FUND T2
KEY TERMS FROM CHAPTERS:
active exercise
activities of daily living (ADLs)
aerobic exercise
atrophy
contractures
ergonomics
flaccidity
footdrop
fracture
instrumental activities of daily living (IADLs)
isokinetic exercise
isometric exercise
isotonic exercise
orthopedics
paralysis
paresis
passive exercise
range of motion
safe patient handling and mobility (SPHM)
spasticity
strength and endurance exercises
stretching exercise
tonus
alopecia
caries
cerumen
cheilosis
gingivitis
glossitis
halitosis
pediculosis
periodontitis
personal
hygiene
plaque
stomatitis
tartar
Learning Objectives Chapter 32:
Hygienic practices include caring for the skin, hair, nails, eyes, ears, nose, mouth, feet, and perineal area. There are strong links between good hygiene practices and a person’s health. Inadequate hygiene practices can contribute to alterations in a person’s health.
. Adequate skin hygiene, including foot care, contributes to maintaining skin condition and integrity, an important first line of defense, preventing the entry of pathogens, minimizing absorption of harmful substances, and preventing excessive water loss.
A person’s general health influences the health of that person’s mouth and teeth, and proper care of the mouth and teeth contribute to overall health. Maintaining good oral hygiene and dental care has several benefits. There is esthetic value in having a clean and healthy mouth. Having one’s own teeth in good condition contributes to an intact body image. In addition, the beginning of the digestive process and tasting pleasure are enhanced when the mouth and teeth are in good condition. Oral health is directly related to systemic health, and poor oral health is associated with diabetes, cardiovascular disease, and metabolic syndrome (American Dental Association, 2019b). Oral health is an important concern in relation to overall health and quality of life.
1.Identify factors affecting personal hygiene.
from my personal lecture notes: religious practices, socioeconomic factors, cultural practices, spiritual practices, developmental levels, health state, personal preferences
from book:
Culture
It is important to identify cultural variations that could affect a patient’s personal hygiene preferences, such as typical bathing habits, and behaviors, such as use of various hygiene-related products (Andrews et al., 2020). For example, people from some cultures place a high value on personal cleanliness and feel unclean unless they shower or bathe at least once daily. Many consider bathing incomplete without the use of products to reduce or mask normal body odors. Other people often find a weekly bath sufficient and may feel no need to mask normal body odors. Culture may also influence whether bathing is a private or communal activity.
Socioeconomic Status
A person’s socioeconomic status and financial resources often define the hygiene options available to that person. A lack of funds to obtain toiletries or clean clothing may contribute to an inability to maintain personal hygiene needs. For example, someone renting a room in a boarding house may have limited or no access to a tub or shower and may have limited finances to buy soap, shampoo, shaving cream, and deodorant. People who are homeless, who often carry all their belongings in a car or shopping cart, may welcome the warm running water and soap available in roadside or public restrooms.
Spiritual Practices
Spiritual practices, including religious beliefs, may dictate ceremonial washings and purifications, sometimes as a prelude to prayer or eating. For example, in the Orthodox Jewish tradition, ritual baths are required for women after childbirth and menstruation. In some religions, contact with a deceased person or a deceased animal may make a person “unclean.” Other religions dictate that no modern facilities be installed in homes. This would prohibit some people from having running water and toilets in their homes. As a result, they may bathe infrequently.
Developmental Level
Children learn hygiene practices while growing up. Family practices often dictate hygiene habits, such as morning or evening baths; the frequency of shampooing, tooth brushing, and clothing changes; feelings about nudity; and so on. As adolescents become more concerned about their personal appearance, they may adopt new hygiene measures, such as taking showers more frequently and wearing deodorant. Bathing frequency commonly decreases as a person ages, possibly due to limitations in mobility and the natural tendency toward drier skin with age. Older adults may experience an increase in skin conditions or problems, increasing the need for education related to hygiene and skin care (Lichterfeld-Kottner et al., 2020; Moore & Merrill, 2019).
Health State
Disease, surgery, or injury may reduce a person’s ability to perform hygiene measures or motivation to follow usual hygiene habits. Weakness, dizziness, and fear of falling may prevent a person from entering a tub or shower or from bending to wash the lower extremities. Illness may also create a demand for new or modified hygiene measures. For example, meticulous foot care becomes a priority for patients with peripheral vascular complications that often accompany diabetes mellitus. The presence of pain with an acute condition or chronic pain can affect a person’s ability to perform and/or tolerate personal hygiene measures.
Personal Preferences
People have different preferences with regard to hygiene practices such as taking a shower versus a tub bath, using bar soap versus liquid soap, and washing to wake oneself or to relax before sleep. A person’s self-concept and sexuality also influence personal hygiene practices. For example, in an effort to promote a positive self-image, older adults may use skin care products advertised to prevent wrinkles and diminish signs of aging. Women who are sexually active may use a variety of hygiene products following intercourse to promote cleanliness.
from power point:
from Knowt lecture recording:
Hygiene and bathing vary widely among individuals and cultures.
Consider the client’s religion, culture, education, and financial resources when planning hygiene care.
Example: Orthodox Jewish cleansing rituals; communal bathing practices in some cultures; resource limitations in homeless shelters impacting access to hygiene products.
Factors affecting hygiene include:
Culture and bathing frequency (e.g., once weekly vs daily; deodorant use or non-use; communal practices).
Socioeconomic status and access to products and clothing.
Spiritual practices (ceremonial washings, purifications before meals, post-childbirth rituals).
Developmental level (children’s hygiene driven by family; adolescents seek more autonomy; braces require coordination with caregivers).
Health status and medical conditions (e.g., diabetes increases infection risk; neuropathy may mask injuries).
2.Assess the adequacy of hygiene practices and self-care behaviors using appropriate interview and physical assessment skills.
from my personal lecture notes: get a patient history of any sensory aids and how they care for themselves and their nutritional status
from book:
Promoting Health 32-1
HYGIENE
Use the assessment checklist to determine how well you are meeting your needs related to hygiene. Then develop a prescription for self-care by choosing appropriate behaviors from the list of suggestions.
Assessment Checklist
□ almost always □ sometimes □ almost never
□
□
□
1. I keep my hair clean and neatly styled.
□
□
□
2. My skin is clean.
□
□
□
3. The condition of my mouth indicates satisfactory oral hygiene.
□
□
□
4. My nails are neatly manicured.
□
□
□
5. My body is free of unpleasant odors.
Self-Care Behaviors
1. Ensure that diet and exercise are appropriate, since this contributes to healthy skin.
2. Brush and floss teeth regularly and visit the dentist every 6 months.
3. Keep hair clean, combed, and brushed regularly.
4. Use certain hair care products (e.g., hair dyes) cautiously, since they may damage the hair.
5. Clean under nails and maintain nails at an appropriate length. Clip all nails straight across and shape or smooth with an emery board or file, if necessary.
6. Bathe and cleanse skin regularly. Apply lotion or cream to dry skin, as necessary. Cleanse the axilla and perineal area thoroughly and apply deodorant or antiperspirant as needed.
7. Appreciate the relationship between hygiene and overall well-being.
NURSING PROCESS FOR PERSONAL HYGIENE AND SKIN CARE
Assessing
The comprehensive nursing assessment uses interview and assessment skills to elicit data about the patient’s hygiene status. When alterations in a patient’s physical or mental health result in impaired ability to maintain acceptable personal hygiene, additional specific assessment skills are needed to determine the patient’s limitations.
Nursing History
Bathing practices and cleansing habits and rituals vary widely. A clear threat to health must exist before a nurse decides that a person’s hygiene practices are inadequate. The nurse assessing the adequacy of a patient’s hygiene practices determines whether the patient has the knowledge, attitude, skills, and resources to care for the skin and mucous membranes. Use neutral and inclusive terms (e.g., partner) and a nonjudgmental manner to obtain information about the patient’s gender identity, biologic sex, and sexual orientation. This information will help identify the needs of individual patients and provide thoughtful, person-centered care (Altarum Institute, 2019; Cahill et al., 2020). Focused Assessment Guide 32-1 provides additional suggested strategies, questions and approaches for an assessment of information related to hygiene practices. When documenting the nursing history, be specific, clearly describing the patient’s typical hygiene practices and any issues or problems.
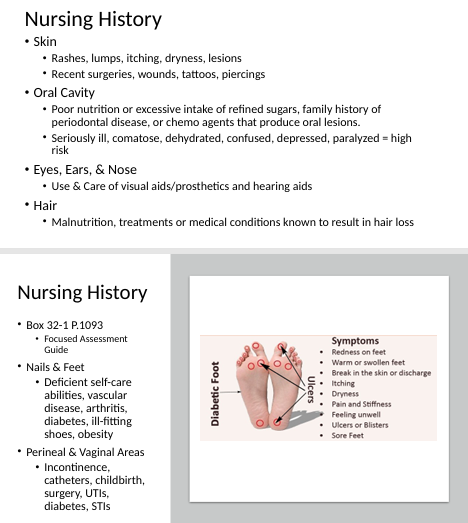
SKIN
Question the patient about any past or current skin problems and changes in their skin (e.g., rashes, lumps, itching, dryness, lesions) as well as recent surgeries, wounds, tattoos, or piercings. When skin problems are present, ask the patient the following:
• How long have you had this problem?
• Does it bother you?
• How does it bother you?
• Does it itch?
• Have you found anything that helps relieve these symptoms?
Additional information related to assessment of the skin is discussed in Chapter 27 and Chapter 33.
ORAL CAVITY
Identify the patient’s normal oral hygiene practices and the variables influencing these practices. Note the history of any oral problems and related treatments.
Identify any variables known to cause oral problems, such as deficient self-care abilities, poor nutrition or excessive intake of refined sugars, family history of periodontal disease, or ingestion of chemotherapeutic agents that produce oral lesions. Patients at increased risk for oral problems include those who are seriously ill, comatose, dehydrated, confused, depressed, or paralyzed. Patients with mental health problems are also at risk for alterations in oral health (Griffiths et al., 2020; Kisely, 2016). Patients who are mouth breathers, those who can have no oral intake of nutrition or fluids, those with nasogastric tubes or oral airways in place, and those who have had oral surgery are also at increased risk.
Additional information related to assessment of the oral cavity is discussed in Chapter 27.
EYES, EARS, AND NOSE
Ask the patient to identify any special eye, ear, or nose care that the patient performs. Also, address any specific care measures related to the use and care of visual aids or prosthetics (glasses, contact lenses, artificial eye) and hearing aids. Inquire about any history of eye, ear, and nose problems, and related treatments.
Focused Assessment Guide 32-1
HYGIENE PRACTICES
Factors to Assess Questions and Approaches
Daily and weekly bathing habits
Tell me about your daily and weekly bathing habits.
Are there special bathing or hygiene products you routinely use or can’t use?
How can the nursing staff best help you to meet your hygiene needs?
Factors interfering with hygiene practices (sensory, cognitive, endurance, mobility, or motivation)
What recently or in the past has interfered with your hygiene practices?
Does anything interfere with your ability to be as clean as you would like?
Pain
Do you have pain? Describe characteristics, onset, location, duration, associated symptoms, and intensity. Does the pain interfere with your ability to perform personal hygiene tasks? Does caring for yourself cause pain or discomfort?
Exposure history
Do you sunbathe? How much sun or tanning booth exposure do you get? Do you use sunscreen?
Does your job or daily activities/hobbies expose you to chemicals, such as bleach, petroleum, paint, insecticides, or cleaning products?
History of skin or mucous membrane problems (nature, onset of problem and frequency, causes, severity, symptoms, interventions attempted, results)
Have you noticed any changes in your skin or mucous membranes?
Describe any skin problems with rashes, lumps, itching, dryness, lesions, ecchymosis, or masses.
What have you used to relieve these symptoms?
Special hygiene practices
• Mouth
How do you clean your teeth and gums?
How often do you have a dental examination?
Do you have any dental appliances?
Are there any tender areas or lesions in your mouth?
• Eyes, ears, and nose
Do you wear glasses or contact lenses to improve your vision?
Do you wear a hearing aid?
Have you noticed any changes in your eyes, ears, or nose?
Have you experienced any discharge or bleeding from or swelling of your eyes, ears, or nose?
• Hair
Have you noticed any changes in your hair?
Have you noticed any unusual dryness of the scalp or changes in hair texture and amount?
• Feet and nails
Have you noticed any changes in your feet or nails?
Is the appearance of the nails normal?
How do you normally care for and clean your nails?
Is the skin intact on the feet?
Have you noticed any swelling of one or both feet?
Do you wear any special shoes?
• Perineum
Have you noticed any changes in your perineum?
Have you noticed any unusual discharge, swelling, itching, or inflammation?
Are you able to complete your own perineal care?
Do you follow any special hygiene practices during menstruation?
What type of feminine hygiene products (e.g., pads, tampons, douches) do you use?
• Piercings/Tattoos
Do you have any body piercings on your face, neck, arms, legs, torso, navel, or genitals? Have you experienced any problems related to the procedure? Do you have any tattoos? Are the tattoos healed? How do you care for your piercing(s) and/or tattoo(s)?
from power point:
from Knowt lecture recording:
Objective of assessment: determine if there is a clear threat to health from hygiene practices before labeling them inadequate.
Example: Unattended foot care in diabetics is a health risk and constitutes inadequate hygiene.
Nursing history and assessment during bathing:
Skin: rashes, bumps, dryness, itching, recent wounds, tattoos or piercings, lesions.
Oral cavity: nutrition, refined sugars, dental caries (cavities); family history of periodontal disease; chemo-related oral lesions; high-risk states (ill, comatose, dehydrated, depressed, paralyzed).
Ears, eyes, nose: visual aids, prosthetics/hearing aids; function and access.
Hair: malnutrition, treatments or conditions causing hair loss (e.g., chemotherapy, hypothyroidism).
Nails and feet: self-care deficits, vascular disease, arthritis, ill-fitting shoes; diabetes-specific foot assessment.
Perineal and vaginal areas: incontinence, catheters, childbirth history, surgeries, UTIs, diabetes, STIs.
General musculoskeletal system: mobility impairments influencing self-care.
Special populations and scenarios:
Diabetes: foot care is crucial due to infection risk and neuropathy; assess for redness, swelling, skin breaks, ulcers.
Patients with limited mobility or chronic pain may tolerate only brief hygiene tasks at a time.
Ventilated or nasogastric tube patients: at high risk for impaired oral hygiene; rely on caregivers for assistance.
Focused assessment guide (Focus areas from Lab/Book):
Skin, oral cavity, eyes/ears/nose, hair, nails, feet, perineal area, and the presence of prosthetics or devices (e.g., nasogastric tubes, ventilators).
Transitions and resource considerations:
When teaching hygiene, assess the patient’s ability to perform tasks and have them demonstrate back to you (e.g., at feet inspection for diabetes).
3.Assess the condition of the patient’s skin, oral cavity, hair, and nails using appropriate interview and physical assessment skills.
from my personal lecture notes: BOX 32-1, assess skin daily (smooth, dry cold, clamy, turger lesions?), oral cavity (lesions, cracking, pink, moist, dry, sores, tongue'/teeth color and swelling, inflammation, flossing?), EEN (sores, foreign bodies, etc?), hair (lice= pediculosis, loss, dry?), nails/feet (cap refill, tenderness, bledding, etc?), perineal/anal/vaginal (odor, colors, polyps, etc)
from book:
Box 32-2 General Skin Care Principles
Assess the patient’s skin at least daily and after every episode of incontinence.
Cleanse the skin when indicated, such as when soiled, using a no-rinse, pH-balanced skin cleanser.
Avoid using soap and hot water; avoid excessive friction and scrubbing.
Minimize skin exposure to moisture (incontinence, wound leakage); use a skin barrier product as necessary.
Use skin emollients after bathing and as needed.
PERINEAL AND VAGINAL AREAS
Note any history of perineal or vaginal problems and related treatments. Identify any variables known to cause perineal or vaginal problems or to create a need for special care, such as urinary or fecal incontinence, an indwelling Foley catheter, childbirth, douching, rectal or genital surgery, and diseases such as urinary tract infection, diabetes mellitus, and certain sexually transmitted infections (STIs; e.g., herpes).
Additional information related to assessment of the perineal area is discussed in Chapter 27.
Physical Assessment
An assessment of pertinent body systems can provide data about the patient’s hygiene status and the patient’s ability to maintain personal hygiene.
MUSCULOSKELETAL SYSTEM
Impairment of the musculoskeletal system can interfere with a patient’s ability to perform tasks related to personal hygiene. Many conditions produce muscle weakness, decreased range of motion, impaired balance, fatigue, and/or lack of coordination. The skills used to assess the musculoskeletal system are described in detail in Chapters 27 and 34.
SKIN
The inspection and palpation skills used to assess the integumentary system are described in detail in Chapters 27 and 33. Assisting patients with basic hygiene measures provides an excellent opportunity for examining a patient’s skin. Many people are unaware that they have skin lesions, such as precancerous moles, that if untreated could prove fatal. Early detection and treatment of skin problems are important nursing functions.
When examining the skin, pay careful attention to cleanliness, color, texture, temperature, turgor, moisture, sensation, vascularity, and any lesions. Follow these general guidelines for assessing the skin:
• Incorporate assessment of the skin during the assessment of other body systems.
• Use a good source of light, preferably daylight.
• Compare bilateral parts for symmetry.
• Use standard terminology to communicate and record findings.
• Allow data obtained in the nursing history to direct the skin assessment.
• Identify any variables known to cause skin problems, such as deficient self-care abilities, immobility, malnutrition, decreased hydration, decreased sensation, sun exposure, vascular problems (altered tissue perfusion or venous return), or the presence of irritants (body secretions or excretions on the skin, other chemicals, mechanical devices).
Because lifestyle factors, changes in health state, illness, and certain diagnostic and therapeutic measures may adversely affect the skin, be alert for patients who may be at high risk for skin problems, and perform the appropriate skin assessment. Assessment may reveal dry skin, acne, or skin rashes. Recommended treatments for these skin problems are discussed in the Promoting Skin Health section on page 1102.
When documenting a physical assessment of the skin, describe exactly what is observed or palpated, including appearance, texture, size, location or distribution, and characteristics of any findings.
ORAL CAVITY
A physical assessment of the oral cavity involves inspection of the oral cavity and surrounding structures with attention to any unusual odors. When performing the physical assessment of the oral cavity, examine the following:
• Lips: color, moisture, lumps, ulcers, lesions, and edema
• Buccal mucosa: color, moisture, lesions, nodules, and bleeding
• Color of the gums and surface of the gums: lesions, bleeding, and edema
• Teeth: any loose, missing, or carious (decayed) teeth. Note the presence and condition of dentures or other orthodontic devices
• Tongue: color, symmetry, movement, texture, and lesions
• Hard and soft palates: intactness, color, patches, lesions, and petechiae (pinpoint round, red, purple, or brown spots that result from bleeding)
• Oropharynx: movement of the uvula and condition of tonsils, if present
Note unusual mouth odors and assess the adequacy of mastication and swallowing. An oral assessment tool can assist with assessment of the status of the oral cavity, as well as help to determine the frequency and procedure for oral care (Chick & Wynne, 2020). Identifying the problem and its cause and initiating appropriate treatment are imperative. This may require consultation with a dentist or health care provider. Refer to Chapter 27 for further description of nursing assessment of the oral cavity.
Dental Caries
The decay of teeth with the formation of cavities is called caries. Caries result from failure to remove plaque, an invisible, destructive, bacterial film that builds up on everyone’s teeth and eventually leads to the destruction of tooth enamel. A successful plaque-fighting program includes limiting sweet snacks such as soft drinks, candy, gum, jams, and jellies between meals; thorough cleansing of the teeth; and regular dental checkups. The use of antiplaque fluoride toothpastes, mouth rinses, and flossing also help prevent dental caries.
Periodontal Disease
Periodontal diseases are the result of infections and inflammation of the gums and bone that surround and support the teeth (CDC, 2013). Periodontal disease and tooth decay are the two biggest threats to dental health (CDC, 2013). Gingivitis is an inflammation of the gingiva, the tissue that surrounds the teeth. Periodontitis, or periodontal disease, is a marked inflammation of the gums that also involves degeneration of the dental periosteum (tissues) and bone. Symptoms include bleeding gums; swollen, red, painful gum tissues; receding gum lines with the formation of pockets between the teeth and gums; pus that appears when gums are pressed; and loose teeth. If unchecked, plaque builds up and, along with dead bacteria, forms hard deposits called tartar at the gum lines. The tartar attacks the fibers that fasten teeth to the gums and eventually attacks bone tissue. The teeth then loosen and fall out. Halitosis, a strong mouth odor or a persistent bad taste in the mouth, may be the first indication of periodontal disease. Regular treatment by a dentist is imperative.
Other Oral Problems
Other oral problems that may be observed when inspecting the oral cavity include the following:
• Stomatitis, an inflammation of the oral mucosa, has numerous causes, such as bacteria, virus, mechanical trauma, irritants, nutritional deficiencies, and systemic infection. Symptoms may include heat, pain, increased flow of saliva, and halitosis.
• Glossitis, an inflammation of the tongue, can be caused by deficiencies of vitamin B12, folic acid, and iron.
• Cheilosis, an ulceration and dry scaling of the lips with fissures at the angles of the mouth, can have multiple causes, including infections of the oral cavity (e.g., strep bacteria), a lack of iron or B vitamin deficiencies (especially riboflavin), and skin irritation (e.g., eczema).
• Dry oral mucosa may simply be related to dehydration or may be caused by mouth breathing, an alteration in salivary functioning, or certain medications (e.g., anticholinergic drugs).
• Oral malignancies, appearing as lumps or ulcers, must be distinguished from benign mouth problems because early detection may lead to cure; later detection can lead to radical surgery or death. Teach patients to see their dentist immediately if they notice white or red patches, persistent sores, swelling, bleeding, numbness, or pain in the mouth.
EYES, EARS, AND NOSE
During the eye examination, note the position, alignment, and general appearance of the eye. Check that eyelashes are distributed equally and curl outward. Note the presence of lesions, nodules, redness, swelling, crusting, flaking, excessive tearing, or discharge of eyelids. Check the color of the conjunctivae.
When examining the ear, note its position, alignment, and general appearance. Pay particular attention to a buildup of cerumen (wax) in the canal, dryness, crusting, or the presence of any discharge or foreign body. Older adults can have a buildup of cerumen that can cause impaired hearing. This is a result of harder, drier cerumen and decreased motility of the cilia in the ear canal.
While examining the nose, note its position and general appearance, patency of the nostrils, and presence of tenderness, dryness, edema, bleeding, discharge, or secretions.
Refer to Chapter 27 for additional information related to nursing assessment of the eyes, ears, and nose.
HAIR
Assess the condition of the hair. Inspect it for texture, cleanliness, and oiliness. Inspect the scalp for any scaling, lesions, inflammation, or infection. Note any abnormalities such as dandruff, hair loss, or infestations. Patients of African American descent may have very dry scalps and dry, fragile hair (Andrews et al., 2020). Patients of Asian descent may have straight hair that does not necessarily require special care (Andrews et al., 2020). When in doubt, ask the patient, a family member, or significant other about the specific manner in which hair care is performed. Refer to Chapter 27 for additional information related to nursing assessment of hair.
Dandruff
Dandruff is a condition characterized by itching and flaking of the scalp and may be complicated by the embarrassment it causes. Persistent, severe cases usually require medical attention, but daily brushing and shampooing with a medicated shampoo may be all that is needed to keep the scalp free of dandruff.
Hair Loss
Hair growth and hair loss are ongoing, daily processes. Hair loss becomes a potential problem only when it exceeds hair growth. Absence or loss of hair is called alopecia. Alopecia on the head is also referred to as baldness. Alopecia can be a partial or complete, local or generalized, loss of hair. Patchy hair loss can result from infections of the scalp. Hair loss from plaiting, excessive backcombing and teasing, or the use of hair rollers is usually temporary; hair returns when the tension on the hair shaft is halted.
Excessive generalized hair loss may occur with infection, nutritional deficiencies, hormonal disorders, childbirth, general anesthesia, drug toxicity, chemotherapy, thyroid disease, liver disease, hepatic and renal failure, and radiation. Alopecia can also occur as part of the aging process. Alopecia related to aging is more common in men than in women. There is no known cure for baldness. Although some medications are currently in use and others are being developed, their long-term efficacy is unknown. For example, minoxidil, a cardiovascular and antihypertensive drug, has reversed balding to some degree when applied to the scalp. Hairpieces, sometimes worn by people who are bald, require the same care as normal hair but less frequent washing.
Hair transplantation is a surgical procedure for baldness. Hair is taken from donor sites, usually from the back or sides of the scalp, and transplanted to areas with no hair. The procedure is long and expensive but reportedly has decided benefits for people who find baldness psychologically unpleasant. Complications include serious scalp infections.
Pediculosis
Infestation with lice is called pediculosis. There are three common types of lice: Pediculus humanus capitis, which infests the hair and scalp; Pediculus humanus corporis, which infests the body; and Phthirus pubis, which infests the shorter hairs on the body, usually the pubic and axillary hair. Lice lay eggs, called nits, on the hair shafts. Nits are white or light gray and look like dandruff but cannot be brushed or shaken off the hair. Frequent scratching and scratch marks on the body and the scalp suggest the presence of pediculosis. Pediculosis can be spread directly by contact with the hair of infested people. It is less common for transmission to occur indirectly through contact with clothing, bed linen, brushes, and combs of infested people. Treatment for pediculosis is discussed in the Providing Hair Care discussion on page 1111.
NAILS AND FEET
Examine nails for intactness and cleanliness. Assess capillary refill and the contour of the nail bed. Observe the nail base for redness, swelling, bleeding, discharge, and tenderness. Patients with dark skin tones may have freckles or pigmented streaks in their nails and nails may be thicker (Jarvis & Eckhardt, 2020). Examine the feet for cleanliness and intactness of skin, and note any swelling, inflammation, lesions, tenderness, or orthopedic problems. Carefully examine the skin between the toes. Refer to Chapter 27 for additional information related to nursing assessment of the nails and feet.
PERINEAL AND VAGINAL AREAS
Examine the male genitalia for color, lesions, swelling, inflammation, excoriation, tenderness, and discharge (amount, color, odor, source). Examine the female genitalia for color, lesions, masses, swelling, inflammation, excoriation, tenderness, and discharge (amount, color, odor, source). Inspect the anal area for cracks, nodules, distended veins, masses, or polyps. Note any perineal odors. Refer to Chapter 27 for additional information related to nursing assessment of the perineum.
Diagnosing Actual or Potential Health Problems and Needs
An assessment of a patient’s hygiene practices and the skin, mucous membranes, and other body areas may lead to the identification of one or more diagnoses or patient problems related to hygiene. Following the formulation of the diagnoses or patient problems, the nurse communicates findings to other nursing and health care professionals through the use of the written and spoken word. The written diagnosis or patient problem becomes a permanent part of the patient’s health record. Examples of health problems and needs with related etiology and signs and symptoms can be found in the box titled Examples of Actual or Potential Health Problems and Needs: Hygiene.
from power point:
from Knowt lecture recording:
Skin: rashes, bumps, dryness, itching, recent wounds, tattoos or piercings, lesions.
Oral cavity: nutrition, refined sugars, dental caries (cavities); family history of periodontal disease; chemo-related oral lesions; high-risk states (ill, comatose, dehydrated, depressed, paralyzed).
Oral health terms to know:
Stomatitis: inflammation of the oral mucosa.
Glossitis: inflammation of the tongue.
Cheilosis: dry, cracked corners of the mouth.
Hair: malnutrition, treatments or conditions causing hair loss (e.g., chemotherapy, hypothyroidism).
Nails and feet: self-care deficits, vascular disease, arthritis, ill-fitting shoes; diabetes-specific foot assessment.
4.Formulate diagnoses/patient problems related to hygiene amenable to nursing intervention.
from my personal lecture notes: self-care deficit, impaired social interaction, increased risk for infection due to decreased skin integrity, get them to verbalize that ehy feel clean, demonstrate the correctskin care measures, verbalize importance of good oral hygiene, demonstrate proper care of visual/auditory aids, ALWAYS CHECK BATHE TEMP FIRST and LEAVE DOOR UNOCKED.
from book:
Diagnosing Actual or Potential Health Problems and Needs
An assessment of a patient’s hygiene practices and the skin, mucous membranes, and other body areas may lead to the identification of one or more diagnoses or patient problems related to hygiene. Following the formulation of the diagnoses or patient problems, the nurse communicates findings to other nursing and health care professionals through the use of the written and spoken word. The written diagnosis or patient problem becomes a permanent part of the patient’s health record. Examples of health problems and needs with related etiology and signs and symptoms can be found in the box titled Examples of Actual or Potential Health Problems and Needs: Hygiene.
Examples of Actual or Potential Health Problems and Needs
HYGIENE
Actual or Potential Health Problems and Needs
Possible Etiologic Factors
Potential Signs and Symptoms
Bathing/hygiene ADL deficit
Sensory, cognitive, endurance, mobility, or motivation deficits; low value attached to regular bathing, brushing, flossing, and dental examinations; pain
“I don’t need a bath. I’m not dirty.” Five days postoperative from left thoracotomy. Transient confusion, generalized postoperative weakness. Unable to ambulate more than a few steps with assistance of two caregivers.
Impaired socialization
Negative body image
“I hate the way I look. Everyone stares at me. I don’t even feel like going to school.” Sixteen-year-old boy has come to the pediatrician’s office for a physical for his driver’s license permit. He has severe acne involving his face, neck, and back.
Risk for Impaired Oral Mucous Membrane Integrity
Inadequate oral hygiene, immunosuppression, inadequate nutrition, dehydration
from power point:
from Knowt lecture recording:
Nursing diagnoses related to hygiene:
Hygiene Self-Care Deficit
Impaired Oral Mucosa Membrane Integrity
Risk for Impaired Skin Integrity
Readiness for Enhanced Self-Care
Social Isolation concerns related to poor self-care or stigma (e.g., colostomies).
5.Describe agents commonly used on the skin and scalp, including any precautions related to their use.
from my personal lecture notes: more expensive does not equal better, bar soaps are good especially ecconomically, keep body/clothes clean best way to prevent BO, brushes and applicators should be kept clean, toss cosmetics after 2-4 months
from Knowt lecture recording:
Good hygiene practices are strongly linked to health outcomes (e.g., brushing teeth reduces cavities).
Hygiene education and resources:
Teach about sun protection; sunscreen should be applied 20-30 minutes before sun exposure and checked for expiration.
Do not share cosmetics; discard cosmetics after 2-4 months; keep brush/appliance/tools clean.
Emphasize that inexpensive products (e.g., bar soap) can be effective; hygiene does not require expensive products.
6.Plan, implement, and evaluate nursing care related to diagnoses/patient problems involving alterations in and related to hygiene.
from my personal lecture notes: skin barriers, hair care/cosmetics, if able to do by self then allow for it, know what’s done in the morning/evening/afternoon/PRN, how are they participating, has it reduced
from book:
Outcome Identification and Planning
The plan of care identifies nursing measures to assist the patient to develop or maintain hygiene practices that contribute to a sense of well-being. The following are examples of appropriate outcomes. The patient will:
• verbalize feeling comfortable and clean.
• participate fully in necessary hygiene measures according to cognitive, sensory, mobility, and endurance abilities.
• maintain intact skin and mucous membranes.
• demonstrate correct skin care measures (when indicated) such as oral care; care of eyes, ears, and nose; nail and foot care; and perineal and vaginal care.
• verbalize importance of good teeth-brushing habits, fluoride use, and regular dental examinations.
• demonstrate proper use and care of visual or auditory aids.
• participate in hair and scalp care as able.
Implementing
When performing general hygiene measures, respect the patient’s personal preferences and encourage as much self-care as the patient can perform. Nurses should implement interventions to meet the patient’s need for privacy, and promote physiologic and psychological wellness.
QSEN PATIENT-CENTERED CARE
Cultural, ethnic, family, and social backgrounds contribute to a patient’s values regarding personal hygiene measures. Individualized care respects and encourages individual expression of patient values, preferences, and needs.
The following sections discuss hygiene measures, including providing scheduled care; assisting with bathing and skin care; massaging; providing routine hygiene care; providing environmental care, including making the bed; and teaching patients about skin care. Refer to the accompanying Focus on the Older Adult display for interventions related to hygiene for this age group.
Nurses who role model good health behaviors are more effective teachers. Use the Promoting Health 32-1 (on page 1098) display for yourself before using it with others.
Providing Scheduled Hygiene Care
When patients require nursing assistance with personal hygiene, provide this care at regular intervals. In most hospitals and long-term care settings, early morning care, morning care, afternoon care, hour of sleep care, and care as needed are provided. These are individualized according to the patient’s personal and cultural preferences. Personal care assistance in the home and other community-based settings centers on patient preferences and routines. Personal care measures may be delegated to assistive personnel (AP). The nurse is responsible for ensuring that hygiene measures are performed satisfactorily and validates, analyzes, documents, communicates, and acts on any items noticed during care and communicated by AP.
EARLY MORNING CARE
Shortly after the patient awakens, assist with toileting if necessary and then provide comfort measures to refresh the patient and prepare them for breakfast (or diagnostic tests, procedures, or therapies). Nursing measures include washing the face and hands and providing mouth care.
MORNING CARE (AM CARE)
In many care environments, it is usual to complete morning care after breakfast. However, patient preferences and scheduled activities should be considered. For example, in rehabilitation settings, patients participate in physical and occupational therapy sessions for a majority of the daytime hours and patient bathing and other personal hygiene measures will be addressed in the evening.
Depending on the patient’s self-care abilities, offer assistance with toileting, oral care, bathing, back massage, special skin care measures (e.g., pressure injury), hair care (includes shaving if indicated), cosmetics, dressing, and positioning for comfort. Facility policies are followed for refreshing or changing bed linens, and the patient’s bedside area is tidied. In the home and other community-based settings, patient and/or family preferences and routines should be considered. When morning care is completed, the patient should feel refreshed and should be in a comfortable and safe environment.
Morning care is often categorized as self-care, partial care, or complete care. Patients identified as self-care are capable of managing their personal hygiene independently once oriented to the bathroom. However, offer a back massage and spend time assessing the patient’s day-to-day needs. Patients identified as partial care often receive morning hygiene care at the bedside or seated near the sink in the bathroom. They usually require assistance with body areas that are difficult to reach. Patients identified as complete care require nursing assistance with all aspects of personal hygiene. A complete bed bath is done, or the patient may be taken to the shower.
AFTERNOON CARE (PM CARE)
Hospitalized patients frequently receive visitors in the afternoon or evening or use this time to rest when not scheduled for tests or therapies. Ensure the patient’s comfort after lunch and offer assistance to nonambulatory patients with toileting, handwashing, and oral care. Bathing and other personal care activities may take place at this time, depending on individual patient circumstances.
HOUR OF SLEEP CARE (HS CARE)
In the evening, at the end of the day, again offer assistance with toileting, washing of the face and hands, and oral care. It may be appropriate to offer a back massage or other method of relaxation to help the patient to be calm and fall asleep. Change any soiled bed linens or clothing, and position the patient comfortably. Ensure that the call light and any other objects the patient desires (e.g., urinal, radio, water glass) are within easy reach.
AS NEEDED CARE (PRN CARE)
In addition to scheduled care, offer individual hygiene measures as needed. Some patients require oral care every 2 hours. Patients who are diaphoretic (sweating profusely) may need their clothing and bed linens changed several times a shift. At other times, a nurse may decide to forego hygiene measures because the patient’s need for undisturbed rest may be a higher priority.
Assisting With Bathing and Skin Care
Bathing serves a variety of purposes, including:
• Cleansing the skin
• Acting as a skin conditioner
• Helping a person to relax
• Promoting circulation by stimulating the skin’s peripheral nerve endings and underlying tissues
• Serving as a musculoskeletal exercise through activity involved with bathing, thereby improving joint mobility and muscle tonus
• Stimulating the rate and depth of respirations
• Promoting comfort through muscle relaxation and skin stimulation
• Providing sensory input
• Helping to improve self-image
• Providing an excellent opportunity to strengthen the nurse–patient relationship, to thoroughly assess the patient’s integumentary system, to observe the patient’s physiologic and emotional status closely, to teach the patient as indicated, and to demonstrate care and interest in the patient’s general welfare
The simple act of bathing a patient is a vital and caring intervention. Although APs are increasingly performing hygiene measures, the nurse is responsible for ensuring that hygiene measures are performed satisfactorily. Refer to Chapters 10 and 17 for discussions of the nurse’s accountability when care is delegated. Nurses whose primary focus is the patient, however, can use the time spent on assisting with bathing to establish a rapport with the patient and to further assess the patient’s integumentary system. Bathing is performed in a matter-of-fact and dignified manner. Refer to the accompanying Through the Eyes of a Student.
SHOWER AND TUB BATHS
A shower may be the preferred method of bathing for patients who are ambulatory and able to tolerate the activity. Tub baths may be an option, particularly in long-term care or other community-based settings, depending on facility policy as well as in a patient’s home environment. Tub, or immersion, bathing may be used for purposes other than personal hygiene. Tub bathing can provide positive physical and mental effects, including mental and physical relaxation, decreased stress, and relief of menstrual cramps and labor contractions (Benfield et al., 2018; Goto et al., 2018).
from power point:
plan…
implement…

evaluating…
from Knowt lecture recording:
Hygiene planning and care plans:
Start with a nursing history during bathing; plan to teach and demonstrate back to the patient how to perform hygiene tasks.
Encourage regular dental exams; acknowledge limited access to dental care and seek community resources (free clinics, clinics offering low-cost care).
Teach about the use of hearing/visual aids and how to maintain and replace batteries or chargers.
Bathing as a therapeutic activity:
Cleansing the skin, promoting relaxation, stimulating circulation, and improving comfort.
Bathing enhances sensory input and supports the nurse–patient relationship.
Ensure privacy through proper draping; always provide as much privacy as possible.
Safety and privacy in bathing:
Showers should have non-slip mats/strips; use a shower chair for those with limited standing ability.
Always check water temperature personally before patient use; never assume the environment’s temperature is safe.
Ensure call devices are accessible (e.g., pull cords in shower rooms).
Care schedules and routines:
AM care (after awakening): assist with toileting, refresh, mouth care, wash hands/face, prepare for day; back massage can promote circulation.
After breakfast: toileting, oral care, bathing, linen change.
Afternoon care: toiletry, head washing, oral care, repositioning, potential gown changes.
HS care (before bed): oral care, back massage, linen/clothing changes, ensure call bell and items within reach.
PRN (as needed) care: hygiene measures as required (e.g., frequent lip care for dry lips).
Outcomes for hygiene care:
Clients verbalize comfort and cleanliness; participate in hygiene measures; skin and mucous membranes remain intact.
Demonstrate correct skin and oral care; visual/auditory aids used properly; participate in hair/scalp care; demonstrate knowledge of upkeep and prevention.
Clients understand importance of regular dental exams and follow prescribed hygiene treatments.
Ethical and practical implications:
Maintain patient dignity, privacy, and nonjudgmental attitude during hygiene and mobility care.
Recognize resource limitations and provide alternatives or referrals (e.g., community resources for dental care and sunscreen).
Encourage independence while ensuring safety and support when needed.
Learning Objectives Chapter 34:
1. Describe the role of the skeletal, muscular, and nervous systems in the physiology of movement.
from my personal lecture notes: know that calcium is a very important electrolyte for muscles!
from book:
from power point:
from Knowt lecture recording:
2. Identify variables that influence body alignment and mobility.
from my personal lecture notes: developmental, mental health, lifestyle, physical health, attitude/values, how feels about safety, fatigue, stress, finances, equipment, etc.
from book:
from power point:

from Knowt lecture recording:
Effects of immobility on the body (system-wide impact):
Cardiovascular: increased cardiac workload; risk of orthostatic hypotension; venous stasis and thrombosis.
Respiratory: decreased ventilatory effort; increased secretions.
Musculoskeletal: muscle atrophy, decreased tone and strength, reduced joint mobility, bone demineralization, limited endurance.
Metabolic: muscle wasting, altered protein metabolism, weight changes.
GI: altered digestion and appetite; slower digestion when lying flat after meals; sit up for at least an hour after eating to facilitate digestion.
Urinary: urinary stasis; higher risk of kidney stones and UTIs.
Skin: increased risk of pressure ulcers and skin breakdown.
Psychosocial: feelings of worthlessness or diminished self-esteem; social isolation risk, especially with stigmatized conditions (e.g., colostomy).
Social and environmental influences on mobility:
Support systems and cultural expectations influence exercise adherence.
Realistic, gradual goals increase adherence and reduce frustration.
Safe, accessible environments (e.g., malls with walking groups) can facilitate activity.
3. Differentiate isotonic, isometric, and isokinetic exercises.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
4. Describe the effects of exercise and immobility on major body systems.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Effects of immobility on the body (system-wide impact):
Cardiovascular: increased cardiac workload; risk of orthostatic hypotension; venous stasis and thrombosis.
Respiratory: decreased ventilatory effort; increased secretions.
Musculoskeletal: muscle atrophy, decreased tone and strength, reduced joint mobility, bone demineralization, limited endurance.
Metabolic: muscle wasting, altered protein metabolism, weight changes.
GI: altered digestion and appetite; slower digestion when lying flat after meals; sit up for at least an hour after eating to facilitate digestion.
Urinary: urinary stasis; higher risk of kidney stones and UTIs.
Skin: increased risk of pressure ulcers and skin breakdown.
Psychosocial: feelings of worthlessness or diminished self-esteem; social isolation risk, especially with stigmatized conditions (e.g., colostomy).
5. Assess body alignment, mobility, and activity tolerance, using appropriate interview and assessment skills.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Assessment framework for mobility and activity:
Usual daily activity level, type, frequency, and duration.
Endurance and ability to perform activities without excessive fatigue.
History of dizziness, dyspnea, angina-like symptoms, and relief with rest.
Personal exercise goals, current mobility problems, pain, depression or anxiety.
External factors: environment and finances affecting activity.
Assessment and safety considerations for transfers:
Know patient’s medical diagnosis, mobility restrictions, and whether they can assist with movement.
Assess patient understanding and ability to cooperate with transfer instructions.
Before moving, assess environment and equipment; ensure orderliness and safety.
6. Diagnose actual and potential health problems and needs related to mobility that may be addressed through nursing intervention.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
ity Amenable to Nursing Intervention
Nursing diagnoses related to mobility:
Hygiene self-care deficit (can also be related to mobility issues preventing self-care).
Risk for impaired skin integrity.
Social isolation concerns related to poor self-care or stigma (e.g., colostomies).
Mobility outcomes:
Improved ease of movement and gait; normal body alignment and joint function; preserved muscle mass and tone.
Adherence to an exercise program; demonstration of correct body alignment and full ROM.
Absence of skin integrity alterations; intact venous return (calf refill).
Freedom from contractures; ability to perform functional ADLs.
7. Utilize principles of ergonomics when appropriate.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Ergonomics and basic principles for safe patient handling:
Use proper draping; protect patient dignity and privacy.
Use ergonomics: face direction of movement, plan before lifting, bend knees, keep back straight, and avoid twisting.
Ensure the floor is dry and surfaces are clear before any movement.
8. Use safe patient handling and mobility techniques and equipment when positioning, moving, lifting, and ambulating patients.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Equipment and devices for safe movement and transfers:
Draw sheet (cloth or disposable) to reduce shear forces; friction-reducing devices (Dirashi / friction-reducing sheet) to prevent skin tears.
Gait belts, placed around the waist; do not use with abdominal/thoracic injuries.
Lateral assist devices, transfer boards, roller boards, sideboards, inflatable mattresses as needed.
Full-body lift slings for patients who cannot bear weight; ensure proper positioning and locking of equipment.
Foot support (footboard) to prevent foot drop; trochanter rolls to prevent outward femur rotation, especially after hip procedures.
Trapeze bars to assist with repositioning and strengthening of upper body.
Assessment and safety considerations for transfers:
Use assistive devices for lifting > 35 lb; ensure adequate staffing.
Clear transfer area of obstacles; lock all wheels on beds/gurneys; prepare and check equipment (gait belts, transfer boards, friction-reducing sheets).
When using a full-body sling or lift, place the sling correctly and ensure patient is secure.
Practical transfer techniques:
Use a gait belt and position yourself behind and to the side of the patient.
If patient has weakness on one side, stand on the weaker side to help stabilize.
Use a draw sheet to minimize skin tearing and friction; friction-reducing devices when moving laterally or around beds.
Ensure multiple caregivers for heavier patients (e.g., >200 lb) and plan for assistance to prevent injury to both patient and staff.
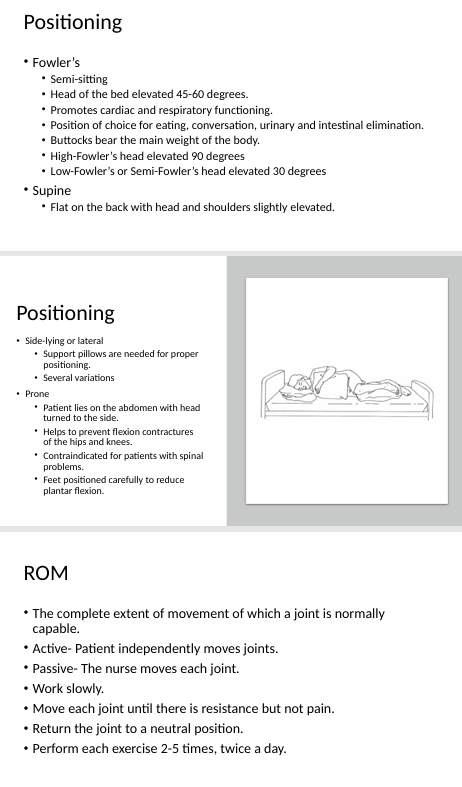
Positioning and postural care:
Fowler's position: 45^{\circ}-60^{ \circ}; High Fowler's: 90^{\circ}; Low Fowler's: 30^{\circ}; Supine; Side-lying; Prone; Prone with head turned; Prone contraindicated for spine problems.
Trochanter rolls to keep hips aligned; footboards to prevent plantarflexion and foot drop; keep legs from rotating.
Use adjustable beds to facilitate repositioning and reduce friction; trapeze bar helps with repositioning and strengthening; some beds have air pressure to reduce shearing forces.
Ensure pressure relief by turning patients every two hours; document positions; many rooms use a clock-like system for positioning.
Positioning and turning schedules:
Turn patients every two hours; document the position to ensure all positions are used.
Use a clock-based positioning plan or bed-label system to guide turns and ensure thorough repositioning.
Special precautions and reminders:
Foot drop prevention: use footboards and avoid prolonged plantar flexion.
Trochanter rolls to keep hips aligned and prevent outward rotation of the femurs.
Trapeze bar can aid repositioning and upper body strengthening; patient can grasp it to help reposition.
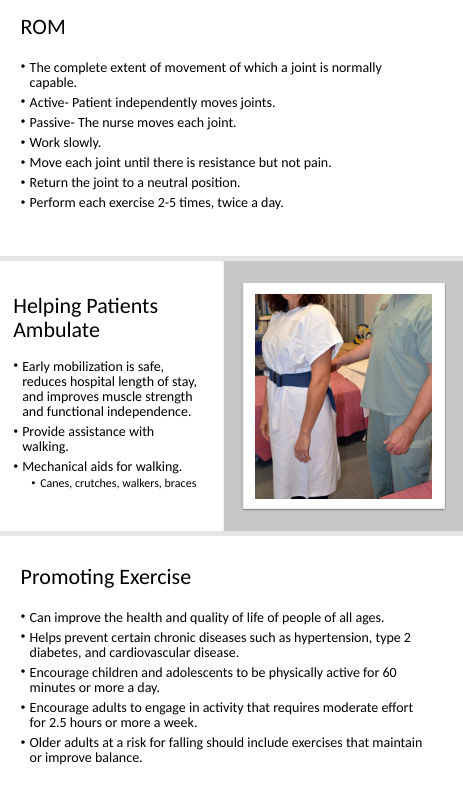
Early mobilization and ambulation:
Early mobilization is safe and reduces hospital length of stay; improves muscle strength and functional independence.
Ambulation often requires staff support; use gait belt and assistive devices when needed.
For safe ambulation: walk behind and slightly to the side of the patient; stand on the weaker/affected side to stabilize; support the patient’s forearm as needed.
Ensuring safe transfer requires adequate staffing; never attempt transfers alone; check environment and equipment locks; ensure pain control before moving when possible (30-45 minutes after analgesia).
Summary of key formulas and numbers (LaTeX):
Fowler’s position ranges: 45^{\circ}-60^{\circ} degrees; High Fowler’s: 90^{\circ}; Low/Medium Fowler’s: 30^{\circ} degrees.
Lifting threshold for assistance: if lift exceeds 35 lb, use assistive devices and additional staff.
Turn frequency: every 2 hours.
9. Develop exercise programs.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Mobility and exercise guidelines:
Children: at least 60 minutes of physical activity daily.
Adults: at least 2.5 hours of moderate-intensity activity per week.
Older adults and fall risk: include balance-focused activities (e.g., Tai Chi, Yoga).
Initiating new exercise programs requires medical clearance if risk factors exist (heart disease, asthma, diabetes, kidney disease, arthritis, etc.).
Two or more risk factors prompt medical evaluation before starting exercise: e.g., age thresholds, smoking, inactivity, obesity, hypertension, elevated cholesterol, impaired glucose tolerance.
Social and environmental influences on mobility:
Realistic, gradual goals increase adherence and reduce frustration.
Summary of key formulas and numbers (LaTeX):
Exercise guidelines:
Children: at least 60 minutes per day.
Adults: at least 2.5 hours per week of moderate-intensity activity.
10.Plan, implement, and evaluate nursing care related to select diagnoses/patient problems involving alterations in and related to mobility.
from my personal lecture notes:
from book:
from power point:
planning…
implement…
evaluating…
from Knowt lecture recording:
Early mobilization and patient education:
Engage patients in their activity plans; emphasize gradual progress and realistic goals.
Teach and have patients demonstrate safety techniques, such as proper body mechanics and safe transfer methods.
Regularly assess pain and adjust mobility plans accordingly to maintain safety and comfort.
ROM and mobility:
ROM terms:
Active ROM: patient moves joints independently.
Passive ROM: nurse moves joints for patient.
Move each joint to a point of resistance but not pain; return to neutral between repetitions.
Typical ROM reps: 2-5 times per joint, twice a day (order may vary by condition).
Range of motion supports movement and helps preserve joint function; focus on joints not freely used.
Summary of key formulas and numbers (LaTeX):
ROM repetitions: 2-5 repetitions per joint, try to perform twice daily.
Closing note: the material emphasizes a holistic, respectful approach to hygiene and mobility, integrating physical safety with dignity and independence. Regular reassessment and adaptation to each client’s context are essential for effective care.
Ethical and practical implications:
Maintain patient dignity, privacy, and nonjudgmental attitude during hygiene and mobility care.
Encourage independence while ensuring safety and support when needed.
EXTRA KNOWT STUFF FROM THIS CLASS:Here are the definitions for the key terms you provided:
Active exercise: Patient moves joints independently.
Activities of daily living (ADLs): Basic self-care tasks such as eating, bathing, dressing, grooming, toileting, and transferring.
Aerobic exercise: Exercise that increases heart rate and oxygen intake, often sustained for a period of time (e.g., running, swimming). (Not explicitly defined in the provided text, but common knowledge).
Atrophy: Decrease in the size of a body organ or tissue; wasting away of muscle mass, often due to disuse or immobility.
Contractures: Permanent shortening of a muscle or joint, often leading to deformity, which can result from immobility.
Ergonomics: The science of fitting a workplace to the user's needs to prevent injury and promote efficiency; in healthcare, applying principles to safe patient handling.
Flaccidity: Lack of muscle tone; limp.
Footdrop: The inability to dorsiflex the foot due to weakness or paralysis of the muscles of the lower leg, causing the foot to drag during walking.
Fracture: A break in the continuity of a bone. (Not explicitly defined in the provided text, but common knowledge).
Instrumental activities of daily living (IADLs): More complex activities necessary for independent living, such as managing finances, preparing meals, shopping, and managing medications. (Not explicitly defined in the provided text, but common knowledge).
Isokinetic exercise: Exercise involving muscle contraction with resistance that changes to maintain a constant speed of movement. (Not explicitly defined in the provided text, but common knowledge).
Isometric exercise: Exercise where muscle length does not change, and the joint angle does not change, even though muscle contraction occurs (e.g., pushing against an immovable object). (Not explicitly defined in the provided text, but common knowledge).
Isotonic exercise: Exercise where the muscle length changes, and the joint angle changes through a range of motion (e.g., lifting weights). (Not explicitly defined in the provided text, but common knowledge).
Orthopedics: The branch of medicine dealing with the correction of deformities of bones or muscles. (Not explicitly defined in the provided text, but common knowledge).
Paralysis: Loss of ability to move (and sometimes to feel anything) in part or most of the body.
Paresis: A condition of muscular weakness caused by nerve damage or disease; partial paralysis.
Passive exercise: Nurse moves joints for patient.
Range of motion (ROM): The full movement potential of a joint, usually expressed in degrees of a circle.
Safe patient handling and mobility (SPHM): Techniques and equipment used to safely move and transfer patients, minimizing injury risk for both patients and caregivers.
Spasticity: A state of increased muscle tone with heightened tendon reflexes.
Strength and endurance exercises: Activities designed to increase muscle power and the ability of muscles to sustain effort over time. (Not explicitly defined in the provided text, but common knowledge).
Stretching exercise: Activities that lengthen muscles to improve flexibility and range of motion. (Not explicitly defined in the provided text, but common knowledge).
Tonus: The normal state of balanced muscle tension existing in the body, which is present even at rest.
Alopecia: Hair loss, which can be caused by malnutrition, treatments, or conditions like chemotherapy or hypothyroidism.
Caries: Tooth decay or dental cavities.
Cerumen: Earwax.
Cheilosis: Dry, cracked corners of the mouth.
Gingivitis: Inflammation of the gums, often caused by plaque accumulation. (Not explicitly defined in the provided text, but closely related to periodontal disease mentioned).
Glossitis: Inflammation of the tongue.
Halitosis: Bad breath. (Not explicitly defined in the provided text, but related to oral hygiene).
Pediculosis: Infestation with lice. (Not explicitly defined in the provided text, but related to hair/scalp hygiene).
Periodontitis: A serious gum infection that damages the soft tissue and, without treatment, can destroy the bone that supports your teeth (mentioned as 'periodontal disease' in the text).
Personal hygiene: Practices such as bathing, brushing teeth, and general body care that promote health and well-being.
Plaque: A sticky, colorless film of bacteria that constantly forms on our teeth. (Not explicitly defined in the provided text, but related to dental caries and oral hygiene).
Stomatitis: Inflammation of the oral mucosa.
Tartar: Hardened plaque that can form on teeth (also known as calculus). (Not explicitly defined in the provided text, but related to dental caries and oral hygiene).
Key Information
Details/Purpose
Diabetes Foot Care
Crucial due to infection risk and neuropathy; assess for redness, swelling, skin breaks, ulcers. Patients should demonstrate inspection.
Lifting Threshold for Staff Assistance
If lift exceeds 35 lb, use assistive devices and additional staff to prevent injury.
Patient Turning Frequency
Turn patients every 2 hours to ensure pressure relief and prevent skin breakdown; document positions using a clock-like system.
Foot Drop Prevention
Use footboards and avoid prolonged plantar flexion to prevent the inability to dorsiflex the foot.
Trochanter Rolls
Used to keep hips aligned and prevent outward femur rotation, especially after hip procedures.
Trapeze Bars
Assist patients with repositioning and strengthening of the upper body.
Water Temperature Check
Always check water temperature personally before patient use during bathing; never assume environmental temperature is safe.
Patient Privacy and Dignity
Ensure privacy through proper draping and maintain patient dignity at all times during hygiene and mobility care.
Early Mobilization Benefits
Safe, reduces hospital length of stay, and improves muscle strength and functional independence.
Range of Motion (ROM) Repetitions
Typically 2-5 repetitions per joint, performed twice a day, moving to resistance but not pain.
Sunscreen Application
Apply 20-30 minutes before sun exposure; check expiration dates.
Cosmetics Hygiene
Do not share cosmetics; discard after 2-4 months; keep brushes/tools clean.
Patient Education & Demonstration
When teaching hygiene or mobility tasks, plan for the patient to demonstrate back to ensure understanding and ability.
Regular Dental Exams
Encourage regular dental exams; acknowledge limited access and seek community resources for low-cost care when needed.
Blended Competencies, Clinical Reasoning and Person-Centered Care (Chapter 13):
Describe each element of thoughtful, person-centered practice
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Thoughtful, person-centered practice integrates several professional attributes and a systematic approach to care:
Professional Nurse Attributes (Chapter 13, Page 349): These are essential for person-centered care.
Open-mindedness: Willingness to consider new ideas and perspectives.
Humility: Understanding your own limitations and the value of others.
Profound Sense of the Value of the Person: Recognizing and respecting the inherent worth of every individual, especially in vulnerable states.
Self-awareness of Own Beliefs: Understanding how personal beliefs influence practice.
Sense of Personal Responsibility for Actions: Acknowledging that every action has an outcome and consequence.
Motivation: Drive to learn and improve.
Leadership Skills: Developing these skills for BSN-prepared nurses stepping into leadership roles.
Describe the historic evolution of the nursing process
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Describe the nursing p-rocess and each of its five phases
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
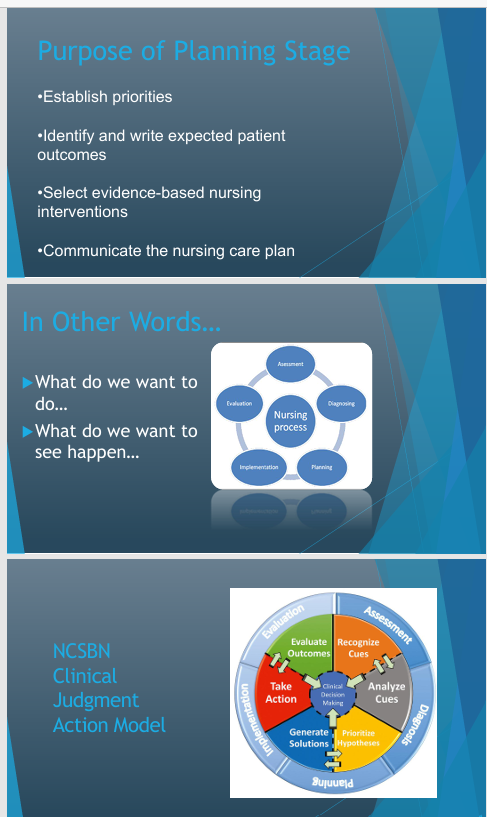
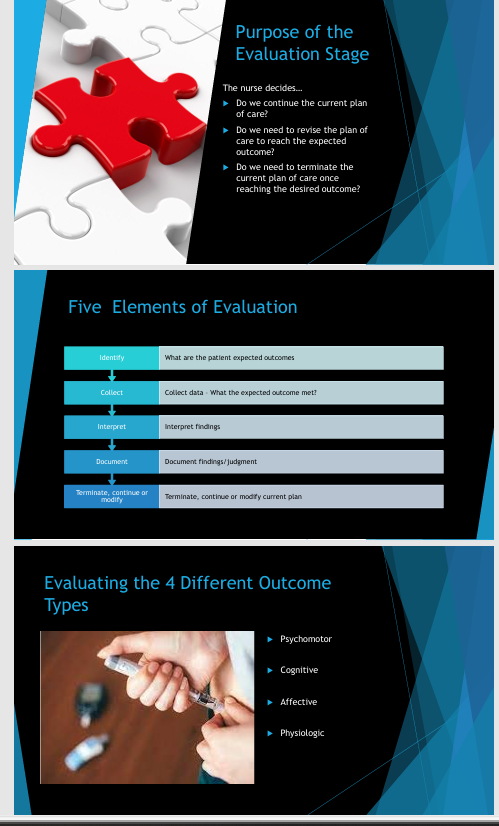
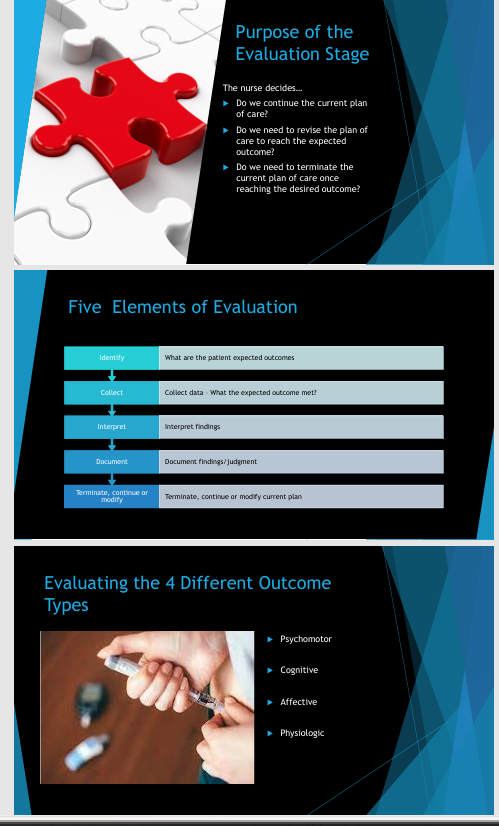
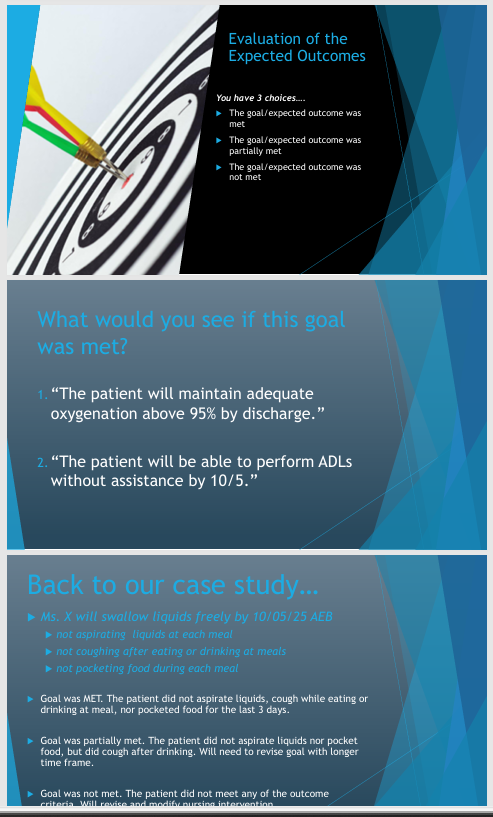
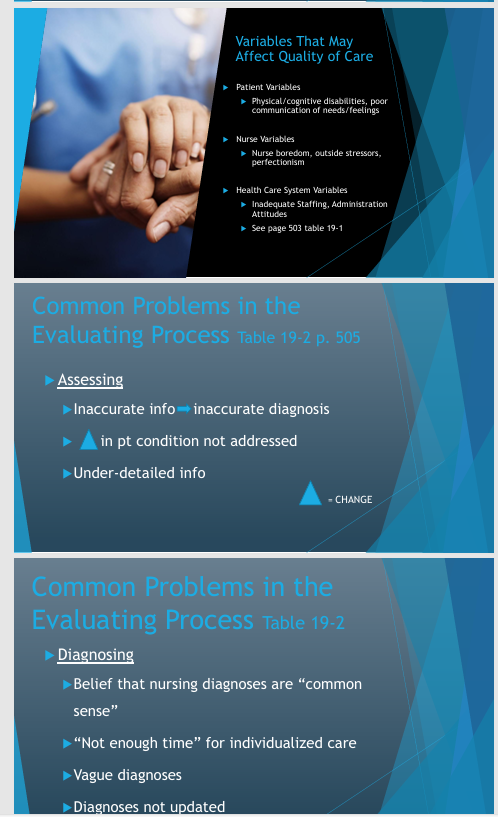
The Nursing Process and Its Five Phases
The nursing process is the systematic way nurses think and provide patient care, foundational to developing a plan of care.
Definition: Outlines the systematic way nurses think and provide patient care. It becomes rapid with experience but should be followed step-by-step by novice nurses.
Distinction: The nursing process and care planning are not the same. The nursing process is used to develop a plan of care.
Five Steps:
Assessment: Gathering data about the client's health status.
Diagnosis: Identifying the client's health problems.
Planning: Establishing goals and interventions.
Implementation: Carrying out the interventions.
Evaluation: Determining the effectiveness of the interventions and plan.
Compare the different blended competencies
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Blended Competencies
The professional attributes listed above can be considered blended competencies essential for effective nursing practice. These competencies blend cognitive, technical, interpersonal, and ethical skills, enabling nurses to provide holistic, patient-centered care.
Clinical Judgment (Chapter 14):
Describe the concepts of critical thinking, clinical reasoning, and clinical judgment.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Concepts of Critical Thinking, Clinical Reasoning, and Clinical Judgment
Critical Thinking: A general cognitive skill relevant to everyday life (e.g., figuring out how to open a difficult box). It can be developed over time.
Clinical Reasoning: The entire process of thought a nurse uses to come to a conclusion. It's the precursor to clinical judgment.
Clinical Judgment: The final decision or conclusion reached after engaging in clinical reasoning. The NCLEX assesses your ability to make safe clinical judgments for patient care.
Discuss the nurse’s responsibility in making clinical decisions.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Nurse's Responsibility in Making Clinical Decisions
Nurses are responsible for making safe clinical judgments and decisions for patient care, which is a core component assessed by the NCLEX. This responsibility is enacted through the application of the Clinical Judgment Model and prioritization frameworks.
Describe cognitive theories used in clinical decision making.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Discuss various models related to clinical judgment.
from my personal lecture notes:
from book:
from power point:

from Knowt lecture recording:
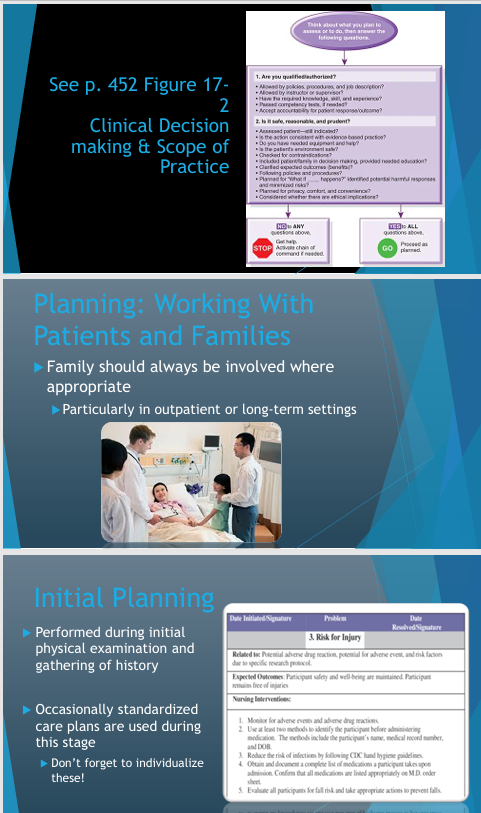
Models Related to Clinical Judgment
Clinical Judgment Model (CJM) and NCLEX Preparation: The NCLEX exam is based on the Clinical Judgment Model.
Steps of the CJM (and Nursing Process Alignment):
Recognize Cues (Assessment)
Analyze Cues (Assessment/Diagnosis)
Prioritize Hypotheses (Diagnosis/Planning)
Generate Solutions (Planning)
Take Actions (Implementation)
Evaluate Outcomes (Evaluation)
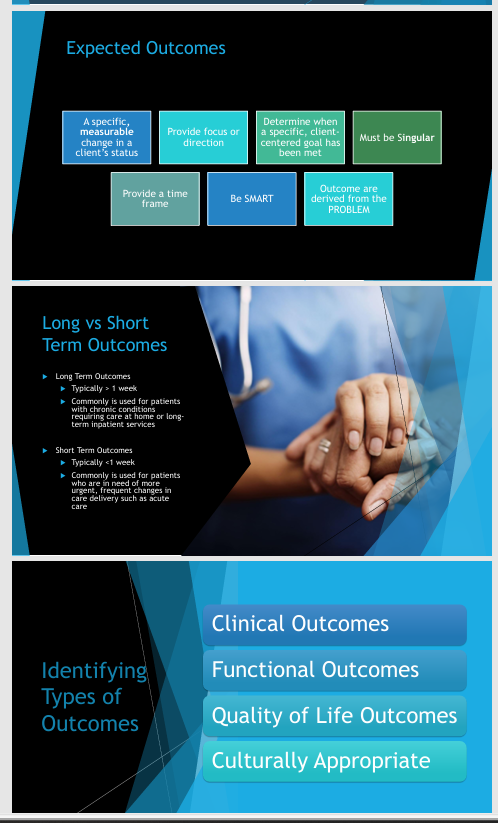
Priority Setting Frameworks for NCLEX: These frameworks help determine which actions or patients to prioritize. NCLEX questions often use bolded keywords like "first," "immediate," or "next action."
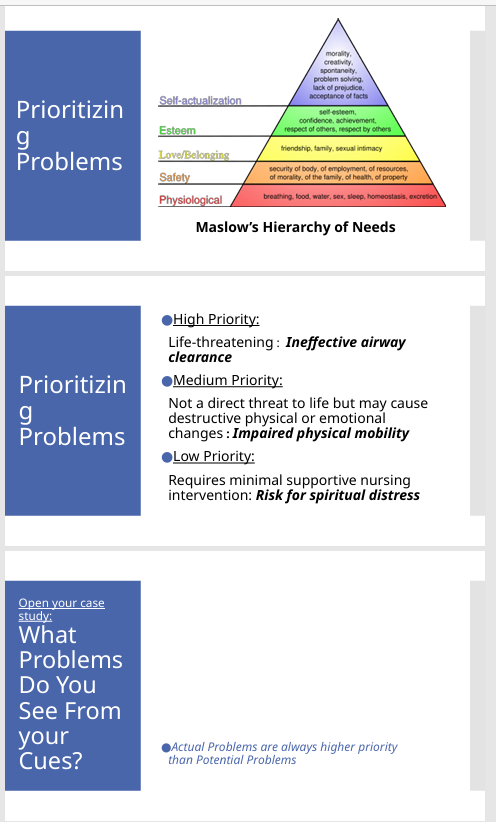
Maslow's Hierarchy of Needs: Prioritize basic physiological needs first, then safety, love, esteem, and self-actualization.
ABCs (Airway, Breathing, Circulation): Always prioritize issues affecting a client's airway, breathing, or circulation.
Safety and Risk Reduction: Address safety risks to the client, especially the greatest threat at that moment.
Least Restrictive/Least Invasive: Always opt for the least restrictive or invasive intervention first.
Acute vs. Chronic, Unstable vs. Stable, Urgent vs. Nonurgent:
Acute: Conditions of sudden onset or short duration (typically prioritized).
Unstable: Condition is changing or unpredictable (prioritized).
General Rule: See the acute, unstable, urgent patient first.
Explain the relationship between clinical experience and critical thinking.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Relationship Between Clinical Experience and Critical Thinking
Critical thinking is a skill developed over time. Clinical experience is crucial for developing and refining assessment skills, which are fundamental to critical thinking and accurate clinical judgment. With experience, the nursing process becomes more rapid and intuitive.
NURSING PROCESS INFORMATION…

Assessment (Chapter 15):
Discuss the steps of nursing assessment
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Steps of Nursing Assessment
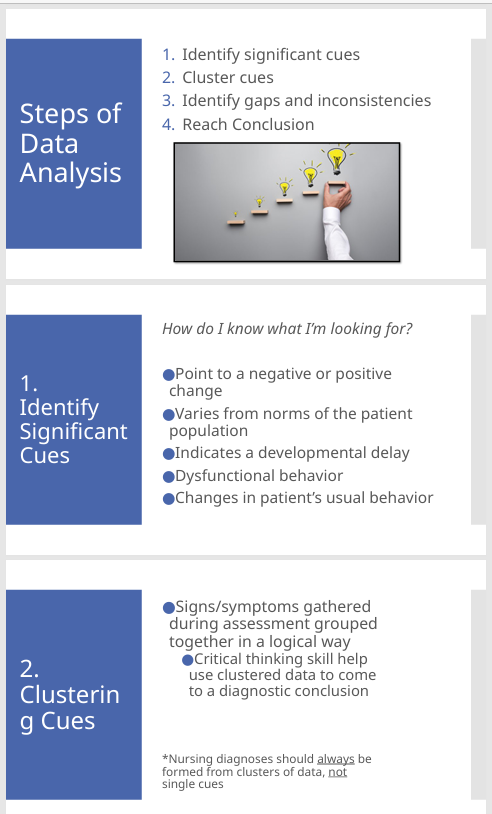
The assessment phase involves gathering data about the client's health status.
Purpose: Determine the patient's current status, identify primary issues, and gather information.
Patient Specificity: Always individualize the assessment and care plan to the patient.
Baseline Assessment: Crucial to perform promptly at the start of a shift or admission to have a reference point.
Trends: Observe trends in vital signs, labs, etc., rather than single data points.
Nurse's "Superpower": Assessment skills are fundamental and developed with experience.
Promoting Clinical Reasoning & Judgment (Page 406-407):
Type of Assessment: Emergent, focused, or comprehensive.
Prioritize: Address the most critical data first.
Complete & Systematic: Follow a logical order (e.g., head-to-toe or body systems).
Accurate: Verify information.
Relevant: Focus on information pertinent to the patient's current health.
Timely: Complete assessments promptly.
Preparing for Data Collection:
Health Orientation/Literacy: Assess patient's understanding.
Developmental Stage: Adjust assessment techniques.
Cultural Considerations: Be aware of cultural influences.
Specific Needs: Adapt based on patient's unique requirements.
Data Collection Methods:
Observation: Using all senses.
Interview: Asking open-ended questions.
Physical Assessment: Inspection, palpation, percussion, auscultation.
Discuss the purpose of competencies related to nursing practice.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Purpose of Competencies Related to Nursing Practice
Competencies, such as the professional attributes discussed, are crucial for ensuring nurses can deliver safe, effective, and person-centered care. They guide the application of the nursing process and clinical judgment to achieve desired patient outcomes.
Differentiate between subjective and objective data.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Differentiating Subjective and Objective Data
Subjective: Perceived by the affected person. Example: Pain (a patient says it's a 2, another a 8).
Objective: Observed and measured. Examples: Vital signs, laboratory values, blood pressure.
Discuss the different sources of data.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Different Sources of Data
Primary Source: The patient (always, unless cognitive impairment or intoxication prevents reliable information).
Secondary Sources: Family members, current and past medical records, medication reconciliation, laboratory and diagnostic test results, therapy notes.
Identify problems related to data collection.
from my personal lecture notes:
from book:
from power point:
from Knowt lecture recording:
Communication Errors to Avoid (Page 407):
Using diminutives ("Honey," "dear").
Talking down (simplistic language like "tummy").
Using excessive medical jargon.
Ignoring nonverbal cues.
Nurse's nonverbal cues (showing shock or disgust).
Interview Issues and Nursing Responses:
Anxiety: Make patients comfortable, avoid false assurances.
Pain: Alleviate pain to a manageable level.
Language Barriers: Utilize interpreters.
Past Experiences: Acknowledge, reassure, show respect.
Communication: Speak clearly and simply.
Patient Involvement: Promote patient-centered care.
Explain the relationship between data interpretation, validation, and clustering.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Clustering Cues: Problems should be identified from a cluster of cues, not a single cue (e.g., "I feel like I'm choking" alone isn't enough; need facial droop, coughing, etc.). This involves interpreting multiple pieces of data together.
Data Validation and Interpretation: This is implicit in the assessment; ensuring data is "Accurate" means validating it. Interpreting is understanding what the data means, especially when looking at "Trends." The "Phases of Problem Identification" in the diagnosis phase further formalize this process.
Diagnosis (Chapter 16):
ALL POWERPOINTS FROM THE CHAPTER…
Apply basic principles of diagnostic reasoning to identify actual and potential diagnoses, problems, and issues.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
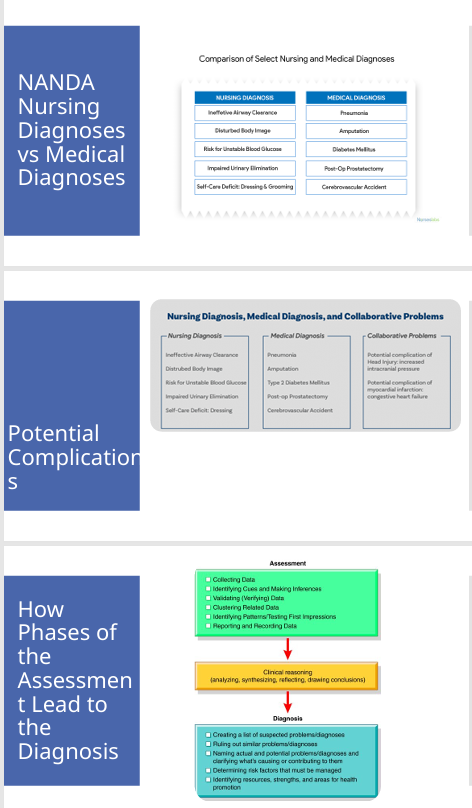
Basic Principles of Diagnostic Reasoning to Identify Actual and Potential Diagnoses, Problems, and Issues
Purpose: Determine and prioritize patient problems. Identify not only actual problems but also potential problems (risk for).
Etiologies: Understand what is causing the problem (e.g., CVA causing dysphagia).
NANDA Terminology: Official terminology for nursing diagnoses (e.g., Ineffective airway clearance, Impaired physical mobility, Self-care deficit).
Collaborative Problems: Potential complications requiring both nursing and medical interventions.
Prioritizing Problems:
Actual vs. Potential: Actual problems are always prioritized over potential (risk for) problems.
Multiple Actual Problems: Prioritize based on Maslow's (physiological first), ABCs (airway first), and urgency/stability.
High Priority: Life-threatening.
Medium Priority: Non-life-threatening but impacts well-being.
Low Priority: Potential issues.
Differentiate between patient problems and medical diagnoses.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording: Nursing Diagnoses/Patient Problems: Focus on the patient's response to health conditions or life processes (e.g., "ineffective airway clearance"). Do not confuse with medical diagnoses.
Medical Diagnoses: Identify diseases or pathophysiological states (e.g., "pneumonia").
Identify nursing diagnoses/problems from a nursing assessment.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Nursing problems are identified by analyzing and clustering cues gathered during the assessment phase. For example, a cluster of cues like frequent coughing, pocketing food, and verbal reports of choking indicates a problem of "Impaired Swallowing."
Refer to the "Case Study Application: Identifying & Prioritizing Problems" for an example of how identified cues lead to specific nursing problems.
Describe the four steps involved in data interpretation
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Clustering Cues: Grouping related subjective and objective data to identify patterns. Verify Data: Confirming the accuracy and reliability of the collected data. Analyze Data / Clinical Reasoning: Critically thinking about what the clustered and verified data means in the context of the patient's health. Identify Gaps: Recognizing any missing or unclear information that requires further assessment.
Chapter 13 (Professional Attributes): While there won't be a dedicated PowerPoint, the content is integrated into the nursing process and care planning. It is important reading, especially page 349.
Professional Nurse Attributes (Chapter 13, Page 349)
These are essential attributes for nursing professionals:
Open-mindedness: Willingness to consider new ideas and perspectives.
Humility: Understanding your own limitations and the value of others.
Profound Sense of the Value of the Person: Recognizing and respecting the inherent worth of every individual, especially in vulnerable states.
Self-awareness of Own Beliefs: Understanding how your personal beliefs influence your practice.
Sense of Personal Responsibility for Actions: Acknowledging that every action has an outcome and consequence.
Motivation: Drive to learn and improve.
Leadership Skills: As a BSN-prepared nurse, you will be expected to step into leadership roles (e.g., charge nurse) relatively quickly, so developing these skills is crucial.
Bravery to Question the System: Advocating for your patients and questioning processes if they are not right, especially concerning systemic problems (e.g., medication errors, which are often system-based).
Clinical Judgment Model (CJM) and NCLEX Preparation
NCLEX Basis: The NCLEX exam is based on the Clinical Judgment Model.
Steps of the CJM (and Nursing Process Alignment):
Recognize Cues (Assessment)
Analyze Cues (Assessment/Diagnosis)
Prioritize Hypotheses (Diagnosis/Planning)
Generate Solutions (Planning)
Take Actions (Implementation)
Evaluate Outcomes (Evaluation)
NCLEX Pass Rates: The most recent NCLEX pass rate was 88.6 ext{%}. While the benchmark required by accrediting bodies is above 80 ext{%}, the goal is to achieve a 90 ext{%+} pass rate.
Note: NCLEX pass rates are often reported based on the State Board of Nursing calendar ( ext{July } 1^{st} ext{}- ext{June } 30^{th} ext{} ), which can affect numbers between graduating classes.
Prioritization: The biggest area where students fail the NCLEX is prioritization. It is critical to practice and master this skill.
Recommendation: Start doing ATI questions now to get accustomed to the question format and critical thinking required.
Understanding Key Concepts
Critical Thinking: A general cognitive skill relevant to everyday life (e.g., figuring out how to open a difficult box). It can be developed over time.
Clinical Reasoning: The entire process of thought a nurse uses to come to a conclusion. It's the precursor to clinical judgment.
Clinical Judgment: The final decision or conclusion reached after engaging in clinical reasoning. The NCLEX assesses your ability to make safe clinical judgments for patient care.
Computerized Adaptive Testing (CAT) for NCLEX:
The exam adapts to your performance: a correct answer leads to a harder question, a wrong answer leads to an easier question.
Minimum Questions: 85
Maximum Questions: 150
Outcome: If your performance consistently falls below a predetermined 'safety line,' you fail the exam, indicating you are not deemed safe to care for patients.
Situational Awareness: Your perception and understanding of the environment around you, particularly in a clinical setting.
60 ext{ Second} Situational Assessment Example: Upon entering a room, observe immediately:
Oxygen presence and function (Is it on?)
IV patency (Is it running? Infiltrated?)
Safety hazards (Cords across the floor, bed alarm on/off)
Patient status (ABCs - Airway, Breathing, Circulation).
NCLEX Key Term: The NCLEX typically uses "client" instead of "patient."
Nursing Process Overview (The Nurse's Thinking Framework)
Definition: The nursing process outlines the systematic way nurses think and provide patient care. It becomes rapid with experience but should be followed step-by-step by novice nurses.
Distinction: The nursing process and care planning are not the same. The nursing process is used to develop a plan of care.
Five Steps:
Assessment: Gathering data about the client's health status.
Diagnosis: Identifying the client's health problems.
Planning: Establishing goals and interventions.
Implementation: Carrying out the interventions.
Evaluation: Determining the effectiveness of the interventions and plan.
NCLEX Test Plan (Access on Blackboard)
Content: This document outlines everything you will be tested on for the NCLEX (current version effective until March 2026 ext{}, new version likely by your graduation in 2027 ext{}).
Categories of Client Needs:
Safe and Effective Care Environment (e.g., Management of Care – 18 ext{%} of test content)
Health Promotion and Maintenance
Psychosocial Integrity (common area of struggle: therapeutic communication)
Physiological Integrity (common area of struggle: pharmacology, physiological adaptation)
Recommendation: Take time to review the NCLEX test plan to understand content areas and typical percentages.
Next Generation NCLEX (NGN): Includes alternate format questions, such as case studies with multiple questions, to prepare you for clinical judgment.
Priority Setting Frameworks for NCLEX
These frameworks help determine which actions or patients to prioritize. NCLEX questions often use bolded keywords like "first," "immediate," or "next action."
Maslow's Hierarchy of Needs: Prioritize basic physiological needs first, then safety, love, esteem, and self-actualization.
Example Question: A nurse is planning care for a client with bipolar disorder experiencing an acute manic episode. Which is the highest priority intervention?
Answer: Providing food and water (physiological need) – e.g., offering fluids and finger foods (Option B)..
ABCs (Airway, Breathing, Circulation): Always prioritize issues affecting a client's airway, breathing, or circulation.
Example Question: A client is wheezing and gasping for breath after receiving amoxicillin. Which action is the nurse's priority?
Answer: Elevating the head of the bed (to improve breathing) – e.g., administering oxygen (Option A)..
Safety and Risk Reduction: Address safety risks to the client, especially the greatest threat at that moment.
Risk Assessment: What is the greatest risk? Compare significant risk factors.
Example Question: A client is experiencing acute alcohol withdrawal. Which medication should the nurse administer first?
Context: Alcohol withdrawal can lead to seizures and increased anxiety.
Medications: Disulfiram (for chronic alcohol disorder), Lorazepam/Ativan (for anxiety and to prevent seizures), Clonidine (for high blood pressure), Atenolol (beta-blocker for heart rate/blood pressure).
Answer: Lorazepam (Ativan) to prevent seizures and manage acute anxiety/withdrawal symptoms (Option B).
Least Restrictive/Least Invasive: Always opt for the least restrictive or invasive intervention first.
Example (Cardiac): Stress test before a heart catheterization.
Example Question: A client is agitated and combative in a chair. What action should the nurse perform first?
Answer: Providing therapeutic communication and de-escalation techniques (Option B) before considering restraints.
Restraints: Require a doctor's order within a specific timeframe (can be initiated for safety, then order obtained). Requires hourly documentation (circulation checks, toileting, water, turning, skin integrity).
Acute vs. Chronic, Unstable vs. Stable, Urgent vs. Nonurgent:
Acute: Conditions of sudden onset or short duration (typically prioritized).
Chronic: Long-standing conditions.
Unstable: Condition is changing or unpredictable (prioritized).
Stable: Condition is not changing.
Urgent: Requires immediate attention (prioritized).
Nonurgent: Can be addressed later.
General Rule: See the acute, unstable, urgent patient first.
The Nursing Process: Detailed Steps
1. Assessment (Data Collection)
Purpose: Determine the patient's current status, identify primary issues, and gather information.
Patient Specificity: Always individualize the assessment and care plan to the patient, even if multiple patients have the same medical diagnosis (e.g., pneumonia, but different comorbidities).
Baseline Assessment: Crucial to perform promptly at the start of a shift or admission to have a reference point.
Trends: Look beyond single data points; observe trends in vital signs, labs (e.g., declining blood pressure, increasing white blood cell count for infection).
Nurse's "Superpower": Assessment skills are fundamental and developed with experience.
Promoting Clinical Reasoning & Judgment (Page 406-407):
Type of Assessment: Emergent, focused (e.g., respiratory only), or comprehensive.
Prioritize: Address the most critical data first.
Complete & Systematic: Don't leave anything out; follow a logical order (e.g., head-to-toe or body systems).
Accurate: Verify information, especially if the primary source (patient) has cognitive impairment (e.g., dementia).
Relevant: Focus on information pertinent to the patient's current health.
Timely: Complete assessments promptly.
Communication Errors to Avoid (Page 407):
Using diminutives: "Honey," "dear," "sweetie," "pop," "grandma."
Talking down: Using overly simplistic language ("tummy" instead of "stomach").
Using excessive medical jargon: Explain terms in layperson's language.
Ignoring nonverbal cues: Pay attention to patient body language.
Nurse's nonverbal cues: Maintain a poker face; avoid showing shock or disgust (e.g., with large pressure ulcers or colostomy odors) to show respect and empathy.
Preparing for Data Collection:
Health Orientation/Literacy: Assess patient's understanding of health information.
Developmental Stage: Adjust assessment techniques (e.g., pediatric patients).
Cultural Considerations: Be aware of how culture influences health practices.
Specific Needs: Adapt the assessment based on patient's unique requirements (e.g., mobility issues, hearing aids).
Types of Assessment (Page 407-411):
Detailed admission history, shift assessment, focused assessment.
Specific tools: Braden scale for skin breakdown, psychological assessments.
Mnemonic (Box 15-1): Look at Health, Environment, Patient, People in the Room (never assume relationships).
Subjective vs. Objective Data:
Subjective: Perceived by the affected person. Example: Pain is always subjective (e.g., one parent says pain is a 2, another says an 8).
Objective: Observed and measured. Examples: Vital signs, laboratory values, blood pressure.
Sources of Data:
Primary Source: The patient (always, unless cognitive impairment or intoxication prevents reliable information).
Secondary Sources: Family members, current and past medical records (electronic health records facilitate this), medication reconciliation (verifying current meds and doses), laboratory and diagnostic test results, therapy notes (PT/OT progress).
Clinical Implication: The rise of hospitalists (doctors who only work in the hospital) may lead to a loss of continuity of care with primary care physicians post-discharge, but they offer immediate in-house medical attention.
**Data Collection Methods:
Observation: Using all senses (sight, smell, hearing, touch). Develops nursing intuition over time.
Interview: Asking open-ended questions. Maintain eye contact, even when documenting.
Physical Assessment: Inspection, palpation, percussion (less common in hospital, more in mission trips), auscultation.
Interview Issues and Nursing Responses:
Anxiety: Make patients comfortable, but avoid false assurances.
Pain: Alleviate pain to a manageable level so the patient can answer questions effectively (don't over-medicate).
Language Barriers: Utilize interpreters or remote translation services.
Past Experiences: Acknowledge previous negative experiences, reassure the patient of a different approach, show respect and confidence.
Communication: Speak clearly and simply, avoid mumbling.
Patient Involvement: Promote patient-centered care; ensure patients are aware of their plan (e.g., bedside report).
Case Study Application: Recognizing Cues (Assessment)
82 ext{ year old female}, admitted to nursing home with CVA.
Extensive Health History (Significant Cues):
CVA (Cerebrovascular Accident)
TIAs (Transient Ischemic Attacks)
Dementia secondary to vascular disease
Hypertension (uncontrolled, indicating vascular issues)
Dysphagia (pre-existing difficulty swallowing)
Assessment Data (Abnormal Cues and Clues):
Neurological/Cognitive:
Alert, awake, oriented x 1 (responds to name)
Confused about time ("time to go to school") and place ("I don't know this place")
Left side facial droop with saliva on chin/shirt (CVA manifestation)
Right grip weak, left hand no grip
Left leg flaccid (paralysis)
Requires constant questions regarding where to go and what to do
Pulmonary:
Breath sounds: scattered crackles throughout (indicates potential aspiration/pneumonia)
Frequent coughing when drinking
Gastrointestinal/Nutritional:
Pocketing of food in left cheek
Verbalizes: "I feel like I'm choking"
Current diet: regular diet with honey thickened liquids (prescribed, but conflicting with "regular diet" and current symptoms)
Elimination:
Incontinent of urine and stool
Mobility/ADLs:
Requires assistance with bathing, toileting, and eating
Moves around with assistance for transfer to wheelchair but requires constant questions.
Vital Signs:
Temperature: 99.2 ext{}^ ext{o} ext{F} (37.3 ext{}^ ext{o} ext{C}) (slightly elevated)
Respirations: 22 ext{ breaths/min} (slightly elevated)
Heart rate: Irregular rate/rhythm, no murmurs
Blood pressure: 132/76 ext{ mmHg} (within normal range)
Oxygen saturation: 95 ext{%} on room air (acceptable)
Other:
Skin intact and dry (current strength, but risk due to incontinence)
Pins in place and dry (irrelevant cue if no problem indicated)
Denies any pain (subjective finding)
Patient Strengths (Positive Cues):
Alert and awake
Cooperative
No impairment of hearing, wears glasses (correctable vision)
Right leg full range of motion
Skin intact and dry (currently)
Heart rate irregular but no murmurs (no current cardiac diagnosis mentioned)
Abdomen flat, bowel sounds present in all 4 ext{ quadrants} (digestive function)
Able to move self around with assistance to a wheelchair
Denies pain
Last bowel movement was recent yesterday (3 ext{ days ago} from admission?)
2. Diagnosis (Problem Identification / Analysis)
Purpose: Determine and prioritize patient problems. Do not confuse with medical diagnoses (e.g., pneumonia is a medical diagnosis; "ineffective airway clearance" or "respiratory problems" are nursing diagnoses).
Key: Identify not only actual problems but also potential problems (risk for).
Etiologies: Understand what is causing the problem (e.g., CVA causing dysphagia).
NANDA (North American Nursing Diagnosis Association): Official terminology for nursing diagnoses, still used in hospitals but less emphasized in current education for students to memorize three-part statements.
Examples: Ineffective airway clearance (for pneumonia), Disturbed body image (for amputation), Risk for unstable blood glucose (for diabetes), Impaired urinary elimination (post-prostatectomy), Self-care deficit.
Collaborative Problems: Potential complications that require nursing and medical interventions (e.g., increased intracranial pressure from head injury, congestive heart failure from MI).
Nurse's Role: Anticipate potential complications and implement preventative measures (e.g., bringing a wheelchair for an unsteady patient ordered to ambulate).
Phases of Problem Identification (Repetition = Retention):
Collect Data
Cluster Cues
Verify Data
Analyze Data / Clinical Reasoning
Identify Gaps
Reach Conclusion / Problem Identification
Identifying Problems: Look for positive/negative changes, variations from the patient's norm (or normal aging process), developmental delays, or changes in usual behavior (e.g., UTI causing confusion in older adults).
Clustering Cues: Problems should be identified from a cluster of cues, not a single cue (e.g., "I feel like I'm choking" alone isn't enough to diagnose impaired swallowing; need facial droop, coughing, etc.).
Prioritizing Problems:
Actual vs. Potential: Actual problems are always prioritized over potential (risk for) problems.
Multiple Actual Problems: Prioritize based on Maslow's (physiological first), ABCs (airway first), and urgency/stability.
High Priority: Life-threatening (e.g., ineffective airway clearance).
Medium Priority: Non-life-threatening but impacts well-being (e.g., impaired physical mobility).
Low Priority: Potential issues (e.g., risk for falls, risk for impaired skin integrity).
Case Study Application: Identifying & Prioritizing Problems
Based on identified cues, the patient's nursing problems (actual and potential) include:
Impaired Swallowing (Dysphagia) / Risk for Aspiration: Evidenced by frequent coughing when drinking, pocketing food, patient stating "I feel like I'm choking," scattered crackles in breath sounds.
Impaired Physical Mobility: Evidenced by weak right grip, no left hand grip, flaccid left leg, requiring assistance for ADLs and transfers, CVA history.
Confusion / Impaired Memory: Evidenced by disoriented to time and place, stating "time to go to school," "I don't know this place," requiring constant questions.
Self-Care Deficit (Bathing, Toileting, Eating): Evidenced by requiring assistance with ADLs due to weakness and confusion.
Incontinence (Urine and Stool): Evidenced by being incontinent of urine and stool.
Ineffective Airway Clearance / Respiratory Problems: Evidenced by scattered crackles, coughing, and risk of aspiration from impaired swallowing (potential pneumonia).
Risk for Falls: Due to weakness, impaired mobility, and confusion.
Risk for Impaired Skin Integrity: Due to incontinence of urine and stool.
Priority Problems for the Case Study:
Impaired Swallowing (Dysphagia) / Risk for Aspiration: This addresses physiological needs (nutrition, hydration) and safety (preventing choking/pneumonia). This is the highest priority due to direct threat to airway and life.
Impaired Physical Mobility: Also a physiological need impacting safety and functional independence.
Both are related to the CVA, which caused these muscular and neurological issues.
Diagnostic Statements (Historical Context & Current Understanding):
Traditional Three-Part Statement (less required now, but understand components):
Problem: The nursing diagnosis (e.g., impaired swallowing).
Related To (R/T): The etiology or cause (e.g., decreased strength of muscles involved in mastication and patient paralysis secondary to CVA).
As Evidenced By (AEB): Signs and symptoms (subjective & objective data) that support the problem (e.g., coughing when drinking, pocketing of food, verbal reports of choking).
Current Emphasis: Understand the problem, its cause, and the supporting signs/symptoms, without necessarily formulating the formal three-part sentence.
Example: "Mobility issues and activity intolerance secondary to CVA, evidenced by reports of fatigue and respirations of 28 ext{ breaths/min}".
Risk Diagnoses: Will not have "as evidenced by" statements, as the problem has not yet occurred.
Remaining Nursing Process Steps
3. Planning
Determining what interventions will be done to address the identified problems and achieve the desired outcomes.
4. Implementation
Carrying out the planned nursing interventions.
5. Evaluation
Assessing whether the interventions were effective in achieving the desired outcomes. This is done for every intervention (e.g., pain medication, ambulation). Always go back and evaluate.
Ch17…Nursing Process: Planning/Goal Setting
Explain the relationship of planning to assessment and nursing diagnosis.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
The planning stage follows assessment and nursing diagnosis, where core priorities and the order of problems are established based on the identified nursing diagnoses.
Accurate assessment data (subjective and objective) informs the development of nursing diagnoses, which in turn guides the formulation of specific patient goals and interventions during planning.
Etiologies, which describe the cause of the nursing problem (not the medical diagnosis), are directly related to the nursing diagnosis and form the basis for targeted planning.
Discuss the criteria used in priority setting.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Maslow's hierarchy of needs: Physiological needs (e.g., airway, breathing, circulation) typically take precedence.
Priority frameworks: Use ABCs (Airway, Breathing, Circulation) as a foundational guide; consider urgent versus nonurgent issues; weigh invasive versus noninvasive approaches.
Scope of practice: Prioritize interventions that nurses can perform independently versus those requiring orders or collaboration.
Actual vs. Risk Diagnoses: Actual problems generally take priority over risk diagnoses.
Describe goal/ expected outcome setting.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Goals and Outcomes: Statements that describe the desired changes in patient condition or behavior.
Singular/focused goals: Each goal should target one outcome at a time (e.g., "Patient will cough" rather than combining multiple targets).
SMART = \text{Specific}, \text{Measurable}, \text{Attainable}, \text{Realistic}, \text{Time-based}Time frames for outcomes:
Short-term outcomes: Typically less than or equal to 1 week.
Long-term outcomes: Commonly greater than 1 week (e.g., months) for chronic conditions.
Types of outcomes by domain:
Psychomotor (action-oriented): Patient demonstrates a skill.
Cognitive: Patient understands and can verbalize knowledge (e.g., teach-back).
Affective: Involve coping, attitudes, and feelings.
Physiological: Measurable physiological parameters (e.g., oxygen saturation, weight).
Utilize SMART goals and Outcomes
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording: Outcomes should be SMART (Specific, Measurable, Attainable, Realistic, Time-based
Discuss the differences between nurse-initiated, physician-initiated, and collaborative interventions.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Nurse-initiated interventions: Actions performed by nurses within their scope of practice without physician orders (e.g., turning a patient, providing comfort measures, patient education on self-care).
Physician-initiated interventions: Orders written by the healthcare provider; nurses execute these orders (e.g., medication administration, specific treatments, diagnostic tests).
Collaborative interventions: Interventions requiring multiple disciplines (e.g., physical therapy, occupational therapy, speech-language pathology) to support patient needs such as mobility, self-care, or safety.
Describe the role that communication plays in planning patient-centered care.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Communication is essential to ensure patient and family involvement in planning and decisions, maintaining patient- and family-centered care.
It facilitates the sharing of the care plan with the entire healthcare team (providers, PT/OT, SLP, etc.) to ensure coordinated care.
SBAR (Situation, Background, Assessment, Recommendation) is used for shift handoffs to ensure continuity of care and effective communication of the plan.
Whiteboards and room boards are used to communicate plans and patient goals to staff and family.
Discuss the process of selecting nursing interventions.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Identify evidence-based interventions: Select actions supported by research or best practices.
Address the actual nursing diagnosis/problem first: Prioritize interventions for actual problems over risk diagnoses.
Consider probability of adverse outcomes: Weigh risks vs. benefits of each intervention.
Ensure feasibility and patient capability: Assess for barriers such as pain, transportation, finances, or health literacy.
Individualize care plans: Tailor interventions to patient-specific needs and circumstances, even when using electronic health record (EHR) auto-populated interventions.
Describe the purposes of a written nursing care plan.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording: Establish core priorities and the order of patient problems. Identify specific and measurable expected outcomes for the patient. Select evidence-based nursing interventions to address the problems. Communicate the care plan effectively with the patient, family, and the entire interdisciplinary healthcare team, ensuring continuity and coordination of care. Serve as a legal and clinical record of patient care, outlining what was planned and executed.
Ch18…Nursing Process: Implementing
Explain the relationship of implementation to the nursing diagnostic process.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Implementation is the action phase where the nursing interventions, determined during the planning stage based on identified nursing diagnoses, are carried out.
It directly translates the goals and outcomes derived from the nursing diagnoses into concrete patient care activities, effectively addressing the identified problems.
Describe the association between critical thinking and selecting nursing interventions.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Critical thinking is crucial for selecting appropriate interventions by continuously assessing patient needs, weighing the risks and benefits of potential actions, and evaluating the feasibility of interventions based on patient capabilities and resources.
Nurses must think critically to adapt standardized interventions to individual patient situations, ensuring the most effective and safe care.
Identify preparatory activities to use before implementation.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
the following is an example…Compare MAR to provider orders first: Verify medication details against the physician's orders.
Bedside verification: Verify patient identity and the right medication at the bedside before administration.
In-room administration: Do not remove medication from packaging until in the patient’s room.
Ensure proper equipment and patient environment: Gather all necessary supplies and ensure the environment is safe and conducive to the intervention.
Check for contraindications and potential interactions: Especially important for medications and IVs.
Prepare for unexpected outcomes: Have contingency plans in place.
Discuss steps used to revise a plan of care before performing implementation.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Before full implementation of a care plan, especially standardized ones, it's crucial to individualize it to the patient's specific needs and circumstances.
This involves reviewing the planned interventions in light of the patient's current condition, preferences, and any new assessment data, making modifications as necessary to ensure the plan remains relevant and effective.
Describe and compare direct and indirect nursing interventions.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording: Direct care: Actions performed directly for the patient (e.g., turning a patient, suctioning, performing range of motion exercises, administering medication, performing wound care). Indirect care: Actions performed to support the patient by interacting with the care team or managing the environment (e.g., participating in planning meetings, advocating for patient resources, documenting care, collaborating with other disciplines, ensuring equipment availability).
Select appropriate interventions for an assigned patient.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
When selecting interventions, first address actual nursing diagnoses/problems, which take priority over risk diagnoses.
Consider the probability of adverse outcomes and weigh risks versus benefits.
Assess feasibility and patient capability, looking for barriers such as pain, transportation, finances, or health literacy that might hinder successful implementation.
For a patient with dysphagia (Ms. X), appropriate interventions include: ensuring liquids are thickened, sitting the patient upright (90 degrees) while eating, avoiding straws, using small bites and appropriate pacing, and coordinating with speech-language pathology for swallow studies and specific diet/testing.
Explain why reassessment after a nursing intervention is important.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Reassessment after a nursing intervention is vital for ongoing evaluation, allowing the nurse to compare current patient data to expected outcomes and immediately identify if the intervention has had the desired effect, no effect, or an adverse effect.
This continuous reassessment informs whether the intervention should be continued, modified, or discontinued, ensuring patient safety and the effectiveness of care.
Ch19…Nursing Process: Evaluating
Discuss the relationship between nursing process and evaluation.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Evaluation is the final, continuous step of the nursing process, wherein the effectiveness of the entire plan of care, from assessment to implementation, is critically reviewed.
It closes the loop of the nursing process, determining if patient goals and outcomes established during planning were achieved, thereby informing whether the plan should be terminated, revised, or modified.
Identify the five elements of the evaluation process.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Explain the relationship between goals of care, expected outcomes, and evaluative measures when evaluating nursing care.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Evaluate a set of nursing actions selected for a patient.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Describe how evaluation leads to discontinuation, revision, or modification of a plan of care.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Explain the association between evaluation and quality improvement (QI).
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Discuss how outcomes management assists an organization in improving the quality of care it delivers.
from my personal lecture notes:
from book:
from power point:from Knowt lecture recording:
Nursing Process Overview
Steps: Assessment, Nursing Diagnosis, Planning, Implementation, Evaluation
Clinical Judgment Model: generating solutions, taking action, evaluating
Scope of practice: nurses use orders; nurse-initiated interventions are allowed within scope; physician-initiated vs collaborative interventions involve different authorships
Emphasis on patient- and family-centered care; involve patient and family in planning and decisions
Etiology and Nursing Diagnoses
Distinguish between medical diagnoses and nursing diagnoses; etiology is what causes the nursing problem, not the medical diagnosis itself
Always relate etiologies to nursing diagnosis first; avoid selecting a medical diagnosis as the etiology
Example case discussion: postoperative respiratory risk can be influenced by pain and limited movement, which affect deep breathing and mobility
Illustrative statement: postoperative pain can be an etiology for impaired breathing/mobility, increasing risk for pneumonia if not addressed
Dysphagia case study (Ms. X): etiology described as decreased chewing muscle strength and facial paralysis secondary to CVA (stroke)
Signs/symptoms that support dysphagia: coughing with liquids, pocketing of food, reports of choking
Possible nursing diagnosis choices in the case: impaired mobility, self-care deficit, or risk for impaired skin integrity; etiology should support the chosen problem without naming a medical diagnosis
Etiology framing for case: describe nonmedical factors leading to the nursing problem (e.g., malnutrition, caregiver support, mobility issues) and link back to the problem while avoiding a medical diagnosis label
Data Types in Assessment: Subjective vs Objective
Subjective data: what the patient says (e.g., dizziness, pain description, perception of symptoms)
Objective data: observable/measurable findings (e.g., heart rate, breath sounds, mobility status)
Examples from discussion: heart rate and breath sounds are objective; patient reports of respiratory problems are subjective
A cue to a nursing diagnosis: data that align with a problem (e.g., shortness of breath on walking a few steps may cue an respiratory/functional problem)
Goals, Outcomes, and Prioritization
Singular/focused goals: goals should target one outcome at a time
Example of singular-focused goal: "Patient will cough" (as opposed to combining multiple targets like diet adherence and weight loss)
Other example outcomes discussed: mix of multiple targets (not singular) should be avoided when a single outcome is more precise
Outcomes should be SMART: Specific, Measurable, Attainable, Realistic, Time-based
SMART = ext{Specific}, ext{Measurable}, ext{Attainable}, ext{Realistic}, ext{Time-based}
Time frames for outcomes:
Short-term outcomes: typically <
1 weekLong-term outcomes: commonly > 1 week (e.g., months) for chronic conditions
Types of outcomes by domain:
Psychomotor (action-oriented): patient demonstrates a skill
Cognitive: patient understands and can verbalize knowledge (teach-back)
Affective: coping, attitudes, and feelings
Physiological: measurable physiological parameters (e.g., oxygen saturation, weight)
Example outcome structure (case study):
Short-term: patient will ambulate 30 feet with no shortness of breath by end of shift
Physiological: O2 saturation maintained > 92% during present shift
Functional: patient will perform activities of daily living with supervision or independently as appropriate
Documentation note: each outcome should derive from a specific problem and be evaluable with a time frame
Case Study: Dysphagia (Ms. X)
Problem: impaired swallowing due to CVA (stroke) with associated dysphagia
Etiology: decreased muscle strength for chewing and facial paralysis secondary to CVA
Objective data supporting the case: left facial droop, left leg flaccidity, left hand weakness
Potential nursing diagnoses to consider: impaired mobility, self-care deficit, or risk for impaired skin integrity
Proposed outcome: "Ms. X will swallow liquids freely by Sunday" with evidence: no aspiration, no coughing, no pocketing of food for liquids at meals
Interventions to address dysphagia (examples):
Ensure liquids are thickened as ordered; reduce risk of aspiration
Sit patient upright (90 degrees) while eating
Avoid straws; use appropriate cup to slow flow
Use small bites and appropriate pacing; consider chin-tuck swallow technique as ordered by speech therapy
Coordinate with speech-language pathology for swallow studies and proper diet/testing
Note: ensure rationales support interventions (e.g., thickened liquids reduce aspiration risk; upright seating improves airway protection)
Planning Stage: Purpose and Process
Goals of planning stage:
Establish core priorities and order of problems
Identify expected outcomes that are specific and measurable
Select evidence-based nursing interventions
Communicate the care plan with patient, family, and the healthcare team (providers, PT/OT, SLP, etc.)
How planning works in practice:
Electronic health record (EHR) auto-populates interventions; tailor to patient
Individualize care plans to patient-specific needs and circumstances
Foundation concepts to support planning:
Maslow's hierarchy of needs (physiological needs first)
Priority frameworks: ABCs (Airway, Breathing, Circulation); urgent vs nonurgent; invasive vs noninvasive
Scope of practice: what nurses can do independently vs what requires orders or collaboration
Delegation and collaboration:
Determine what can be delegated and what requires provider orders
Collaboration with physical therapy, occupational therapy, speech therapy, and others to address mobility, self-care, and safety needs
Communication and documentation:
Use SBAR (Situation, Background, Assessment, Recommendation) for handoffs
Document plan and patient progress; ensure plan is visible to all care team
Medication safety and MAR:
Five rights: ext{Patient}, ext{Dose}, ext{Route}, ext{Time}, ext{Documentation}
Compare MAR to provider orders first; bedside verification before administration
Do not pour pills out of packaging until in the room; verify patient identity and right medication
Inpatient pharmacology concerns:
IV meds require careful consideration of drug interactions and potential need for separate IV lines
Always check contraindications and potential interactions before administration
Real-world planning considerations:
Always involve patient and family preferences; respect privacy and comfort levels
Prepare for discharge planning early (e.g., heart failure patients require teaching on daily weights, sodium restriction, medications)
Consider community resources and case management for post-discharge support
Practical example: discharge planning for heart failure
Daily weights to monitor fluid status
Education on medications and low-sodium diet
Arranging follow-up appointments and home support; explore readmission risk and strategies to prevent readmission
Standardized care plans and protocols:
Some conditions have standardized care plans (e.g., total joint replacements; heparin protocols with PTT-based titration; sliding-scale insulin)
Standardized plans must be adapted to the individual patient
Care planning resources:
LivingCare Advisor resources for problem-based care plans with goals and interventions
UpToDate handouts and drug information through library access
The book itself as a resource for rationales and interventions
Medication Safety and Administration Details
Five rights of medication administration: ext{Patient}, ext{Dose}, ext{Route}, ext{Time}, ext{Documentation}
MAR checks:
Always compare MAR to the doctor's order first, then verify with the patient and the medication at the bedside
In-room administration:
Do not remove medication from packaging until you are in the patient’s room
IV medications and interactions:
Be aware of potential drug interactions and separate IV lines if necessary
Documentation and accountability:
If it’s not documented, it wasn’t done
Example incident:
Infiltration risk requiring assessment, warm compresses, elevation, and provider notification if the IV site is compromised
Interventions: What Nurses Do
Types of interventions:
Direct care: actions performed directly for the patient (e.g., turning, suctioning, performing ROM)
Indirect care: actions performed to support the patient by interacting with the care team (e.g., participating in planning meetings, advocating for patient resources)
Physician-initiated vs collaborative interventions:
Physician-initiated: orders written by the provider; nurses execute these orders
Collaborative: interventions requiring multiple disciplines (PT/OT/SLP) to support mobility and safety
Protocols, standing orders, and care bundles:
Stroke protocol: coordinated diagnostic and treatment steps within a time window
Heparin protocol: anticoagulation management with PTT-based titration
Sliding-scale insulin: insulin dosing based on blood glucose levels per order
Considerations when selecting interventions:
Address the actual nursing diagnosis/problem first; actual problems take priority over risk diagnoses
Consider the probability of adverse outcomes and weigh risks vs benefits
Ensure feasibility and patient capability; assess for barriers such as pain, transportation, finances, or health literacy
Documentation in implementation:
Document what you actually did, not just that you did something
Use real-time documentation when possible, but if not feasible, keep contemporaneous notes
Patient safety during interventions:
Ensure proper equipment and patient environment
Check for contraindications and potential interactions (especially with medications and IVs)
Prepare for unexpected outcomes and have contingency plans
Implementation and Communication Tools
SBAR: Situation, Background, Assessment, Recommendation
Shift handoffs and group planning meetings to ensure continuity of care
Use of whiteboards and room boards to communicate plan and patient goals to staff and family
Evaluation of Care: How to Know if Outcomes Are Met
Ongoing evaluation is essential; compare current data to expected outcomes
Types of outcomes to evaluate:
Psychomotor: motor/skill performance
Cognitive: knowledge retention and understanding (teach-back)
Affective: emotional and coping responses
Physiological: vital signs, labs, functional status
Decision rules after evaluation:
If outcomes are met: terminate the plan and discharge or move to a new problem
If partially met: revise the plan, adjust interventions or time frame
If not met: modify the plan and possibly extend time frame
Common evaluation pitfalls:
Inaccurate or outdated data leading to poor problem identification
Vague diagnoses or goals not aligned with the problem
Inadequate or incomplete documentation
Case example for Ms. X (dysphagia):
Outcome: swallow liquids freely by Sunday; evidenced by no aspiration and no coughing; if coughing persists or pocketing occurs, revise goal or extend time frame
Documentation, Communication, and Resources
Documentation is critical for legal and clinical accountability; everything done must be documented
Resources for care planning and evidence-based interventions:
Care plan templates and resources in LivingCare Advisor
UpToDate drug handouts and patient education sheets via library access
Course book as a reference for rationales and intervention ideas
Self-care project expectations:
Include problem, etiology, objective and subjective data, expected outcomes, and three nursing interventions with rationales
Determine whether outcomes were met, partially met, or not met; indicate continuation, modification, or termination of interventions
Practice exam and remediation (ATI):
Practice exams A and B; focused review for missed questions; remediation; then take a quiz
Benchmarks toward NCLEX-style questions; benchmarks vary by level in the handbook
Emphasis on applying knowledge to scenarios, not memorizing definitions
Ethical, Philosophical, and Practical Implications
Ethical considerations:
Respect patient autonomy and involve family when appropriate
Consider cultural differences and ensure care plans are congruent with the patient’s culture and values
Practical implications:
Early discharge planning improves outcomes and reduces readmissions; 30-day readmission penalties affect hospital reimbursement
Daily weights for heart failure patients help detect fluid overload early
Collaboration with social work and case management to address transportation, finances, and access to care
Real-world challenges:
Pressure from staffing and time constraints can affect quality of care; must still document care and adhere to standards
The risk of nonadherence due to education gaps, affordability, or access; address root causes and advocate for patient needs
Quick Reference: Formulas, Thresholds, and Key Lists
Five rights of medication administration:
\text{Patient},\; \text{Dose},\; \text{Route},\; \text{Time},\; \text{Documentation}
Oxygen saturation goal examples:
\text{O}_2 \text{ sat} > 92\% (example threshold mentioned)
SMART goals:
SMART = {Specific,\; Measurable,\; Attainable,\; Realistic,\; Time-based}$$
Short-term vs long-term outcomes:
Short-term: typically less than or equal to 1 week
Long-term: commonly greater than 1 week (e.g., months for chronic conditions)
Example discharge considerations for heart failure:
Daily weights, low-sodium diet, medications, home monitoring, and arranging follow-up care
Final Takeaways
Always connect the nursing diagnosis to nonmedical etiologies and patient-centered goals
Prioritize actual conditions over risks; plan using SMART, singular-focused outcomes
Use a structured planning process that includes patient/family input, evidence-based interventions, and clear communication
Evaluate iteratively, documenting outcomes as met, partially met, or not met, and adjust the plan accordingly
Leverage available resources (care plan templates, UpToDate, ATI practice/remediation) to support evidence-based practice
POWERPOINTS OVER THESE LAST THREE CHAPTERS…