein is activated and formation of 2nd messenger
- Activation or inhibition of enzymatic pathways
- Stimulation of growth through cell division
- Stimulation of cellular secretions
- Change in plasma membrane ion permeability
- Muscle contraction relaxation or contraction
Target cell and cellular response to hormones
Number of Receptors:
Up-regulation:
- Increase in the number of receptors
Down-regulation:
- Decrease in the number of receptors
Being able to change the receptor number allows a target cell to modify its responsiveness to a hormone
Hormone Interactions:
- A single target cell may possess receptors for many different hormones
- Multiple hormones may interact with target cells to have one of three effects:
- Synergistic: “working together” estrogen and progesterone
- Permissive: “gives permission” prolactin is required (produce milk) for oxytocin (milk ejection)
- Antagonist: “opposes” insulin opposing glucagon, vice versa
Sodium and Potassium Pumps
- Pumps maintain specific concentration gradients by moving substances up (against) a concentration gradient
- Requires expenditure of energy
Endocrine vs. Nervous System
- Complement each other to maintain homeostasis
Features | Endocrine System | Nervous System |
|---|---|---|
Communication Method | Secrete hormones to be transported within the blood to target cells throughout body | A nerve signal causes neurotransmitter release from a neuron into a synaptic cleft |
Target of Stimulation | Any cell in the body with a receptor for the hormone | Other neurons, muscle cells, gland cells |
Response Time | Relatively slow reaction time | Rapid reaction time |
Range of Effect | Typically has widespread effects throughout the body | Typically has localized, specific effects in the body |
Duration of Response | long-lasting | short-term |
Endocrine Stimulation
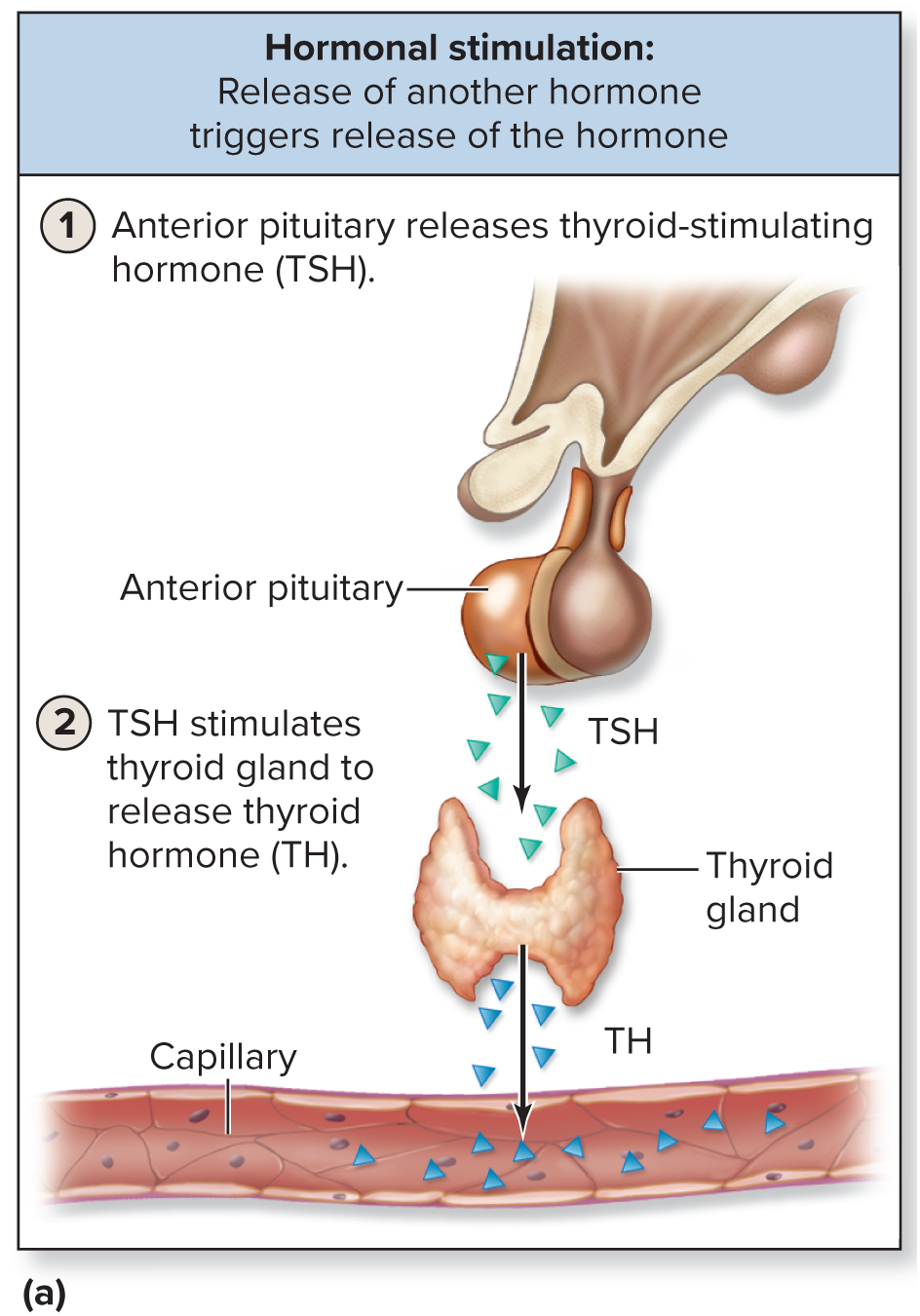
Hormonal:
- The stimulus of release of many hormones from an endocrine gland is the binding of another hormone
- TSH binding to follicular cells on thyroid gland to release TH
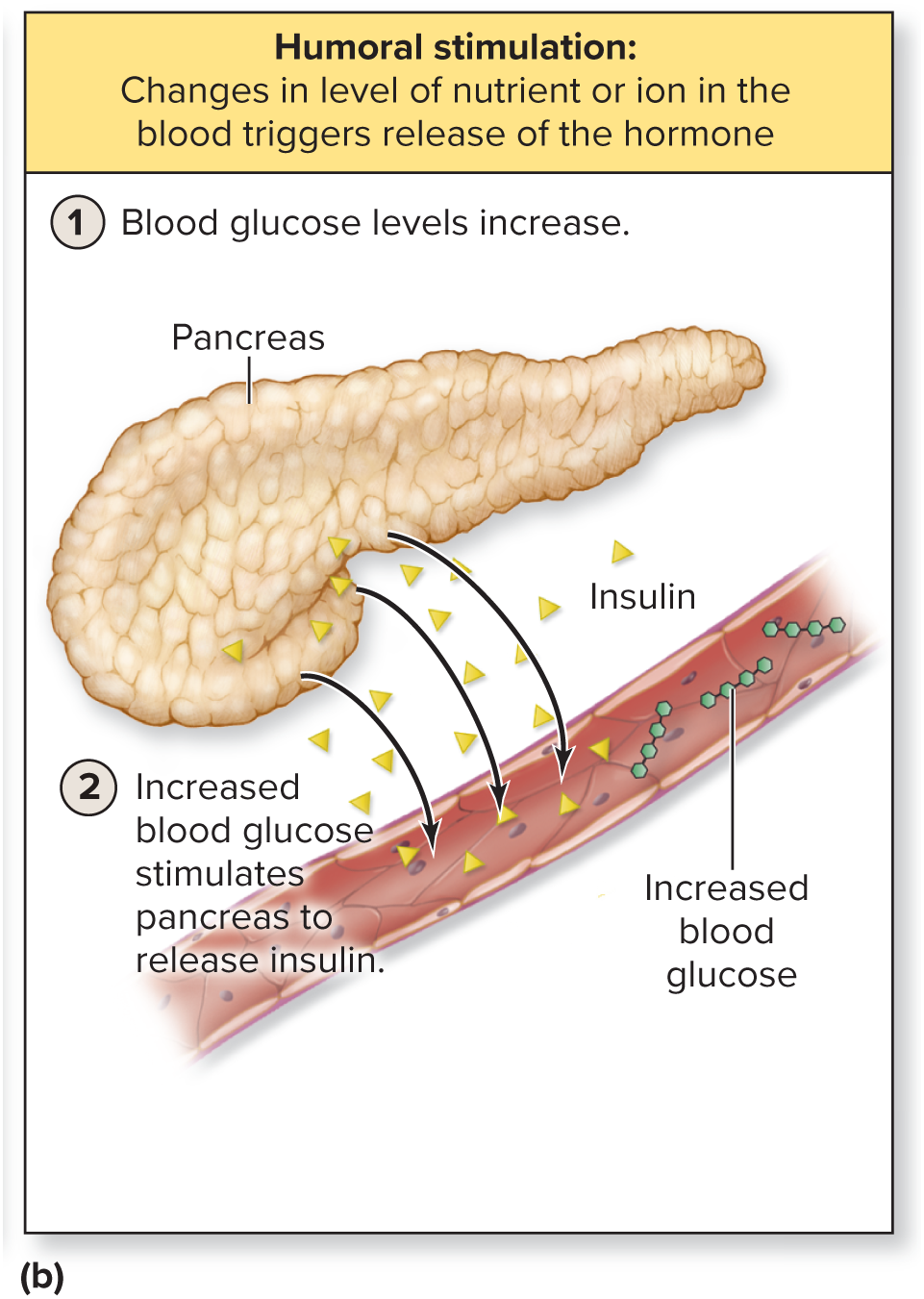
Humoral:
- When either the nutrient of ion levels decrease or increase within the blood, an endocrine gland is stimulated to release its hormone molecules
- Blood glucose increases and the alpha cells release insulin
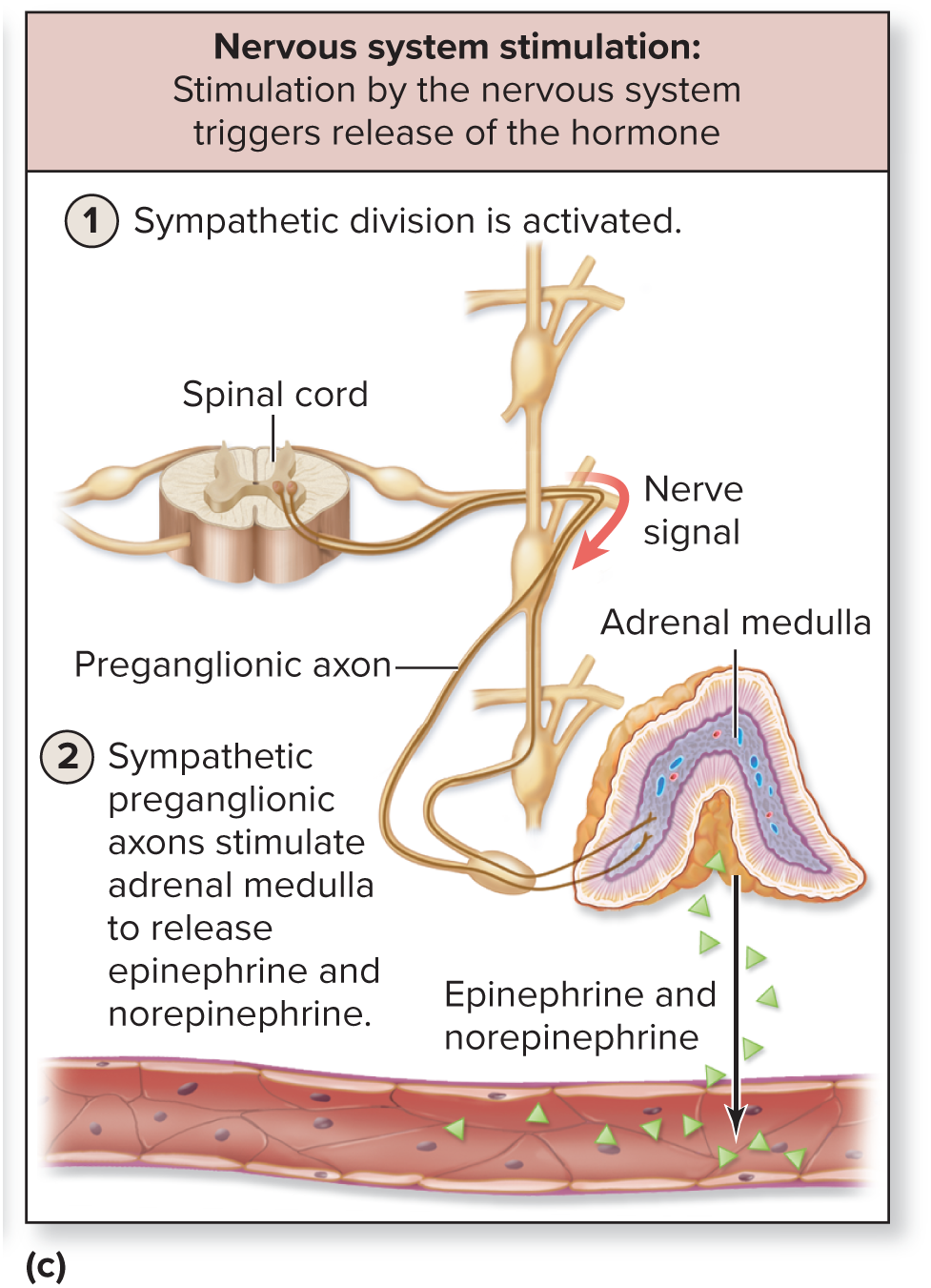
Nervous:
- By direct stimulation from nervous system
- Release of epinephrine and norepinephrine by adrenal medulla in response to stimulation by the sympathetic division of the autonomic nervous system
Mechanism of Action for Hormones
Feedback Mechanism
Negative Feedback:
- Initiated by either an increase or a decrease in the stimulus
- The end result is to return the stimulus to within its normal range or set point
Positive Feedback:
- Initiated by a stimulus
- Maintain or increase the activity of the original stimulus until a climactic event occurs
Membrane Transport
Diffusion (Passive):
- Movement of a solute from an area where it is more concentrated to an area where it is less concentrated
- Simple diffusion is the unassisted movement of small, nonpolar molecules, through the phospholipid bilayer
- Channel-mediated facilitated diffusion is the transport of ions through channels that either are always open (leak channels), or open or close as a result of a stimulus (gated channels)
- Carrier-mediated facilitated diffusion is the transport of polar molecules by a carrier protein that is induced to change shape to move the molecules across the plasma membrane
Osmosis (Passive):
- Passive movement of water across a semipermeable membrane down a water concentration gradient
- Osmotic pressure is the pressure exerted by the movement of water across a semipermeable membrane due to a difference in water concentration
- The greater the difference, the greater the osmotic pressure
Active Processes:
- Require the expenditure of cellular energy
- Primary active transport (energy from ATP)
- Secondary active transport (powered by the movement of a second substance)
- Vesicular transport
- Exocytosis, phagocytosis, pinocytosis, receptor-mediated endocytosis
Joint Classifications
Structural Classifications of Joints:
- Fibrous
- Cartilaginous
- Synovial
Fibrous Joints: connected by dense regular connective tissue and has NO joint cavity
- Gomphosis:
- Periodontal membranes that hold a tooth to bony jaw (synarthrosis)
- Suture:
- Connects skull bones (synarthrosis)
- Syndesmosis:
- Interosseous membranes between bones (amphiarthrosis)
Cartilaginous Joints: connected by hyaline cartilage or fibrocartilage and has NO joint cavity
- Synchondrosis:
- Contain hyaline cartilage (synarthrosis)
- Symphysis:
- Contain fibrocartilage (amphiarthrosis)
Synovial Joints: all diarthroses (mobile)
Movements: uniaxial, biaxial, multiaxial
Functional Classifications of Joints:
Synarthrosis - immovable
Amphiarthrosis - slightly movable
Diarthrosis - freely movable
Recall from Lab: plane (uniaxial), hinge (uniaxial), pivot (uniaxial), condylar (biaxial), saddle (biaxial), ball-and-socket (multiaxial)
Resting Membrane Potential
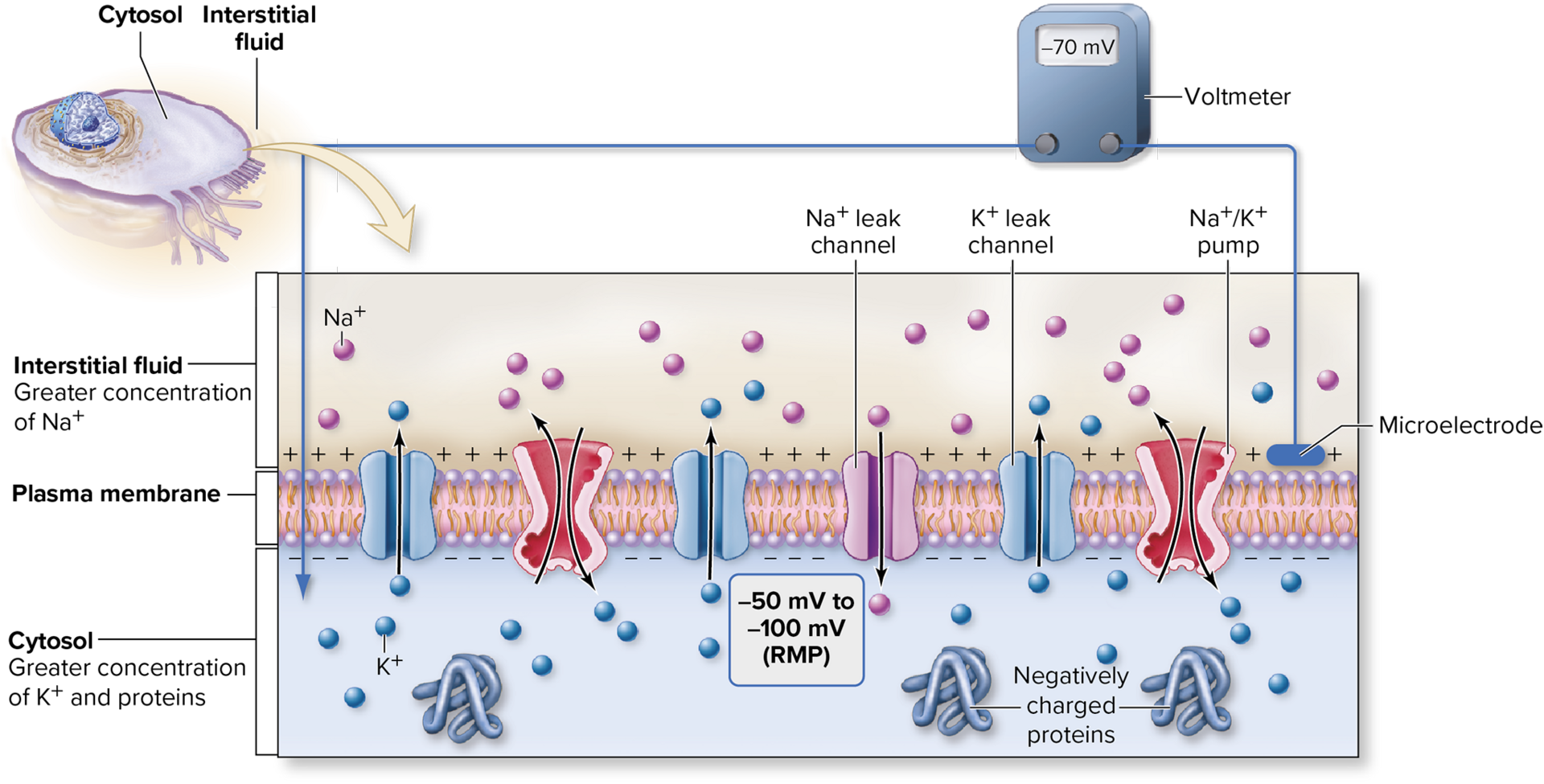
- The RMP is the electrical charge difference at the plasma membrane when a cell is at rest; typically ranges between -50mV and -100mV
Establishing and Maintaining an RMP:
- K+ leaks out of a cell through K+ leak channels
- Na+ leaks into a cell through Na+ leak channels
- This movement of ions is primarily responsible for maintaining an RMP
Skeletal Muscle Contraction
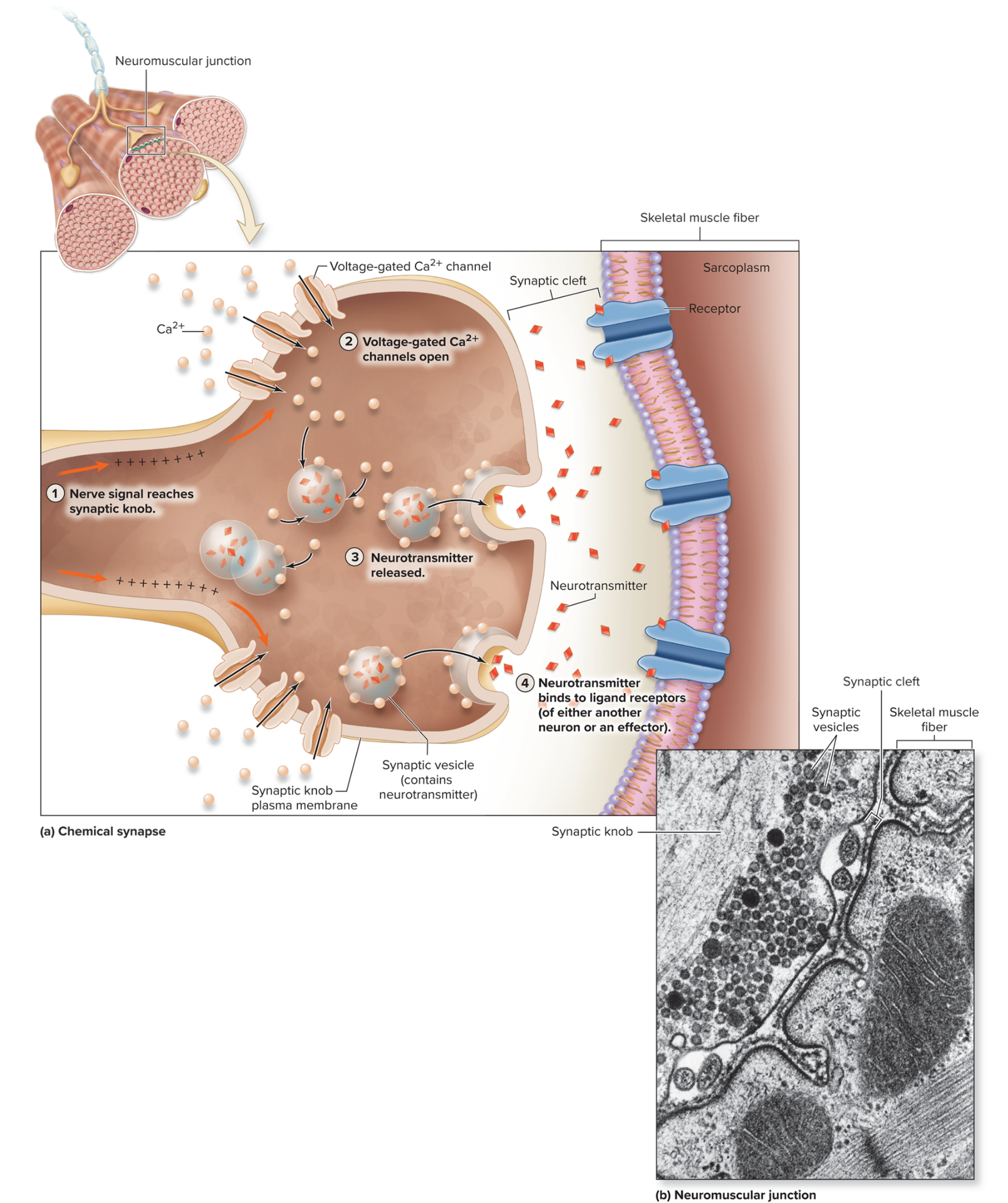
Parts of a neuromuscular junction: Excitation of a Skeletal Muscle Fiber. The first physiologic event of skeletal muscle contraction.
Calcium Entry at Synaptic Knob:
A nerve signal is sent along a motor neuron
The nerve signal triggers the opening of voltage-gated calcium channels within the synaptic knob and calcium moves down its gradient
Release of ACh from Synaptic Knob:
The binding of calcium to synaptic vesicles triggers the merging of synaptic vesicles with the synaptic knob
Exocytosis of ACh into synaptic cleft
Binding of ACh at Motor End Plate:
ACh diffuses across the fluid-filled synaptic cleft to bind with ACh receptors within the motor membrane - causes excitation
Excitation-Contraction Coupling*: The second physiologic event of skeletal muscle contraction involving the sarcolemma, T-tubules, and sarcoplasmic reticulum.
Development of an End-Plate Potential at the Motor End Plate:
The opening of ACh receptors/channels allow relatively small amounts of sodium to rapidly diffuse into the skeletal muscle fiber
Potassium diffuses out
These changes in membrane potential are short-lived and local
If there is a sufficient gain of positive charge to depolarize the RMP, and end-plate potential is produced, causing an action potential
Initiation and Propagation of Action Potential Along the Sarcolemma and T-tubules:
EPP triggers an action potential that is propagated along the sarcolemma and T-tubules
Voltage-gated sodium channels open - depolarization
Voltage-gated potassium channels open - repolarization, that reestablishes the RMP
Release of Calcium from the Sarcoplasmic Reticulum:
When the action potential reaches a triad it:
i. Stimulates a shape change to voltage-sensitive calcium channels within the T-tubule membrane
ii. Causes a shape change in calcium release channels, causing them to open
This allows calcium to diffuse out of the terminal cisternae of the SR into the cytosol
Calcium now “mingles” with the thick filaments and thin filaments of myofibrils
Crossbridge Cycling*: The third physiologic event in contraction that involves binding of calcium and cross bridge cycling.
Calcium Binding:
Calcium released from SR binds to a subunit of globular troponin (component of thin filaments; this changes the shape of troponin
RECALL: troponin-tropomyosin complex
When troponin changes shape, the entire complex is moved and the myosin binding sites of actin are exposed
(2-5) - Crossbridge Cycling: repeated
Crossbridge Formation:
Myosin heads attach to exposed myosin binding sites of actin
Formation of a crossbridge within thick (myosin) and thin (actin) filaments
Power stroke:
After forming a crossbridge, the myosin head swivels
This causes the thin filaments to pull a small distance past the the thick filament toward center of the sarcomere
ADP and P1 are released and ATP binding sites are available again
Release of Myosin Head:
ATP binds to ATP binding site of a myosin head
Release of myosin head from binding site of actin
Resetting of Myosin Head:
Myosin ATPase splits ATP into ADP and P1 providing the energy to reset myosin head
Skeletal Muscle Relaxation:
- Termination of rapid nerve signals propagated along motor neuron, when it stops ACh is no longer released
- ACh is hydrolyzed by acetylcholinesterase
- ACh receptors close, end-plate potentials at the motor end plate and the action potentials along the sarcolemma and T-tubules cease
- Calcium channels return to their original position
- Calcium is returned to the terminal cisternae by pumps and returned to its storage within sarcoplasmic reticulum
- Troponin returns to its original shape when calcium is removed, with tropomyosin being simultaneously moved over to myosin binding sites on actin - prevents crossbridge formation
- Muscle returns to its original position from the release of tension in connectin (springs)
Smooth Muscle Contraction
- resembles skeletal muscle contraction as it is initiated by calcium, the sliding of thin filaments past thick filaments, and requires ATP.