Unit 4 AOS 1
7A – Antigens, the markers, types of pathogens
Pathogen: an agent that causes disease in a host
antigen: any molecule that may trigger an immune response
2 functions of the immune system:
recognise foreign cells as antigens and eliminate them
recognise their own body cells as self and not attack
MHC
a group of receptor proteins present on the surface of body cells
help the immune system to distinguish the body’s proteins from foreign proteins
2 types of MHC:
MHC-I
MHC-II
MHC-I
found on all nucleated body cells
mark cells as self so the immune system doesn’t attack them
MHC-II
found on antigen-presenting cells (APCs)
interact with T helper cells during antigen presentation
Types of Pathogens
non cellular agents: prions and Viruses
Cellular agents: bacteria, fungus, protists, insects
Non-cellular
Prions
normal, harmless proteins found in the nervous system
change in shape and become infectious
makes all proteins it contacts change shape
cannot be cured
e.g. scrapie, CJO
Viruses
An infectious agent composed of genetic material (DNA or RNA) inside a protein coat (capsid).
In some instances, the protein coat is surrounded by a lipid envelope.
Viruses cannot independently reproduce, instead, they insert their genetic material into a host’s cell and use the cell to replicate.
Viruses can cause disease through the lysis of cells during viral replication
e.g The flu, Covid
Cellular
Bacteria
Unicellular prokaryotes can infect almost any part of the body.
Bacteria can cause disease through the production of toxins and enzymes which either affect the functioning of cells or cause their death
reproduces through binary fission
e.g. Meningitis, Tetanus
Worms
Fungi
7B- The First Line of Defence
Plants
Chemical barriers
Defensins – small peptides that are toxic to microbes and fungi
Glucanases – defend plants against fungi
Physical Barriers
Thick bark
Waxy cuticles of leaves
Closing of stomata to prevent pathogen invasion during carbon dioxide uptake
Animals
Physical
intact skin
mucus secretion
Chemical
tears and saliva
sweat
stomach acid
earwax
Biological
bacteria on skin
gut microbiota
7C- The Second Line of Defence.
NK cells
Destroys infected or abnormal cells with insufficient MHC Class I markers
Mast cells
Causes inflammation through the release of histamine
Phagocytes
phagocytosis: consume and destroy foreign or dead material present in the body by engulfing it
Neutrophils
Phagocytosis of pathogens
macrophages
engages in phagocytosis and antigen presentation
dendritic cells
engages in phagocytosis and antigen presentation
connects the innate immune response with the adaptive immune response
Inflammation
the first reaction when an injury is caused
initiation
in response to injury macrophages activate and along with damaged cells release cytokines. mast cells release histamines
vasodilation
histomines travel to the blood vessels and bind to receptors causing vasodilation, increasing blood flow to the injury site. gaps form in the vessel wall, increasing permeability for immune cells
Migration
complement proteins such as macrophages are guided by the cytokines to the injury site where they phagocytose pathogens and digest them using enzymes such as lysosomes
Complement proteins
25 proteins form a complement system
react with each other in the presence of pathogens
3 major outcomes:
opsonisation
complement proteins bind to the surface of the pathogen making it easier for immune cells to recognise it as foreign
chemotaxis
they gather near a pathogen and attract phagocytes making it more likely to be destroyed
lysis
join on the surface of the pathogen to form a membrane attack complex (MAC)
forms a pore on the pathogen membrane allowing fluid to enter it
the pathogen swells and bursts
7D- Third Line of Defence
Antigen presentation
an APC engulfs and processes the antigen
MHC II binds to a small piece of the antigen presented by the APC
A T cell receptor on a TH cell binds to the antigen if it is complementary
When this interaction occurs, the T helper cell becomes activated
The activated T helper cell can then help initiate the adaptive immune response through either the humoral or cell-mediated immune responses
Lymphocytes
memory B cells: keep a memory of the pathogen
Plasma B cells: secrete antibodies to destroy the antigen
T helper cells: coordinate the actions of the immune system: activate naive B cells and cytotoxic T cells
cytotoxic T cells: target intracellularly infected cells, inducing cell death
Humoral immunity
targeted towards extracellular pathogens
a naive B-cell that can recognise an antigen presented by an APC gets selected (B-Cell clonal selection)
the naive B-cell gets activated by the T helper Cell with the same receptor
the naive b cell differentiates and proliferates into plasma b cells and memory b cells
memory B cells keep a memory of the pathogen for future infection and plasma B cells secrete antibodies to destroy the antigen
Cell-mediated immunity
targeted towards intracellular pathogens
viruses
cancers
The activated T helper cells rapidly divide, differentiating into memory T cells and more T helper Cells
The T helper Cell activates cytotoxic T Cells which then proliferate into more Cytotoxic T cells and T memory cells
infected self-cells present the antigen of the intracellular pathogen on their MHC I markers
Cytotoxic T cells detect the non-self antigens presented on the MHC I markers and kill the infected cells via apoptosis or lysis
Antibodies
composed of four polypeptide chains,
including two heavy chains and two light chains, arranged into a ‘Y’ shape
The two heavy chains are joined by a disulphide bond
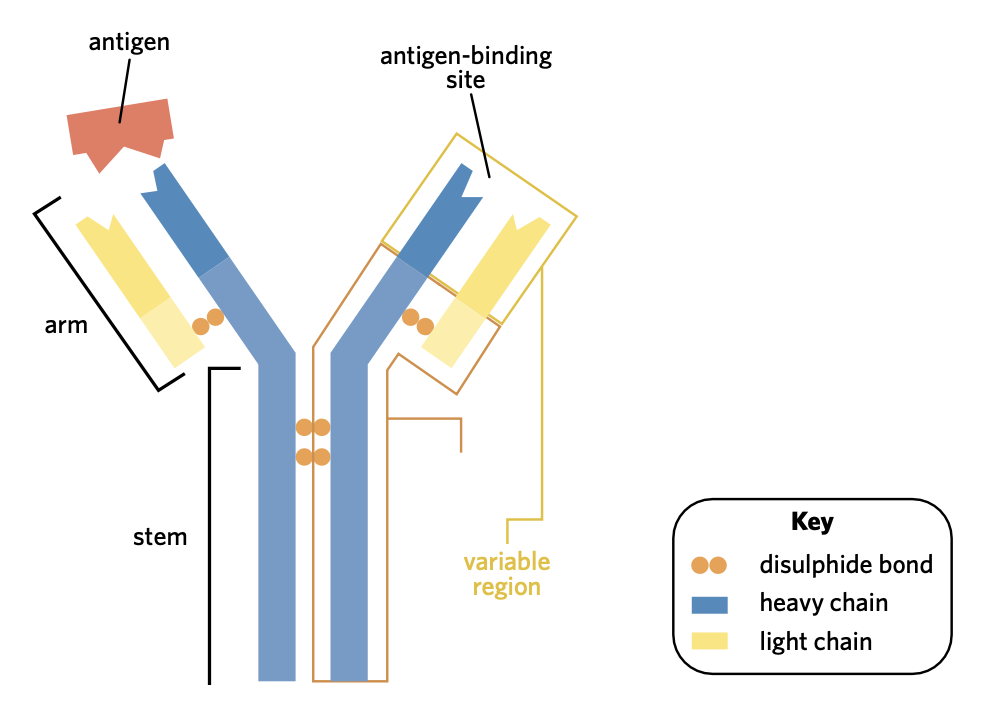
The ‘stem’ of the antibody is known as the constant region
the tops of the ‘arms’ are known as the variable region
These regions come together to form two identical binding sites for the same specific complementary antigen.
This allows antibodies to bind with antigens on the surface of pathogens
can bind with 2 pathogens at once
Functions
Immobilisation
Antibodies can restrict the movement of pathogens around the body through the formation of large antigen-antibody complexes.
Activation of complement proteins
Antibodies attached to the surface of pathogens can facilitate the actions of complement proteins, including the formation of membrane attack complexes (MACs).
7E- Lymphatic system
Primary lymphoid tissue
Bone Marrow
b and T cells are produced
B cells mature
Thymus
T cells mature
Secondary lymphoid tissue
Lymph nodes
filter the lymph (cancer cells, Pathogens, infected cells)
where antigen is presented by APC to the lymphocytes
Spleen
B cells also mature here
8A- Immunity
Types of immunity
active immunity: memory cells are produced
antibodies produced in a person’s own body
natural
catch the disease
make your own antibodies
artificial
vaccination which contain dead or treated pathogens
symptoms of disease do not generally occur
passive immunity: no memory of infection
antibodies from another organism enter the body
natural
from mother to foetus through placenta
in breast milk
artificial
antibodies obtained from another organism are injected into patient
blood plasma
Vaccinations
designed to stimulate a person’s adaptive immune system to create immunity to a pathogen without actually causing disease
primary immune function
After a person receives their first vaccination, there is a delay in the adaptive immune system’s response
Eventually, a primary immune response takes place in which a moderate number of antibodies and memory cells are formed
these quickly diminish over time.
secondary immune function
Upon receiving a second vaccination, the memory cells created by the first vaccine quickly recognise the antigen in the vaccine
This results in the generation of a large number of antibodies and memory cells that go on to create long-lasting immunity.
Herd Immunity
when the majority of the population is immune to a particular pathogen, helping to prevent the spread of the pathogen to those who haven’t been vaccinated or who haven’t already been infected with the pathogen.
important because it protects people in the community who have no immunity towards a particular disease
8D- Immunotherapy
treating cancer (naked and conjugated monoclonal antibodies).
Immunotherapy: a form of medical treatment that modulates the functioning of the immune system to treat disease.
dendritic cell therapy
Car T therapy
cytokine therapy
monoclonal antibodies
Monoclonal antibodies
laboratory-made proteins that can be used to treat a number of different diseases.
Produced:
mouse injected with antigen X, activates production of B cells that produce specific antibodies
the mouse spleen is removed and the cells are removed and cultured
myeloma cells are added to the culture
myeloma cells fuse with the B cells to form hybridoma cells
the hybridoma cells are cultured and allowed to divide repeatedly to produce multiple copies of each hybridoma cell
each clone is screened for the presence of antibodies against antigen X. The hybridomas that produce the specific antibody are cloned, which results in the mass production of these antibodies.
Antibodies are then collected and purified before being administered to a patient.
Naked Monoclonal antibodies
there are no additional molecules added
can bind to cancer cells and interact with complement proteins to for MAC
conjugated monoclonal antibodies
have other molecules such as chemotherapy or radiotherapy drugs added
can be used to deliver chemotherapy drugs or radioactive isotopes directly to cancer cells