Chapter 30
The Child with Cerebral Dysfunction
1. Describe the composition and function of the central nervous system.
3 functioning part: Central Nervous System (CNS), Peripheral Nervous System (PNS) and the. Autonomic Nervous System (ANS)
2 cerebral hemispheres: brainstem,cerebellum & spinal cord
PNS is composed of the cranial nerves & spinal nerves: efferent/afferent
ANS is composed of the Sympathetic & Parasympathetic system
2. Identify the clinical manifestations of increased intracranial pressure in infants and children.
Clinical Manifestations of Increased Intracranial Pressure in Infants and Children
Infants
Tense, bulging fontanel
Separated cranial sutures
Macewen (cracked-pot) sign
Irritability and restlessness
Drowsiness
Increased sleeping
High-pitched cry
Increased frontooccipital circumference
Distended scalp veins
Poor feeding
Crying when disturbed
Setting-sun sign
Children
Headache
Nausea
Forceful vomiting
Diplopia, blurred vision
Seizures
Indifference, drowsiness
Decline in school performance
Diminished physical activity and motor performance
Increased sleeping
Inability to follow simple commands
Lethargy
Late Signs in Infants and Children
Bradycardia
Decreased motor response to command
Decreased sensory response to painful stimuli
Alterations in pupil size and reactivity
Extension or flexion posturing
Cheyne-Stokes respirations
Papilledema
Decreased consciousness
Coma
3. Discuss the evaluation of the neurologic status in infants and children, including the history and physical examination.
Younger than 2- special evaluation since they cant elicit specific.
Early neurologic responses in infants are primarily reflexive; these responses are gradually replaced by meaningful movement in the characteristic cephalocaudal direction of development.
Most information about infants and small children comes from observation of spontaneous and elicited reflex responses.
Delay or deviation from expected milestones helps identify high-risk children.
Persistence or reappearance of primitive reflexes indicates a pathologic condition.
In evaluating the infant or young child, it is important to obtain the history of the pregnancy, delivery, respiratory status at birth, and neonatal health including any need for intensive care hospitalization to determine the possible impact of intrauterine and extrauterine environmental influences known to affect the orderly maturation of the CNS.
These influences include maternal infections, chemical exposure, trauma, medication, illicit drug use, and metabolic insults.
A review of family members often identifies conditions that might otherwise be overlooked, especially increased number of miscarriages or siblings or relatives who died at an early age.
The nurse asks questions regarding specific neurologic problems, such as intellectual and developmental disabilities, deafness, epilepsy, blindness, unusual movements, weakness, ataxia, stroke, and progressive mental deterioration. History of consanguinity is also important.
A health history provides valuable clues regarding the cause of neurologic dysfunction.
A history is assessed for injury with loss of consciousness, febrile illness, an encounter with an animal or insect, ingestion of neurotoxic substances, inhalation of chemicals, past illness, and known diabetes mellitus or sickle cell disease.
Sudden or progressive alterations in movement or mental abilities may provide clues for investigation.
Physical examination includes observation of the size and shape of the head (particularly in the infant and young child), spontaneous activity and postural reflex activity, and sensory responses.
Note whether the patient is lethargic, drowsy, stuporous, alert, active, or irritable.
The nurse also observes the overall tone, noting whether there is a normal flexed posture or one of extreme extension, opisthotonos, or hypotonia.
Symmetry of movement is also assessed.
Facial features may suggest a specific syndrome.
A high-pitched, piercing cry in an infant is often associated with CNS disorders.
An abnormal respiratory cycle, such as prolonged apnea, ataxic breathing, paradoxic chest movement, and hyperventilation, may be the result of a neurologic problem.
In addition, an estimation of the level of development provides essential information about neurologic function.
Muscular activity and coordination, including ocular movements and gait, are valuable sources of information.
Ocular movements, pupillary response, facial movements, and mouth functions provide clues regarding CNS involvement or impingement.
Testing reflexes, strength, and coordination and for the presence and location of tremors, twitching, tics, or other unusual movements is also an aspect of the neurologic assessment
4. Describe characteristics of altered states of consciousness, unconsciousness, and coma.
A altered state of consciousness usually refers to varying states of unconsciousness that may be momentary or may last for hours, days, or indefinitely.
Unconsciousness is depressed cerebral function—the inability to respond to sensory stimuli and have subjective experiences.
Coma is defined as a state of unconsciousness from which the patient cannot be aroused, even with powerful stimuli.
5. Discuss the assessment of altered states of consciousness using the pediatric Glasgow Coma Scale.
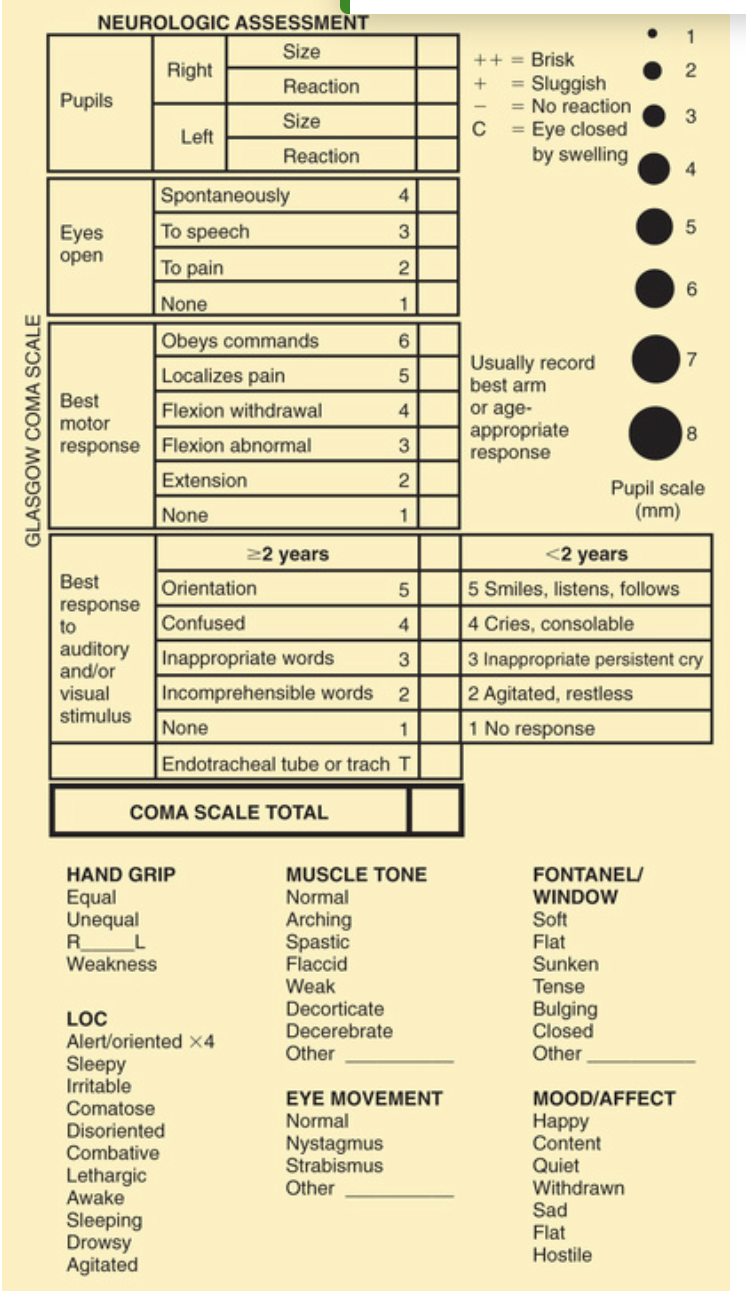
A pediatric version of the GCS recognizes that expected verbal and motor responses must be related to the child's age
The pediatric coma scale does not assess verbal responses as such but records smiling, crying, and interaction
6-point motor scale that is inappropriate for children below the age of 6 months
In children under 5 years of age, speech is understood to be any sound at all, even crying.
Young children demonstrate orientation by identifying their parents correctly or giving their own names.
have parent available cause infant or child may not respond if they are in an unfamiliar environment or hear unfamiliar voices.
Numeric values are assigned to the levels of response in each category.
The sum of these numeric values provides an objective measurement of the patient's LOC.
The lower the score, the deeper the coma.
A person with an unaltered LOC would score the highest 15; a score of 8 or below is generally accepted as a definition of coma.
The lowest score, 3, indicates deep coma or death.
a child with quadriplegia cannot respond to commands physically, the child's GCS can be very low but the child may be cognitively intact.
6. Describe criteria for brain death pronouncement.
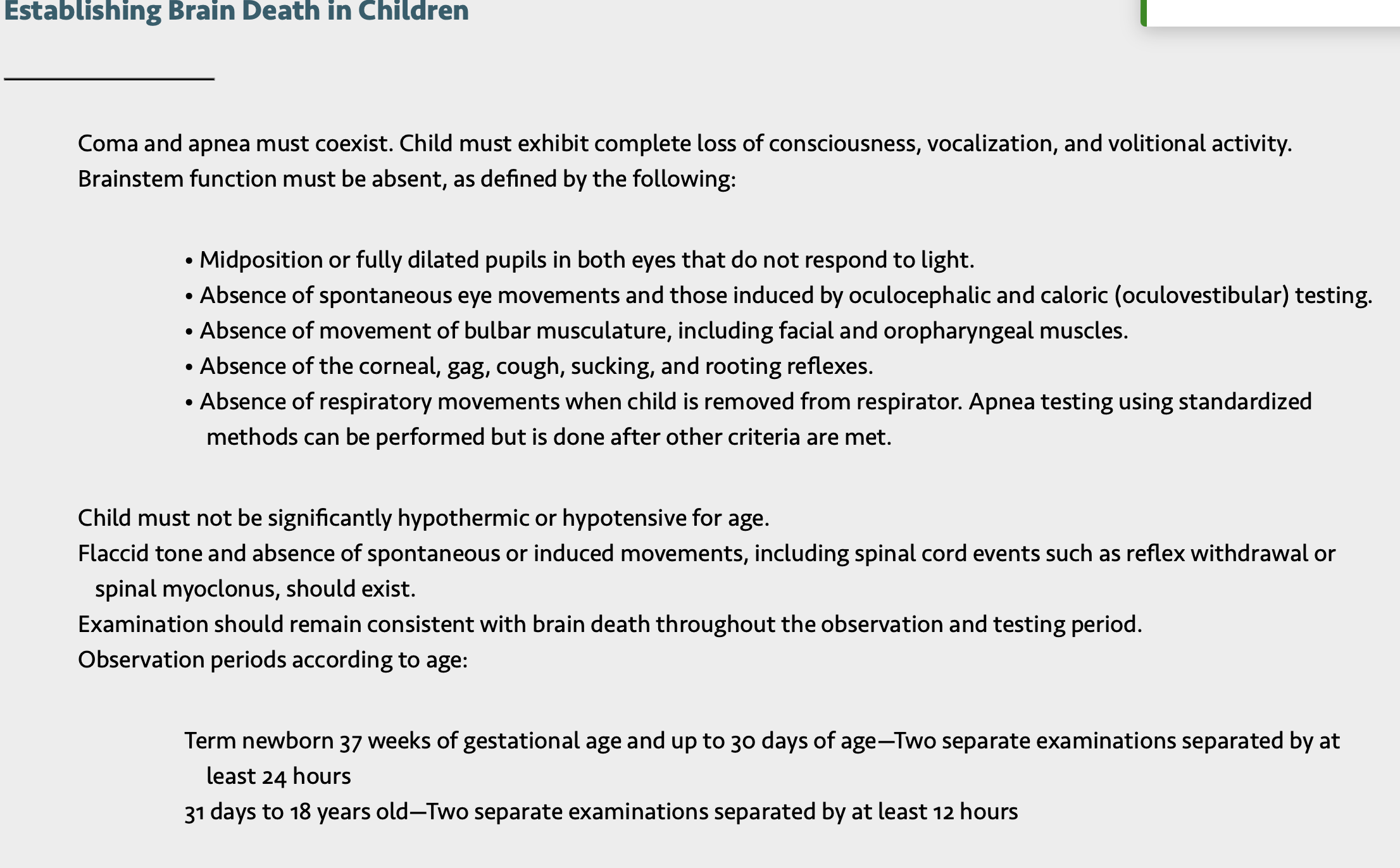
The pronouncement of brain death requires two conditions:
(1) complete cessation of clinical evidence of brain function
(2) irreversibility of the condition.
It is essential to establish the absence of a reversible condition, especially a toxic and metabolic disorder, sedative-hypnotic drugs, paralytic agents, hypothermia, hypotension, and surgically remediable conditions
7. Discuss components of the neurologic examination in infants and children and indications of abnormal findings.
Purpose of the neurologic exam is to esablish an accurate baseline and Trended information
Descriptions behaviors should be objective, simple & easily interpreted
Vital signs: Bp, RR and HR provides info on possible cause of altered consiousness
Autonomic activity: intensively disturbed in deep coma and in brainstem lesions.
Body temperature is often elevated; high temp is sign for infection and heatstroke, meds or bleeding esp subarachnoid hemorrhage. Hypothalamic involvement may cause elevated or decreased temperature. Serious infection may produce hypothermia.
Pulse is variable and may be rapid, slow and bounding, or feeble. Blood pressure may be normal, elevated, or very low. When cushing reflex or pressor response its a late sign of ICP
Respiration are more often slow, deep, and irregular. Slow and deep breathing often occurs in the heavy sleep caused by sedatives, after seizures, or in cerebral infections.
Slow, shallow breathing may result from sedatives or opioids. Hyperventilation (deep and rapid respirations) is usually the result of metabolic acidosis or abnormal) . Periodic or irregular breathing is a sign of brainstem (especially medullary) dysfunction. This is an ominous sign that often precedes complete apnea.
Skin: The body surface should be examined for injury, needle marks, petechiae, bites, and ticks.
Evidence of toxic substances may be found on the hands, face, mouth, and clothing, esp with small children
Eyes
Pupils either do or do not react to light.
Pinpoint pupils are commonly observed in poisoning (e.g., opiate or barbiturate poisoning) or in brainstem dysfunction.
Widely dilated and reactive pupils are often seen after seizures and may involve only one side.
Widely dilated and fixed pupils suggest paralysis of CN III (oculomotor nerve) secondary to pressure from herniation of the brain through the tentorium.
A unilateral fixed pupil usually suggests a lesion on the same side.
Bilateral fixed pupils if present for more than 5 minutes usually imply brainstem damage.
Dilated and nonreactive pupils also occur in hypothermia, anoxia, ischemia, poisoning with atropine-like substances, or prior instillation of mydriatic drugs.
“The sudden appearance of a fixed and dilated pupil is a neurosurgical emergency.”
Blinking observed at rest or in response to a sudden loud noise or bright light implies that the pontine reticular formation is intact.
The corneal reflex, blinking of the eyelids when the cornea is touched with a wisp of cotton, can test the integrity of the ophthalmic division of CN V (trigeminal nerve).
Posttraumatic strabismus indicates CN VI (abducens nerve) damage.
Eye movements are assessed by the doll's head maneuver, in which the child's head is rotated quickly to one side and then to the other.
When the brainstem centers for eye movement are intact, there is conjugate (paired or working together) movement of the eyes in the direction opposite the head rotation.
Absence of this response suggests dysfunction of the brainstem or CN III.
Downward or lateral deviation is often observed in association with pupillary dilation in dysfunction of CN III.
Motor Functioning- observation described instead of labelling
Asymmetric movements of the limbs or the absence of movement suggests paralysis
In hemiplegia the affected limb lies in external rotation and falls uncontrollably when lifted and allowed to drop.
In the deeper comatose states the child has little or no spontaneous movement, and the musculature tends to be flaccid.
There is considerable variability in motor behavior in lesser degrees of coma
Hyperactivity is more common in acute febrile and toxic states than in cases of increased ICP.
Seizures are common in children and may be present in coma as a result of any cause.
Any repetitive movements and movements during seizures are described.
Posturing
Primitive postural reflexes emerge as cortical control over motor function is lost in brain dysfunction.
Posturing reflects a balance between the lower exciting and the higher inhibiting influences.
Strong muscles overcome weaker ones.
Flexion posturing: occurs with severe dysfunction of the cerebral cortex or with lesions to corticospinal tracts above the brainstem.
flexion posturing includes rigid flexion, with arms held tightly to the body; flexed elbows, wrists, and fingers; plantar flexed feet; legs extended and internally rotated; and possibly fine tremors or intense stiffness.
Extension posturing: a sign of dysfunction at the level of the midbrain or lesions to the brainstem. It is characterized by rigid extension and pronation of the arms and legs, flexed wrists and fingers, clenched jaw, extended neck, and possibly an arched back.
Unilateral extension posturing is often caused by tentorial herniation.
Posturing may not be evident when the child is quiet but can usually be elicited by applying painful stimuli such as a blunt object pressed on the base of the nail.
Reflexes
The corneal, pupillary, muscle-stretch, superficial, and plantar reflexes tend to be absent in deep coma.
The state of reflexes is variable in lighter grades of unconsciousness and depends on the underlying pathologic process and the location of the lesion.
The doll's eye reflex maneuver, reflects paralysis of CN III.
The absence of corneal reflexes (CN V) and the presence of a tonic neck reflex are associated with severe brain damage.
The Babinski reflex, in which the lateral portion of the bottom of the foot is stroked and causes the big toe to go up, may be of value if it is found to be present consistently in children older than 1 year.
A positive Babinski reflex is significant in the assessment of pyramidal tract lesions when it is unilateral and associated with other pyramidal signs.
A fluctuating Babinski reflex is often observed after seizures.
8. Describe diagnostic procedures used to assess children for neurologic functioning.
Blood testing: Laboratory tests that may help determine the cause of unconsciousness include blood glucose, urea nitrogen, and electrolyte (pH, sodium, potassium, chloride, calcium, and bicarbonate) tests; clotting studies, hematocrit, and a complete blood count; liver function tests.
Blood cultures: blood cultures if there is fever; and sometimes studies to detect lead or other toxic substances, such as drugs.
Lumbar Puncture (LP) or tap: Lumbar puncture: Spinal needle is inserted between L3 and L4 or L4 and L5 vertebral spaces into subarachnoid space; cerebrospinal fluid (CSF) pressure is measured, and sample is collected for examination.
Purpose: Measures spinal fluid pressure, Obtains CSF for laboratory analysis, Injection of medication
Contraindicated in patients with increased intracranial pressure (ICP) or infected skin over puncture site.
Examination of spinal fluid is carried out when toxic encephalopathy or infection is suspected. Lumbar puncture is delayed if intracranial hemorrhage is suspected, and is contraindicated in the presence of increased ICP because of the potential for brainstem herniation.
Subdural tap: Needle is inserted into anterior fontanel or coronal suture (midline to pupil).
Purpose: Helps rule out subdural effusions and removes CSF to relieve pressure
Place infant in semierect position after subdural tap to minimize leakage from site; prevent child from crying if possible, and check site frequently for evidence of leakage.
Electroencephalogram (EEG): electroencephalogram (EEG) may provide important information. For example, generalized random, slow activity suggests suppressed cortical function, and localized slow activity suggests a space-occupying lesion. A flat tracing is one of the criteria used as evidence of brain death.
EEG records changes in electrical potential of brain. Electrodes are placed at various points to assess electrical function in a particular area. Impulses are recorded by electromagnetic pen or digitally.
Purpose: Detects spikes, or bursts of electrical activity that indicate the potential for seizures. Used to determine brain death
Patient should remain quiet during procedure; may require sedation. Minimize external stimuli during procedure.
Auditory & visual evoked potential tests
Auditory and visual evoked potentials are sometimes used in neurologic evaluation of very young children.
Brainstem auditory evoked potentials are useful for evaluating the continuity of brainstem auditory tracts and are particularly useful for detecting demyelinating disease and neoplasms of the brainstem and for distinguishing between brainstem and cortical lesions.
For example, a normal evoked potential in a comatose patient suggests involvement of the cerebral hemispheres.
CT & MRI
CT: Pinpoint x-ray beam is directed on horizontal or vertical plane to provide series of images that are fed into computer and assembled in image displayed on video screen. CT uses ionizing radiation.
Purpose: Visualizes horizontal and vertical cross section of brain in three planes (axial, coronal, sagittal). Distinguishes density of various intracranial tissues and structures—congenital abnormalities, hemorrhage, tumors, demyelinating and inflammatory processes, calcification
Requires IV access if contrast agent is used. Patient may require sedation.
MRI: MRI produces radiofrequency emissions from elements (e.g., hydrogen, phosphorus), which are converted to visual images by computer.
Purpose: Permits visualization of morphologic feature of target structures Permits tissue discrimination unavailable with many techniques
MRI is noninvasive procedure except when IV contrast agent is used. No exposure to radiation occurs. Patient may require sedation. Parent or attendant can remain in room with child. MRI does not visualize bone detail or calcifications. No metal can be present in scanner.
Nuclear brain scan: Radioisotope is injected intravenously, then counted and recorded after fixed time intervals.Radioisotope accumulates in areas where blood-brain barrier is defective
Purpose: Identifies focal brain lesions (e.g., tumors, abscesses). Positive uptake of material with encephalitis and subdural hematoma. Visualizes CSF pathways
Requires intravenous (IV) access; patient may require sedation. In normal children or noncommunicating hydrocephalus, no retrograde filling of ventricles occurs. Areas of concentrated uptake of material are termed hot spots.
9. Discuss the assessment findings in the unconscious child that indicate the occurrence of syndrome of inappropriate antidiuretic hormone or diabetes insipidus.
reqired nursing attendance with careful observation, recording & evaluation of changes in objective signs. vital functions must be maintained and complications prevented through conscientious and meticulous nursing care.
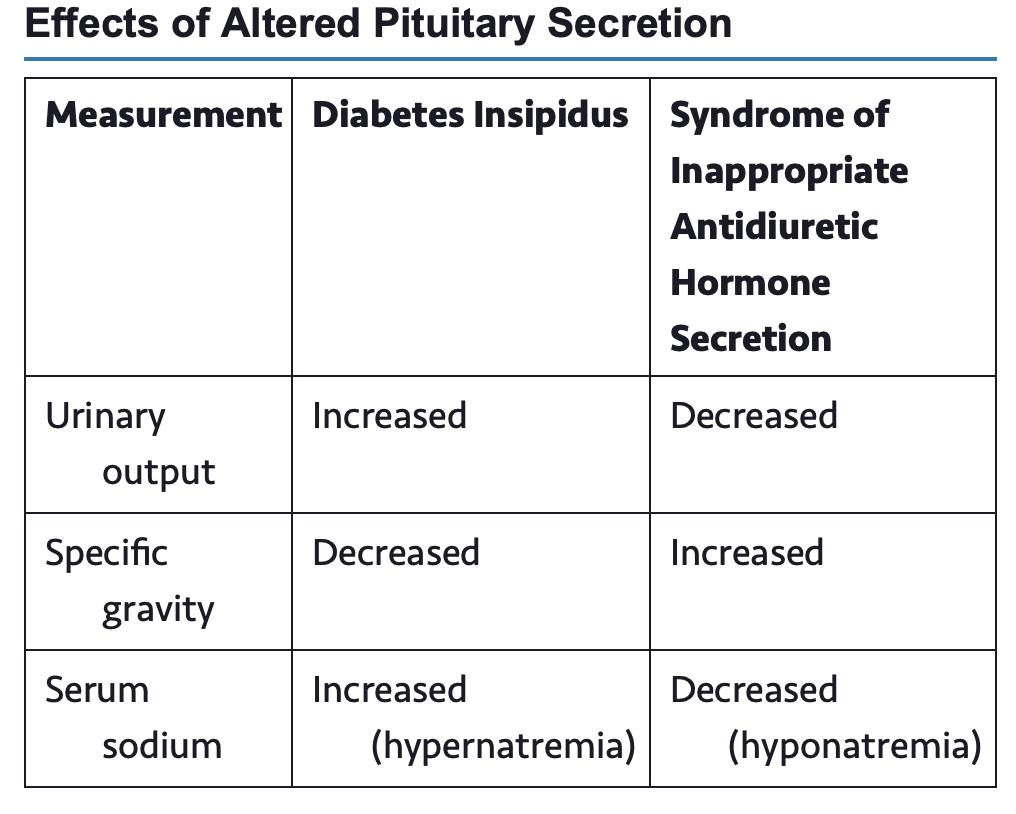
For altered pituitary secretion-SIADH or DI
SIADH often accompanies CNS conditions such as head injury, meningitis, encephalitis, brain abscess, brain tumor, and subarachnoid hemorrhage.
In the child with SIADH, scant quantities of urine are excreted, electrolyte analysis reveals hyponatremia and hypoosmolality, and manifestations of over-hydration are evident.
It is important to evaluate all parameters because the reduced urinary output might be erroneously interpreted as a sign of dehydration.
The treatment of SIADH consists of fluid restriction until serum electrolytes and osmolality return to normal levels.
If fluid restriction is not completely ineffective, medications such as sodium chloride and diuretics may be used.
DI may occur after intracranial trauma. In DI there is increased urinary volume and the accompanying danger of dehydration.
Adequate replacement of fluids is essential, and observation of electrolyte balance is necessary to detect signs of hypernatremia and hyperosmolality.
Exogenous vasopressin may be administered.
Direct measures to ensure patent airway, breathing & circulation
LOC
Stabilization of the spine
Treating shockReducing ICP
Thermoregulation
Pain management
Protection of skin
10. Identify the major causes of brain damage in childhood.
Unintentional injuries are the number one health risk for children and the leading cause of death in children older than 1 year of age.
Children less than 1 year of age though had a significantly higher rate of severe head injury
In 2013 approximately 660,000 children 0 to 14 years old experienced a traumatic brain injury and 17,900 of those children were hospitalized; 1484 children died as a result of their brain injury
The most common causes of head injury in children are falls, being struck by or striking an object with one's head, and motor vehicle accidents, in that order.
Assaults are the leading cause of death from traumatic brain injury in children 4 years of age or younger
Neurologic injury accounts for the highest mortality rate, with boys usually affected twice as often as girls. .
11. Discuss the pathology of brain injury in children.
Directly related to the force of impact.
Intracranial contents (brain, blood, CSF) are damaged because the force is too great to be absorbed by the skull and musculoligamentous support of the head.
nervous tissue is delicate but require severe bloe to cause significant damage
The larger head size in proportion to body size and insufficient musculoskeletal support render the very young child particularly vulnerable to acceleration-deceleration injuries.
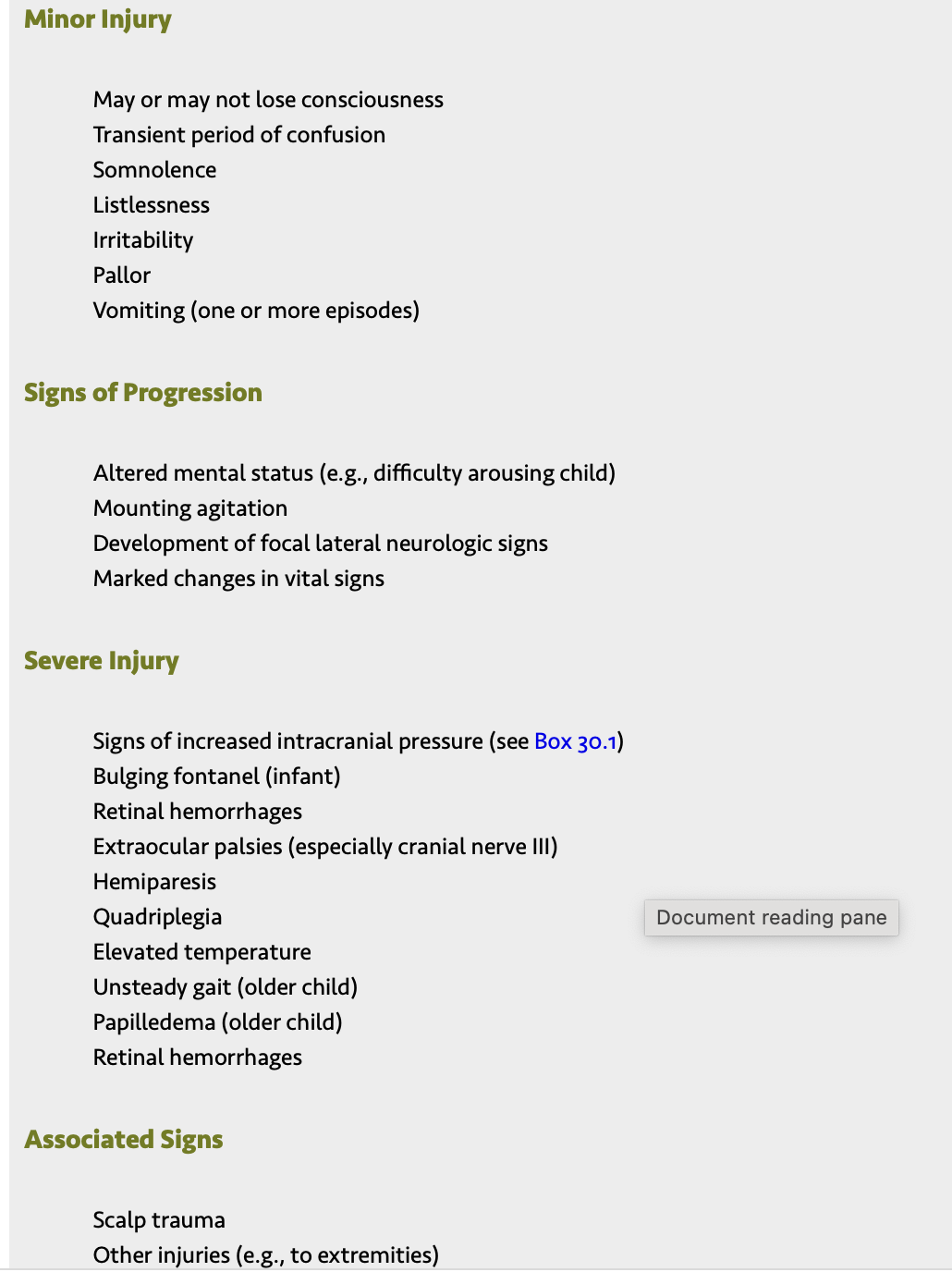
Primary head injuries are those that occur at the time of trauma and include skull fractures, contusions, intracranial hematomas, and diffuse injuries.
Subsequent complications include hypoxic brain injury, increased ICP, and cerebral edema.
The predominant feature of a child's brain injury is the diffuse amount of swelling that occurs. Hypoxia and hypercapnia threaten the energy requirements of the brain and increase CBF.
The added volume across the BBB along with the loss of autoregulation exacerbates cerebral edema.
Pressure inside the skull that is greater than arterial pressure results in inadequate perfusion.
Since the cranium of very young children has the ability to expand and the thin skull is more compliant, they may tolerate increases in ICP better than older children and adults.
Acceleration or deceleration is more descriptive of the circumstances responsible for most head injuries.
sudden acceleration causes deformation of the skull and mass movement of the brain.
This deformation can cause bruising at the point of impact (coup) or at a distance as the brain collides with the unyielding surfaces opposite or far removed from the point of impact (contrecoup)
When a moving head strikes a stationary surface, such as during a fall, sudden deceleration occurs and causes the greatest cerebral injury at the point of impact.
Deceleration is responsible for most severe brainstem injuries.
Children with an acceleration-deceleration injury demonstrate diffuse generalized cerebral swelling produced by increased blood volume or by a redistribution of cerebral blood volume (cerebral hyperemia) rather than by the increased water content (edema).
A shearing force may tear small arteries that travel from the cerebral surfaces through the meninges to the dural sinuses and cause subdural hemorrhages.
12. Discuss the major complications of head trauma.
The major complications of trauma to the head are hemorrhage, infection, edema, and herniation through the brainstem.
Infection is always a hazard in open injuries.
Edema is related to tissue trauma.
Vascular rupture may occur even in minor head injuries, causing hemorrhage between the skull and cerebral surfaces.
Compression of the underlying brain produces effects that can be rapidly fatal or insidiously progressive.
13. Describe signs and symptoms of cerebral edema and postconcussion syndrome.
Cerebral edema
Cerebral edema peaks at 24 to 72 hours after injury
2 mechanism: Cytotoxic edema is a result of direct cell injury
is caused by intracellular swelling.
In many cases the brain cells are irreversibly damaged.
Vasogenic edema is due to increased permeability of capillary endothelial cells.
Results in increased intracellular fluid.
In vasogenic edema the nerve cells are not primarily injured.
Either mechanism can result in increased ICP as a result of increased intracranial volume and changes in CBF as a result of loss of autoregulation and/or hypercapnia or hypoxia.
Children at risk for deterioration can be identified by abnormalities seen on noncontrast CT scans.
Postconcussion syndrome: is a sequela to brain injury with or without loss of consciousness.
It is a symptom complex that includes at least three of the following symptoms: headaches, dizziness, light sensitivity, fatigue, nausea, irritability, restlessness, difficulty concentrating, and memory impairment, change in sleep partern.
The symptoms develop within days of the injury and resolve within 3 months.
14. Describe clinical manifestations of acute head injury.
Primary head injury involves features that occur at the time of trauma, including fractured skull, contusions, intracranial hematoma, and diffuse injury.
Secondary complications include hypoxic brain damage, increased ICP, infection, cerebral edema, and posttraumatic syndromes.
Young children’s response to head injury is different from the response of older children and adults because of the following features: larger head size; expandable skull; larger blood volume to the brain; small subdural spaces; and thinner, softer brain tissue.
15. Discuss the nursing care management of a child with a head injury and the child’s family.
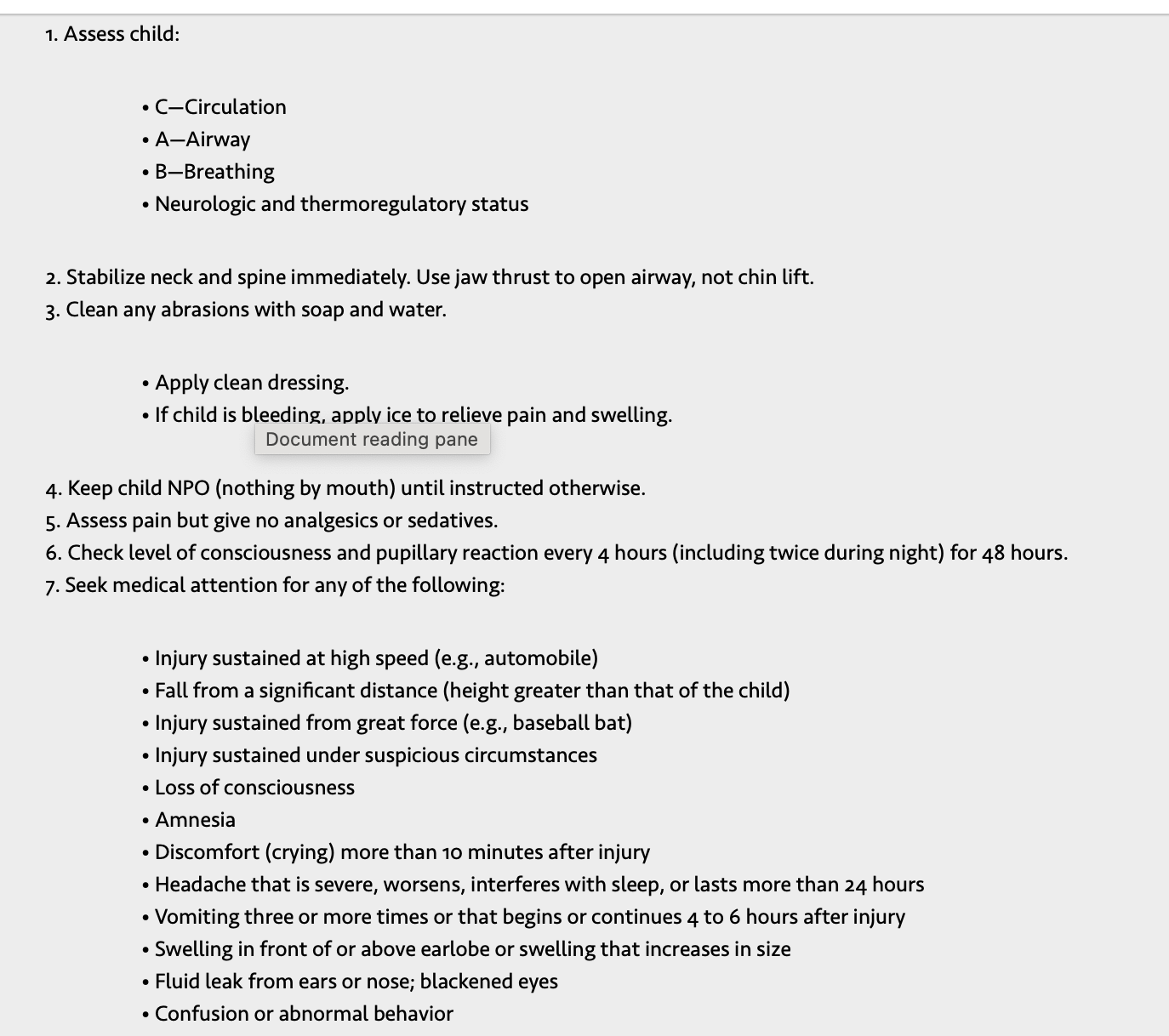
The majority of children with mild TBI who have not lost consciousness can be cared for and observed at home after careful examination reveals no serious intracranial injury.
The nurse should give parents both verbal and written instructions of signs and symptoms that warrant concern and the need for reevaluation.
These include persistent or worsening headaches, vomiting, change in mental status or behavior, unsteady gait, or seizure.
The child should have a physical examination in 1 or 2 days after the injury.
The manifestations of epidural hematoma in children do not generally appear until 24 hours or more after injury.
Maintaining contact with parents for continued observation and reevaluation of the child, when indicated, facilitates early diagnosis and treatment of possible complications from head injury, such as hematoma, cerebral edema, and posttraumatic seizures.
Children are generally hospitalized for 24 to 48 hours of observation if their family lives far from medical facilities or lacks transportation or a telephone, which would provide access to immediate help.
Other circumstances, such as language or other communication barriers or even emotional trauma, may hinder learning and make it difficult for families to feel confident caring for their child at home.
Nursing care management:
The hospitalized child requires careful neurologic assessment
frequently assessment done every 15 minutes to establish a correct diagnosis
identify signs and symptoms of increased ICP
determine clinical management and prevent many complications.
The goals of nursing management of the child with a head injury are to maintain adequate ventilation, oxygenation, and circulation; to monitor and treat increased ICP; to minimize cerebral oxygen requirements; and to support the child and family during recovery.
child is placed on bed rest
HOB slightly elevated in midline position
side rails up, seizure precaution
if child is restless, hard surfaces may be padded and restraints used to prevent further injury. Individualize care according to the child's specific needs.
Key nursing role: provide sedation and analgesia for the child.
A quiet environment can help reduce restlessness and irritability.
Bright lights are irritating.
This often makes checking the ocular responses more difficult and aggravating to the child
Frequent examinations of vital signs, neurologic signs, and LOC are extremely important nursing observations.
Pupils are checked for size, symmetry, reaction to light, and accommodation.
Unless there is brainstem involvement, vital signs generally return to normal after the initial changes seen after injury.
most important nursing observation is assessment of the child's LOC.
alterations in consciousness appear earlier than alterations of vital signs or focal neurologic signs.
The child who is too young to describe a headache may be fussy and resist being handled.
The child who suffers from vertigo often vigorously resists being moved from a position of comfort.
Forcible movement causes the child to vomit and display spontaneous nystagmus.
Seizures are relatively common in children at the time of head injury and may be of any type. children in postictal phase are lethargic, with slugish pupils.
16. Discuss the pathophysiology of submersion injury.
most organ systems are affected, especially the pulmonary, cardiovascular, and neurologic systems.
The major pulmonary changes that occur in submersion injury are directly related to the length of submersion.
Cerebral hypoxia is a major component of morbidity and mortality in these individuals. Therefore early and aggressive resuscitation is imperative.
Physiologic factors in submersion injuries are hypothermia, aspiration, and hypoxia. The temperature of the liquid plays an important role.
Hypothermia occurs rapidly in infants and children, partly because of their large surface area relative to size and partly as a result of the cold water itself.
Profound hypothermia is usually evidence of lengthy submersion.
Submerged children struggle initially to stay above water, and often breath-holding leads to air hunger.
Reflex inspiration eventually occurs, which leads to aspiration
Fluid is quickly absorbed in the pulmonary circulation, resulting in pulmonary edema, atelectasis, and airway spasm.
Hypoxia is the primary problem because it results in global cell damage, with different cells tolerating variable lengths of anoxia.
Neurons, especially cerebral cells, sustain irreversible damage after 4 to 6 minutes of submersion.
is a major cause of unintentional injury-related death in children ages 1 to 19 years.
The term submersion injury is no longer used; instead, the term submersion injury should be used up until the time of drowning-related death.
Submersion injury can take place in any body of water, and potential sites of drowning are important to consider for preventative education.
All children who have a submersion injury should be admitted to the hospital for observation.
Although many patients do not appear to have sustained adverse effects from the event, complications (e.g., respiratory compromise, cerebral edema) may occur 24 hr after the incident.
17. Identify the primary causes of meningitis in children of varying ages.
Meningitis can be caused by a variety of organisms, but the three main types are
(1) bacterial, or pyogenic, caused by pus-forming bacteria, especially meningococci and pneumococci,
(2) viral, or aseptic, caused by a wide variety of viral agents.
(3) tuberculous, caused by the tuberculin bacillus.
The majority of children with acute febrile encephalopathy have either bacterial meningitis or viral meningitis as the underlying cause.
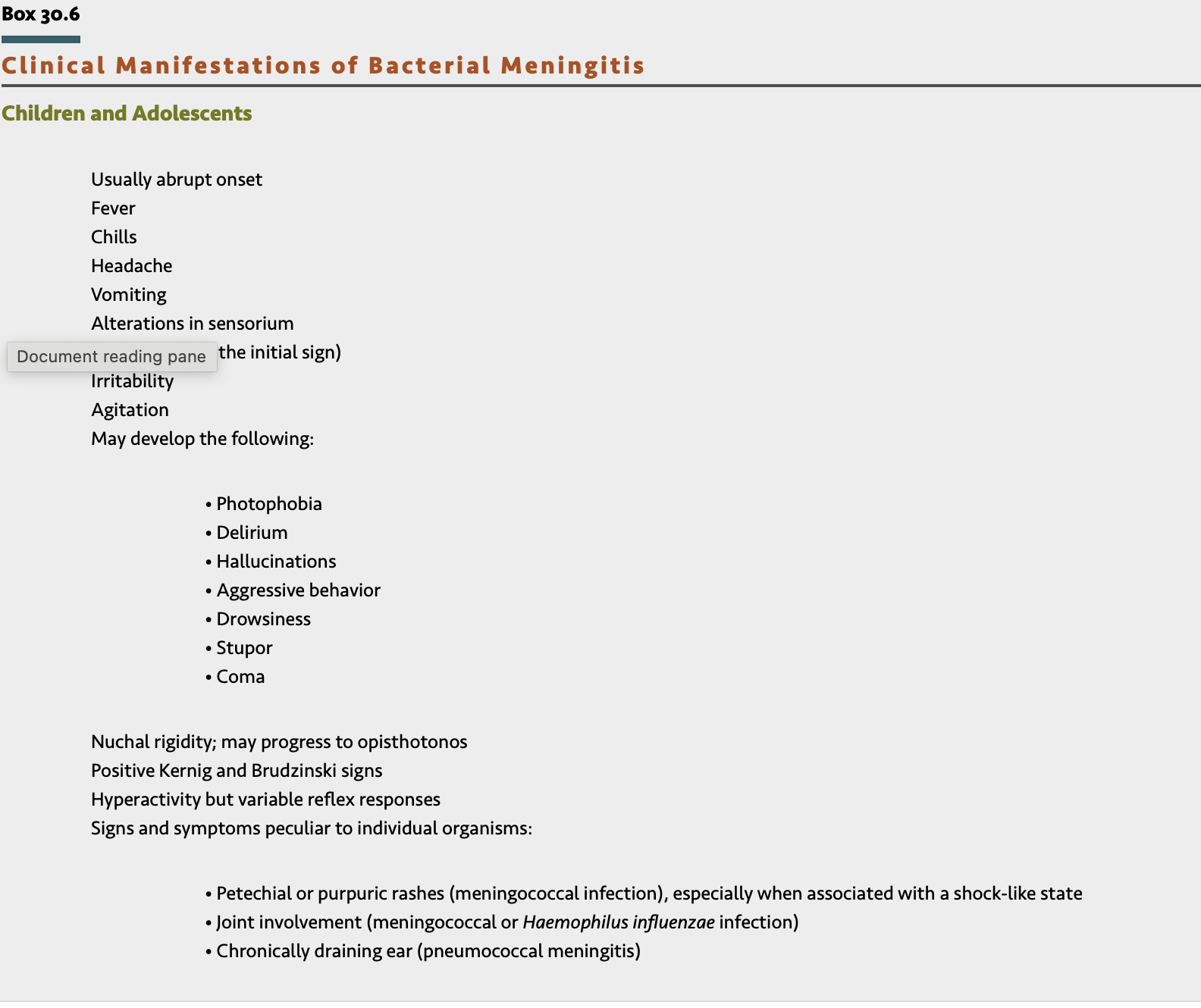
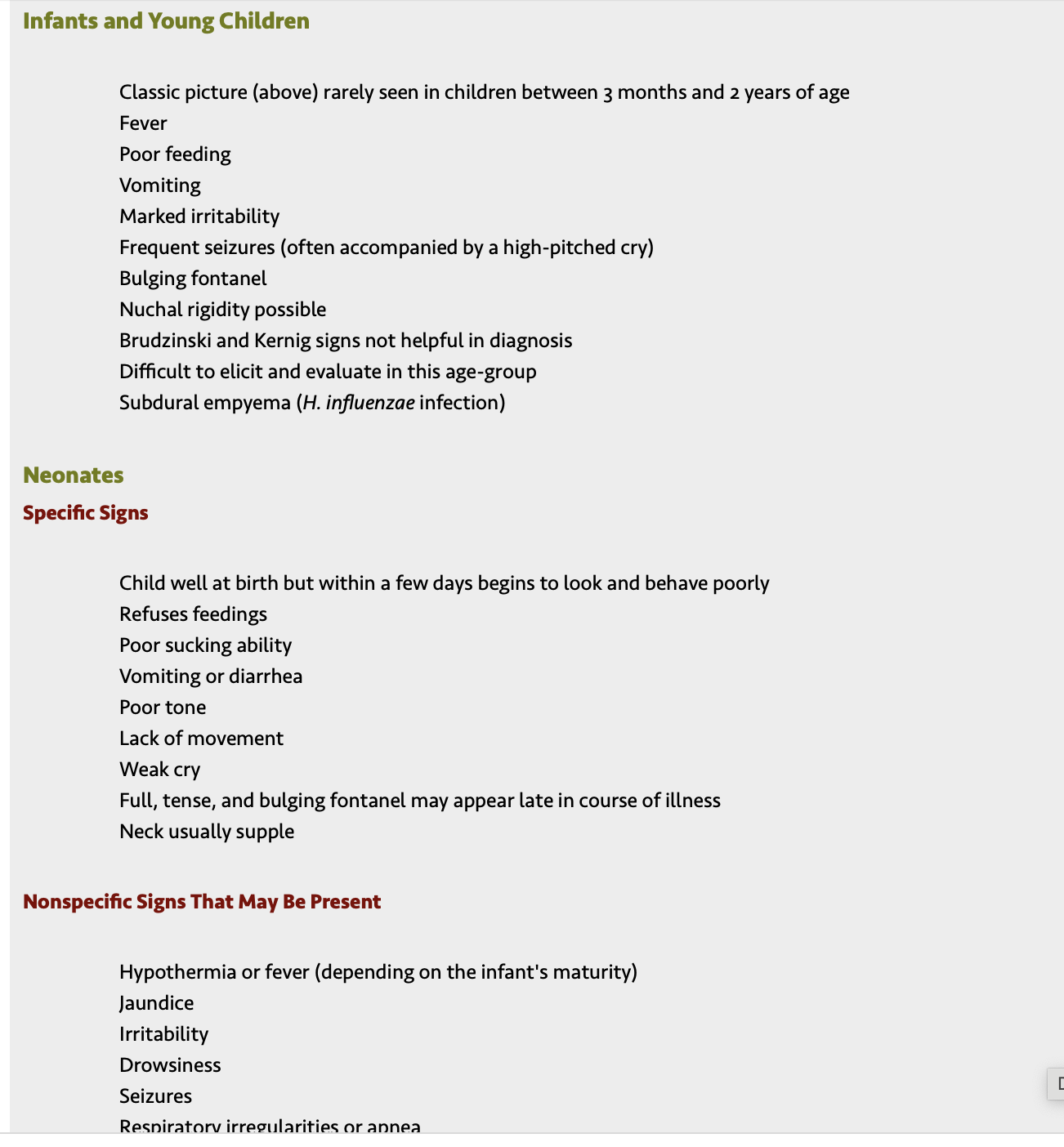
18. Describe the pathophysiology, clinical manifestations, diagnostic evaluation, and complications of bacterial meningitis in children.
Bacterial meningistis is an acute inflammation of the meninges and cerebrospinal fluid.
Acute bacterial meningitis is a medical emergency that requires early recognition and immediate therapy to prevent death and avoid residual disabilities.
The leading causes of neonatal meningitis are group B streptococcus (GBS) and Escherichia coli
Meningitis caused by pneumococcal and meningococcal infections can occur at any time but is more common in late winter and early spring.
The most common route of infection is vascular dissemination from a focus of infection elsewhere.
The infective process is like that seen in any bacterial infection: inflammation, exudation, white blood cell accumulation, and varying degrees of tissue damage.
The brain becomes hyperemic and edematous, and the entire surface of the brain is covered by a layer of purulent exudate that varies with the type of organism
The child is isolated from other children, usually in an intensive care unit for close observation.
An intravenous (IV) infusion is started to facilitate administration of antimicrobial agents, fluids, antiepileptic drugs, and blood, if needed.
The child is placed in respiratory isolation.
Diagnostic Evaluation
Lumbar puncture is the definitive diagnostic test
The patient generally has an elevated white blood cell count, often predominantly polymorphonuclear leukocytes. The glucose level is reduced, generally in proportion to the duration and severity of the infection
Blood culture is advisable for all children suspected of having meningitis if antibiotics are started before obtaining CSF.
Complications
acute bacterial meningitis
obstructive hydrocephalus
Subdural effusions
Thrombosis
Destructive changes may take place in the cerebral cortex
brain abscesses may form by direct extension of the infection or by vascular dissemination
compression necrosis from increased pressure may cause deafness, blindness, or weakness or paralysis of facial or other muscles of the head and neck.
Adverse complication: meningococcal sepsis, or meningococcemia.
severe, sudden, and rapid, it is known as the Waterhouse-Friderichsen syndrome.
characterized by overwhelming septic shock, disseminated intravascular coagulation, massive bilateral adrenal hemorrhage, and purpura
Meningococcemia requires immediate emergency treatment, hospitalization, and intensive care because of the serious sequelae that can quickly develop
SIADH
subdural effusions, seizures, cerebral edema and herniation, and hydrocephalus. Obstruction to the flow of CSF occurs during the acute phase of illness by clumping of purulent material in the drainage channels and during the chronic phase by adhesive arachnoiditis or fibrotic obstruction through any of the ventricular foramina. Postmeningitic complications in neonates include ventriculitis, which results in cystic, walled-off areas of the brain with fluid accumulation and pressure.
Extension of the inflammation to cranial nerves or compression and destruction of the nerves from ICP can produce permanent impairment of vision or hearing and other nerve palsies.
CN VIII damage is usually followed by permanent deafness, the most common permanent neurologic sequela of bacterial meningitis
long-term complications include cerebral palsy, cognitive impairments, learning disorders, attention-deficit/hyperactivity disorder, and seizures.
Hemiparesis and quadriparesis may result from damage caused by arteritis or thrombosis or other mechanisms.
Behavioral changes occur in some children.
Evidence indicates that psychometric and behavioral defects may be a significant concomitant sign of meningitis in childhood
19. Discuss nonbacterial (aseptic) and tuberculous meningitis and the characteristics that distinguish these conditions from bacterial meningitis.
Nonbacterial- Aseptic Meningitis: term aseptic meningitis refers to the onset of meningeal symptoms, fever, and pleocytosis without bacterial growth from CSF cultures.
Many different viruses cause aseptic meningitis; Aseptic meningitis is caused by many different viruses, including arbovirus, enterovirus, herpes simplex virus, cytomegalovirus, and human immunodeficiency virus.
Enterovirus is the most common
The onset may be abrupt or gradual.
The initial manifestations are headache, fever, photophobia, and nuchal rigidity.
Diagnosis is based on clinical features and cerebral spinal fluid findings.
Treatment is primarily symptomatic
Tuberculous Meningitis: considered in children who have traveled or lived in, live with, or are immigrants from developing countries.
Tuberculous is more likely to be disseminated (including CNS involvement) in very young or immunosuppressed children.
Ischemic infarction can occur with tuberculous meningitis.
The most common clinical findings are meningeal signs, fever, altered consciousness, cranial nerve involvement, seizures, and focal neurologic deficit.
Early diagnosis of tuberculous meningitis in the child can significantly reduce the disability caused by hydrocephalus
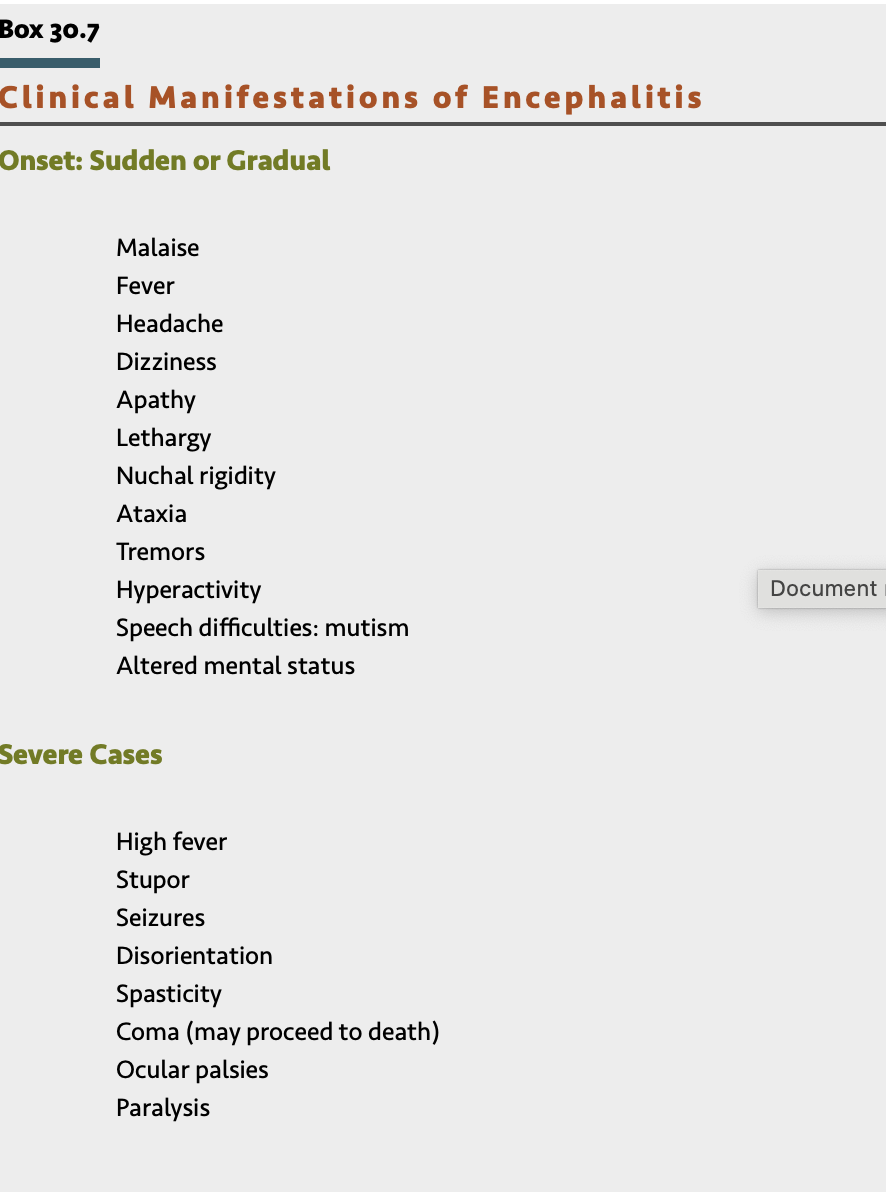
20. Describe the etiology, clinical manifestations, and therapeutic management of encephalitis.
is an inflammatory process of the CNS that is caused by a variety of organisms, including bacteria, spirochetes, fungi, protozoa, helminths, and viruses.
Most infections are associated with viruses and may result from direct invasion of the CNS by a virus or from involvement of the CNS after viral disease.
Patients suspected of having encephalitis are hospitalized promptly for observation, including ICP monitoring.
Treatment is primarily supportive and includes conscientious nursing care, control of cerebral manifestations, and adequate nutrition and hydration, with observations and management as for other cerebral disorders.
21. Describe the etiology, clinical manifestations, and therapeutic management of rabies and Reye syndrome.
Reyes Syndrome (RS) is a disorder defined as a metabolic encephalopathy associated with other organ involvement.
It is characterized by fever, profoundly impaired consciousness, and disordered hepatic function.
RS is a condition characterized pathologically by cerebral edema and fatty changes of the liver.
The onset of RS is notable for profuse effortless vomiting and lethargy that quickly progresses to neurologic impairment, including delirium, seizures, and coma, and can ultimately lead to increased ICP, herniation, and death.
Elevated serum ammonia levels tend to correlate with the clinical manifestations and prognosis.
The most important aspects of successful management of a child with RS are early diagnosis and aggressive therapy.
Definitive diagnosis is established by liver biopsy.
Cerebral edema with increased ICP represents the most immediate threat to life.
Recovery from RS is rapid and usually without sequelae if the diagnosis was made and therapy implemented early.
The potential association between aspirin therapy for the treatment of fever in children with varicella or influenza and the development of RS precludes its use in these patients.
Rabies : Rabies is an acute infection of the nervous system caused by a virus that is almost invariably fatal if left untreated.
It is transmitted to humans by the saliva of an infected mammal introduced through a bite or skin abrasion.
After entry into a new host, the virus multiplies in muscle cells and is spread through neural pathways without stimulating a protective host immune response.
The incubation period usually ranges from 1 to 3 months but may be as short as 5 days or longer than 6 months
(CM): The disease is characterized by a period of nonspecific flulike symptoms, including general malaise, anorexia, fever, and sore throat, followed by a phase of excitement that features hypersensitivity and increased reaction to external stimuli, seizures, hallucinations, hypersalivation, and choking. Severe Spams of respiratory muscles: Apnea, cyanosis and anoxia.
Hydrophobia is a cardinal sign of rabies.
The diagnosis is confirmed by skin biopsy.
Antibodies maybe detected 7 to 8 days after the onset of clinical symptoms.
Therapeutic management: Two types of immunizing products are available for use in humans:
(1) the inactivated rabies vaccines, which induce an active immune response, and
(2) the globulins, which contain preformed antibodies.
The current therapy for a rabid animal bite consists of three steps:
(1) thorough cleansing of the wound with soap and water (suturing should be avoided whenever possible)
(2) administration of rabies vaccine
(3) administration of rabies immunoglobulin
4 dose administered IM at days 0, 3, 7, and 14.
10-day observation period or is proved to be negative for rabies by a reliable laboratory
Rabies immunoglobulin- administered directly on the wound.
Rabies immunoglobulin is given once within 7 days after the first vaccine dose before the child develops an active immune response
22. Define epilepsy and discuss the etiology of acute and chronic seizures in children.
Epilepsy is a condition characterized by two or more unprovoked seizures and can be caused by a variety of pathologic processes in the brain.
Epilepsy is a disease of the brain defined by the following conditions: (1) at least two unprovoked seizures occurring more than 24 hours apart
(2) one unprovoked seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures occurring over the next 10 years”
Seizures are a symptom of an underlying disease process.
A single seizure event should not be classified as epilepsy and is generally not treated with long-term antiepileptic drugs.
23. Discuss the pathophysiology of seizures.
Seizures are caused by excessive and disorderly neuronal discharges in the brain.
The manifestation of seizures depends on the region of the brain in which they originate and may include unconsciousness or altered consciousness; involuntary movements; and changes in perception, behaviors, sensations, and posture.
Regardless of the etiologic factor or type of seizure, the basic mechanism is the same.
Abnormal electrical discharges
(1) may arise from central areas in the brain that affect consciousness
(2) may be restricted to one area of the cerebral cortex, producing manifestations characteristic of that particular anatomic focus.
(3) may begin in a localized area of the cortex and spread to other portions of the brain; if sufficiently extensive, this produces generalized seizure activity
occurs when there is sudden excessive excitation and loss of inhibition within neuronal circuits, allowing the circuits to amplify their discharges simultaneously.
These discharges occur in response to the activity of sodium, potassium, calcium, and chloride ion channels.
Primary generalized seizures begin with abnormal discharges in both hemispheres, which can involve connections between the thalamus and neocortex.
seizures are designated as focal, generalized, and unclassified epileptic seizures.
24. Describe how seizures are classified and identify characteristics of each type.
Partial Seizures
Simple Partial Seizures With Motor Signs
Characterized by the following:
• Localized motor symptoms
• Somatosensory, psychic, autonomic symptoms
• Abnormal discharges remaining unilateral
Manifestations
• Aversive seizure (most common motor seizure in children)—Eye or eyes and head turn away from the side of the focus; awareness of movement or loss of consciousness
• Rolandic (Sylvan) seizure—Tonic-clonic movements involving the face, salivation, arrested speech; most common during sleep
• Jacksonian march (rare in children)—Orderly, sequential progression of clonic movements beginning in a foot, hand, or face and moving, or “marching,” to adjacent body parts
Focal Seizures With Impaired Awareness
Observed more often in children from 3 years through adolescence
Characterized by the following:
• Period of altered behavior
• Amnesia for event (no recollection of behavior)
• Inability to respond to environment
• Impaired consciousness during event
• Drowsiness or sleep usually following seizure
• Confusion and amnesia possibly prolonged
• Complex sensory phenomena (aura)—(e.g., déjà vu, a feeling of familiarity in a strange environment), fear and anxiety
Patterns of motor behavior:
• Stereotypic
• Similar with each subsequent seizure
• May suddenly cease activity, appear dazed, stare into space, become confused and apathetic, and become limp or stiff or display some form of posturing
• May be confused
May perform purposeless, complicated activities in a repetitive manner (automatisms), followed by postictal confusion or sleep; may exhibit oropharyngeal activities followed by stiffness, a fall, and postictal sleep; rarely manifests actions such as rage or temper tantrums; aggressive acts uncommon during seizure
Generalized Seizures
Tonic-Clonic Seizures (Formerly Known as Grand Mal)
Most common and most dramatic of all seizure manifestations
Occur without warning
Tonic phase lasts approximately 10 to 20 seconds
Manifestations:
• Eyes roll upward
• Immediate loss of consciousness
• If standing, falls to floor or ground
• Stiffens in generalized, symmetric tonic contraction of entire body musculature
• Arms usually flexed
• Legs, head, and neck extended
• May utter a peculiar piercing cry
Apneic, may become cyanotic
Increased salivation and loss of swallowing reflex
Clonic phase: lasts about 30 seconds but can vary from only a few seconds to a half-hour or longer
Manifestations:
• Violent jerking movements as the trunk and extremities undergo rhythmic contraction and relaxation
• May foam at the mouth
• May be incontinent of urine and feces
As event ends, movements less intense, occurring at longer intervals, then ceasing entirely
Status epilepticus—Series of seizures at intervals too brief to allow the child to regain consciousness between the time one event ends and the next begins
• Requires emergency intervention
• Can lead to exhaustion, respiratory failure, and death
Postictal state:
• Appears to relax
• May remain semiconscious and difficult to arouse
• May awaken in a few minutes
• Remains confused for several hours
• Poor coordination
• Mild impairment of fine motor movements
• May have visual and speech difficulties
• May vomit or complain of severe headache
• When left alone, usually sleeps for several hours
• On awakening is fully conscious
• Usually feels tired and complains of sore muscles and headache
• No recollection of entire event
Absence Seizures (Formerly Called Petit Mal)
Characterized by the following:
• Onset usually between 4 and 12 years of age
• More common in girls than in boys
• Usually cease at puberty
• Brief loss of consciousness
• Minimum or no alteration in muscle tone
• May go unrecognized because of little change in child's behavior
• Abrupt onset; suddenly develops 20 or more attacks daily
• Event often mistaken for inattentiveness or daydreaming
• Events possibly precipitated by hyperventilation, hypoglycemia, stresses (emotional and physiologic), fatigue, or sleeplessness
Manifestations:
• Brief loss of consciousness
• Appear without warning or aura
• Usually last about 5 to 10 seconds
• Slight loss of muscle tone may cause child to drop objects
• Ability to maintain postural control; seldom falls
• Minor movements such as lip smacking, twitching of eyelids or face, or slight hand movements
• Not accompanied by incontinence
• Amnesia for episode
• May need to reorient self to previous activity
Atonic and Akinetic Seizures (Also Known as Drop Attacks)
Characterized by the following:
• Onset usually between 2 and 5 years of age
• Sudden, momentary loss of muscle tone and postural control
• Events recurring frequently during the day, particularly in the morning hours and shortly after awakening
Manifestations:
• Loss of tone causing child to fall to the floor violently; unable to break fall by putting out hand; may incur a serious injury to the face, head, or shoulder
Loss of consciousness only momentary
Myoclonic Seizures
May be isolated as benign essential myoclonus
Characterized by the following:
• Sudden, brief contractures of a muscle or group of muscles
• Occur singly or repetitively
• No postictal state
• May or may not be symmetric
• May or may not include loss of consciousness
25. Discuss the primary treatment options for seizures, including drug therapy, ketogenic diet, vagus nerve stimulation, and surgery.
Management of epilepsy has four treatment options: drug therapy, the ketogenic diet, vagus nerve stimulation, and epilepsy surgery.
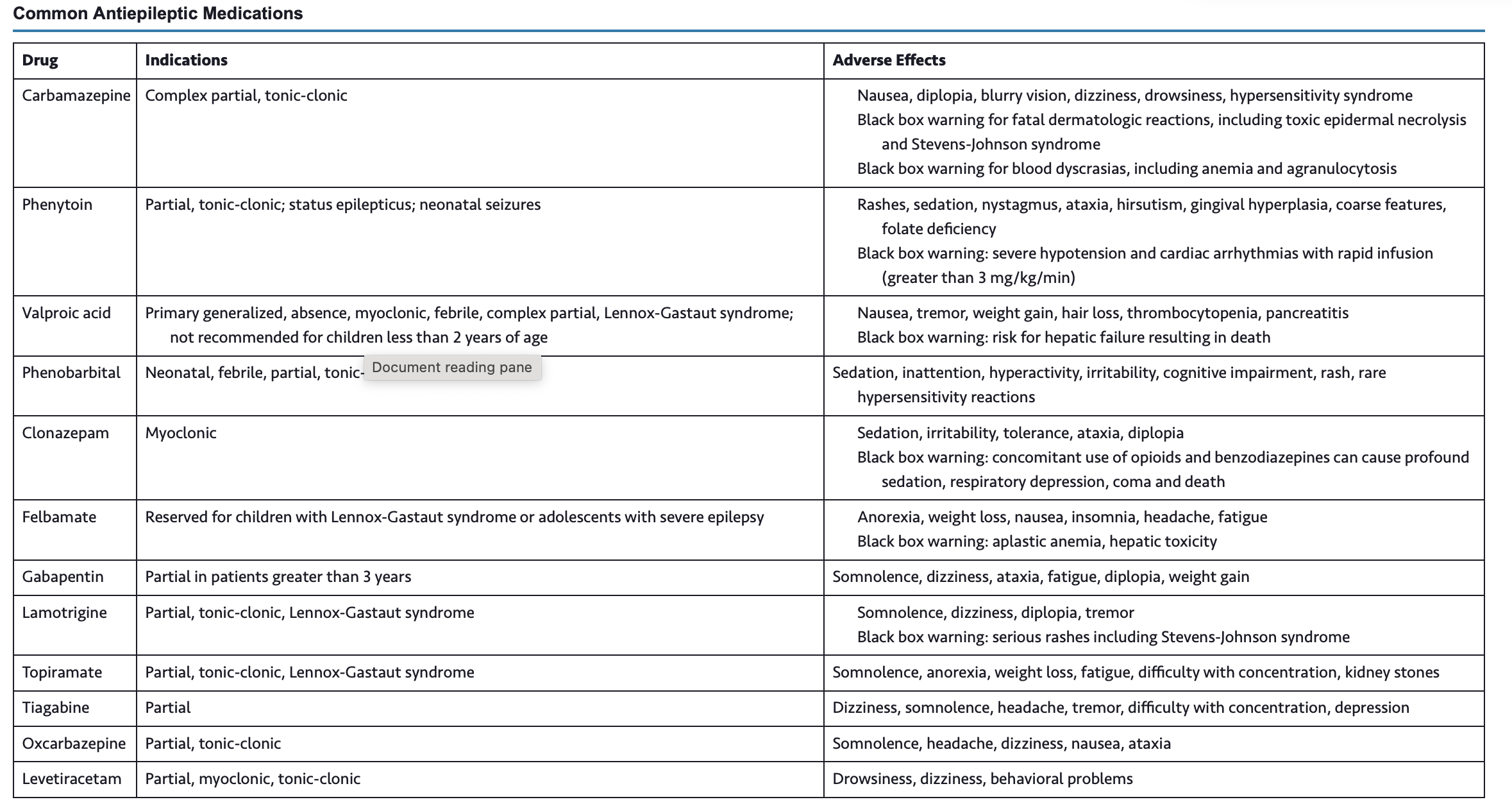
Drug therapy: The initiation of anticonvulsant therapy is based on several factors, including the child's age, type of seizure, risk of recurrence, and other comorbid or predisposing medical issues.
For children who develop recurrent seizures or epilepsy, treatment is begun with a single drug known to be effective for the child's seizure type and have the lowest risk of adverse side effects.
The dosage is gradually increased until the seizures are controlled.
If a child develops intolerable side effects, the medication is stopped and another one tried.
If the drug at maximum doses reduces but does not stop all seizures, a second drug is added in gradually increasing doses.
When seizures are controlled, the first drug may be tapered to reduce the potential adverse effects and drug interactions of polytherapy.
Monotherapy remains the treatment of choice for epilepsy, but a combination of medications may be a viable alternative for children who do not have total seizure control with only one medication
The ketogenic diet: is a high-fat, very-low-carbohydrate, and adequate-protein diet that has shown effectiveness for treatment of epilepsy.
It is also the first-line treatment for certain metabolic disorders, including pyruvate dehydrogenase deficiency, glucose transporter type I deficiency, and glutaric aciduria type I.
ketogenic diet forces the body to shift from using glucose as the primary energy source to using fat, and the individual develops a state of ketosis
The diet is deficient in vitamins and minerals; therefore vitamin and mineral supplementation is necessary.
Potential adverse side effects of the diet include constipation, hypoglycemia during initiation of the diet, acidosis, and lethargy. Less common but more serious side effects include urinary tract infections, kidney stones, and insufficient weight gain
Vagus Nerve Stimulation: developed as palliative treatment for patients with seizures not controlled by drugs and who are not candidates for diet or surgical therapy
A programmable signal generator is implanted subcutaneously in the chest.
Electrodes tunneled underneath the skin deliver electrical impulses to the left vagus nerve (CN X).
The device is programmed noninvasively to deliver a precise pattern of stimulation to the left vagus nerve.
The patient or caregiver can activate the device using a magnet at the onset of a seizure.
Surgery therapy: When seizures are caused by a hematoma, vascular malformation, tumor, or other cerebral lesion, surgical removal is usually recommended.
Epilepsy surgery is the most effective treatment for children with medically refractory epilepsy due to focal cortical dysplasia and mesial temporal sclerosis
26. Describe the nurse’s role in caring for a child experiencing a seizure, including safety measures, general observations, and documentation of seizure activity.
nursing responsibility is to observe the seizure episode and accurately document the events.
Record and note any alterations in behavior preceding the seizure and the characteristics of the episode, such as sensory-hallucinatory phenomena (e.g., an aura), motor effects (e.g., eye movements, muscular contractions), alterations in consciousness, and postictal state.
The nurse should describe only what is observed, rather than trying to label a seizure type.
Note the time that the seizure began and the duration of the seizure.
27. Discuss the etiology and risk factors of febrile seizures and the management of a child experiencing this event.
Febrile seizure: A febrile seizure is a seizure associated with a febrile illness in the absence of a CNS infection. By definition, children who have a febrile seizure cannot have a history of afebrile seizures, must have a temperature of at least 38°C (100.4°F), and must be between the age of 6 and 60 months
most common type of seizure, affecting 2% to 4% of children
There is evidence for both genetic and environmental causes of febrile seizures. Children with a family history of febrile seizures are at increased risk for both a single febrile seizure (10% to 46%) and for recurrent febrile seizures
If a febrile seizure lasts more than 5 minutes, parents should seek medical attention immediately. Instruct parents to call for emergency assistance (911) and not to place the child who is actively having a seizure in the car.
Most febrile seizures have stopped by the time the child is taken to a medical facility and require no treatment.
There is no benefit of antiepileptic prophylaxis in these children
The child whose seizure does not stop within 10 minutes of administration of acute treatment will need treatment for febrile status epilepticus with IV administration of both short-acting and long-acting antiepileptic medications.
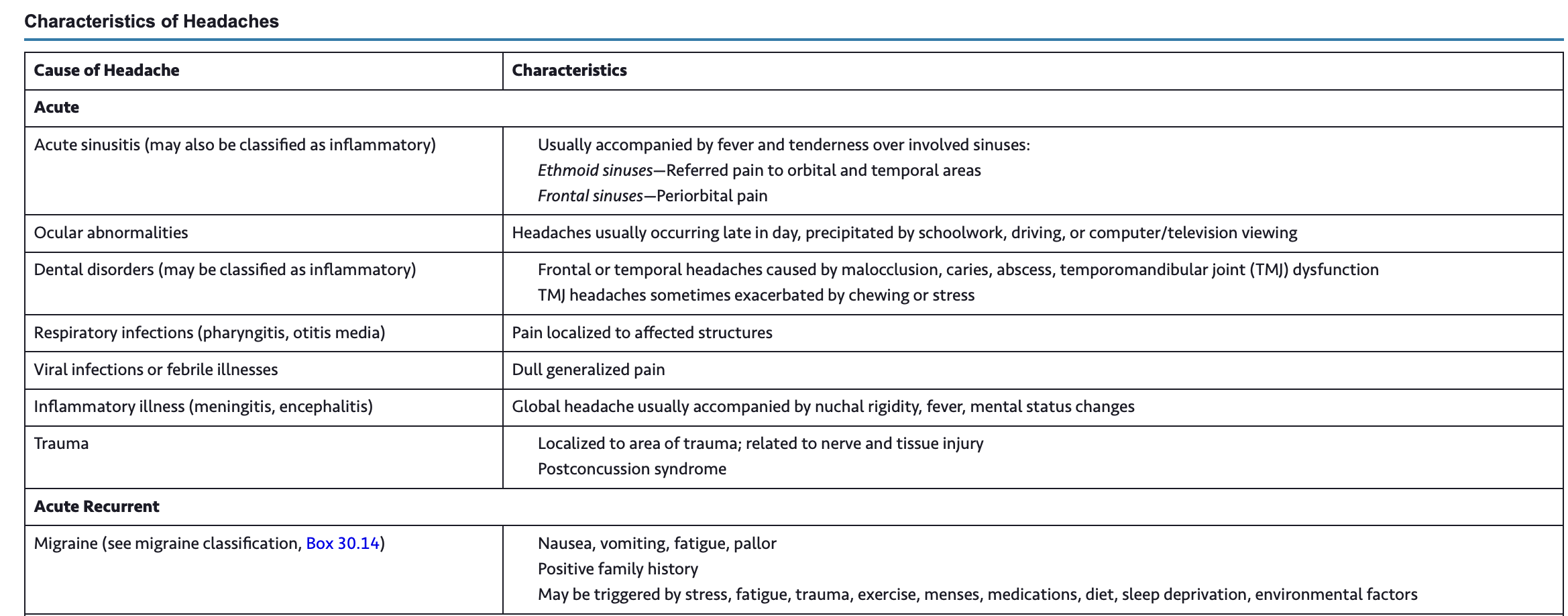
28. Discuss characteristics of headaches including acute, acute recurrent, chronic progressive, and chronic nonprogressive types.
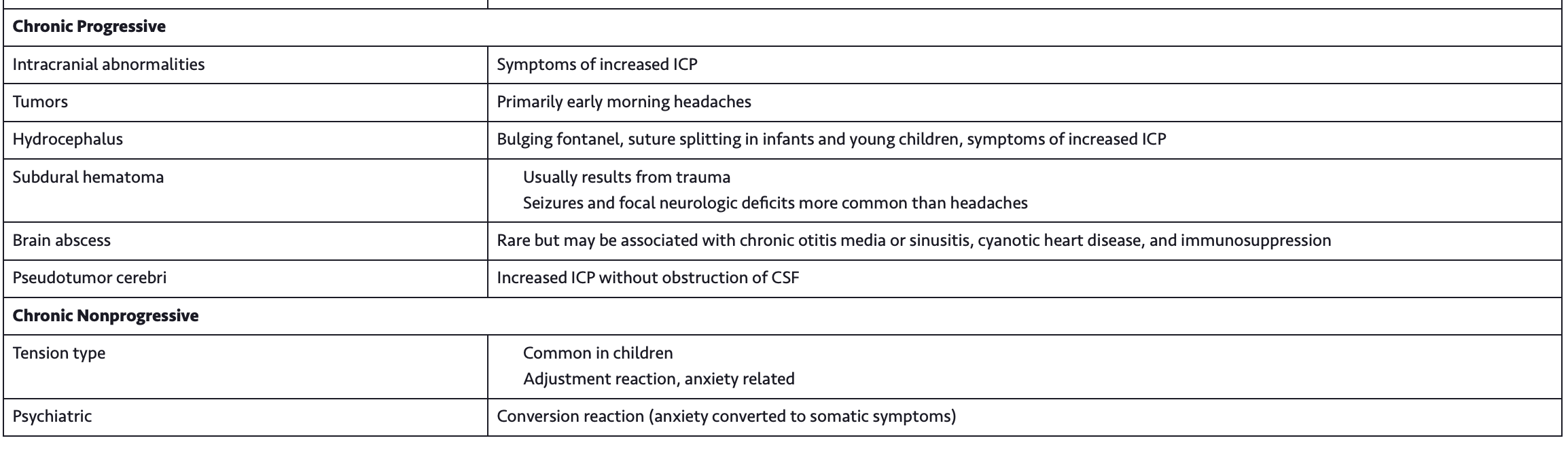
29. Discuss questions used for evaluating headaches.
30. Describe nursing indications for the treatment of migraines.
Migraine headaches occur in children as well as adults.
Typical symptoms include nausea, vomiting, and abdominal pain, which are relieved by sleep.
Migraine headaches are managed with general measures (education, a headache diary to identify and eliminate precipitating factors, and documented response to treatment), abortive treatment, and prophylactic treatment.
At the onset of the headache, the child should rest or sleep in a quiet, dark room when feasible.
Migraine therapy, if administered early in the course of the headache, may provide rapid relief.
Acetaminophen or ibuprofen is often effective if given early.
31. Discuss the pathophysiology and clinical manifestations of hydrocephalus and the therapeutic management of a child with this condition.
Hydrocephalus is a group of conditions resulting from disturbances in the dynamics of cerebral circulation and cerebrospinal fluid (CSF) caused by either
(1) impaired absorption of CSF fluid (nonobstructive or communicating hydrocephalus)
(2) obstruction to the flow of CSF through the ventricular system (obstructive or noncommunicating hydrocephalus).
Surgical treatment is the therapy of choice in almost all cases of hydrocephalus; however, most children require a shunt to promote CSF drainage.
(CM): The three factors that influence the clinical picture in hydrocephalus are the acuity of onset, timing of onset, and associated structural malformations.
In infancy, before closure of the cranial sutures, head enlargement (increasing occipitofrontal circumference [OFC]) is the predominant sign
With the increase in intracranial volume, the bones of the skull become thin and the sutures become palpably separated to produce the cracked-pot sound (Macewen sign)
on percussion of the skull. In severe cases there may be frontal protrusion, or frontal bossing, with depressed eyes, and the eyes may be rotated downward, producing a setting-sun sign, in which the sclera may be visible above the iris. Pupils are sluggish, with unequal response to light.
The infant is irritable and lethargic, feeds poorly, and may display changes in level of consciousness, opisthotonos (often extreme), and lower extremity spasticity.
The infant cries when picked up or rocked and quiets when allowed to lie still. Early infantile reflexes may persist, and normally expected responses may not appear, indicating failure in the development of normal cortical inhibition.
Infants with Chiari malformations may exhibit behaviors that reflect cranial nerve dysfunction as a result of brainstem compression, including swallowing difficulties, stridor, apnea, aspiration, respiratory difficulties, and arm weakness.
The preterm infant with posthemorrhagic hydrocephalus may not exhibit any clinical signs and symptoms other than a gradual increase in head circumference.
Childhood: early to late childhood are caused by increased ICP, and specific manifestations are related to the location of the focal lesion.
Most commonly resulting from posterior fossa neoplasms and aqueduct stenosis, the clinical manifestations are primarily those associated with space-occupying lesions (i.e., headache on awakening with improvement after emesis, papilledema, strabismus, and extrapyramidal tract signs such as ataxia.
As with infants, the child is irritable, lethargic, apathetic, confused, and often incoherent.
In one of the congenital defects with later onset (by age 3 months), the Dandy-Walker syndrome, characteristic manifestations are a bulging occiput, nystagmus, ataxia, and cranial nerve palsies.
Manifestations of Chiari malformation in children over 3 years of age are related to spinal cord dysfunction rather than brainstem compression as observed in infants.
Scoliosis proximal to the level of the myelomeningocele (usually associated with Chiari malformation) and development of upper extremity spasticity, which may progress to weakness and atrophy, are common.